Abstract
Objectives
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study aims to examine associations between sociocultural and psychosocial factors and cardiovascular disease (CVD) and metabolic syndrome prevalence in Hispanics/Latinos. The conceptual framework is based on the Reserve Capacity and Lifespan Biopsychosocial Models, which emphasize multiple risk and protective pathways underlying socioeconomic and ethnic influences in health. This study describes the rationale, participants, and procedures for the HCHS/SOL Sociocultural Ancillary Study.
Design and Setting
The Sociocultural Ancillary Study to the HCHS/SOL is a cross-sectional cohort study with future opportunities for prospective investigation.
Participants
Participants were 5,313 adults, aged 18-74 years, of self-identified Hispanic/Latino descent and representing multiple Hispanic/Latino background groups, recruited from the Bronx, NY, Chicago, IL, Miami, FL, and San Diego, CA.
Intervention
Participants completed an interview-administered sociocultural assessment battery within 9 months of their HCHS/SOL clinical baseline exam.
Outcome Measures
The primary outcomes are CVD and the metabolic syndrome and its component risk factors.
Results
The Sociocultural Ancillary Study sample is broadly representative of the HCHS/SOL cohort. Weighted demographics are: 55% male, 56% 18-44 years, 44% 45 years and older, and 37% Mexican, 20% Cuban, 16% Puerto Rican, 12% Dominican, 8% Central American, and 5% South American descent.
Conclusions
By testing theoretically driven hypotheses concerning sociocultural and psychosocial factors in CVD, the Sociocultural Ancillary Study seeks to inform future prevention and intervention efforts for U.S. Hispanic/Latinos.
Keywords: Cardiovascular Disease, Culture, Hispanic, Latino, Metabolic Syndrome, Psychosocial Factors, Social Factors
Introduction
The Hispanic/Latino population grew by 43% between 2000 and 20101 and Hispanics/Latinos are expected to comprise 30% of the U.S. population by 2050.2 The terms Hispanic or Latino encompass more than 20 national origins groups, with substantial diversity in ancestry, sociodemographic and cultural characteristics, migration, and U.S. geographic distribution. However, many studies have evaluated the Hispanic/Latino population as a unitary entity or have examined individual ethnic groups (e.g., Mexican Americans). Therefore, critical knowledge gaps limit progress in effectively addressing the health needs of the Hispanic/Latino population.
To contribute a clearer picture of Hispanic/Latino health, the National Institutes of Health (NIH) and the National Heart, Lung and Blood Institute (NHLBI) and established the Hispanic Community Health Study/Study of Latinos (HCHS/SOL).3,4 This landmark epidemiologic cohort study includes more than 16,000 Hispanics/Latinos aged 18-74 years, representing multiple Hispanic/Latino backgrounds, recruited from four U.S. communities. The goals are to describe the prevalence of risk and protective factors of CVD, pulmonary disease, and other chronic diseases, and to quantify all-cause mortality, fatal and non-fatal CVD, and pulmonary disease exacerbation over time. The first study based on the HCHS/SOL cohort reported relatively low rates of self-reported heart disease and stroke, but high rates of CVD risk factors that were comparable or greater to those identified in non-Hispanic Whites in other national studies.5 Prevalence of individual risk factors varied significantly across Hispanic/Latino background groups. Participants who were born in the U.S. were at greater risk than first-generation immigrants for CVD and multiple risk factors; greater duration in the U.S. was also associated with higher CVD prevalence. These findings demonstrate the need to look beyond pan-ethnic groupings to examine patterns of CVD and associated risk factors within the diverse U.S. Hispanic/Latino population.
Sociocultural factors are posited to have an important role in Hispanic/Latino health. However, most studies in this area have been limited to proxy indicators of acculturation, such as nativity or language preference.6 Researchers have called for expanding this area with studies that examine specific processes that may help explain epidemiological patterns in Hispanic/Latino health.7,8 Other research suggests that psychosocial factors (e.g., depression, social support) predict CVD incidence and progression, with effect magnitudes similar to those of traditional risk factors.9 However, to date only limited research has addressed psychosocial influences in health among Hispanics/Latinos. The HCHS/SOL included brief assessments of select sociocultural factors,3 but did not include well-established measures of psychosocial constructs related to CVD, such as social support, stress, and intrapersonal resources (e.g., optimism), or cultural constructs with purported relevance to Hispanic/Latino health, including spirituality, gender roles, and family relationships.
