Abstract
Purpose
To evaluate the financial experiences of a racially and ethnically diverse cohort of long-term breast cancer survivors (17% African American, 40% Latina) identified through population-based registries.
Methods
Longitudinal study of women diagnosed with nonmetastatic breast cancer in 2005 to 2007 and reported to the SEER registries of metropolitan Los Angeles and Detroit. We surveyed 3,133 women approximately 9 months after diagnosis and 4 years later. Multivariable models evaluated correlates of self-reported decline in financial status attributed to breast cancer and of experiencing at least one type of privation (economically motivated treatment nonadherence and broader hardships related to medical expenses).
Results
Among 1,502 patients responding to both surveys, median out-of-pocket expenses were ≤ $2,000; 17% of respondents reported spending > $5,000; 12% reported having medical debt 4 years postdiagnosis. Debt varied significantly by race: 9% of whites, 15% of blacks, 17% of English-speaking Latinas, and 10% of Spanish-speaking Latinas reported debt (P = .03). Overall, 25% of women experienced financial decline at least partly attributed to breast cancer; Spanish-speaking Latinas had significantly increased odds of this decline relative to whites (odds ratio [OR], 2.76; P = .006). At least one privation was experienced by 18% of the sample; blacks (OR, 2.6; P < .001) and English-speaking Latinas (OR, 2.2; P = .02) were significantly more likely to have experienced privation than whites.
Conclusion
Racial and ethnic minority patients appear most vulnerable to privations and financial decline attributable to breast cancer, even after adjustment for income, education, and employment. These findings should motivate efforts to control costs and ensure communication between patients and providers regarding financial distress, particularly for vulnerable subgroups.
INTRODUCTION
Considerable attention has focused on the financial burden of medical care,1,2 and experts have advocated for further research to investigate both the objective financial cost of cancer care and the subjective experiences of patients relating to these costs.3 Patients increasingly bear some of the cost of treatment through rising insurance premiums, deductibles, and copayments,4–6 and patients with cancer in particular have been shown to face higher out-of-pocket expenses than patients with other chronic conditions.7,8 Patients with cancer also face challenges in maintaining employment-related income to pay for these costs.9–12
Given the potential for both substantial expenses and challenges to maintaining income, patients with cancer may be particularly vulnerable to financial distress after diagnosis and treatment. Indeed, patients with cancer are more than twice as likely to file for bankruptcy as others,13 but less is known about how patients with cancer finance expenses or the privations they suffer as a result.14 In a population-based study of colon cancer survivors, 38% reported accruing debt, selling or refinancing their home, borrowing from friends or family, or experiencing ≥ 20% income decline.15 Further research is necessary to define the financial burden of care for other types of cancer and to identify which patients are most vulnerable.
We evaluated the financial experiences of a diverse cohort of breast cancer survivors identified through population-based registries and how they varied by race/ethnicity. We specifically investigated self-reported out-of-pocket medical expenses, how they financed these expenses, their perceptions of their financial status, and the privations they experienced in the currently challenging broader economic environment. We also described these breast cancer survivors' experiences with employment after diagnosis and treatment. Finally, we evaluated whether certain racial/ethnic subgroups of long-term breast cancer survivors were more vulnerable to financial distress.
METHODS
Study Sample
We conducted a longitudinal cohort study of women diagnosed with breast cancer in metropolitan Los Angeles and Detroit. Patients age 20 to 79 years diagnosed with stage 0 to III breast cancer between June 2005 and February 2007, as reported to the National Cancer Institute's SEER population-based program registries in those regions, were eligible for sample selection.
Patients were excluded if they had stage IV breast cancer or could not complete a questionnaire in English or Spanish. Asian women in Los Angeles were excluded because of enrollment in other studies. Latina (in Los Angeles) and black (in both Los Angeles and Detroit) patients were oversampled to ensure sufficient minority representation.
Questionnaire Design and Content
Questionnaires were based on existing literature, measures previously developed to assess relevant constructs, and theoretical models. For the items relating to financial experiences, we adapted questions previously utilized by the Consumer Bankruptcy Project16; for items relating to employment and insurance experiences, we adapted questions from surveys conducted by the Bureau of Labor Statistics in the general population, and items previously developed by labor economists for use in patients with cancer.17,18 We utilized standard techniques of content validation,19 including systematic review by design experts20–22 and pretesting with 40 patients in three waves, including 12 detailed cognitive interviews.23,24
Data Collection
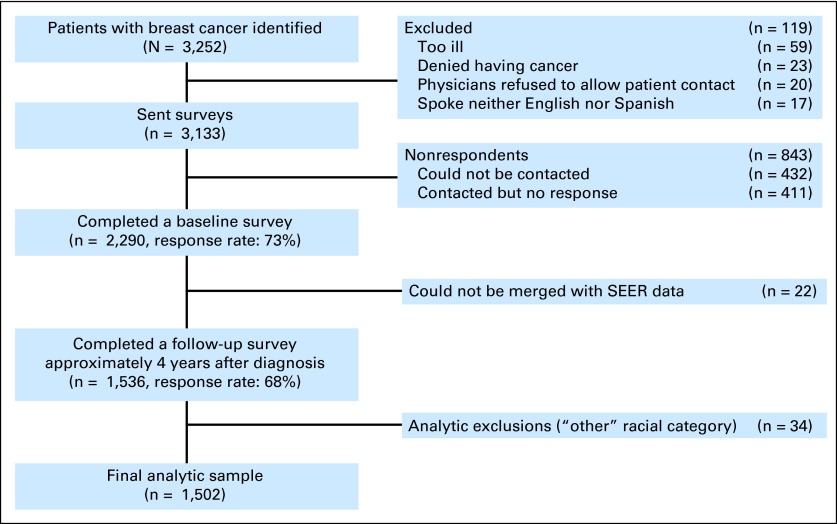
After institutional review board approval, patients were identified via rapid case ascertainment and surveyed a mean of 9 months after diagnosis, and again approximately 4 years later. To encourage response, we provided a $10 cash incentive and used a modified Dillman method.25 All materials were sent in English and Spanish to those with Spanish surnames.26 The response rate to the baseline survey was 73%, and the response rate to the follow-up survey was 68%. Survey responses were combined into a single data set, into which clinical data from SEER were merged. More details regarding the flow of patients into the sample are provided in Appendix Fig A1, online only.
