Abstract
Background
Several barriers to the adoption of electronic medical records (EMRs) by family physicians have been discussed, including the costs of implementation, impact on work flow and loss of productivity. We examined billings and payments received before and after implementation of EMRs among primary care physicians in the province of Ontario. We also examined billings and payments before and after switching from a fee-for-service to a capitation payment model, because EMR implementation coincided with primary care reform in the province.
Methods
We used information from the Electronic Medical Record Administrative Data Linked Database (EMRALD) to conduct a retrospective before–after study. The EMRALD database includes EMR data extracted from 183 community-based family physicians in Ontario. We included EMRALD physicians who were eligible to bill the Ontario Health Insurance Plan at least 18 months before and after the date they started using EMRs and had completed a full 18-month period before Mar. 31, 2011, when the study stopped. The main outcome measures were physicians’ monthly billings and payments for office visits and total annual payments received from all government sources. Two index dates were examined: the date physicians started using EMRs and were in a stable payment model (n = 64) and the date physicians switched from a fee-for-service to a capitation payment model (n = 42).
Results
Monthly billings and payments for office visits did not decrease after the implementation of EMRs. The overall weighted mean annual payment from all government sources increased by 27.7% after the start of EMRs among EMRALD physicians; an increase was also observed among all other primary care physicians in Ontario, but it was not as great (14.4%). There was a decline in monthly billings and payments for office visits after physicians changed payment models, but an increase in their overall annual government payments.
Interpretation
Implementation of EMRs by primary care physicians did not result in decreased billings or government payments for office visits. Further economic analyses are needed to measure the effects of EMR implementation on productivity and the costs of implementing an EMR system, including the costs of nonclinical work by physicians and their staff.
Canadian primary care physicians lag in the adoption of information technology, ranking last out of 11 industrialized countries in use of electronic medical records (EMRs).1 Several barriers to the adoption of EMRs within primary care have been identified, including confusion with the array of products available in the market, lack of expertise, security and privacy concerns, costs of implementation, impact on work flow and loss of productivity.2–5 Some of these barriers have been addressed through programs such as OntarioMD’s EMR Adoption Program, through which financial support and coaching is provided to physicians to assist with converting from paper charts and records to EMRs.6
The conversion to an EMR system requires additional nonclinical work for family physicians and their staff.4,5 However, the impact on productivity and income has been examined in few studies. A case study of qualitative data for the implementation of electronic health records in California found that the costs of implementation were recovered within about 2.5 years, after which clinic profits continued to improve.7 Another US study measured the effect of implementing electronic health records by examining episodic treatment groups based on case-mix–adjusted payments to providers; no change in short-term costs per episode were observed.8 Although concern persists that implementing EMRs will affect productivity and potentially income, we are unaware of any studies that have evaluated changes in billings or physician income related to adopting EMRs in Canada.
For many family physicians in Ontario, EMR adoption coincided with primary care reform in the province.9 In the past decade, the Ontario Ministry of Health and Long-Term Care introduced a number of new primary care enrolment models, starting with Family Health Networks, which include a base payment per patient for the provision of comprehensive care (capitation) plus incentives, premiums and bonuses for providing preventive care and managing certain chronic diseases.10 Family Health Groups were then introduced; this enhanced fee-for-service model offers fee-for-service payments plus bonuses and incentives for achieving targets, such as the proportion of patients receiving preventive care. Family Health Organizations came next and are also based on capitation-based physician payments. Finally, Family Health Teams were developed; this model expands interdisciplinary care within a family practice. The introduction of these payment models has had a substantial impact on family physicians’ incomes since 2005.11
We examined whether family physicians’ billings and payments received for office visits, and total payments received from all government sources, would be affected by the implementation of EMRs. Because a change in payment model could also affect billings and payments, we also examined separately the effect of switching from a fee-for-service to a capitation payment model.
Methods
Study design
We conducted a retrospective before–after study of billings and payments received for office visits, as well as total annual payments received from all government sources, among primary care physicians in Ontario. We used the date they implemented EMRs or the date they changed from a fee-for-service payment model (traditional fee for service or Family Health Group) to a capitation-based model (Family Health Network, Family Health Organization or Family Health Team) as the index dates.