In 2009, the HCHS/SOL Sociocultural Ancillary Study was initiated to expand the focus on socioeconomic, cultural, and psychosocial processes in the HCHS/SOL. The aims of the HCHS/SOL Sociocultural Ancillary Study are: 1) To examine associations of sociocultural and psychosocial factors with CVD and metabolic syndrome prevalence10 and its component risk factors (i.e., obesity, diabetes, hypertension, dyslipidemia) among HCHS/SOL participants and 2) to simultaneously examine the relative contributions of multiple sociocultural and psychosocial determinants of CVD prevalence and the metabolic syndrome and its components, using structural equation modeling (SEM). The sociocultural assessment battery was chosen with attention to psychometric considerations and appropriateness for use in Hispanic/Latinos. Nonetheless, one obstacle to examining sociocultural influences in Hispanic/Latino health is the lack of systematic evidence regarding measurement properties of relevant scales. Thus, a secondary aim of the study is to thoroughly examine the psychometric characteristics of key assessment instruments.
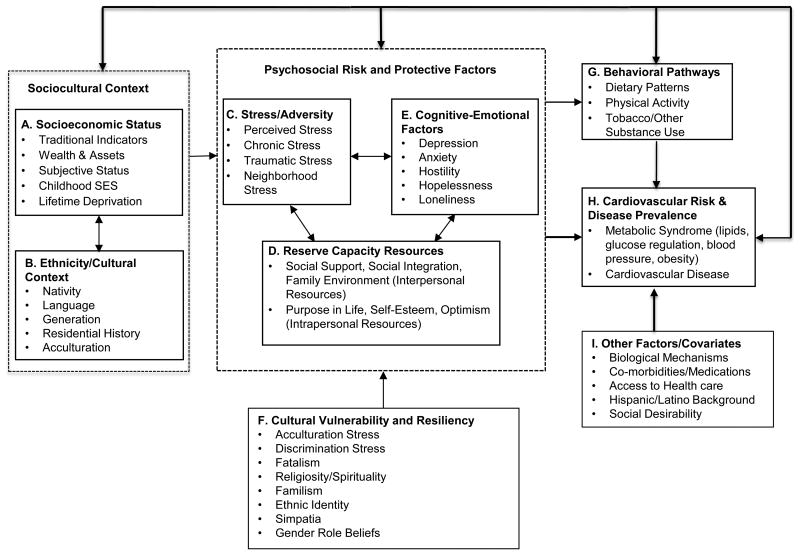
The guiding conceptual framework for the HCHS/SOL Sociocultural Ancillary Study blends elements of the Reserve Capacity Model, which focuses on psychosocial risk and resource factors underlying socioeconomic status (SES)-related health disparities,8,11 and the Lifespan Biopsychosocial Model, which focuses on multiple psychosocial and biobehavioral pathways that explain how ethnicity/race and SES combine to influence health across the lifespan.12 Thus, as shown in Figure 1, the framework suggests that SES combined with ethnic/cultural context shapes psychosocial risk and protective factors in several domains. First, aspects of the sociocultural context (e.g., low SES, acculturation) may increase exposure to stress and adversity across the lifespan, while reducing positive events. Second, such processes may shape psychosocial risk (e.g., negative emotions) and protective factors (e.g., social support). The detrimental effects of stress may be compounded by lower resources with which to manage life's demands, and fewer opportunities to replenish resources as a consequence of ongoing stress exposure. These protective resources have been referred to as “Reserve Capacity”.11,12 Limited protective resources may create feedback loops that perpetuate stress and related negative cognitive-emotional states.
Figure 1. Conceptual Model of Sociocultural & Psychosocial Influence on CVD Risk and Prevalence.