Measures
We included several measures of financial impact in the follow-up survey. First, we measured patients' perceptions of whether, since diagnosis, they were worse off financially (financial decline). Among those perceiving financial decline, we asked whether this was due to breast cancer. We dichotomized responses for analysis (a little bit, somewhat, quite a bit, or very much versus not at all). Those who indicated they were worse off because of breast cancer (a little bit, somewhat, quite a bit, or very much) were considered to have had financial decline attributed at least partly to breast cancer.
We also asked how much the respondent paid in total for out-of-pocket medical expenses related to breast cancer, including copayments, hospital bills, and medication costs, with categorical response options. We then asked how they paid for out-of-pocket expenses and asked whether survivors currently had debt from their breast cancer treatments.
We evaluated privations related to breast cancer by using two sets of items in the follow-up survey. First, we evaluated economically motivated treatment nonadherence by asking whether in the past 12 months survivors had gone without medication, taken less than the fully prescribed amount of a medication, missed a doctor's appointment, or missed a mammogram because of cost. Second, we evaluated broader hardships related to the patient's medical expenses by asking whether, since breast cancer diagnosis, she or anyone in her household had gone without health insurance, had utilities turned off because of unpaid bills, or had to move out of their home because of the respondent's own personal medical expenses.
We also inquired regarding employment and insurance status in the follow-up survey, including whether, since diagnosis, women perceived they were worse off, and if so, if this was due to breast cancer. The follow-up survey inquired whether survivors had worked for pay since diagnosis. Among those who did, we asked how important it had been to avoid changing jobs because of worry about losing health insurance, to keep working to keep health insurance, or to get a new job in order to get health insurance (dichotomized for analysis as at least a little important versus not at all important). Among those working at any time since diagnosis, we asked whether they would look for a new job if they could be assured of comparable benefits, had increased work hours to cover breast cancer-related medical expenses, had decreased work hours because of breast cancer-related health issues, or been denied job opportunities because of breast cancer. We also assessed the extent to which the costs of prescription medications had been covered by health insurance in the past 12 months.
We defined four race/ethnic groups by using responses from the baseline survey: non-Hispanic whites, non-Hispanic blacks, English-speaking Latinas (ES-Latina), and Spanish-speaking Latinas (SS-Latina), using the Short Acculturation Scale for Hispanics to subdivide the latter two groups. Of note, the three participants who identified as both black and Latina were coded as Latina. We measured other pertinent sociodemographic factors in the baseline survey: age, education, employment status at diagnosis, marital status, and household income. Clinical factors measured in the baseline survey were comorbidity, chemotherapy receipt, radiotherapy receipt, and surgery. SEER records provided clinical stage, and the follow-up survey inquired about breast cancer recurrence.
Analytic Approach
To allow statistical inferences to represent the original targeted population, we applied complex survey weights to the calculation of percentages and regression analyses. Design weights compensated for the oversampling of minorities and disproportionate selection across SEER sites; nonresponse weights compensated for the fact that women with certain characteristics were not as likely to respond to the surveys at each time point, as described further in the Data Supplement. Analyses were conducted by using SAS (SAS/STAT User's Guide, Version 9.2; SAS Institute, Cary, NC).
We compared self-reported financial and employment experiences of survivors by race/ethnicity by using the χ2 test, limiting analysis to those who could be assigned to one of the four race/ethnic groups. We further constructed two adjusted logistic regression models to evaluate the correlates of decline in financial status attributed to breast cancer, as well as of having experienced at least one type of privation. Both models included the following theoretically selected independent variables: age, race/ethnicity, education, employment status at diagnosis, marital status, household income, comorbidity, stage, chemotherapy receipt, radiotherapy receipt, surgery, breast cancer recurrence, prescription drug coverage during survivorship, reduction in work hours during survivorship, and geographic site. Although missing data for most variables selected for model inclusion were less than 5%, income information was missing for 18.9%, so we employed multiple imputation for missing income data as described in the Data Supplement.
RESULTS
Of 3,133 women surveyed, 2,290 (73%) completed the baseline survey and 1,536 (68%) completed the follow-up, of whom 1,502 could be categorized for race/ethnicity. Table 1 reports the characteristics of these 1,502 patients. The sample was diverse, with 17% black and 40% Latina. A total of 52% had stage 0 to I disease, 62% received breast-conserving surgery, and 52% received chemotherapy.
Table 1.
