Abstract
Humeral avulsion of the inferior glenohumeral ligament (HAGL) has recently gained more recognition as a cause of shoulder instability. Posterior HAGL lesions, being much more infrequent than anterior disruptions, have only recently been documented as a notable cause of posterior instability. We detail the treatment of a previously unreported case of a posterior HAGL variant lesion consisting of a bony avulsion with involvement of the teres minor tendon. Arthroscopic fixation was facilitated by use of a “sheathless” arthroscopic approach with a 70° arthroscope and suture anchor.
Glenohumeral instability can result from a wide range of factors. Increased recognition has been given to the humeral avulsion of the inferior glenohumeral ligament (HAGL) lesion. The typical HAGL lesion most commonly described is an avulsion of the anterior inferior glenohumeral ligament from its attachment on the humerus.1,2 This leads to anterior instability, which occurs much more frequently than posterior instability.3,4 The posterior HAGL lesion, however, has been described as a cause of posterior shoulder instability or pain.5,6 Diagnosis can be difficult and is often delayed because of nonspecific shoulder pain or multiple potential etiologies for isolated posterior shoulder pain. These may include tears of the labrum, capsule, or rotator cuff or bony insufficiency. Posterior HAGL lesions have been documented in association with anterior and posterior Bankart lesions; anterior, superior, and posterior labral lesions; and anterior labral periosteal sleeve avulsion lesions. Both open repair and arthroscopic repair have subsequently been described.5,7-9 Teres minor avulsions are rare and, when present, frequently occur in combination with supraspinatus, infraspinatus, or massive rotator cuff tears.10-12
To our knowledge, there is no mention in the literature of a bony posterior HAGL lesion that also involves an isolated teres minor tendon avulsion. We describe the arthroscopic treatment of a traumatic posterior HAGL variant with a bony avulsion and a lesion involving the teres minor tendon.
Case
A 16-year-old right hand–dominant male baseball player sustained a traumatic injury to his left shoulder when he ran into an outfield fence chasing a fly ball. He forcefully struck the wall with a direct blow to the anterior and lateral aspects of the shoulder. He described the sensation of a “slip” of his shoulder but did not sustain a frank dislocation. Radiographs obtained the day of injury yielded negative findings. His examination showed good active motion with minimal rotator cuff weakness. Conservative management for a shoulder strain was subsequently initiated.
After 4 weeks of physical therapy, the patient still had persistent shoulder pain, localized anteriorly, with no symptomatic improvement. His physical examination at that time showed diffuse anterior tenderness to palpation. He had full active range of motion with generalized discomfort. His pain was exacerbated by external rotation with the shoulder in abduction. He had no acromioclavicular joint tenderness or deformity. He showed good rotator cuff strength on stress testing, and findings of all impingement tests were negative. He had a trace sulcus sign that was also present in the contralateral shoulder. His shoulder seemed stable on load-and-shift stress testing, and the result of the relocation maneuver was negative.
A gadolinium magnetic resonance imaging (MRI) study showed a posterior avulsion of the inferior glenohumeral ligament complex off the humeral head with an associated teres minor avulsion (Figs 1 and 2). There was no discernible labral tear—or obvious marrow edema or chondral defect—of the glenoid or humeral head.
Fig 1.
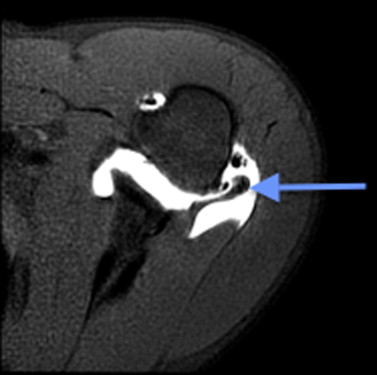
Axial MRI study with an arrow pointing to a posterior bony HAGL lesion.
Fig 2.
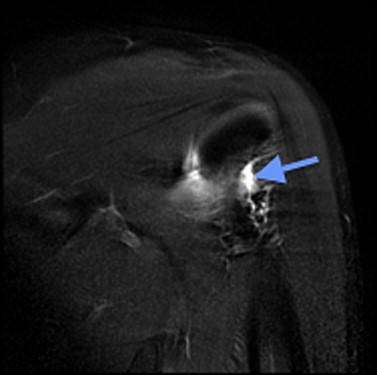
Coronal MRI study of a posterior bony HAGL lesion with an arrow pointing to an associated teres minor tendon avulsion.
