Abstract
The management of pre-collapse osteonecrosis of the femoral head is controversial. Core decompression is a technique that theoretically decreases the intraosseous pressure of the femoral head, resulting in a local vascularized healing response. Its efficacy has been shown in delaying early subchondral collapse. We describe the technique of arthroscopic-assisted core decompression of the femoral head for osteonecrosis. The advantages of this technique include evaluation of the presence or absence of articular cartilage injury, subchondral collapse, and guidance during reaming and curettage. It also allows the ability to address any concomitant soft-tissue or bony pathology associated with or in addition to the osteonecrotic lesion.
Osteonecrosis (ON) of the femoral head is a condition in which subchondral bone loses its viability. This results in sclerosis, weakening of the surrounding bone, and subsequent subchondral collapse. Subchondral collapse can then lead to articular incongruity and resultant osteoarthritis. Treatment delay may preclude a joint preservation procedure and necessitate total hip arthroplasty.1,2 This may not be the best option in young, active patients. Early diagnosis before subchondral collapse lends itself to treatment options that can potentially delay collapse. One such technique is core decompression. Core decompression is a technique in which the necrotic lesion is reamed or drilled to decrease local intraosseous pressure and stimulate a vascularized healing response. Effective results for pre-collapse stages have been shown.2 Using this technique, we describe the use of hip arthroscopy to aid in the diagnosis and treatment of pre-collapse ON of the femoral head (Table 1).
Table 1.
Technical Pearls for Arthroscopically Assisted Core Decompression
| Hip Arthroscopy | Core Decompression |
|---|---|
| Establish AL and anterior portals. | Maintain arthroscope in joint to assist in avoiding subchondral penetration. |
| Evaluate femoral head for subchondral collapse. | Introduce drill and reamer under radiographic guidance; lesion is typically in anterosuperior femoral head. |
| Evaluate integrity of articular cartilage. | Introduce arthroscope into socket to confirm integrity of subchondral bone at lesion site. |
| Evaluate labrum and bony margin of acetabulum. | Implant ceramic putty to provide compressive strength. |
| Use interportal or T-capsulotomy to address concomitant labral and/or femoral head-neck pathology. | Perform dynamic arthroscopy of femoral head. |
Case Example and Surgical Technique
A 51-year-old white woman presented with a complaint of left hip pain localized to the groin and buttock for more than 1 year. Conservative treatment including nonsteroidal anti-inflammatory medications and physical therapy failed. She had 2 intra-articular cortisone injections that provided immediate relief, but each lasted less than 2 weeks. Examination showed limited hip flexion, adduction, and internal rotation because of pain compared with the contralateral hip. Radiographs showed a concentric joint without evidence of joint space narrowing (Fig 1A). There was no dysplasia or significant cam or pincer impingement lesions. Standard T1, T2, and Short T1 Inversion Recovery magnetic resonance imaging (MRI) showed ON of the anterosuperior femoral head without evidence of subchondral collapse (Fig 1B). The articular cartilage was intact, and there was increased signal within the labrum suggestive of a possible tear. Because of persistent pain and failed conservative management, the patient underwent hip arthroscopy and core decompression.
Fig 1.

(A) AP radiograph showing well-preserved joint space without evidence of collapse, cam lesion, pincer lesion, or dysplasia. (B) MRI study showing ON of anterosuperior femoral head.
The patient is positioned on the traction table with a well-padded perineal post placed in the groin between the legs (Smith & Nephew hip traction system; Smith & Nephew, Andover, MA). Traction is applied with the leg axially distracted and adducted to provide a cantilever movement to the operative hip. The greater trochanter and anterior superior iliac spine borders are marked. Under fluoroscopic visualization, a standard anterolateral (AL) portal is used 1 cm proximal and 1 cm anterior to the AL aspect of the greater trochanter. While the surgeon is viewing from the AL portal, needle localization is used to establish an anterior portal, penetrating the capsule at the 2-o'clock position. The anterior portal is approximately 1 cm lateral to a line drawn vertically from the anterior superior iliac spine and a line drawn horizontally from the AL portal.