Baseline Demographic and Clinical Characteristics of the Sample
| Characteristic | No. | Weighted % of Sample |
|---|---|---|
| Age at diagnosis, years | ||
| < 46 | 282 | 21.0 |
| 46-55 | 423 | 26.1 |
| 56-64 | 396 | 26.0 |
| 65+ | 401 | 26.8 |
| Comorbidity | ||
| 0 | 588 | 41.5 |
| 1 | 456 | 28.9 |
| 2 or more | 458 | 29.6 |
| Race | ||
| White | 728 | 42.7 |
| Black | 380 | 17.4 |
| English-speaking Latina | 191 | 19.5 |
| Spanish-speaking Latina | 203 | 20.4 |
| Education | ||
| High school or less | 557 | 42.1 |
| Some college | 510 | 31.5 |
| College graduate or greater | 411 | 24.4 |
| Missing | 24 | 2.0 |
| Family income at baseline survey | ||
| < $50,000 | 637 | 44.0 |
| $50,000+ | 600 | 36.1 |
| Missing or do not know | 265 | 19.8 |
| Marital status | ||
| Not married or partnered | 635 | 42.0 |
| Married or partnered | 849 | 56.6 |
| Missing | 18 | 1.4 |
| Stage | ||
| 0 | 370 | 18.1 |
| I | 540 | 34.2 |
| II | 416 | 32.5 |
| III | 140 | 11.8 |
| Missing | 36 | 3.2 |
| Chemotherapy receipt | ||
| No | 758 | 45.4 |
| Yes | 691 | 52.4 |
| Missing | 53 | 2.2 |
| Surgery type | ||
| Breast conservation | 994 | 62.4 |
| Mastectomy without reconstruction | 269 | 21.4 |
| Mastectomy with reconstruction | 233 | 18.2 |
| Radiation receipt | ||
| No | 410 | 31.1 |
| Yes | 1,040 | 66.5 |
| Missing | 52 | 2.5 |
| Work status at diagnosis | ||
| Full time | 651 | 42.4 |
| Part time | 196 | 13.1 |
| Not working | 643 | 43.3 |
| Missing | 12 | 1.2 |
| Geographic site | ||
| Los Angeles | 829 | 79.3 |
| Detroit | 671 | 20.7 |
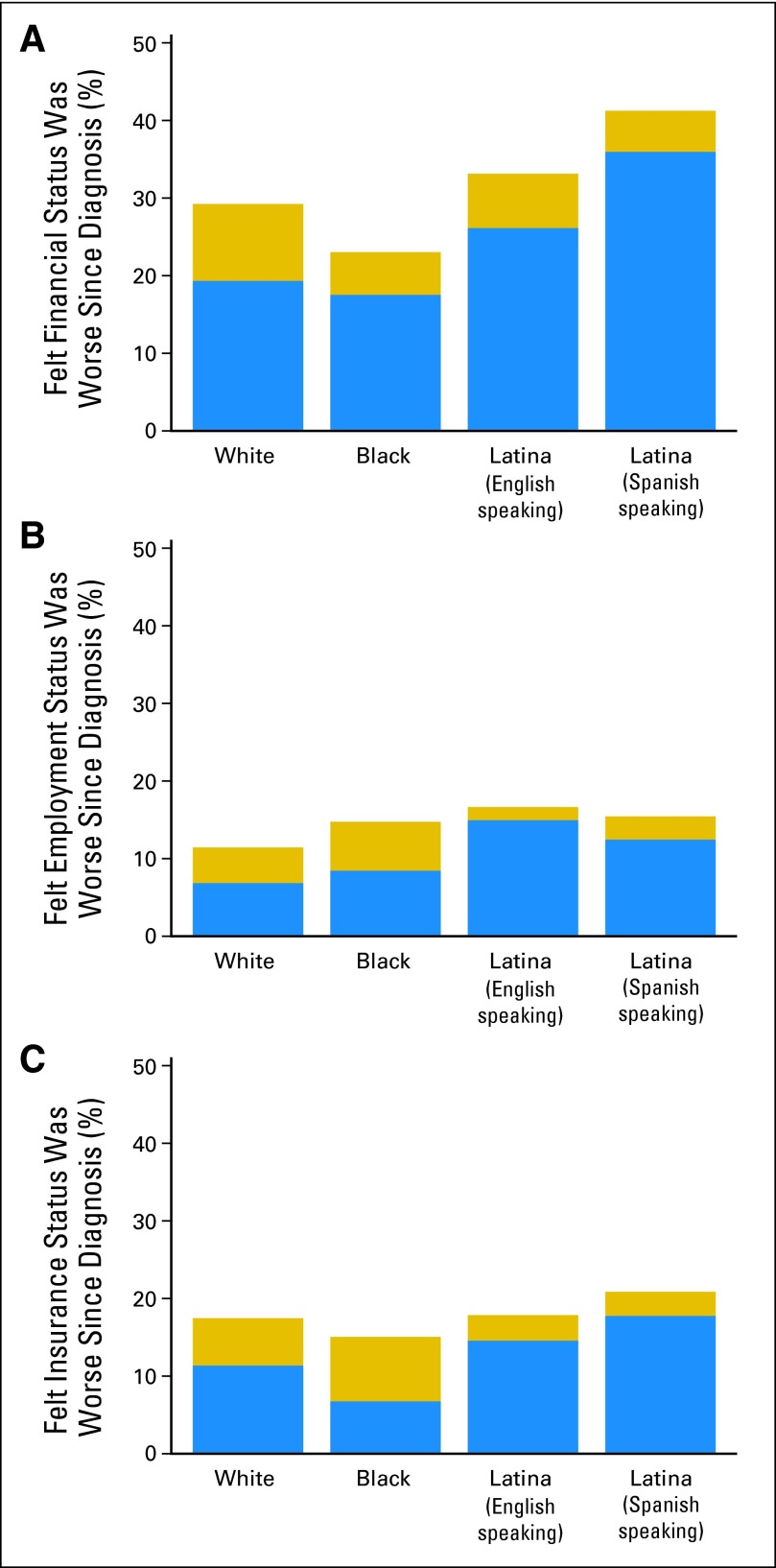
Overall, 33% of respondents reported decline in financial status since diagnosis. Of those, 77% felt this was at least partly because of breast cancer (for a total of 25% reporting decline attributed at least partly to breast cancer). As Figure 1A depicts, both the proportion reporting decline in financial status (P < .001) and the proportion of those who attributed this to breast cancer (P < .001) varied significantly by race/ethnicity. Table 2 presents a multivariable logistic regression model, in which SS-Latinas had significantly increased odds of financial decline attributed to breast cancer, as did those with age younger than 65, household income < $50,000 at diagnosis, part-time employment at diagnosis, reduction in work hours, lack of substantial prescription drug coverage, breast cancer recurrence, and chemotherapy receipt.