Data sources
The EMR-related information used in this study came from the Electronic Medical Record Administrative Data Linked Database (EMRALD).12 The database was started in 2007 using a mechanism to extract and securely transfer data provided by enrolled Ontario physicians using Practice Solutions EMR software; the data are linked to the health administrative data held at the Institute for Clinical Evaluative Sciences. Practice Solutions EMR software is the most frequently adopted government-supported EMR software in Ontario.13 At the time this study was conducted, there were 183 community-based family physicians contributing their primary care data to EMRALD.
For this study, we linked data from the EMRALD database with those from the Ontario Health Insurance Plan (OHIP) database of physician fee-for-service billings and shadow billings (where physicians participating in capitation models submit billing claims primarily for administrative purposes rather than for remuneration). Physicians were linked by encrypted OHIP billing numbers, and patient data were linked by key numbers assigned by the Institute for Clinical Evaluative Sciences; the key numbers are an encrypted form of health card number. No identifying information was used.
Study cohorts
We included family physicians enrolled in EMRALD who were eligible to bill OHIP at least 18 months before and 18 months after the date they started using EMRs. We used the Corporate Provider Database to determine OHIP billing eligibility. Because our study period ended Mar. 31, 2011, we excluded physicians who started using EMRs less than 18 months before that date. The EMR start date was defined as the day on which there were at least 5 progress notes with billings in the physician’s EMR record. Of the 183 family physicians enrolled in EMRALD at the time of the study, 68 did not meet the inclusion criteria: 14 had less than 18 months of billings after their EMR start date, 39 did not have 18 months of billings before their EMR start date, and 15 had insufficient look-back and follow-up times.
For the analysis of the effect of changing from a fee-for-service payment model to a capitation model, we selected family physicians who switched to a capitation model more than 18 months before they started using EMRs (n = 42). This ensured that the 18-month follow-up period after switching payment models did not include their EMR start date.
To get the most accurate estimate of the effect of EMR implementation on billings and payments, we constructed a cohort of 64 physicians whose payment model did not change during the 18 months before and the 18 months after their EMR start date. This cohort included the 42 physicians in the payment-model cohort (because they switched payment models more than 18 months before their EMR start date) and 22 physicians whose payment model either did not change 18 months before or after their EMR start date or changed more than 18 months after the EMR start date.
Study periods
For the EMR analyses, the maximum follow-up date was Mar. 31, 2011. Therefore, the latest EMR start date included in the study was 18 months before that date. Look-back and follow-up periods were 18 months before and 18 months after each EMR start date (Appendix 1, available at www.cmajopen.ca/content/1/3/E120/suppl/DC1).
For the study examining the effect of changing from a fee-for-service to a capitation payment model, the date on which the physician switched had to be more than 18 months before his or her EMR start date. The look-back and follow-up periods were 18 months before and 18 months after the capitation start date (Appendix 1).
Outcome measures
The primary outcome measures were physicians’ monthly billings and payments received for office visits and total annual payments received from all government sources. Billings for office visits included OHIP billings for assessments and consultations. We excluded visits that took place in an emergency department, hospital, long-term care facility or patient’s home. Billings for procedures were also excluded. Payments for office visits were the sum of all OHIP fee-for-service payments for office visits as defined above.
To estimate the impact of implementing EMRs or switching payment models on payments received from all government sources, not just fee-for-service payments for office visits, we used data generated for the report “Payments to Ontario Physicians from Ministry of Health and Long-Term Care Sources.”11 These data included fee-for-service payments plus payments from a number of other sources and mechanisms, such as alternate payment plans, capitation and a variety of incentives, bonuses and premiums. The data are calculated for individual physicians but are available only for an entire fiscal year. Thus, the pre-capitation or pre-EMR year is defined as the full fiscal year before, but not including, the capitation or EMR start date. Similarly, the post-capitation or post-EMR year is the first full fiscal year after the year containing the capitation or EMR start date.
Generalizability of data
We compared characteristics of the 183 physicians enrolled in EMRALD in 2010/11 with those of all other general practitioners and family physicians in Ontario in that period who had active practices (n = 11 385). Characteristics included age, sex, location of undergraduate medical training (Canada v. elsewhere), practice rurality (rural, suburban or urban), proportion of billed visits in emergency departments and full-time affiliation with a patient-enrolment model.9,10 We also compared patients who visited EMRALD physicians (n = 286 177) with patients of all other family physicians in primary care models with rostered patients (n = 9 728 198) and who had used health services in Ontario in the past 7 years. Patient characteristics included age, sex, socioeconomic status (income quintile), rurality, degree of comorbidity (determined by the number of Adjusted Clinical Groups, with 0 = no comorbidity and ≥ 10 = high comorbidity), and medical history (prior acute myocardial infarction, current diabetes, hypertension, chronic obstructive pulmonary disease, asthma, congestive heart failure or mental health issues).