Diagnostic arthroscopy begins with the arthroscope in the AL portal (Dyonics Arthroscopy System; Smith & Nephew). The posterosuperior and posteroinferior labrum, superior and lateral femoral head, and acetabular articular surface are evaluated for labral tears or chondral lesions. Any unstable tissue or cartilage is probed through the anterior portal to determine whether instability is present (Figs 2A and 2B). The arthroscope is then switched to the anterior portal, and the remainder of the labrum, acetabulum, and femoral head is visualized. The anterior portal is best for visualizing the anterosuperior femoral head, the most common site of ON. It provides a “birds-eye” view. The site, however, can also be visualized from the AL portal with the 70° arthroscope lens. Capsulotomy is reserved for circumstances in which labral or articular cartilage work must be performed. In this case the patient had mild degenerative fraying of the labrum with no associated delamination (Fig 2C). Therefore, a debridement of the labrum was performed through the anterior portal until a healthy rim remained.
Fig 2.
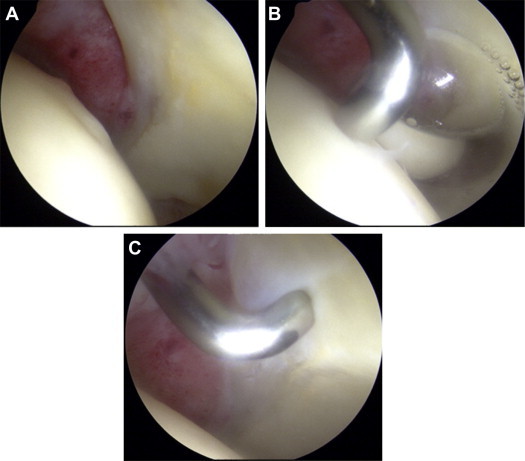
Femoral head articular surface, with visualization through AL portal. (A) Evidence of articular cartilage depression at site of ON. (B) Probing showing intact subchondral bone. (C) Degenerative fraying of labrum.
Fluoroscopic assistance confirms the location of the ON lesion. The articular surface is evaluated and probed for any depression, softening, and/or delamination. If softening or delamination is present, a chondroplasty or microfracture is performed based on the size, stability, and depth of the lesion. This is typically performed through the anterior portal while one is visualizing through the AL portal. In this case there was no evidence of either. The arthroscope is then switched back to the AL portal while any instrumentation in the anterior portal is removed to allow for adequate visualization of the femoral neck on anteroposterior (AP) and frog-leg lateral fluoroscopic views. A spinal needle is placed into the anterior portal to allow for outflow, and the pressure of the inflow is reduced to 40 mm Hg.
Core decompression is then performed through a separate 3-cm incision distal and posterior to the AL portal. This incision is localized under fluoroscopic guidance. Blunt dissection is carried down to the tensor fascia lata, which is incised longitudinally. The vastus lateralis muscle belly is elevated anteriorly to expose the proximal intertrochanteric portion of the femur. The starting point of the guide pin is based posterior to the midpoint of the proximal femur in the sagittal plane and proximal to the lesser trochanter. The trajectory is posterolateral to anteromedial to penetrate the necrotic lesion. The guide pin is advanced to 1 to 2 mm deep to the subchondral bone (Fig 3A). Appropriate positioning in the femoral head is confirmed with AP and cross-table lateral radiographs. A soft-tissue guide is placed over the guide pin, and a reamer is advanced to the same depth (Fig 3B) (Advanced Core Decompression System; Wright Medical Technology, Arlington, TN). Careful attention is paid not to allow the guide pin or reamer to advance beyond the subchondral bone. Confirmation that the reamer has penetrated the necrotic lesion is obtained fluoroscopically as well as by tactile sensation: the surgeon will feel resistance while reaming the sclerotic bone. The pin/reamer is removed, a 30° curved curette is advanced up the socket, and residual necrotic bone is removed (Fig 3C). A syringe is inserted into the socket, and a combination of calcium phosphate (CaPO4)/calcium sulfate (CaSO4) synthetic putty (PreDense; Wright Medical Technology) is injected into the socket (Fig 3D).3 Throughout each of the steps (guide pin placement, reaming, curettage, and putty placement), the arthroscope is maintained in the AL portal, focused on the articular side of the area of necrosis, to ensure that the subchondral bone and articular cartilage are not violated. The 70° arthroscope enables visualization of the articular side of the lesion so that combined fluoroscopic imaging can be performed to evaluate debridement and filling of the socket without the radiopaque arthroscope obscuring fluoroscopic visualization. Final AP and lateral fluoroscopic views are obtained verifying filling of the socket. Once the putty is cured (as evidenced on the side table), the instruments are removed from the hip and traction is released. Dynamic fluoroscopy is performed verifying joint reduction and no head penetration. The tensor fascia lata is closed with No. 0 absorbable braided suture, the dermis with No. 2-0 braided absorbable suture, and the skin (along with portals) with No. 3-0 monofilament suture. Video 1 shows the surgical technique.