Fig 1.
Each bar depicts the percent of respondents who reported being worse off since diagnosis; the blue portion indicates those who attributed this at least partly to breast cancer. (A) The overall proportion of patients reporting decline in financial status varied significantly by race/ethnicity (P < .001), as did the proportion attributing decline at least partly to breast cancer (P < .001). (B) The overall proportion reporting decline in employment status did not vary by race/ethnicity (P = .23), but the proportion of those attributing the decline at least partly to breast cancer did (P = .005). (C) The overall proportion reporting decline in insurance status did not vary by race/ethnicity (P = .52), but the proportion of those attributing it at least partly to breast cancer did (P = .006).
Table 2.
Multivariable Model of Reporting Decline in Financial Status Attributed at Least Partly to Breast Cancer
| Covariate | Worsening Financial Status at Least Partly Due to Breast Cancer (N = 1,244) |
||
|---|---|---|---|
| OR | 95% CI | P | |
| Site | |||
| Los Angeles (reference) | 1.00 | ||
| Detroit | 1.07 | 0.72 to 1.61 | .732 |
| Age at diagnosis, years | |||
| < 46 | 3.99 | 1.98 to 8.07 | < .001 |
| 46-55 | 3.25 | 1.68 to 6.28 | < .001 |
| 56-64 | 2.96 | 1.63 to 5.37 | < .001 |
| 65+ | 1.00 | ||
| Race | |||
| White (reference) | 1.00 | ||
| Black | 0.87 | 0.52 to 1.44 | .587 |
| Latina, English-speaking | 1.45 | 0.83 to 2.53 | .190 |
| Latina, Spanish-speaking | 2.76 | 1.33 to 5.72 | .006 |
| Education | |||
| College graduate or greater | 0.77 | 0.47 to 1.26 | .300 |
| Some college/technical school (reference) | 1.00 | ||
| High school graduate | 0.81 | 0.48 to 1.38 | .443 |
| Less than high school | 0.67 | 0.34 to 1.33 | .255 |
| Marital status | |||
| Married/partnered (reference) | 1.00 | ||
| Not married | 1.25 | 0.82 to 1.90 | .303 |
| Household income | |||
| $50,000+ (reference) | 1.00 | ||
| < $50,000 | 1.77 | 1.04 to 3.00 | .034 |
| Working at diagnosis | |||
| Not working (reference) | 1.00 | ||
| Part time | 1.88 | 1.11 to 3.19 | .019 |
| Full time | 1.11 | 0.70 to 1.75 | .663 |
| Reduction in work hours | |||
| No (reference) | 1.00 | ||
| Yes | 1.68 | 1.02 to 2.78 | .042 |
| Prescriptions covered by health insurance | |||
| Completely (reference) | 1.00 | ||
| Mostly | 1.09 | 0.64 to 1.85 | .746 |
| Partially | 3.67 | 2.09 to 6.45 | < .001 |
| Not covered | 2.70 | 1.27 to 5.73 | .010 |
| Comorbidities | |||
| 0 (reference) | 1.00 | ||
| 1+ | 0.84 | 0.56 to 1.25 | .386 |
| Stage of disease | |||
| 3 | 1.92 | 0.98 to 3.76 | .058 |
| 2 | 1.34 | 0.84 to 2.14 | .216 |
| 1 (reference) | 1.00 | ||
| 0 | 1.05 | 0.61 to 1.80 | .869 |
| Surgery | |||
| Lumpectomy (reference) | 1.00 | ||
| Mastectomy without reconstruction | 0.62 | 0.33 to 1.17 | .140 |
| Mastectomy with reconstruction | 1.00 | 0.53 to 1.87 | .995 |
| Chemotherapy | |||
| No (reference) | 1.00 | ||
| Yes | 2.14 | 1.32 to 3.47 | .002 |
| Radiotherapy | |||
| No | 1.01 | 0.58 to 1.77 | .961 |
| Yes (reference) | 1.00 | ||
| Recurrent breast cancer | |||
| No (reference) | 1.00 | ||
| Yes | 2.44 | 1.17 to 5.06 | .017 |
Abbreviation: OR, odds ratio.
As shown in Table 3, the median out-of-pocket spending for breast cancer medical expenses was ≤ $2,000; 17% of respondents spent > $5,000. A much lower proportion of SS-Latinas (57%) reported being able to rely on income or savings than other groups (P < .001). ES-Latinas were considerably more likely than other groups to increase credit-card debt to finance their medical expenses (P = .03). Blacks were more likely to report leaving medical bills unpaid (P < .001). Minority respondents were more likely to borrow from family or friends than whites (P = .04).
Table 3.
