Abstract
Resection is a standard surgical procedure for a talocalcaneal coalition (TCC). A posterior approach is the representative technique for hindfoot endoscopy, and there is only 1 report of endoscopic resection of TCC using this approach. Disadvantages of the posterior approach for TCC are as follows: (1) the indication is limited to posterior-facet coalition, (2) the flexor hallucis longus can be an obstacle in approaching the coalition, (3) the acute insertion angle between the endoscope and instrument reduces operability, and (4) a position change and additional skin incision are essential for conversion to an open procedure. In contrast, a posteromedial approach for TCC with established portals at the entrance and exit of the flexor retinaculum is a useful technique because (1) the indication is allow to middle- and posterior-facet coalitions, (2) increased perfusion pressure allows the creation of sufficient working space, (3) operating the instrument only at the coalition site decreases the risk of tendon injury and neurovascular damage, (4) the obtuse insertion angle between the endoscope and instrument improves operability, and (5) a position change and additional skin incision are unnecessary for conversion to an open procedure.
Since the first clinical report of arthroscopy of the ankle by Watanabe,1 the use of endoscopic surgery in the foot and ankle region has increased. In recent years the extra-articular application has markedly increased. Endoscopy with a posterior approach (PA) is extra-articular endoscopy of the foot and ankle. Os trigonum, flexor hallucis longus (FHL) tendinitis, and insertional Achilles tendinopathy are primary disorders treated with PA endoscopy. Many reports concerning the utility and safety of this approach are available.
Tarsal coalition, a condition that is observed in approximately 1% of the overall population, is often asymptomatic and sometimes overlooked.2 An incomplete coalition is considered to become painful as a result of microfracturing at the coalition-bone interface. Therefore external fixation is often applied for 4 to 6 weeks as conservative therapy, and surgical therapy is performed in treatment-resistant cases. The majority of tarsal coalitions are calcaneonavicular coalitions (CNCs) or talocalcaneal coalitions (TCCs). Resection is the standard surgical procedure for a CNC, whereas resection or arthrodesis is chosen based on the extent of coalition for a TCC.
Since Lui3 reported endoscopic resection of a CNC in 2006, occasional studies have shown therapeutic outcomes of endoscopies for CNCs.4,5 The first report about endoscopic resection of TCCs was published by Bonasia et al.6 in 2011, and they limited the indication to posterior-facet coalition. On the other hand, Jagodzinski et al.7 reported in 2013 that the lateral approach was useful for middle-facet coalition but had a risk of neurovascular damage for a posterior-facet coalition.
This study aims to introduce and examine the utility of endoscopic resection of a TCC using a posteromedial approach (PMA), which has not been previously reported.
Surgical Technique
Hyperbaric spinal anesthesia with 0.5% bupivacaine is administered. The patient is placed in the supine position with the hip joint in a flexed, abducted, and externally rotated position; the knee in a flexed position; and the ankle in a neutral position. In addition, the posteromedial side of the hindfoot is stabilized and placed facing up (Fig 1). A tourniquet is placed on the femur before surgery in case of vascular injury but is not generally used.
Fig 1.

Intraoperative photograph showing the endoscope in the proximal portal and the power instrument in the distal portal.
Portal positions, the medial malleolus, the posterior tibial artery, and the site of the coalition are marked in advance by use of palpation or under fluoroscopy. The viewing portal is created approximately 2 fingerbreadths posterior to the vertex of the medial malleolus (the entrance of the flexor retinaculum), and the working portal is created approximately 3 fingerbreadths inferior to the vertex of the medial malleolus (the exit of the flexor retinaculum) (Fig 2).
Fig 2.