Surgical treatment was recommended with a plan to perform arthroscopic fixation of the posterior capsular avulsion injury if possible and, if not, to perform an open repair. On examination of the patient's shoulder under anesthesia, it was grossly unstable with posterior load-and-shift stress testing.
Surgical Technique
The identification and subsequent repair technique are shown in Video 1, with key points for an arthroscopic repair shown in Table 1. Arthroscopy was performed with the patient in the lateral decubitus position. A posterolateral portal just off the posterolateral margin of the acromion was established for initial viewing, along with a standard anterosuperior portal in the rotator interval, and a port-of-Wilmington posterosuperior portal.10 Clear cannulas, 5.75 mm in diameter (Arthrex, Naples, FL), were placed in the rotator interval and the port of Wilmington. A larger 8.25-mm clear cannula (Arthrex) was placed posterolaterally. This allowed for a “sheathless” operative approach, interchanging the arthroscope and instrumentation from portal to portal with ease (Fig 3).
Table 1.
Key Points for Arthroscopic Repair of Posterior Bony HAGL Lesion With Teres Minor Avulsion
| Perform a thorough preoperative examination with the patient under anesthesia to evaluate the extent of posterior instability. |
| Perform a thorough arthroscopic evaluation of the shoulder to identify other concurrent lesions. |
| Use standard anterosuperior and posterolateral shoulder arthroscopy portals, but the addition of a posterosuperior port-of-Wilmington portal aids in visualization and fixation of posterolateral lesions. |
| Placement of multiple cannulas to create a sheathless approach allows for interchanging the arthroscope and instrumentation from portal to portal with ease. |
| When attempting to visualize the posterior HAGL lesion, use of a 70° arthroscope placed through the posterosuperior port of Wilmington provides the best visualization. |
| Use a shaver and curette to prepare the bony bed of the humerus and create a good healing surface. |
| Use of a small (3.0-mm) SutureTak preloaded with 2 sutures (1 No. 2 FiberWire and 1 No. 2 TigerWire) allows for ease of management of the tissue with adequate strength of fixation. |
| Drill a hole in the previously prepared bony bed with a 2.9-mm drill, and use a mallet to place the SutureTak into position. |
| Pass the sutures through the tissue and around the bony avulsion fragment using a curved SutureLasso. |
| Tie both the FiberWire and TigerWire with a locking knot (we use a Tuckahoe knot), backed up by 3 alternating half-hitches. |
| Visually ensure that there is good bony apposition of the bony avulsion to its site of origin on the humerus. |
Fig 3.
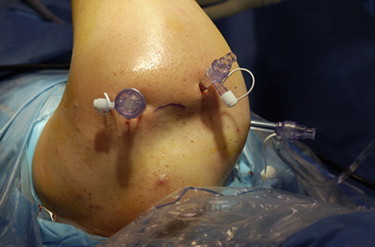
Intraoperative photograph showing sheathless arthroscopy setup of left shoulder with patient placed in lateral decubitus position.
Intraoperative findings with the 30° arthroscope included a normal biceps tendon and superior labral complex. There was a normal anterior and inferior labrum, but a localized, acute-appearing posterior labral tear at the 3-o'clock position was present (Fig 4).
Fig 4.

Arthroscopic view showing posterior labral tear in left shoulder as viewed from posterolateral portal.
Other than a small area of grade 2 chondromalacia of the posterior humeral head, the articular surfaces of the humeral head and glenoid were normal. The posterior HAGL–teres minor lesion was seen but was poorly visualized. A 70° arthroscope was then placed in the port-of-Wilmington cannula and provided excellent visualization of the extent of the lesion, which appeared to have both attached posterior capsular tissue and part of the teres minor tendon with bone attached (Fig 5).
Fig 5.

Arthroscopic view from a posterosuperior portal with a 70° arthroscope in a left shoulder with the arrow pointing to a bony posterior HAGL lesion with teres minor avulsion.
The lesion was probed, and the bony avulsion component had an approximate size of 1 × 1 cm. It was then grasped from the posterolateral cannula and reduced toward its humeral attachment, with good evidence of mobilization. Therefore we believed that arthroscopic repair would be feasible. Attention was first directed toward the posterior labral tear. The posterior glenoid rim in the area of the tear was debrided with a curette and shaver. The posterior labrum was then repaired with 1 No. 2 FiberLink knotless cinch suture (Arthrex) and secured to the posterior glenoid with a 2.9-mm BioComposite PushLock (Arthrex) (Fig 6). Attention was then returned to the posterior HAGL lesion.