Fig 3.
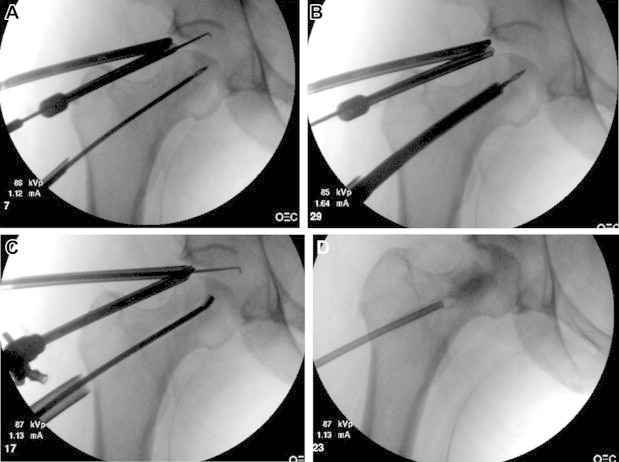
Intraoperative fluoroscopic images showing (A) guide pin placement into center of lesion, (B) introduction of reamer over pin, (C) curettage of lesion, and (D) filling of socket with calcium sulfate–calcium phosphate cement mixture.
Postoperatively, the patient was allowed touch-down weight bearing with crutches for 6 weeks. Immediate passive range of motion began the evening of surgery. At 6 weeks, the patient progressed to weight bearing as tolerated. Return to athletic activity was delayed until 3 months.
Discussion
The pathogenesis of ON of the femoral head is not fully understood but is thought to be multifactorial because of environmental and genetic factors. Common risk factors include long-term corticosteroid or alcohol use, prior trauma or slipped capital femoral epiphysis, and hypercoagulable states. Chronic conditions commonly associated with an increased incidence of ON include sickle cell disease, systemic lupus erythematosus, inflammatory bowel disease, endocrine disorders, and human immunodeficiency virus.
Several treatment options for pre-collapse ON have been described, including core decompression, vascularized bone graft, nonvascularized bone graft, cell-based treatment (stem cells, platelet rich plasma),4,5 and osteotomies.1,2 The efficacy of such techniques has not been fully elucidated because of a lack of prospective comparative data. In addition, vascularized bone grafting (e.g., free fibula transfer) requires a team of microsurgeons with significant experience to yield effective results.6 Trans-trochanteric rotational osteotomy also requires very careful planning and execution by an experienced surgeon, with the potential risk of nonunion and hardware complications. A lack of experience with such techniques can lead to undesirable outcomes. Therefore core decompression remains an accepted treatment modality for patients with pre-collapse ON of the femoral head.
Over the past 2 decades, hip arthroscopy has evolved to where it is now the gold standard for the diagnosis of intra-articular hip pathology.7 Various advances in hip-specific radiography, MRI, and computed tomography have assisted in understanding of bony and soft-tissue pathology in patients with femoroacetabular impingement and hip dysplasia. The incidence and prevalence of soft-tissue and bony intra- and extra-articular pathology with ON of the femoral head is currently not known. In addition, the ability of radiography, MRI, and computed tomography to predict collapse and/or associated hip pathology in addition to ON, at the time of surgery, is also not known. We therefore advocate that arthroscopy at the time of decompression provides the most accurate means to confirm the presence or absence of femoral head subchondral collapse, chondral delamination, and associated labral pathology (Table 2). If present, these can be addressed at the time of decompression and obviate the need for a subsequent surgery. In addition, this will allow for verification and guidance during drilling and/or reaming to prevent penetration of the articular surface.