Statistical analysis
We summed the number of billings for office visits by physician for each month. We then calculated the monthly average across all physicians in a given study cohort. Recognizing that situations such as maternity, illness and parental leave could result in a drop in billings that would erroneously be attributed to EMR implementation or a change in payment model, the average for each month was based only on data for physicians who had at least 50 billings during the month.
To determine the effect of implementing EMRs or of switching to a capitation model, we calculated the mean number of billings and payments for office visits before and after the respective index date. We used a t test to determine statistical significance and conducted an interrupted time series analysis to test for a change in the slope before and after the index dates using SAS software (version 9.1 of the SAS System for Unix, SAS Institute Inc.).
For total payments from all government sources, we calculated the mean annual payments from all sources before and after the change to a capitation model or the start of EMRs. The total weighted mean was estimated by weighing the mean annual payment by the number of family physicians in each year from 2005 to 2009. The percentage change was calculated as the mean payment after the change (change to capitation or start of EMRs) minus the mean payment before the change, divided by the mean payment before the change.
Results
Physician and patient characteristics
The characteristics of the 183 family physicians enrolled in EMRALD and all other primary care physicians in active practice in Ontario in 2010/11 are provided in Table 1. Physicians in EMRALD were younger and more likely to be female, to be a Canadian medical graduate and to participate in a patient-enrolment model. They were also less likely to practise in urban locations.
Table 1: Characteristics of 183 family physicians (FPs) enrolled in EMRALD* and all other general practitioners/family physicians (GP/FPs) in Ontario in 2010/11.
| Group; no. (%) of physicians or mean ± SD |
|||
|---|---|---|---|
| Characteristic | EMRALD FPs n = 183 |
All other GP/FPs n = 11 385 |
p values |
| Sex |
|||
| Male |
85 (46.4) |
6833 (60.0) |
0.008 |
| Female |
98 (53.6) |
4552 (40.0) |
0.007 |
| Age group, yr |
|||
| < 35 |
35 (19.1) |
1094 (9.6) |
0.08 |
| 35−44 |
63 (34.4) |
2617 (23.0) |
0.04 |
| 45−54 |
38 (20.8) |
3312 (29.1) |
0.4 |
| ≥ 55 |
47 (25.7) |
4362 (38.3) |
0.1 |
| Age, yr, mean ± SD |
44.9 ± 10.8 |
50.6 ± 11.8 |
< 0.001 |
| Location of medical training |
|||
| Canada |
157 (86.6) |
8731 (76.7) |
0.005 |
| Elsewhere |
16 (8.3) |
2647 (23.2) |
0.2 |
| Missing data |
10 (5.1) |
7 (0.1) |
– |
| No. of years in practice, mean ± SD |
14.0 ± 9.7 |
17.0 ± 9.3 |
< 0.001 |
| Rurality |
|||
| Rural |
35 (19.1) |
850 (7.5) |
0.02 |
| Suburban |
40 (21.9) |
1871 (16.4) |
0.4 |
| Urban |
108 (59.0) |
8664 (76.1) |
< 0.001 |
| % billing more than 25% of patient visits in an emergency department |
15.3 |
13.7 |
0.4 |
| Full-time affiliation with a patient enrolment model group on Mar. 31, 2011 | 173 (94.5) | 6866 (60.3) | < 0.001 |
Note: EMRALD = Electronic Medical Record Administrative Data Linked Database, SD = standard deviation. *Family physicians who started using EMR software and were contributing data to this database at the time of the study.
When comparing characteristics of patients of physicians in the 2 groups, we found no major differences in distribution by age or sex (Table 2). Higher proportions of patients of physicians in EMRALD were in the highest income quintile and lived in rural and suburban regions. A slightly higher proportion of patients of EMRALD physicians had no or lower comorbidity, and lower proportions had diabetes or hypertension. We did not find a difference between the patient groups with respect to the proportion who had a previous acute myocardial infarction, asthma, congestive heart failure, chronic obstructive pulmonary disease or mental health issues.