Preoperative marking for PMA. The portal positions, medial malleolus, posterior tibial artery, and site of the coalition are marked. (Po1, viewing portal; Po2, working portal.)
After both portals have been established, the soft tissue is separated from the coalition thoroughly with a Cobb rasp or mosquito forceps to prevent the soft tissue from obstructing the viewing field. Subsequently, a 2.7-mm 30° endoscope (Stryker, Kalamazoo, MI) is inserted. At the beginning of surgery, high perfusion pressure is required to prevent interpositioning of the soft tissue in the viewing field. Therefore the perfusion pressure must be adjusted from 20 to 80 mm Hg throughout the surgical procedure.
Soft tissue such as the joint capsule or periosteum adheres to the surface of the coalition (Fig 3A). Therefore, by use of a shaver (Stryker CORE shaver system) or a radiofrequency device (Stryker SERFAS Energy RF Ablation System), as much soft tissue must be removed as possible to allow easy coalition resection (Video 1). Furthermore, because the neurovascular bundle is on the side that is opposite the coalition, the working surface of the instrument must face only the coalition side to prevent any neurovascular damage (Fig 3B, Video 1).
Fig 3.
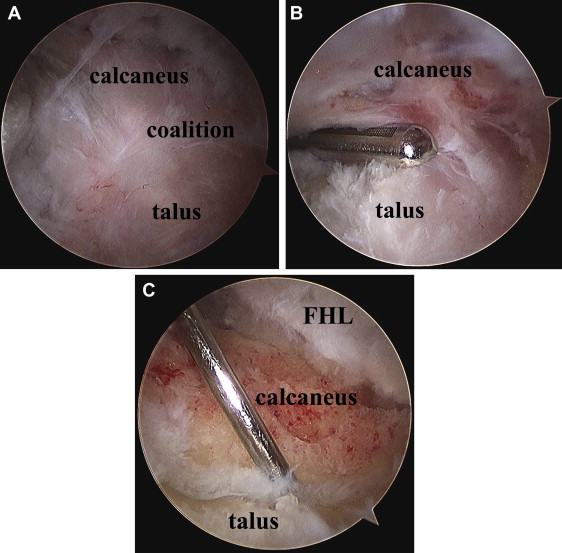
Endoscopic photographs of a left foot. (A) The TCC is visualized. (B) The surface of the coalition is debrided with a shaver. (C) A probe can be inserted in the subtalar joint after sufficient resection of the coalition.
While periodically checking the positions of the FHL and flexor digitorum longus (FDL), the surgeon performs sufficient resection of the coalition using an abrader (Stryker CORE shaver system) until the normal articular surface can be confirmed (Fig 3C, Video 1). When it is difficult to determine whether the coalition is being correctly resected, the position of the power instrument must be confirmed under fluoroscopy (Fig 4). A bone wax coating or fat grafts are not added to the resected surface of the coalition.
Fig 4.

Intraoperative fluoroscopic picture showing that the power instrument is positioned correctly.
The post-treatment care is as follows. Immediately after surgery, movement of the toes is permitted, although movement of the ankle is prohibited for 1 week to prevent hemorrhaging and swelling. Movement of the ankle and weight bearing are permitted 1 week after surgery. If there is no swelling or pain, sports activities are permitted 4 to 6 weeks after surgery. Computed tomography is adequate to evaluate the extent of the coalition in detail (Fig 5).
Fig 5.

Coronal computed tomography images of a TCC. (A) The preoperative image shows an extensive non-osseous coalition (oval). (B) The postoperative image shows that the coalition is sufficiently resected (circle).
Discussion
A TCC occurs on the medial side of the subtalar joint in the area from the sustentaculum tali to the medial tubercle of the talus. The site of the coalition is posterior to the FDL and anterior to the FHL, and the neurovascular bundle is adjacent to the posteromedial side of the FHL.8 While one is performing endoscopy under a narrow viewing field, it is essential to understand this anatomy.
The coalition is located anterior to the medial tubercle of the talus, and the neurovascular bundle is adjacent to the posteromedial side of the FHL. To perform a safe endoscopic resection of the coalition using the PA, it is necessary to access the lateral side of the FHL9 and perform FHL decompression and then resection, including the medial tubercle of the talus (Fig 6). Keeling and Guyton10 conducted a cadaveric study in which they performed endoscopic FHL decompression in 8 cases. Although no neurovascular damage was observed in any case, tendon injuries were observed in 3 cases. Therefore, while one is performing this technique, the risk of neurovascular damage and tendon injury should be considered.
Fig 6.

Schema of PA. (Po1, viewing portal; Po2, working portal.)
However, resection of a coalition using the PMA has the advantage of allowing a direct approach to both the middle- and posterior-facet coalitions without obstruction, despite the FDL being anterior, the FHL being posterior, and the neurovascular bundle being posteromedial to the coalition site (Fig 7); this is considered to be because of increased perfusion pressure, which allows the creation of sufficient working space, and operation of the instrument only at the coalition site, which may decrease the risk of tendon injury and neurovascular damage. Consequently, both the middle- and posterior-facet coalitions can be treated with the PMA.
Fig 7.