Financial Experiences Reported by Breast Cancer Survivors
| Total (%) | Spanish-Speaking Latinas (%) | English-Speaking Latinas (%) | Blacks (%) | Whites (%) | P* | |
|---|---|---|---|---|---|---|
| Out-of-pocket spending† | ||||||
| < $500 | 40 | 64 | 42 | 47 | 25 | < .001 |
| $500-$2,000 | 25 | 20 | 20 | 30 | 28 | |
| $2,001-$5,000 | 18 | 7 | 17 | 16 | 24 | |
| $5,001-$10,000 | 10 | 6 | 12 | 4 | 14 | |
| > $10,000 | 7 | 4 | 10 | 3 | 9 | |
| Financing of medical expenses | ||||||
| Used income and/or savings | 80 | 57 | 79 | 81 | 90 | < .001 |
| Borrowed from family or friends | 7 | 10 | 8 | 9 | 4 | .04 |
| Borrowed against house | 2 | 0 | 2 | 2 | 2 | .41 |
| Left some medical bills unpaid | 5 | 3 | 5 | 14 | 3 | < .001 |
| Increased credit card debt | 10 | 6 | 15 | 8 | 10 | .03 |
| Debt | ||||||
| Reporting debt from breast cancer treatment | 12 | 10 | 17 | 15 | 9 | .03 |
| Privations | ||||||
| In past 12 months, because of cost, reported | ||||||
| Going without medication | 5 | 6 | 7 | 6 | 4 | .08 |
| Taking less than fully prescribed amount | 4 | 4 | 4 | 6 | 3 | .01 |
| Missing doctor's appointment | 8 | 6 | 10 | 11 | 6 | .02 |
| Since diagnosis, because of personal medical expenses, reported | ||||||
| Going without health insurance | 6 | 8 | 9 | 8 | 2 | < .001 |
| Having utilities turned off because of unpaid bills | 5 | 5 | 4 | 11 | 2 | < .001 |
| Having to move out of home because could not afford to stay | 4 | 5 | 6 | 6 | 2 | < .001 |
P values on the basis of comparison across the four race/ethnic groups by using the weighted χ2 test statistic.
Totals do not sum to 100% because of rounding.
Twelve percent of respondents reported that they had medical debt 4 years postdiagnosis. Debt varied significantly by race/ethnicity, with 9% of whites, 15% of blacks, 17% of ES-Latinas, and 10% of SS-Latinas reporting debt (P = .03). As also reported in Table 3, minority respondents were more likely to report foregoing medical care because of cost and other privations because of their medical expenses. At least one privation was experienced by 18% of the sample and, on multivariable analysis, blacks and ES-Latinas were significantly more likely to have experienced at least one privation than whites (Table 4). Other correlates of at least one privation were Detroit location, middle age (46 to 64) compared with younger (≤ 45) or older (≥ 65) age, household income < $50,000, reduction in work hours, and lack of substantial prescription drug coverage.
Table 4.
Multivariable Model of Reporting at Least One Major Privation Because of Medical Expenses
| Covariate | Privations (N = 1,298) |
||
|---|---|---|---|
| OR | 95% CI | P | |
| Site | |||
| Los Angeles (reference) | 1.00 | ||
| Detroit | 1.59 | 1.03 to 2.45 | .035 |
| Age at diagnosis, years | |||
| < 46 | 0.94 | 0.91 to 0.96 | < .001 |
| 46-55 | 3.40 | 1.63 to 7.12 | .001 |
| 56-64 | 1.88 | 0.97 to 3.61 | .060 |
| 65+ | 1.00 | ||
| Race | |||
| White (reference) | 1.00 | ||
| Black | 2.62 | 1.58 to 4.33 | < .001 |
| Latino, English speaking | 2.17 | 1.15 to 4.09 | .017 |
| Latino, Spanish speaking | 1.30 | 0.53 to 3.18 | .559 |
| Education | |||
| College graduate or greater | 0.75 | 0.43 to 1.30 | .298 |
| Some college/technical school (reference) | 1.00 | ||
| High school graduate | 1.18 | 0.68 to 2.06 | .557 |
| Less than high school | 1.53 | 0.76 to 3.05 | .231 |
| Marital status | |||
| Married/partnered (reference) | 1.00 | ||
| Not married | 1.01 | 0.66 to 1.56 | .960 |
| Household income | |||
| $50,000+ (reference) | 1.00 | ||
| < $50,000 | 2.05 | 1.16 to 3.60 | .013 |
| Working at diagnosis | |||
| Not working (reference) | 1.00 | ||
| Part time | 1.25 | 0.66 to 2.38 | .489 |
| Full time | 1.13 | 0.68 to 1.86 | .646 |
| Reduction in work hours | |||
| No (reference) | 1.00 | ||
| Yes | 2.00 | 1.20 to 3.33 | .008 |
| Prescription covered by health insurance | |||
| Completely (reference) | 1.00 | ||
| Mostly | 1.57 | 0.84 to 2.91 | .155 |
| Partially | 4.16 | 2.17 to 7.99 | < .001 |
| Not covered | 12.04 | 5.38 to 26.94 | < .001 |
| Comorbidities | |||
| 0 (reference) | 1.00 | ||
| 1+ | 1.05 | 0.67 to 1.63 | .840 |
| Stage of disease | |||
| 3 | 1.23 | 0.55 to 2.76 | .608 |
| 2 | 0.97 | 0.58 to 1.61 | .894 |
| 1 (reference) | 1.00 | ||
| 0 | 1.14 | 0.66 to 1.99 | .639 |
| Surgery | |||
| Lumpectomy (reference) | 1.00 | ||
| Mastectomy without reconstruction | 0.66 | 0.32 to 1.37 | .263 |
| Mastectomy with reconstruction | 0.94 | 0.47 to 1.91 | .874 |
| Chemotherapy | |||
| No (reference) | 1.00 | ||
| Yes | 1.54 | 0.89 to 2.66 | .119 |
| Radiotherapy | |||
| No | 1.35 | 0.69 to 2.65 | .375 |
| Yes (reference) | 1.00 | ||
| Recurrent breast cancer | |||
| No (reference) | 1.00 | ||
| Yes | 1.74 | 0.77 to 3.91 | .183 |
Abbreviation: OR, odds ratio.