Table 2: Characteristics of patients of 183 family physicians (FPs) enrolled in EMRALD* and rostered patients of all other general practitioners/family physicians (GP/FPs) in Ontario in 2010/11.
| Characteristic | Patients of EMRALD FPs, % n = 286 177 |
Patients of all other GP/FPs, % n = 9 728 198 |
|---|---|---|
| Sex |
||
| Male |
45.4 |
47.4 |
| Female |
54.6 |
52.6 |
| Age group, yr |
||
| ≤ 4 |
6.3 |
4.0 |
| 5−17 |
13.4 |
14.6 |
| 18−29 |
14.9 |
15.1 |
| 30−44 |
21.6 |
20.5 |
| 45−64 |
28.3 |
30.2 |
| 65−74 |
7.7 |
8.3 |
| 75−84 |
5.3 |
5.3 |
| ≥ 85 |
2.5 |
2.0 |
| Income quintile |
||
| 1 (lowest) |
16.8 |
17.7 |
| 2 |
17.7 |
19.3 |
| 3 |
18.9 |
20.3 |
| 4 |
21.0 |
21.7 |
| 5 (highest) |
23.9 |
20.7 |
| Unknown/missing data |
1.8 |
0.3 |
| Rurality |
||
| Rural |
14.9 |
5.5 |
| Suburban |
20.0 |
17.6 |
| Urban |
65.0 |
76.9 |
| No. of adjusted clinical groups (comorbidity) |
||
| 0 (no comorbidity) |
7.6 |
6.2 |
| 1−5 |
48.0 |
45.7 |
| 6−9 |
35.9 |
39.4 |
| ≥ 10 (high comorbidity) |
8.5 |
8.6 |
| Chronic condition |
||
| Previous acute MI |
1.3 |
1.3 |
| Asthma |
14.0 |
14.7 |
| Congestive heart failure |
2.1 |
1.8 |
| COPD |
6.3 |
6.3 |
| Diabetes |
8.3 |
9.7 |
| Hypertension |
20.7 |
22.9 |
| Mental health issue |
21.4 |
20.8 |
| ≥ 1 chronic condition† | 46.5 | 50.4 |
Note: COPD = chronic obstructive pulmonary disease, EMRALD = Electronic Medical Record Administrative Data Linked Database, MI = myocardial infarction. *Family physicians who started using EMR software and were contributing data to this database at the time of the study. †One or more of asthma, congestive heart failure, COPD, diabetes, hypertension or mental health issue.
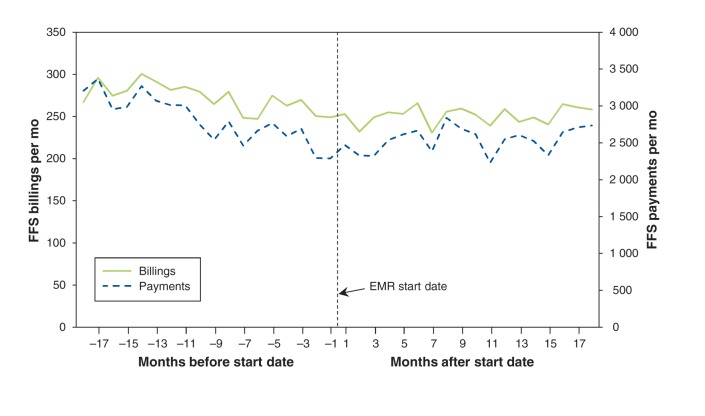
Effect of implementing EMRs
Figure 1 shows the mean number of monthly billings and payments for office visits before and after the implementation of EMRs among the 64 family physicians in EMRALD who did not change their payment model during the 18 months before and after the EMR start date. During the 18 months before the EMR start date, there was a significant decline in both the mean number of monthly billings (slope −2.05, 95% CI −3.23 to −0.88) and the mean number of monthly payments (slope −52.1, 95% CI −66.7 to −37.5). After the EMR start date, monthly billings and payments stabilized, with no significant change during the 18-month follow-up period (billings: slope 0.47, 95% CI −0.50 to 1.44; payments: slope 10.1, 95% CI −5.3 to 25.6).