Schema of PMA. (Po1, viewing portal; Po2, working portal.)
The positional relations between the portals and the coalition site in the 2 approaches are as follows: In the PA, it is necessary to go around the FHL to the lateral side, which increases the distance between the 2 portals and the coalition site. In contrast, during the PMA, the flexor retinaculum is the only obstruction; therefore the distance between the 2 portals and the coalition site is shorter than that in the PA. Furthermore, whereas the angle of insertion of the endoscope and the instrument is acute in the PA, but it is an obtuse angle in the PMA; therefore interference between the endoscope and instrument is unlikely, which makes the PMA advantageous from a technical perspective as well. In addition, because the PA necessitates complete resection of the medial tubercle of the talus, the FHL dislocates easily to the medial side, which causes a problem of increased posterior instability of the talus11 (Figs 6 and 7). The PA requires a position change and an additional skin incision for conversion to an open procedure, whereas the PMA only requires extension of the skin incision and no position change.
On the basis of the advantages, such as the low frequency of complications and ease of surgical technique, endoscopic resection of a TCC using the PMA is considered a useful technique.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Patient positioning, technique to establish posteromedial portals, and main steps of procedure, including (1) soft-tissue debridement of surface of coalition, (2) resection of coalition, and (3) evaluation of complete resection and adequate subtalar motion.
References
- 1.Watanabe M. Teishin Hospital; Tokyo: 1972. Selfoc-Arthroscope (Watanabe no. 24 arthro-scope). Monograph. [Google Scholar]
- 2.Lemley F., Berlet G., Hill K., Philbin T., Isaac B., Lee T. Current concepts review: Tarsal coalition. Foot Ankle Int. 2006;27:1163–1169. doi: 10.1177/107110070602701229. [DOI] [PubMed] [Google Scholar]
- 3.Lui T.H. Arthroscopic resection of the calcaneonavicular coalition or the “too long” anterior process of the calcaneus. Arthroscopy. 2006;22:903.e1–903.e4. doi: 10.1016/j.arthro.2005.12.059. [DOI] [PubMed] [Google Scholar]
- 4.Bauer T., Golano P., Hardy P. Endoscopic resection of a calcaneonavicular coalition. Knee Surg Sports Traumatol Arthrosc. 2010;18:669–672. doi: 10.1007/s00167-010-1086-4. [DOI] [PubMed] [Google Scholar]
- 5.Knörr J., Accadbled F., Abid A. Arthroscopic treatment of calcaneonavicular coalition in children. Orthop Traumatol Surg Res. 2011;97:565–568. doi: 10.1016/j.otsr.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 6.Bonasia D.E., Phisitkul P., Saltzman C.L., Barg A., Amendola A. Arthroscopic resection of talocalcaneal coalitions. Arthroscopy. 2011;27:430–435. doi: 10.1016/j.arthro.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Jagodzinski N.A., Hughes A., Davis N.P., Butler M., Winson I.G., Parsons S.W. Arthroscopic resection of talocalcaneal coalitions—A bicentre case series of a new technique. Foot Ankle Surg. 2013;19:125–130. doi: 10.1016/j.fas.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Lijoi F., Lughi M., Baccarani G. Posterior arthroscopic approach to the ankle: An anatomic study. Arthroscopy. 2003;19:62–67. doi: 10.1053/jars.2003.50003. [DOI] [PubMed] [Google Scholar]
- 9.van Dijk C.N. Hindfoot endoscopy. Foot Ankle Clin. 2006;11:391–414. doi: 10.1016/j.fcl.2006.03.002. vii. [DOI] [PubMed] [Google Scholar]
- 10.Keeling J.J., Guyton G.P. Endoscopic flexor hallucis longus decompression: A cadaver study. Foot Ankle Int. 2007;28:810–814. doi: 10.3113/FAI.2006.0810. [DOI] [PubMed] [Google Scholar]
- 11.Kapandji I.A. Elsevier; Amsterdam: 2010. Physiology of the joints: Volume 2 Lower Limb. Ed 6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient positioning, technique to establish posteromedial portals, and main steps of procedure, including (1) soft-tissue debridement of surface of coalition, (2) resection of coalition, and (3) evaluation of complete resection and adequate subtalar motion.