Fig 6.

Arthroscopic view showing labral repair in left shoulder as viewed from posterolateral portal.
The 70° arthroscope through the port of Wilmington was used to optimize visualization of the posterolateral shoulder. A shaver through the posterolateral portal was initially used to remove soft tissue at the origin site of the bony avulsion from the posteroinferior aspect of the greater tuberosity of the humerus. A curette was then used to debride this “bony bed” and create a good potential healing surface (Fig 7).
Fig 7.

Arthroscopic view of preparation of humeral origin of posterior bony HAGL lesion in left shoulder as viewed from posterosuperior portal.
A 3.0-mm SutureTak (Arthrex) with 1 No. 2 FiberWire suture (Arthrex) and 1 No. 2 TigerWire suture (Arthrex) attached was selected for fixation. A 2.9-mm drill hole was made in the mid portion of the previously prepared site on the humerus, and the SutureTak was placed in position to the appropriate depth by use of a mallet. A curved SutureLasso (Arthrex) was then used to make a pass through the tissue just posterior to the bony avulsion fragment, and a nitinol wire was threaded through the SutureLasso. One end of the TigerWire suture was then shuttled through the tissue with the wire so that it wrapped around the bony fragment. A second pass through the tissue was made with the lasso more anterior and inferior to the first, closer to the humeral side, and the nitinol wire and 1 end of the FiberWire suture were passed in the same fashion. The FiberWire was then tied with a locking, sliding Tuckahoe-type knot,13 backed up by 3 alternating half-hitches. The TigerWire suture was tied in the same fashion. The result was excellent apposition of the bony avulsion to the site of its origin on the humerus (Figs 8 and 9). This restored adequate tension of the posterior HAGL and teres minor tears.
Fig 8.

Arthroscopic view of final suture fixation of posterior bony HAGL lesion in left shoulder as viewed from posterosuperior portal.
Fig 9.

Arthroscopic view from posterosuperior portal underneath repair of posterior bony HAGL lesion, confirming apposition of bony avulsed fragment to native humerus in left shoulder. Both blue FiberWire and TigerWire sutures are visible.
During the subsequent postoperative course, the patient had no complications. He was immobilized in a splint in the gunslinger position for 2 weeks and then started range-of-motion exercises. At his follow-up appointment 6.5 weeks from surgery, he had no further shoulder pain. His examination showed full active overhead elevation of the left upper extremity, with external rotation of 80° in abduction. His shoulder was stable posteriorly on load-and-shift stress testing. A repeat non-contrast MRI study was obtained at this visit and showed good reduction and apparent healing of the posterior labral tear. In addition, lucency from the posterolateral suture anchor in the humerus was noted (Fig 10), along with excellent approximation of the teres minor and posterior capsule to the humerus (Fig 11). The patient was last seen 4.5 months after surgery. He had no pain or complaints and was anxious to return to playing high school basketball. He had a full range of motion on examination with rotator cuff strength rated as 5 of 5 on stress testing. The O'Brien labral maneuver was negative, and his shoulder was stable on posterior load-and-shift stress testing with no apprehension. He was then allowed to return to full activities including basketball.
Fig 10.

Axial T2-weighted MRI study with an arrow pointing to a lucency from an absorbable suture anchor, which was used for repair of posterior bony HAGL lesion and placed in posterolateral humeral head.
Fig 11.
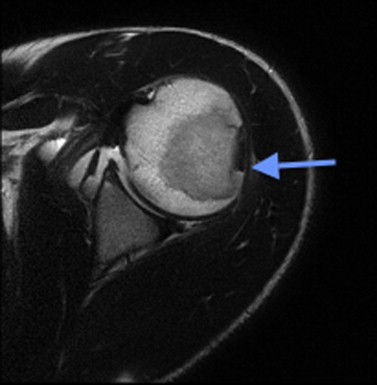
Axial T2-weighted image with an arrow pointing to the interval healing of previous posterior HAGL variant lesion and teres minor attachment. In addition, the posterior labrum appears healed.