As shown in Figure 1, the model also accounts for culturally driven processes that have been proposed as possible protective or risk factors in Latino health.8 Hispanics/Latinos may experience a high burden of stress due to SES disadvantage, immigration experiences, or ethnic discrimination. However, traditional Hispanic/Latino values could bear resources, such as high family interconnectedness and spirituality, that mitigate exposure to or effects of stress.8,13 Empirical studies supporting the associations of cultural factors with objective health outcomes are scarce. Thus, our conceptual framework addresses criticisms of the acculturation literature, and its typical emphasis on proxy indicators,14 by directly examining the explicit beliefs (e.g., fatalism), values (e.g., family interdependence, gender roles), and behaviors (e.g., religiosity, social integration) that may help explain how Hispanic/Latino ethnicity relates to health.
The proposed conceptual model will be used to guide hypothesis driven studies concerning the main effects, additive impact, and synergistic (i.e., interaction) effects of associations among sociocultural and psychosocial constructs and CVD risk factors and prevalence. Further, capitalizing on the large and diverse sample, analyses will examine variability in observed associations according to SES, Hispanic/Latino ethnic background, and acculturation (i.e., tests of effect moderation), and the degree to which intermediate psychosocial processes explain differences in risk and health profiles attributable to broad sociocultural factors (e.g., SES, nativity) (i.e., tests of indirect effects). Ultimately, the study aims to contribute to the understanding of the complex patterns and determinants of Hispanic/Latino health, to inform future prevention and intervention efforts that will capitalize on areas of resilience while reducing disproportionate risk.
Methods
Overview of the HCHS/SOL
Details concerning the HCHS/SOL have been presented previously.3,4 Briefly, the HCHS/SOL is an observational cohort study of 16,415 Hispanic/Latino persons aged 18-74 years, who were recruited from the Bronx, NY, Chicago, IL, Miami, FL, and San Diego, CA, using a two-stage probability sample of household addresses. The selected communities are in diverse regions of the US and represent 4 of the 10 largest Hispanic/Latino urban metropolitan areas. The sampling approach was designed to allow comparison of some of the largest US Hispanic/Latino background groups, including Mexican, Puerto Rican, Cuban, Dominican, Central American, and South American. However, all individuals who self-identified as being of “Hispanic” or “Latino” descent at the sampling stage, and who were Spanish and/or English speaking, were eligible. The 45-74 year age group was oversampled to allow accurate ascertainment of chronic disease rates. Participants underwent baseline examination (2008-2011) and at least 3 yearly telephone follow-up assessments to identify new CVD and pulmonary events or exacerbations, with adjudication via medical records. The baseline examination included comprehensive physiological, behavioral, and sociodemographic assessments, and limited assessment of sociocultural factors.3 A follow-up clinical exam is planned that will allow ascertainment of incident cardiovascular, metabolic, and other disease outcomes.
HCHS/SOL Sociocultural Ancillary Study
Design
The HCHS/SOL Sociocultural Ancillary Study is a cross-sectional cohort study15 of associations between sociocultural and psychosocial factors and prevalence of CVD and metabolic syndrome and its component risk factors. Using data from HCHS/SOL yearly telephone based follow-up assessments, and pending completion of a follow-up clinical visit, incident disease outcomes and risk factor progression will also be examined.
Participants and Recruitment
The target sample was 5,280 participants, distributed equally across the four field centers. The Sociocultural Ancillary Study began recruitment following the first wave of parent study enrollment. All participants who completed the parent study, consented to being contacted for future research, and were willing to attend a separate visit within 9 months were eligible. Bilingual study recruiters attempted to reach 7,321 HCHS/SOL participants; 6,246 (85.3%) were successfully contacted (1,075 could not be reached), and 5,313 (73% of targeted and 85% of screened participants) participated between February 2010 and June 2011. The majority of participants completed the Sociocultural Assessment within 6 months (88.3%) and most within 4 months (72.6%) of the baseline exam. Because HCHS/SOL sample households were randomly sampled to form three waves and years of recruitment, eligible participants were representative of the broader parent study.4 The Sociocultural Ancillary Study has at least one participant in 550 (82%) of the 670 block groups (i.e., statistical divisions of census tracts that typically contain 600 to 3,000 people) comprising the HCHS/SOL recruitment catchment area. The Sociocultural Ancillary Study sample can be considered a representative sub-sample of the HCHS/SOL parent study cohort, with the exception of lower participation in some higher SES strata. Table 1 displays sample characteristics in the target population overall and by field center. 3,278 participants (61.7%) in the Sociocultural Ancillary Study are 45-74 years old, which reflects the HCHS/SOL oversampling in this older age group. Most participants preferred being interviewed in Spanish (ranging from 65% in the Bronx to 93% in Miami). In the target population, 43.54% were 45 and older, 54.9% were women, 48.2% were married or cohabitating, and 66.2% had annual incomes below $30K. The Hispanic/Latino background distribution in the Sociocultural Ancillary Study was similar to that of the parent study target population.