Overall, 15% of the 1,502 respondents reported decline in employment status since diagnosis, and 72% of these attributed the decline to breast cancer. As depicted in Figure 1B, the overall proportion reporting decline in employment status did not vary by race/ethnicity (P = .23), but the proportion of those attributing the decline at least partly to breast cancer did (P = .005). Eighteen percent reported that their health insurance status was worse since diagnosis, and of those, 73% felt this was at least somewhat because of breast cancer. As depicted in Figure 1C, the overall proportion reporting that their insurance status was worse did not vary by race/ethnicity (P = .52), but the proportion of those attributing being worse off at least partly to breast cancer did (P = .006).
Of the respondents, 741 reported that they worked for pay at some time after diagnosis. As detailed in Table 5, in this subgroup, 60% reported that it was at least a little important to work to keep health insurance, 53% to avoid changing jobs because of worry about losing health insurance, and 27% to get a new job in order to get health insurance. Of note, 25% of this subgroup reported that they would look for a new job if they could be assured of comparable benefits (48% of SS-Latinas, 30% ES-Latinas, 24% blacks, and 18% whites; P < .001). Of those who worked at some time after diagnosis, 7% had increased work hours to cover cancer-related expenses, 27% had decreased work hours because of cancer-related health issues, and 7% believed they had been denied job opportunities because of cancer.
Table 5.
Employment Experiences Reported by Breast Cancer Survivors Who Worked for Pay at Some Time Since Diagnosis (n = 741)
| Total (%) | Spanish-Speaking Latinas (%) | English-Speaking Latinas (%) | Blacks (%) | Whites (%) | P* | |
|---|---|---|---|---|---|---|
| Reporting at least a little important to … | ||||||
| Keep working in order to keep health insurance | 60 | 64 | 68 | 70 | 53 | .04 |
| Avoid changing jobs because of worry about losing health insurance | 53 | 65 | 59 | 59 | 47 | .07 |
| Get a new job to get health insurance | 27 | 54 | 32 | 36 | 16 | < .001 |
| Reporting … | ||||||
| Would look for a new job if could be assured of comparable benefits | 25 | 48 | 30 | 24 | 18 | < .001 |
| Having to increase work hours to cover breast cancer–related medical expenses | 7 | 13 | 9 | 2 | 6 | .053 |
| Having to decrease work hours because of breast cancer–related health issues | 27 | 35 | 33 | 22 | 25 | .16 |
| Being denied job opportunities because of breast cancer | 7 | 7 | 9 | 5 | 7 | .76 |
DISCUSSION
In this sample of long-term breast cancer survivors from two metropolitan areas, one quarter perceived being worse off financially as a result of their breast cancer. Even 4 years after diagnosis, 12% reported having medical debt. Patients reported both economically motivated treatment nonadherence and more general privations related to their medical expenses. Minority patients were most vulnerable to privations and financial decline attributed to breast cancer, even after adjustment for income, education, and employment. To our knowledge, this is the first study to report individual financial experiences in a racially and ethnically diverse sample of patients with breast cancer drawn from population-based registries.
Previous studies have suggested that patients with cancer face substantial financial burden from treatment. Analysis of Medical Expenditure Panel Survey data from 2001 to 2008 suggested that 13.4% of patients with cancer spent > 20% of income on out-of-pocket health care expenses, including insurance premiums. This burden may translate into significant privations. In a national survey of 930 patients with cancer, 11% reported inability to pay for food, heat, or housing because of the costs of cancer treatment.27 National Health Interview Survey data from 2003 to 2006 suggested that 7.8% of cancer survivors reported forgoing medical care because of cost, although it could not define whether survivors were forgoing cancer care or elective services.28 Financial stress has also been shown to compromise the quality of life in patients with cancer.29
We are aware of only one other survey of patients identified through a population-based registry on this subject.15 That study focused on colon cancer survivors treated with curative intent, closer to their initial treatment than the long-term breast cancer survivors in the current study. That study also revealed that patients with younger age, minority race, and lower annual household income were more likely to report treatment-related financial hardship. Together, these studies suggest that there is an identifiable subgroup of patients with cancer who are particularly vulnerable to financial distress.
Several studies were conducted to evaluate the out-of-pocket expenses of patients with breast cancer treated one to two decades ago.6,30,31 These older studies estimated the monthly out-of-pocket costs for medical expenses incurred by women during chemotherapy to be between $300 and $1,180 per month, and approximately $500 per month by 1 year after diagnosis.32 The findings of the current study reveal that median total out-of-pocket spending on breast cancer expenses 4 years postdiagnosis was < $2,000, consistent with a study that revealed that from 1987 to 2001 through 2005, the proportion of cancer costs funded by private insurance increased and the out-of-pocket share decreased.33 Nevertheless, a substantial minority reported worsening of financial status, and certain subgroups—including those of minority race or ethnicity—appeared particularly vulnerable.
Previous studies have also raised concerns about the effects of cancer on employment, including reduction of income and loss of employment-based insurance, which can in turn adversely affect financial status.34 We found that many survivors reported ways in which cancer influenced their subsequent employment experiences and decisions; concerns about maintaining insurance and benefits were particularly common.
This study has strengths that include its identification of a diverse sample of patients treated in multiple settings through population-based registries, its longitudinal design, and its detailed measures of financial status and burden derived from the broader literature on financial distress. However, a limitation of our study was that we did not compare the experiences of patients in our sample to noncancer control patients. Although we asked patients whether they believed that decline in financial status and privations were attributable to their breast cancer, it is possible that these attributions are inaccurate. Also, as in any survey study, bias may have been introduced by nonresponse. Although the response rate to each of our surveys was high compared with other survey studies of patients with cancer,35 there was attrition in the sample at each step in the longitudinal evaluation, and it is possible that respondents differed meaningfully from those who did not respond. To minimize the impact of nonresponse bias, we employed complex survey weights. Finally, the study was located in two large metropolitan areas, which may limit the generalizability of the findings, particularly to more rural areas and those in which access to Medicaid differs from that in California and Michigan at the time of the study.