Figure 1:
Mean number of billings and payments received for office visits per month before and after implementing electronic medical records (EMRs) among 64 family physicians who did not change their primary care payment model in the 18 months before or after the EMR start date. FFS = fee for service.
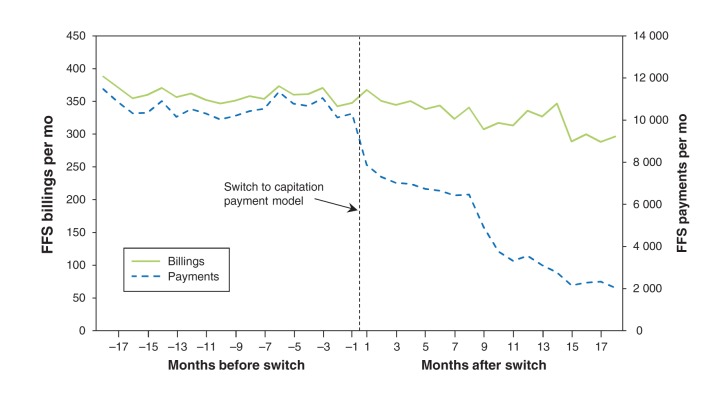
Effect of switching to capitation model
Figure 2 shows the mean number of monthly billings and payments for office visits before and after the switch to a capitation model among the 42 family physicians in EMRALD who made the switch at least 18 months before their EMR start date. There was a decline in monthly billings during the 18 months before switching payment models; however, the change was not statistically significant (slope −0.93, 95% confidence interval [CI] −1.91 to 0.06). The decline in billings for office visits after changing payment models was significant (slope −0.36, 95% CI −4.94 to −2.22), as was the decline in monthly payments for office visits (slope −385.9, 95% CI −437.0 to −334.8). There was no statistically significant change in payments before changing models (slope −10.5, 95% CI −50.8 to 29.7).
Figure 2:
Mean number of billings and payments received for office visits per month before and after switching from fee-for-service to capitation payment model among 42 family physicians not using electronic medical records. FFS = fee for service.
Effect on total payments
The mean total payments received from all government sources increased by 20.9% in the fiscal year after implementation of EMRs among the 64 family physicians from EMRALD included in this analysis. A larger increase in total annual payments (44%) was observed after the switch to a capitation model among the 42 family physicians from EMRALD included in this analysis.
When we compared mean annual payments from all government sources before and after EMRs were started among family physicians in EMRALD with the mean annual payments among all other primary care physicians in Ontario during the same period, we noted increases in both physician groups (Table 3). The increases among the EMRALD physicians were larger than those for the other physicians in every year except 2007 and 2009. The overall weighted mean annual payment increased by 27.7% after the start of EMRs among the physicians enrolled in EMRALD. An increase was also observed among the other primary care physicians in Ontario during the same time interval, but it was not as great (14.4%).
Table 3: Mean total annual payments from all government sources before and after implementation of EMRs for family physicians (FPs) enrolled in EMRALD* and for all other general practitioners/family physicians (GP/FPs) in Ontario during the same period.
| EMRALD FPs |
All other GP/FPs |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| EMR start | No. who started using EMRs | Mean annual payment in pre-EMR yr† |
Mean annual payment in post-EMR yr‡ | % change | No. of physicians | Mean annual payment in same yr as pre-EMR yr† | No. of physicians | Mean annual payment in same yr as post-EMR yr‡ | % change |
| 2005 |
18 |
191 342 |
351 251 |
83.6 |
9 865 |
183 570 |
10 046 |
243 427 |
32.6 |
| 2006 |
38 |
200 836 |
256 882 |
27.9 |
10 129 |
214 025 |
10 149 |
248 381 |
16.1 |
| 2007 |
8 |
196 967 |
210 036 |
6.6 |
10 046 |
243 427 |
10 352 |
273 962 |
12.5 |
| 2008 |
12 |
257 110 |
347 938 |
35.3 |
10 149 |
248 381 |
10 666 |
285 366 |
14.9 |
| 2009 |
26 |
271 144 |
275 190 |
1.5 |
10 352 |
273 962 |
10 872 |
279 978 |
2.2 |
| Total weighted mean | 223 399 | 285 240 | 27.7 | 233 100 | 266 679 | 14.4 | |||
Note: EMR = electronic medical record, EMRALD = Electronic Medical Record Administrative Data Linked Database. *Family physicians who started using EMR software and were contributing data to this database. †The pre-EMR year is the full fiscal year before, but not including, the EMR start date. ‡The post-EMR year is the first full fiscal year after the year containing the EMR start date.