Table 1. HCHS/SOL Sociocultural Ancillary Study Demographic Characteristics by Field Center and Overall.
| Characteristic* | Bronx (n=1342) |
Chicago (n=1329) |
Miami (n=1315) |
San Diego (n=1327) |
Overall (n=5313) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Age: 18-44 | 527 | 58.67 | 502 | 65.56 | 442 | 44.10 | 564 | 62.52 | 2035 | 56.46 |
| 45+ | 815 | 41.33 | 827 | 34.44 | 873 | 55.90 | 763 | 37.48 | 3278 | 43.54 |
| Gender: Male | 505 | 42.04 | 522 | 46.58 | 530 | 47.34 | 457 | 45.45 | 2014 | 45.15 |
| Female | 837 | 57.96 | 807 | 53.42 | 785 | 52.66 | 870 | 54.55 | 3299 | 54.85 |
| Hispanic/Latino Background: Dominican | 496 | 36.31 | 14 | 0.69 | 22 | 1.74 | 2 | 0.45 | 534 | 11.70 |
| Central American | 67 | 4.80 | 153 | 8.38 | 323 | 16.00 | 10 | 0.61 | 553 | 7.57 |
| Cuban | 16 | 1.05 | 8 | 0.90 | 745 | 67.33 | 6 | 0.96 | 775 | 20.32 |
| Mexican | 69 | 10.90 | 752 | 61.38 | 10 | 1.04 | 1249 | 93.39 | 2080 | 36.55 |
| Puerto Rican | 570 | 36.76 | 253 | 20.52 | 40 | 3.62 | 17 | 1.57 | 880 | 15.76 |
| South American | 67 | 4.33 | 116 | 5.88 | 149 | 7.97 | 18 | 0.94 | 350 | 4.79 |
| More than one | 56 | 5.86 | 32 | 2.26 | 24 | 2.30 | 25 | 2.08 | 137 | 3.31 |
| Marital Status: Single | 557 | 46.42 | 265 | 28.47 | 371 | 29.82 | 303 | 27.19 | 1496 | 33.98 |
| Married/with partner | 491 | 37.27 | 784 | 57.28 | 627 | 47.57 | 746 | 56.55 | 2648 | 48.21 |
| Separated/divorced | 230 | 12.19 | 218 | 11.99 | 268 | 19.04 | 219 | 13.54 | 935 | 14.49 |
| Widow(er) | 64 | 4.12 | 61 | 2.27 | 46 | 3.58 | 54 | 2.72 | 225 | 3.32 |
| Household yearly income: Less than $30K | 957 | 68.46 | 911 | 66.80 | 1004 | 75.30 | 768 | 52.51 | 3640 | 66.21 |
| $30K or more | 309 | 25.80 | 363 | 29.23 | 185 | 14.13 | 522 | 45.23 | 1379 | 27.79 |
| Missing | 76 | 5.74 | 55 | 3.97 | 126 | 10.57 | 37 | 2.26 | 294 | 6.00 |
| Educational attainment: Less than high school | 523 | 39.71 | 602 | 38.43 | 351 | 27.67 | 422 | 26.42 | 1898 | 32.69 |
| High school or greater | 792 | 60.29 | 701 | 61.57 | 939 | 72.33 | 876 | 73.56 | 3308 | 67.31 |
| Nativity: US Mainland | 343 | 28.78 | 203 | 24.30 | 46 | 4.52 | 325 | 32.40 | 917 | 21.91 |
| Other | 999 | 71.22 | 1125 | 75.70 | 1268 | 95.48 | 1001 | 67.60 | 4393 | 78.09 |
| Language of interview: Spanish | 872 | 58.93 | 1063 | 70.47 | 1249 | 93.31 | 1021 | 68.74 | 4205 | 73.21 |
| English | 468 | 41.07 | 266 | 29.53 | 66 | 6.69 | 302 | 31.26 | 1102 | 26.79 |
Statistics are: Unweighted count (N) and sample design weighted percent (%)
Procedures
Institutional Review Board approval was obtained from all study sites for all HCHS/SOL Sociocultural Ancillary Study procedures and materials, and all participants provided written informed consent. Participants attended a 1-2 hour interview, during which trained bilingual research assistants described the study, obtained written informed consent, and administered the assessments. Data were entered directly into a computer data management system, which maximized data accuracy. Participants who expressed significant distress or a desire for psychosocial services received a list of referrals for low or no-cost counseling. Safety protocols were in place to manage urgent scenarios (e.g., reported suicidal intent). Participants were compensated $60 for their time and effort.