Discussion
The HAGL lesion has been shown to be a prominent cause of shoulder instability and pain.5,6,8,9 Anterior instability occurs with much more frequency than posterior instability, often due to Bankart anterior capsulolabral lesions, generalized laxity, or the classic anterior HAGL lesion. Nicola4 reported the first HAGL lesion in 1942 based on cadaveric dissection. Wolf et al.2 first referred to the injury as humeral avulsion of the glenohumeral ligaments (HAGL) in 1995. Only with the advances in modern imaging techniques and arthroscopy within the past 20 years have HAGL lesions become increasingly recognized and diagnosed.1,3 Posterior HAGL lesions remain infrequent, with primarily case reports and small series documented in the orthopaedic literature.5,6,8,9 More specifically, the posterior HAGL lesion is reported to represent only 7% of cases of HAGL lesions versus anterior lesions in 93% of cases.14 Bony HAGL lesions have also been reported but primarily in relation to anterior tears and instability.15 Bui-Mansfield et al.16 developed the West Point classification system to describe these HAGL lesions. They classify each lesion into 1 of 6 categories based on anterior or posterior involvement, the presence or absence of bony avulsion, and the presence of associated labral pathology. In their literature review they found that anterior HAGL lesions comprised 55% of cases; anterior bony HAGL lesions, 17%; anterior inferior HAGL lesions, 21%; posterior HAGL lesions, 3%; posterior inferior HAGL lesions, 4%; and posterior bony HAGL lesions, 0%.
Isolated teres minor avulsions are also extremely rare. Teres minor injuries occur primarily in concert with injury to other musculotendinous portions of the rotator cuff, although the teres minor tendon is noted to be intact in 90.8% of rotator cuff injuries.12
We describe a case of a posterior bony HAGL variant and associated teres minor tendon avulsion. To our knowledge, this represents the first reported case of this type of lesion. The clinical setting of our teenage patient was traumatic, but the history and physical examination were relatively nonspecific. Notably, as reported by Brown et al.,7 the few cases of reverse HAGL lesions previously reported in the literature also typically comprised teenagers with a singular event—a high-impact injury. The abnormalities in our case that differentiate it were the bony component and the teres minor avulsion. Our patient had no definitive episode of dislocation and presented with nonfocal but primarily anterior shoulder pain. Physical therapy may often be helpful in patients with nonspecific shoulder pain or with mild posterior instability through strengthening of the external rotators. After physical therapy was unsuccessful in this case, however, a contrast MRI study was obtained and showed the unique posterior HAGL variant with teres minor avulsion. Surgery was recommended, and examination of the patient under anesthesia confirmed significant posterior instability consistent with the identified arthroscopic pathology of the bony avulsion of the posterior capsule and teres minor tendon.
HAGL lesions have been successfully treated with both open repair and arthroscopic repair.5,7-9 In our case we were able to repair the lesion through standard arthroscopy portals using a 70° arthroscope. This was a key step for achieving arthroscopic fixation of the lesion through standard portals because adequate visualization of the posterolateral working area could not be achieved solely with a 30° arthroscope. Furthermore, using a sheathless arthroscopic approach provided a very efficient means for smoothly changing the viewing and instrument working portals as necessary without ever reinserting the arthroscopic sheath itself. This would have been difficult to do while working in the small space of the posterolateral shoulder. This technique allowed us to achieve good preparation and anatomic bony apposition of this unique avulsion lesion to the posterolateral humerus with a strong suture anchor repair. Postoperative MRI showed excellent reapproximation of the posterolateral capsule and teres minor tendon approximately 7 weeks after surgery, indicating early signs of a successful repair of this unique HAGL variant.
In conclusion, we believe that one should maintain a high level of suspicion that a posterior HAGL lesion, though uncommon, may present with vague shoulder pain after a traumatic injury in a young patient. Appropriate imaging with MRI, preferably with contrast, is critical to establish the diagnosis. Surgical repair is indicated in a young, active patient to optimize shoulder stability. Although repair can be performed in an open manner, it would necessitate an extensile exposure and potential neurovascular risk, particularly to the axillary nerve in the quadrangular space. A minimally invasive arthroscopic repair, however, has minimal risks but has significant advantages. Limitations of an arthroscopic approach include difficulty gaining adequate visualization for repair of a lesion in this area of the shoulder. In our case we found use of the 70° arthroscope critical for visualization and access to the posterolateral compartment of the shoulder to facilitate a straightforward repair.
Footnotes
The authors report the following potential conflict of interest or source of funding: P.A.S. receives support from Arthrex for consultancy, grants for research staff and support of clinical trials, payment for development of educational presentations, funding for support staff and the engagement of clinical trials and research studies at the group practice. He is a stockholder in Spinal Simplicity.
Supplementary Data
Intraoperative video showing identification of pathologic posterior bony HAGL lesion with teres minor avulsion and subsequent arthroscopic repair in left shoulder as viewed from posterior portal.
