Abstract
The use of the 70° arthroscope in knee surgery is not a new concept, and it is frequently used in posterior cruciate ligament reconstruction. There are previous reports of its use in anterior cruciate ligament surgery, but it has not achieved routine use. With the move toward anatomic anterior cruciate ligament reconstruction, it is recognized that accurate tunnel placement is vital for a good clinical outcome. Visualization of the femoral and tibial footprints can be variable with the use of only an anterolateral viewing portal, and it may be necessary to create accessory anteromedial portals, which can cause problems with instrument crowding. Overall, the 70° arthroscope provides an excellent view of the femoral and tibial footprints and a view of the full length of the femoral and tibial tunnels through a single anterolateral viewing portal.
Various parameters are important for successful anterior cruciate ligament reconstruction (ACLR). When performing anatomic ACLR (either double bundle or single bundle), tunnel placement is 1 of the most important aspects of successful ACLR.1,2
The 70° arthroscope is the workhorse in hip arthroscopy3; its use has also been described in knee surgery.4 The reported advantage is an excellent view of the femoral footprint allowing accurate femoral tunnel placement.4,5 Despite this, most surgeons use a 30° arthroscope for ACLR.
Transtibial femoral tunnel placement has now largely been superseded by the transportal technique. Using a standard 30° arthroscope through the anterolateral (AL) portal gives a variable view of the femoral footprint, and it is often recommended to switch to an accessory medial portal to allow accurate tunnel placement.1 This results in 2 problems: increased surgical time in establishing and switching portals and instrument crowding. There is simulator evidence that a 45° arthroscope can increase visualization of the femoral footprint.6
Although the advantages of the 70° arthroscope for femoral placement are well described, we also believe that it provides a superior view of the tibial footprint and allows more accurate tibial tunnel placement.
Technique
The key points of the technique are summarized in Table 1, and the technique is demonstrated in Video 1.
Table 1.
Key Points
|
PBAHLM, posterior border of the anterior horn of the lateral meniscus.
The lower limb in prepared and draped after application of a thigh-high tourniquet. Initial assessment of the joint and treatment of meniscal pathology are performed with a standard 30° arthroscope through an AL viewing portal. We use a Stryker arthroscopy stack (Kalamazoo, MI). To facilitate rapid switching between the 30° and 70° arthroscopes, we use a Clinicon quick-change camera drape (P3 Medical, Bristol, England) coupled with Olympus 30° and 70° arthroscopes (Center Valley, PA). The use of a quick-change camera drape means that only 1 camera is required (Fig 1).
Fig 1.

Stryker camera covered with Clinicon quick-change camera drape (left) and Olympus 30° and 70° arthroscopes (right). This allows rapid changing between the 30° and 70° arthroscopes and the need for only 1 camera.
Femoral Tunnel
At this stage, the 30° arthroscope is exchanged for a 70° arthroscope, using the quick-change camera drape, and the femoral footprint is defined and debrided of soft tissue with a combination of a shaver and a wand. Figure 2 shows the different views obtained with a 30° arthroscope from the AL portal and the accessory anteromedial portal and, finally, the improved view using the 70° arthroscope from the AL portal. This facilitates accurate identification of the anatomic point for the femoral guide pin.
Fig 2.

(A) Femoral footprint view with 30° arthroscope from AL portal showing inadequate visualization of femoral footprint. (B) Femoral footprint view with 30° arthroscope from anteromedial portal. (C) Femoral footprint view with 70° arthroscope from AL portal. Excellent visualization of the femoral footprint is achieved.
Tibial Tunnel
The other significant advantage of the 70° arthroscope is in visualization of the tibial footprint. Preservation of the tibial stump is desirable to preserve mechanoreceptor function and improve graft healing.7 Standard landmarks such as the tibial spine may therefore be covered in soft tissue. We prefer to use the landmark of the posterior border of the anterior horn of the lateral meniscus as the midpoint of the anterior cruciate ligament (ACL) origin.8 Figure 3 shows the tibial footprint viewed through a 70° arthroscope, giving a bird’s-eye view of the PBAHLM.
Fig 3.
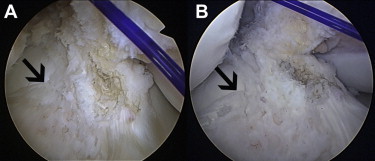
(A) Bird’s-eye view of the tibial footprint through the 70° arthroscope from the AL portal, showing the relation of the PBAHLM (arrow) with the center of the tibial stump (marked with diathermy). (B) View of the same patient using the 30° arthroscope from the AL portal, which does not show a clear relation between the PBAHLM and the tibial stump because of the more oblique view obtained with the 30° arthroscope.
Discussion
Although the use of the 70° arthroscope has been described previously, to our knowledge, this is the first description of its routine use to visualize the tibial footprint and establish the tibial tunnel.
For anatomic ACLR, there is a need to place both femoral and tibial tunnels in the center of the respective footprints, and therefore it is very important to have clear visualization of the footprint in its entirety and at an appropriate angle so that the center of the footprint is appropriately identified. Although it is possible to achieve this with a transportal technique, for better visualization of the femoral footprint, visualization of the footprint through an accessory medial portal while using a standard 30° arthroscope is recommended. Although this provides a good view of the femoral footprint, technically, it can be difficult especially because of crowding of instruments on the medial side while creating the tunnel.
The use of the 70° arthroscope from the AL portal gives an excellent view of the femoral footprint, and there is no overcrowding of instruments as can happen on the medial side. It is important to place the AL portal very close to the patellar tendon to gain the maximum advantage of the 70° arthroscope through the AL portal. In addition, the use of the 70° arthroscope through the AL portal provides an excellent view of the entire femoral tunnel, which is especially important in revision cases to make sure that the entire tunnel wall is healthy (Fig 4).
Fig 4.