Study staff members were centrally trained and certified by principal investigators and coordinating center personnel in all procedures. Study coordinators observed field center interviewers on at least two recruitment calls per month, and promptly corrected any protocol deviations. Assessment interviews were audiotaped and study coordinators reviewed at least one randomly selected tape per interviewer per month, to ensure protocol fidelity. An external review process was also implemented, with cross-center exchange of two randomly selected audiotapes per interviewer every two months. Data management reports were examined monthly to monitor recruitment progress and data quality.
Assessment Battery1
The battery was designed by investigators with considerable measurement expertise to assess all major constructs in the proposed conceptual model. Where possible, instruments available in both English and Spanish, and shown to be psychometrically sound and appropriate to Hispanics/Latinos in prior research, were used. Most constructs were represented by multiple indicators to provide a thorough approach and reliability of measurement, and to allow modeling of latent constructs. For measures not previously available in Spanish, bilingual HCHS/SOL staff and investigators translated the measures, using forward and back translation with reconciliation by committee composed of individuals from diverse Hispanic/Latino backgrounds, to ensure semantic and conceptual equivalence across Hispanic/Latino groups.16
Study Outcomes
Data from the parent study exam are used to ascertain CVD [coronary heart disease (CHD), stroke, other CVDs] prevalence, metabolic syndrome prevalence, and its component risk factors. Details concerning assessment of physiological factors and health history have been reported elsewhere.3 CHD was assessed through a combination of self-reported information (history of a cardiac event or procedure) and electrocardiographic evidence of myocardial infarction observed at baseline. The American Heart Association/NHLBI modified National Cholesterol Education Program criteria17 were used to determine presence of the metabolic syndrome. Additional analyses will examine major risk factors that underlie the metabolic syndrome and contribute to CVD, i.e., obesity, hypertension, diabetes, and dyslipidemia.18
Statistical Analyses
Logistic regression analyses will be used to identify unique predictors of CVD and metabolic syndrome prevalence and risk factors, as defined by Aim 1. For Aim 2, SEMs will test integrated models of associations among social, psychological, and cultural factors with CVD and the metabolic syndrome and its component risk factors, guided by the conceptual framework shown in Figure 1. First, exploratory and confirmative factor analysis will be applied to identify latent variables underlying major theoretical constructs (e.g., SES, stress, reserve capacity). Alternative models will be considered, since the boundaries between constructs are quite permeable. Multiple group analyses will be used to test invariance of the measurement models across Hispanic/Latino background groups.19 In evaluating the fit of all models, multiple indices will be examined (e.g., root mean square error of approximation, comparative fit index).20 Analyses will control for demographic variables (collected in the parent study baseline exam), including age, gender, Hispanic/Latino background group, and field center. Other demographic (e.g., nativity, language, SES) and health-related covariates (e.g., access to care, comorbidity) will be selected using theory-guided hypotheses and preliminary analyses. In some reports, demographic variables such as age, gender, nativity, and Hispanic/Latino background group will also be examined as potential effect modifiers (i.e., using interaction terms or in the context of multigroup SEMs).