Despite these limitations, our findings suggest that a substantial proportion of breast cancer survivors perceive a negative financial impact from diagnosis and treatment, and they experience a variety of privations. Racial and ethnic minorities appeared more vulnerable than whites. Unfortunately, communication between patients and physicians regarding financial concerns is suboptimal.36–41 The current findings should motivate increased efforts to ensure communication between patients and providers regarding the financial implications of cancer diagnosis and treatment decisions. Further research should consider how changes since the time of our study, including the availability of lower-cost generic equivalents for commonly prescribed endocrine therapies, impending changes in Medicaid eligibility mandated by the Affordable Care Act, and the creation of a federal Consumer Financial Protection Bureau to regulate consumer credit more tightly, may have modified the experiences of patients currently being diagnosed, as compared with those reported by the patients in our study. Additional research is also important to further define the long-term financial experiences of patients with other types of cancer, whose experiences may differ from those in our sample for various reasons (including differences in treatments, prognosis, and insurance eligibility), as well as the predictors for vulnerability to financial decline and privations in those settings, to allow for the rational targeting of interventions and support.
Although we are deservedly proud of advances in our ability to cure an increasing proportion of patients diagnosed with breast cancer, we must ensure that we do not leave them in financial ruin as a result of our efforts. Providers, researchers, and policymakers alike must make dedicated efforts to reduce the cost of medical care in order to help prevent the lasting deleterious impact on the financial well-being of patients of the sort observed in this study.
Supplementary Material
Acknowledgment
We thank our project staff: Barbara Salem, MS, MSW, and Ashley Gay, BA (University of Michigan); Ain Boone, BA, Cathey Boyer, MSA, and Deborah Wilson, BA (Wayne State University); and Alma Acosta, Mary Lo, MS, Norma Caldera, Marlene Caldera, and Maria Isabel Gaeta (University of Southern California). All of these individuals received compensation for their assistance. We thank the American College of Surgeons Commission on Cancer (David Winchester, MD, and Connie Bura) and the National Cancer Institute Outcomes Branch (Neeraj Arora, PhD, and Steven Clauser, PhD) for their support. We acknowledge with gratitude the patients with breast cancer who responded to our survey.
Appendix
Fig A1.
This figure depicts the evolution of the analytic sample of women diagnosed with breast cancer in metropolitan Los Angeles and Detroit. Cases were initially selected on the basis of rapid case ascertainment, which lacks the level of quality control that is ultimately used to determine inclusion in the SEER registry. Certain cases that were initially identified and surveyed were ultimately excluded from SEER because they were no longer considered to be reportable cases after quality control; as shown above, 22 cases could not be merged to SEER and were therefore excluded from the sample.
Support information appears at the end of this article.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Support
Supported by Grants No. R01 CA109696 and R01 CA088370 from the National Cancer Institute (NCI) to the University of Michigan. R.J. was supported by a Mentored Research Scholar Grant No. MRSG-09-145-01 from the American Cancer Society. S.J.K. was supported by an Established Investigator Award in Cancer Prevention, Control, Behavioral, and Population Sciences Research from the NCI (Award No. K05CA111340). The collection of Los Angeles County cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the NCI's SEER program under Contract No. N01-PC-35139 awarded to the University of Southern California, Contract No. N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under Agreement No. 1U58DP00807-01 awarded to the Public Health Institute. The collection of metropolitan Detroit cancer incidence data was supported by the NCI SEER program Contract No. N01-PC-35145.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Reshma Jagsi, John A.E. Pottow, Steven J. Katz, Sarah T. Hawley
Financial support: Steven J. Katz, Sarah T. Hawley
Administrative support: Steven J. Katz, Sarah T. Hawley
Provision of study materials or patients: Ann S. Hamilton, John Graff
Collection and assembly of data: Ann S. Hamilton, John Graff, Steven J. Katz, Sarah T. Hawley
Data analysis and interpretation: Reshma Jagsi, John A.E. Pottow, Kent A. Griffith, Cathy Bradley, Steven J. Katz, Sarah T. Hawley
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Bach PB, Saltz LB, Wittes RE. The New York Times; 2012. Oct 14, In cancer care, cost matters; p. A25. http://www.nytimes.com/2012/10/15/opinion/a-hospital-says-no-to-an-11000-a-month-cancer-drug.html?_r=0. [Google Scholar]
- 2.Moriates C, Shah NT, Arora VM. First, do no (financial) harm. JAMA. 2013;310:577–578. doi: 10.1001/jama.2013.7516. [DOI] [PubMed] [Google Scholar]
- 3.Zafar SY, Abernethy AP. Financial toxicity, Part I: A new name for a growing problem. Oncology (Williston Park) 2013;27:80–81. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaiser Family Foundation and Health Research & Trust. Employer health benefits, 2013 annual survey. http://ehbs.kff.org/pdf/2011/8225.pdf.