Table 2.
Advantages and Disadvantages of Arthroscopic-Assisted Core Decompression
| Advantages | Disadvantages |
|---|---|
| Direct visualization of articular side of lesion | Risks of hip distraction
|
| Evaluation of cartilage integrity | Capsular-related morbidity (i.e., iatrogenic instability) |
| Address concomitant pathology: labral tear and pincer and/or cam lesion | Risk of iatrogenic cartilage injury |
| Confirmation of drilling/reaming into lesion | |
| Avoidance of joint penetration |
Hip arthroscopy, however, is not a procedure without associated complications (Table 2). A recent meta-analysis showed an overall 4% complication rate.8 Complications include, but are not limited to, perineal skin breakdown, nerve palsy, vascular injury, instability, compartment syndrome, hematoma, portal instrument breakage, and infection.8-10 Such complications can be minimized if the procedure is performed by a well-experienced surgeon. The risks and benefits of arthroscopy at the time of decompression need to be weighed with the patient. In circumstances in which a patient has superimposed cam- or pincer-type femoroacetabular impingement, the benefit of combined arthroscopy and decompression may outweigh the risks.
In conclusion, arthroscopically assisted core decompression of the femoral head for pre-collapse ON provides the added advantage of intra-articular visualization to confirm the diagnosis, allow for treatment of associated bony and soft-tissue pathology, and avoid the risk of joint penetration in carefully selected patients.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.C.M. is a consultant for Pivot Medical and KNG Health Consulting and holds stock options with For. S.J.N. is a consultant for, receives royalties from, and receives research support from Pivot Medical, Stryker, and AlloSource.
Supplementary Data
Arthroscopic visualization of femoral head lesion. Concomitant pathology, including articular cartilage loss and labral- and/or acetabular-sided bony rim morphology, is addressed concomitantly. Once intra-articular pathology is addressed, a fluoroscopically guided open core decompression of the osteonecrotic lesion is performed. Intra-articular arthroscopic visualization is maintained during this process.
References
- 1.Mont M.A., Carbone J.J., Fairbank A.C. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res. 1996;(324):169–178. doi: 10.1097/00003086-199603000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Marker D.R., Seyler T.M., Ulrich S.D., Srivastava S., Mont M.A. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;(466):1093–1103. doi: 10.1007/s11999-008-0184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Civinini R., De Biase P., Carulli C. The use of an injectable calcium sulphate/calcium phosphate bioceramic in the treatment of osteonecrosis of the femoral head. Int Orthop. 2012;36:1583–1588. doi: 10.1007/s00264-012-1525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao D., Cui D., Wang B. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone. 2012;50:325–330. doi: 10.1016/j.bone.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Guadilla J., Fiz N., Andia I., Sánchez M. Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip. Knee Surg Sports Traumatol Arthrosc. 2012;20:393–398. doi: 10.1007/s00167-011-1587-9. [DOI] [PubMed] [Google Scholar]
- 6.Gaskill T.R., Urbaniak J.R., Aldridge J.M., III Free vascularized fibular transfer for femoral head osteonecrosis: Donor and graft site morbidity. J Bone Joint Surg Am. 2009;91:1861–1867. doi: 10.2106/JBJS.H.01105. [DOI] [PubMed] [Google Scholar]
- 7.Kelly B.T., Williams R.J., III, Philippon M.J. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 8.Kowalczuk M., Bhandari M., Farrokhyar F. Complications following hip arthroscopy: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1669–1675. doi: 10.1007/s00167-012-2184-2. [DOI] [PubMed] [Google Scholar]
- 9.Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: Complications in 1054 cases. Clin Orthop Relat Res. 2003;(406):84–88. doi: 10.1097/01.blo.0000043048.84315.af. [DOI] [PubMed] [Google Scholar]
- 10.Harris J.D., McCormick F., Abrams G.D. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic visualization of femoral head lesion. Concomitant pathology, including articular cartilage loss and labral- and/or acetabular-sided bony rim morphology, is addressed concomitantly. Once intra-articular pathology is addressed, a fluoroscopically guided open core decompression of the osteonecrotic lesion is performed. Intra-articular arthroscopic visualization is maintained during this process.