Interpretation
We found that, among the family physicians in our study who implemented EMRs, their monthly billings and payments for office visits declined in the 18 months before starting EMRs and then stabilized after their EMR start dates. The overall annual payments from all government sources increased after EMR implementation, similar to the increases seen among all other primary care physicians in Ontario. Among the family physicians in our study who changed from a fee-for-service to a capitation payment model, their monthly billings and payments for office visits decreased in the 18 months after the switch. However, their overall annual payments from all government sources increased during the same period.
Family physicians who participate in capitation models are supposed to submit their claims (shadow billings). In an effort to encourage the submission of shadow billings, the provincial government provides a small proportion of the payment for these claims as an incentive.14,15 However, there is work associated with submitting billing information, and family physicians may not bother to submit claims for all of their patient encounters. The decline in billings observed before the EMR start date may therefore have been a continuation of the decline in billings after switching payment models. Total payments from all government sources increased after the EMR start date, but increases were generally seen for all primary care physicians in Ontario over time.11 One possible explanation for the plateau in billings observed after implementing EMRs is that the use of EMR-provided billing features made it easier to submit claims. Also, during this time, more billing options were introduced for physicians participating in the newer primary care models, and this stabilization may have reflected uptake of these new codes.
For primary care physicians in Ontario, billings or claims do not equal income. Many physicians now receive most of their payments as capitation payments for rostered patients. Additional sources of revenue include bonus payments, incentive payments for rural practice and other global payments. Physicians may also receive payments directly from patients for services not covered by the government (e.g., fees for cosmetic procedures and block fees [annual fees charged to patients for a number of services not covered by OHIP, such as sick notes for work, copy and transfer of medical records, and prescription refills over the phone]), which were not included in our analyses. Electronic medical records may assist practices with tracking, flagging and reporting some of these services for payments. However, adoption of EMRs among physicians in Canada, including the use of the full functionality of EMRs to track their work, is not well known.16 Also, payments to family physicians do not include the costs associated with running a practice, including the costs associated with implementing an EMR system. Financial help was made available to family physicians via OntarioMD for start-up costs. Nevertheless, much nonclinical work and time is taken by physicians and their staff when they adopt an EMR system, and we did not estimate the costs associated with this learning curve.
A systematic review of the potential benefits and limitations of EMRs in primary care practices found structural benefits of EMRs compared with paper records, including improving legibility, encouraging patient questions and completeness of encounters, keeping medical records up to date and improving the quality of the medical record overall.17 Another systematic review revealed some, but limited, positive benefits of EMRs on physicians’ practices in certain areas, including prescribing support, disease management, work practice and preventive care.18 A recommendation from this review was for studies to demonstrate value for money.
Limitations
We included a convenience sample of family physicians enrolled in EMRALD who differed in some characteristics from other primary care physicians in Ontario. The proportion of physicians who had rural practices was higher in our study. Although incentive payments for rural practices are included in the total government payments, there may be other independent factors related to rural practices that influence billings. Our study did not have a sufficient sample size to examine any interactions between provider or patient characteristics and billings or payments. Currently, data about EMR use for all Ontario primary care physicians is not available. For the analysis of total government payments, the comparison with all other primary care physicians in Ontario included physicians who also started using EMRs; therefore, this is not a comparison of EMR and non-EMR users. Our study did not include income for noninsured services. There may be an association between EMR use and income from noninsured services, but the direction of this income has not been well documented. We included family physicians whose EMR software is from a single vendor, which may limit the generalizability to those using EMR software from other vendors or to specialists who start using EMRs.