To evaluate scale measurement properties (secondary aim), analyses will examine internal consistency (i.e., Chronbach's alpha) by language, and in each ethnic background group. Confirmatory factor analyses will be conducted to examine if the factor structure established in prior research is replicated in the current study, and multigroup models will test the structural invariance of scales across English and Spanish versions and Hispanic/Latino groups. Minor modifications may be made to scales to improve psychometric properties. If a scale is shown to lack adequate reliability and validity, the aims of the study will not be compromised given the latent construct approach and the use of multiple indicators for each major theoretical construct assessed.
Statistical Power
The study sought a sample size of 5280, or approximately 1/3 of the parent cohort, which provides adequate statistical power (at least 80%) to detect an association of small-moderate magnitude (OR = 1.25 to 1.50) for a relatively common outcome (e.g., 30% prevalence, such as metabolic syndrome or obesity), and to detect an effect of moderate magnitude (OR = 1.50) for a less frequent outcome (e.g., 5%, our pre-study estimate for CVD prevalence), assuming an alpha of .05 and covariates accounting for 25% of variance in a given outcome. The target sample size also ensures adequate power to identify overall model fit and tests of specific model parameters within planned SEMs.21
Discussion
The landmark HCHS/SOL will provide critical information regarding health risk and protective factors and patterns of CVD and other chronic diseases in the U.S. Hispanic/Latino population. The HCHS/SOL Sociocultural Ancillary Study will provide important complementary data regarding socioeconomic, cultural, and psychosocial factors that may serve as barriers or facilitators to optimal health among Hispanics/Latinos. The research is based in a conceptual model that will guide hypothesis testing for numerous studies. The approach addresses several important methodological and conceptual limitations of prior research, including a focus on a limited representation of the Hispanic/Latino population, or (alternatively) aggregation across diverse groups, the focus in the acculturation literature on proxy indicators, rather than examining the specific processes that may best explain patterns of health among Hispanics/Latinos, and a lack of theoretical grounding. The study examines CVD, a leading cause of death in Hispanics/Latinos, and related metabolic conditions that disproportionately affect this population. Because all ancillary study data are linked with the parent study, there is vast potential for future research examining associations of sociocultural and psychosocial factors with a range of endpoints, such as healthcare use patterns, lifestyle factors, and other health conditions.
Limitations of the parent HCHS/SOL and the Sociocultural Ancillary study include the focused sampling approach, and the fact that findings cannot be generalized to the entire Hispanic/Latino population. For example, growing Hispanic/Latino communities in rural areas were not included. A further limitation is that CVD and stroke prevalence—central outcomes in the Sociocultural Ancillary study—are primarily based on self-report. Other researchers have noted limitations of this approach, in terms of discrepancies relative to medical records information.22,23 Additional limitations specific to the HCHS/SOL Sociocultural Ancillary Study include data collection conducted within 9 months but not concurrent with the parent study examination. Adopting a relatively broad time window was important to allow an inclusive sample, since the Ancillary study commenced one year after the parent study; however, this may create interpretive difficulties in relation to some research questions. A more general limitation of the Sociocultural Ancillary Study is its cross-sectional design. Telephone follow-up assessments, and a second clinical exam planned for the parent study, will allow ascertainment of sociocultural influences in chronic disease incidence and risk factor progression over time.
Manuscripts documenting associations of sociocultural and psychosocial factors with CVD and metabolic syndrome prevalence and component risk factors will contribute to the limited existing knowledge base in diverse Hispanic/Latino groups across the U.S. Findings may also help guide future efforts aimed at improving health among Hispanics/Latinos, with potential contributions to understanding health and disease models in other ethnic minorities. Until recently, very limited empirical data has documented the contribution of multiple factors in health among Hispanics/Latinos in the U.S., particularly in a large sample that is diverse in regard to SES, background, nativity, and acculturation. Therefore, findings from the HCHS/SOL and the Sociocultural Ancillary Study may help shape policy aimed at augmenting prevention efforts in the largest ethnic minority group in the U.S.
Acknowledgments
The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements. The HCHS/SOL Sociocultural Ancillary Study was supported by grant 1 RC2 HL101649 (Gallo/Penedo) from the NIH/NHLBI. The authors thank the staff and participants of HCHS/SOL and the HCHS/SOL Sociocultural Ancillary Study for their important contributions.