(A) View of femoral tunnel with 70° arthroscope from AL portal. (B) Tibial tunnel viewed through 70° arthroscope from AL portal. (C) Tibial tunnel view in revision ACLR with 70° arthroscope through AL portal. One should note the ability to inspect the entire tunnel, which is particularly important if using an interference screw as femoral fixation and is also useful in revision ACLR.
The landmark for tibial tunnel placement should be easy to analyze preoperatively for anatomic ACLR in the individual patient. It should be easily identifiable arthroscopically and allow preservation of the tibial stump, which maintains mechanoreceptor function, provides biomechanical benefit, and promotes graft healing.7 The PBAHLM serves this purpose. We analyzed the relationship between the PBAHLM and the midpoint of the ACL footprint on 100 magnetic resonance imaging scans and found that the PBAHLM correlates with the midpoint of the ACL tibial footprint in the majority of the cases.8 This therefore allows accurate tibial tunnel placement without debridement of the tibial stump. It is also possible to obtain a good view of the tibial tunnel, which is particularly important in revision ACLR (Fig 4).
The advantages of the described technique are that it is technically straightforward to learn and the surgeon is quickly able to obtain a superior view of patient anatomy to facilitate accurate tunnel placement. The potential disadvantages of the technique are the requirement for new equipment and the need to switch from a 30° arthroscope to a 70° arthroscope once initial joint inspection has been performed and meniscal pathology has been treated. There may be a short learning curve in adjusting to the routine use of the 70° arthroscope.
Overall, the 70° arthroscope provides an excellent view of the femoral and tibial footprints and a view of the full length of the femoral and tibial tunnels through a single AL viewing portal.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Setup and equipment required to perform procedure. The different views obtained when establishing the femoral and tibial tunnels between the 30° and 70° arthroscopes are also presented.
References
- 1.Chhabra A., Starman J.S., Ferretti M., Vidal A.F., Zantop T., Fu F.H. Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. J Bone Joint Surg Am. 2006;88(suppl 4):2–10. doi: 10.2106/JBJS.F.00616. [DOI] [PubMed] [Google Scholar]
- 2.Hofbauer M., Muller B., Murawaski C.D., van Eck C.F., Fu F.H. The concept of individualized anatomic anterior cruciate ligament (ACL) reconstruction. Knee Surg Spots Traumatol Arthrosc. June 6, 2013 doi: 10.1007/s00167-013-2562-4. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 3.Bond J.L., Knutson Z.A., Ebert A., Guanche C.A. The 23-point arthroscopic examination of the hip: Basic setup, portal placement, and surgical technique. Arthroscopy. 2009;25:416–429. doi: 10.1016/j.arthro.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 4.Bedi A., Dines J., Dines D.M. Use of the 70° arthroscope for improved visualization with common arthroscopic procedures. Arthroscopy. 2010;26:1684–1696. doi: 10.1016/j.arthro.2010.04.070. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A., Altchek D.W. The “footprint” anterior cruciate ligament technique: An anatomic approach to anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:1128–1138. doi: 10.1016/j.arthro.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Okazaki K. The 45-degree arthroscope improves visualization of the femoral attachment of the anterior cruciate ligament. Surg Sci. 2012;3:43–46. [Google Scholar]
- 7.Borbon C.A., Mouzopoulos G., Siebold R. Why perform an ACL augmentation? Knee Surg Sports Traumatol Arthrosc. 2012;20:245–251. doi: 10.1007/s00167-011-1565-2. [DOI] [PubMed] [Google Scholar]
- 8.Mandalia V., Kassam A., Schranz P. The lateral meniscus as a guide to anatomic tibial tunnel placement during ACL reconstruction. Bone Joint J. 2013;95-B:11. (abstr, suppl 19) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Setup and equipment required to perform procedure. The different views obtained when establishing the femoral and tibial tunnels between the 30° and 70° arthroscopes are also presented.