Conclusion
We found that monthly billings and payments received for office visits did not decrease after family physicians in the study cohort started using EMRs. The overall weighted mean annual payment from all government sources increased after they implemented EMRs, similar to increases among all other primary care physicians in Ontario. There was a decline in monthly billings and payments for office visits after family physicians changed from a fee-for-service to a capitation payment model, but their total annual payments from all government sources increased during the same period. Further economic analyses are needed to measure the effects of EMR implementation on productivity and the costs of starting an EMR system, including the costs of nonclinical work by physicians and their staff.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/1/3/E120/suppl/DC1
Supplementary Material
References
- 1.Schoen C, Osborn R, Doty MM, et al. A survey of primary care physicians in eleven countries, 2009: perspectives on care, costs, and experiences. Health Aff (Millwood) 2009;28:w1171-83 [DOI] [PubMed] [Google Scholar]
- 2.Matambo W. EMR lessons learned: taking a page from Denmark, New Zealand & UK: George Brown student delves into EMR lessons learned in a winning student essay. Healthcare Info Manage Commun Can 2012;56-58. Available: www.coachorg.com/en/resourcecentre/resources/Student-Essay.pdf (accessed 2012 Oct. 30).
- 3.Terry AL, Giles G, Brown JB, et al. Adoption of electronic medical records in family practice: the providers’ perspective. Fam Med 2009;41:508-12 [PubMed] [Google Scholar]
- 4.Ludwick D, Manca D, Doucette J. Primary care physicians’ experiences with electronic medical records. Can Fam Physician 2010;56:40-7 [PMC free article] [PubMed] [Google Scholar]
- 5.Joos D, Chen Q, Jirlis J, et al. An electronic medical record in primary care: impact on satisfaction, work efficiency and clinic processes. AMIA Annu Symp Proc 2006;394-8 [PMC free article] [PubMed] [Google Scholar]
- 6.New EMR Adopter Funding Program. Toronto (ON): OntarioMD; 2013. Available: www.ontariomd.ca/portal/server.pt/community/emr_funding/new_emr_adopters (accessed 2012 Nov. 1).
- 7.Miller RH, West C, Brown TM, et al. The value of electronic health records in solo or small group practices. Health Aff (Millwood) 2005;24:1127-37 [DOI] [PubMed] [Google Scholar]
- 8.Welch WP, Bazarko D, Ritten K, et al. Electronic health records in four community physician practices: impact on quality and cost of care. J Am Med Inform Assoc 2007;14:320-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutchison B, Levesque JF, Strumpf E, et al. Primary health care in Canada: systems in motion. Milbank Q 2011;89:256-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collier R. Shifting towards capitation. CMAJ 2009;181:668-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henry DA, Schultz SE, Glazier RH, et al. Payments to Ontario physicians from Ministry of Health and Long-Term Care sources, 1992/93 to 2009/10: ICES investigative report Toronto (ON): Institute for Clinical Evaluative Sciences; 2012. Available: www.ices.on.ca/file/ICES_PhysiciansReport_2012.pdf (accessed 2012 Oct. 30).
- 12.Tu K, Mitiku T, Ivers N, et al. Validation of an Electronic Medical Record Administrative Data Linked Database (EMRALD) [abstract]. Proceedings of the 2011 North American Primary Care Research Group annual meeting; 2011 Nov. 12–16; Banff (AB). Fam Med J 2012;44(Suppl 1). [Google Scholar]
- 13.Liston T, Kew J. QHR Technologies Inc.: a play on electronic medical record (EMR) adoption in Canada; initiating coverage. Equity Research, Versant Partners; 2011 Jan. 21.
- 14.Wranik DW, Durier-Kopp M. Physician remuneration methods for family physicians in Canada: expected outcomes and lessons learned. Health Care Anal 2010;18:35-59 [DOI] [PubMed] [Google Scholar]
- 15.Wooder SD. Primary care compensation models [Hamilton Niagara Haldimand Brant Board presentation]. Toronto (ON): Ontario Medical Association; 2011. Available: www.hnhblhin.on.ca/uploadedFiles/Public_Community/Board_of_Directors/Board_Meeting/Primary%20Care%20Compensation%20Models%20-%20LHIN%20Presentation%20-%20Wooder-FINAL%20revised.pdf (accessed 2012 Oct. 1).
- 16.Price M, Singer A, Kim J. Adopting electronic medical records: Are they just electronic paper records? Can Fam Physician 2013;59:e322-9 [PMC free article] [PubMed] [Google Scholar]
- 17.Holroyd-Leduc JM, Lorenzetti D, Straus SE, et al. The impact of the electronic medical record on structure, process, and outcomes within primary care: a systematic review of the evidence. J Am Med Inform Assoc 2011;18:732-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lau F, Price M, Boyd J, et al. Impact of electronic medical record on physician practice in office settings: a systematic review. BMC Med Inform Decis Mak 2012;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.