Footnotes
A table detailing the major constructs assessed, measures, sources, and translation procedures is available from the first authors (LCG or FJP) upon request.
Contributor Information
Linda C. Gallo, Department of Psychology, San Diego State University
Frank J. Penedo, Department of Medical Social Sciences, Northwestern University.
Mercedes Carnethon, Department of Preventive Medicine, Northwestern University
Carmen Isasi, Department of Epidemiology and Population Health, Albert Einstein College of Medicine
Daniela Sotres-Alvarez, Department of Biostatistics, Collaborative Studies Coordinating Center, University of North Carolina at Chapel Hill
Vanessa L. Malcarne, Department of Psychology, San Diego State University
Scott C. Roesch, Department of Psychology, San Diego State University
Marston E. Youngblood, Department of Biostatistics, Collaborative Studies Coordinating Center, University of North Carolina at Chapel Hill
Martha L. Daviglus, Department of Preventive Medicine, Northwestern University, Department of Medicine, University of Illinois at Chicago
Patricia Gonzalez, Department of Psychology, San Diego State University
Gregory P. Talavera, Graduate School of Public Health, San Diego State University
References
- 1.Pew Hispanic Center. Census 2010: 50 Million Latinos. Washington, D.C.: Pew Hispanic Center; 2011. [Google Scholar]
- 2.Passel JS, Cohn DV. US Population Projections: 2005-2050. Washington D.C.: Pew Research Center; 2008. [Google Scholar]
- 3.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, et al. Design and Implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LaVange LM, Kalsbeek WD, Sorlie PD, et al. Sample Design and Cohort Selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69(7):983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: Do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 9.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 10.Grundy SM. Metabolic Syndrome: Connecting and Reconciling Cardiovascular and Diabetes Worlds. J Am Coll Cardiol. 2006;47(6):1093–1100. doi: 10.1016/j.jacc.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 11.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 12.Myers HF. Ethnicity- and socio-economic status-related stresses in context: An integrative conceptual model. J Behav Med. 2009;32(1):9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- 13.Escarce JJ, Morales LS, Rumbaut RG. The health status and health behaviors of Hispanics. In: Tienda M, Mitchell F, editors. Hispanics and the future of America. Washington, DC: National Academies Press; pp. 2006pp. 362–409. [PubMed] [Google Scholar]
- 14.Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59(5):973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Hudson JI, Pope HG, Jr, Glynn RJ. The cross-sectional cohort study: an underutilized design. Epidemiology. 2005;16(3):355–359. doi: 10.1097/01.ede.0000158224.50593.e3. [DOI] [PubMed] [Google Scholar]
- 16.Maneesriwongul W, Dixon JK. Instrument translation process: a methods review. J Adv Nurs. 2004;48(2):175–186. doi: 10.1111/j.1365-2648.2004.03185.x. [DOI] [PubMed] [Google Scholar]
- 17.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome - An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 18.Go AS, Mozaffarian D, Roger VL, et al. Heart Disease and Stroke Statistics' 2013 Update: A Report From the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ployhart RE, Oswald FL. Applications of mean and covariance structure analysis: Integrating correlational and experimental approaches. Organ Res Meth. 2004;7(1):27–65. [Google Scholar]
- 20.Bentler PM. On tests and indices for evaluating structural models. Pers Individ Dif. 2007;42(5):4. [Google Scholar]
- 21.Hancock GR. Power analysis in covariance structure models. In: Hancock GR, Mueller RO, editors. Structural Equation Modeling: A Second Course. Greenwood CT: Information Age Publishing; 2006. [Google Scholar]
- 22.Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of self-report, hospital discharge codes, and adjudication of cardiovascular events in the Women's Health Initiative. Am J Epidemiol. 2004;160(12):1152–1158. doi: 10.1093/aje/kwh314. [DOI] [PubMed] [Google Scholar]
- 23.Barr EL, Tonkin AM, Welborn TA, Shaw JE. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: the AusDiab study. Intern Med J. 2009;39(1):49–53. doi: 10.1111/j.1445-5994.2008.01864.x. [DOI] [PubMed] [Google Scholar]