References
- 1.Field L.D., Bokor D.J., Savoie F.H., III Humeral and glenoid detachment of the anterior inferior glenohumeral ligament: A cause of anterior instability. J Shoulder Elbow Surg. 1997;6:6–10. doi: 10.1016/s1058-2746(97)90064-1. [DOI] [PubMed] [Google Scholar]
- 2.Wolf E.M., Cheng J.C., Dickson K. Humeral avulsion of the glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11:600–607. doi: 10.1016/0749-8063(95)90139-6. [DOI] [PubMed] [Google Scholar]
- 3.Bokor D.J., Conboy V.B., Olson C. Anterior instability of the glenohumeral joint with humeral avulsion of the glenohumeral ligament: A review of 41 cases. J Bone Joint Surg Br. 1999;81:93–96. doi: 10.1302/0301-620x.81b1.9111. [DOI] [PubMed] [Google Scholar]
- 4.Nicola T. Anterior dislocation of the shoulder: The role of the articular capsule. J Bone Joint Surg. 1942;25:614–616. [Google Scholar]
- 5.Castagna A., Snyder S.J., Conti M., Borroni M., Massazza G., Garofalo R. Posterior humeral avulsion of the glenohumeral ligament: A clinical review of 9 cases. Arthroscopy. 2007;23:809–815. doi: 10.1016/j.arthro.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Safran O., DeFranco M.J., Hatem S., Iannotti J.P. Posterior humeral avulsion of the glenohumeral ligament as a cause of posterior shoulder instability. A case report. J Bone Joint Surg Am. 2004;86:2732–2736. doi: 10.2106/00004623-200412000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Brown T., Barton S., Savoie F.H. Reverse humeral avulsion glenohumeral ligament and infraspinatus rupture with arthroscopic repair. Am J Sports Med. 2007;35:2135–2139. doi: 10.1177/0363546507305012. [DOI] [PubMed] [Google Scholar]
- 8.Chhabra A., Diduch D.R., Anderson M. Arthroscopic repair of posterior humeral avulsion of the inferior glenohumeral ligament (HAGL) lesion. Arthroscopy. 2004;20:73–76. doi: 10.1016/j.arthro.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 9.Hasan S.S., Fleckenstein C., Albright J. Open treatment of a posterior humeral avulsion of the glenohumeral ligaments: A case report and review of the literature. J Shoulder Elbow Surg. 2007;16:e3–e5. doi: 10.1016/j.jse.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Hottya G.A., Tirman P.F., Bost F.W., Montgomery W.H., Wolf E.M., Genant H.K. Tear of the posterior shoulder stabilizers after posterior dislocation: MR imaging and MR arthrographic findings with arthroscopic correlation. AJR Am J Roentgenol. 1998;171:763–768. doi: 10.2214/ajr.171.3.9725313. [DOI] [PubMed] [Google Scholar]
- 11.Keener J.D., Brophy R.H. Superior labral tears of the shoulder: Pathogenesis, evaluation and treatment. J Am Acad Orthop Surg. 2009;17:627–637. doi: 10.5435/00124635-200910000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Melis B., DeFranco M.J., Ladermann A., Barthelemy R., Walch G. The teres minor muscle in rotator cuff tears. Skeletal Radiol. 2011;40:1335–1344. doi: 10.1007/s00256-011-1178-3. [DOI] [PubMed] [Google Scholar]
- 13.Wiley W.B., Goradia V.K. The Tuckahoe knot: A secure locking slip knot. Arthroscopy. 2004;20:556–559. doi: 10.1016/j.arthro.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 14.George M.S., Khazzam M., Kuhn J.E. Humeral avulsion of glenohumeral ligaments. J Am Acad Orthop Surg. 2011;19:127–133. doi: 10.5435/00124635-201103000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Oberlander M.A., Morgan B.E., Visotsky J.L. The BHAGL lesion: A new variant of anterior shoulder instability. Arthroscopy. 1996;12:627–633. doi: 10.1016/s0749-8063(96)90205-4. [DOI] [PubMed] [Google Scholar]
- 16.Bui-Mansfield L.T., Banks K.P., Taylor D.C. Humeral avulsion of the glenohumeral ligaments: The HAGL lesion. Am J Sports Med. 2007;35:1960–1966. doi: 10.1177/0363546507301081. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative video showing identification of pathologic posterior bony HAGL lesion with teres minor avulsion and subsequent arthroscopic repair in left shoulder as viewed from posterior portal.