- 5.Howard DH, Molinari NA, Thorpe KE. National estimates of medical costs incurred by nonelderly cancer patients. Cancer. 2004;100:883–891. doi: 10.1002/cncr.20063. [DOI] [PubMed] [Google Scholar]
- 6.Arozullah AM, Calhoun EA, Wolf M, et al. The financial burden of cancer: Estimates from a study of insured women with breast cancer. J Support Oncol. 2004;2:271–278. [PubMed] [Google Scholar]
- 7.Bernard DS, Farr SL, Fang Z. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol. 2011;29:2821–2826. doi: 10.1200/JCO.2010.33.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langa KM, Fendrick AM, Chernew ME, et al. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health. 2004;7:186–194. doi: 10.1111/j.1524-4733.2004.72334.x. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Tangka FK, Trogdon JG, et al. The personal financial burden of cancer for the working-aged population. Am J Manag Care. 2009;15:801–806. [PubMed] [Google Scholar]
- 10.de Boer AG, Taskila T, Ojajärvi A, et al. Cancer survivors and unemployment: A meta-analysis and meta-regression. JAMA. 2009;301:753–762. doi: 10.1001/jama.2009.187. [DOI] [PubMed] [Google Scholar]
- 11.Mujahid MS, Janz NK, Hawley ST, et al. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat. 2010;119:213–220. doi: 10.1007/s10549-009-0389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mujahid MS, Janz NK, Hawley ST, et al. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv. 2011;5:102–111. doi: 10.1007/s11764-010-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 2013;32:1143–1152. doi: 10.1377/hlthaff.2012.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient's experience. Oncologist. 2013;18:381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shankaran V, Jolly S, Blough D, et al. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: A population-based exploratory analysis. J Clin Oncol. 2012;30:1608–1614. doi: 10.1200/JCO.2011.37.9511. [DOI] [PubMed] [Google Scholar]
- 16.Lawless RM, Littwin AK, Porter KM, et al. Did bankruptcy reform fail? An empirical study of consumer debtors. Am Bankruptcy Law J. 2008;82:349–406. [Google Scholar]
- 17.Bradley CJ, Neumark D, Luo Z, et al. Employment-based health insurance, illness, and labor supply of women: Evidence from married women with breast cancer. Health Econ. 2006;16:719–737. doi: 10.1002/hec.1191. [DOI] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics, US Census Bureau. Technical Paper 63RV Design and Methodology. 2002. http://www.census.gov/prod/2002pubs/tp63rv.pdf.
- 19.Fowler FJ. Improving Survey Questions: Design and Evaluation (Applied Social Research Methods) Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 20.Katz SJ, Lantz PM, Paredes Y, et al. Breast cancer treatment experiences of Latinas in Los Angeles county. Am J Public Health. 2005;95:2225–2230. doi: 10.2105/AJPH.2004.057950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hawley ST, Griggs JJ, Hamilton AS, et al. Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. J Natl Cancer Inst. 2009;101:1337–1347. doi: 10.1093/jnci/djp271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zikmund-Fisher BJ, Smith DM, Ubel PA, et al. Validation of the Subjective Numeracy Scale: Effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27:663–671. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]
- 23.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
- 24.Mauceri S. Cognitive interviewing: A tool for improving questionnaire design. Int J Soc Res Methodol. 2008;11:79–83. [Google Scholar]
- 25.Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. ed 3. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 26.Hamilton AS, Hofer TP, Hawley ST, et al. Latinas and breast cancer outcomes: Population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidemiol Biomarkers Prev. 2009;18:2022–2029. doi: 10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The USA Today/Kaiser Family Foundation/Harvard School of Public Health: National survey of households affected by cancer. 2006. Nov, http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7591.pdf.
- 28.Weaver KE, Rowland JH, Bellizzi KM, et al. Forgoing medical care because of cost: Assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116:3493–3504. doi: 10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ell K, Xie B, Wells A, et al. Economic stress among low-income women with cancer: Effects on quality of life. Cancer. 2008;112:616–625. doi: 10.1002/cncr.23203. [DOI] [PubMed] [Google Scholar]
- 30.Moore KA. Breast cancer patients' out-of-pocket expenses. Cancer Nurs. 1999;22:389–396. doi: 10.1097/00002820-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Given BA, Given CW, Stommel M. Family and out-of-pocket costs for women with breast cancer. Cancer Pract. 1994;2:187–193. [PubMed] [Google Scholar]
- 32.Pisu M, Azuero A, McNees P, et al. The out of pocket cost of breast cancer survivors: A review. J Cancer Surviv. 2010;4:202–209. doi: 10.1007/s11764-010-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tangka FK, Trogdon JG, Richardson LC, et al. Cancer treatment cost in the United States: Has the burden shifted over time? Cancer. 2010;116:3477–3484. doi: 10.1002/cncr.25150. [DOI] [PubMed] [Google Scholar]
- 34.Lauzier S, Maunsell E, Drolet M, et al. Wage losses in the year after breast cancer: Extent and determinants among Canadian women. J Natl Cancer Inst. 2008;100:321–332. doi: 10.1093/jnci/djn028. [DOI] [PubMed] [Google Scholar]
- 35.Kelly BJ, Fraze TK, Hornik RC. Response rates to a mailed survey of a representative sample of cancer patients randomly drawn from the Pennsylvania Cancer Registry: A randomized trial of incentive and length effects. BMC Med Res Methodol. 2010;10:65. doi: 10.1186/1471-2288-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Neumann PJ, Palmer JA, Nadler E, et al. Cancer therapy costs influence treatment: A national survey of oncologists. Health Aff (Millwood) 2010;29:196–202. doi: 10.1377/hlthaff.2009.0077. [DOI] [PubMed] [Google Scholar]
- 37.Alexander GC, Casalino LP, Tseng CW, et al. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19:856–860. doi: 10.1111/j.1525-1497.2004.30249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schrag D, Hanger M. Medical oncologists' views on communicating with patients about chemotherapy costs: A pilot survey. J Clin Oncol. 2007;25:233–237. doi: 10.1200/JCO.2006.09.2437. [DOI] [PubMed] [Google Scholar]
- 39.Kim P. Cost of cancer care: The patient perspective. J Clin Oncol. 2007;25:228–232. doi: 10.1200/JCO.2006.07.9111. [DOI] [PubMed] [Google Scholar]
- 40.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: The cost of cancer care. J Clin Oncol. 2009;27:3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 41.Weinfurt KP. Value of high-cost cancer care: A behavioral science perspective. J Clin Oncol. 2007;25:223–227. doi: 10.1200/JCO.2006.08.9029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.