Abstract
In addition to operative intervention for the patient with recurrent shoulder instability, current literature suggests that younger athletic patients unwilling to modify their activities may benefit from an early surgical shoulder stabilization procedure. Although open shoulder stabilization clearly has a role to play in some cases, we believe that further optimization of arthroscopic fixation techniques may allow us to continue to refine the indications for open stabilization. In particular, when an arthroscopic approach is used for capsulolabral repair in relatively high-risk groups, it may be beneficial to use a double-row repair technique. We describe our technique for shoulder stabilization through double-row capsulolabral repair of a soft-tissue Bankart lesion in the high-risk patient with shoulder instability or the patient with a small osseous Bankart lesion.
The glenohumeral joint is the most common major joint to dislocate, at a rate of 11.2 per 100,000 persons per year.1,2 More than 90% of traumatic shoulder dislocations are anterior. Biomechanical and clinical studies have shown that traumatic dislocation or subluxation of the shoulder leads to anteroinferior capsulolabral detachment from the glenoid—the Bankart lesion.1 Although many patients may be managed nonoperatively, the overall challenge with this condition is the high rate of recurrence, particularly among younger patients.1-3 For example, in the athletic population aged younger than 20 years, recurrent dislocation rates have been reported to be as high as 90%.3 Therefore, in addition to operative intervention for the patient with recurrent instability, current literature suggests that younger athletic patients unwilling to modify their activities may benefit from a stabilization procedure after their initial dislocation in an effort to reduce the chance of recurrent instability.3 This is particularly the case for young male athletes involved in contact sports.4
At present, the role of arthroscopic versus open approaches to shoulder stabilization remains undefined. The risk factors associated with failure (recurrent instability or functional issues) after arthroscopic repair include the following: age, sex, presence of osseous Bankart and/or large Hill-Sachs lesions, competitive sports, collision or forced overhead sports, hypermobility, and number of instability episodes before surgery.5-8 Given this range of risk factors, there has been a shift toward more open stabilization procedures being performed in patients who do not have significant bone lesions but are otherwise regarded as being at high risk for failure of an arthroscopic approach to stabilization. However, although open stabilization clearly has a role to play in some cases (e.g., presence of any significant osseous lesion, poor-quality tissue, or some revision settings), we believe that further optimization of arthroscopic fixation techniques may allow us to continue to refine the indications for open stabilization. In particular, when an arthroscopic approach is used for capsulolabral repair in relatively high-risk groups, it may be best to use a double-row repair technique. It has previously been noted that arthroscopic techniques place an emphasis on re-creating the labral bumper effect by placing anchors on the glenoid articular surface but without attempting to restore the normal insertional anatomy.9 Cadaveric studies have shown that double-row capsulolabral fixation, on the other hand, may better restore normal anatomy than that which occurs with the current arthroscopic standard of single-row fixation.9-11 Arthroscopic approaches to shoulder stabilization may possibly benefit from applying these principles in the clinical setting. We describe our technique for shoulder stabilization through double-row capsulolabral repair of a soft-tissue Bankart lesion in the high-risk patient or the patient with a small osseous Bankart lesion (Tables 1-3).
Table 1.
Key Points of Procedure
| 1. Mark portal sites (anterosuperior, anteroinferior, and posterior). |
| 2. Measure 3 cm inferior to coracoid (safe zone for percutaneous access). |
| 3. Perform examination with patient under anesthesia. |
| 4. Perform arthroscopic assessment with 30° and 70° lenses. |
| 5. Place bump for inferior joint access. |
| 6a. For acute tear, prepare footprint with mechanical shaver. |
| 6b. For chronic tear, elevate sharply with Samurai blade; then prepare footprint with mechanical shaver. |
| 6c. For osseous Bankart, elevate and assess size of bony fragment. |
| 7. Place percutaneous long needle—stay lateral to conjoined tendon. |
| 8. Shuttle guidewires and drill cannula. |
| 9. Identify location sites for medial-row anchors 10 to 15 mm medial to articular surface of glenoid. (Use two to four 2.4-mm BioComposite SutureTak anchors.) |
| 10. View from posterior or anterosuperior portals with 70° and 30° lenses. |
| 11. Place each anchor without removing drill guide—inferior to superior. |
| 12. Pass sutures from medial row using “outside-in” or “inside-out” technique. |
| 13. Prepare sutures on knotless anchors for lateral-row fixation. (Use 3 to 4 BioComposite PushLock anchors, 2.9 × 15.5 mm.) |
| 14. Inspect finished repair from anterosuperior and posterior portals using both 30° and 70° lenses. |
| 15. Inspect subacromial space. |
Table 2.
Indications and Contraindications (Relative)
| Indications |
| Young, male contact athletes with recurrent instability and athletes without significant bone loss (25% glenoid width, large Hill-Sachs lesion or engaging lesion) |
| Contraindications |
| Patients with shoulder instability in the presence of significant bone defects or poor-quality tissue; revision surgery in contact athletes |
Table 3.
Pearls
| Careful arthroscopic evaluation and sizing of glenoid and Hill-Sachs lesion, as well as dynamic engagement of any lesions present |
| Use of both 30° and 70° arthroscopic lenses |
| Elevation of Bankart lesion with Samurai Blade |
| Careful attention to suture management and appropriate portal placement |
| Use of needle to percutaneously localize ideal anchor insertion site and approach angle |
Clinical Presentation
Our case example is a 30-year-old man who presented with recurrent left shoulder instability. He had his initial dislocation when he was aged 16 years while playing football. Subsequently, he had 25 more instability episodes that were self-reduced. His physical examination showed significant guarding beyond 130° of forward elevation and 45° of external rotation. Load-and-shift tests were unable to be obtained because of guarding. Radiographs showed a large Hill-Sachs lesion, as well as periosteal elevation along the anterior glenoid neck (Fig 1A). Magnetic resonance imaging showed a Hill-Sachs lesion with marrow edema and a large area of capsulolabral avulsion (Fig 1B). The computed tomography scan showed an osseous Bankart lesion that comprised less than 20% of the articular surface (Fig 1C). A double-row arthroscopic capsular shift was performed. This is detailed in the “Surgical Technique” section, but in summary, the repair construct consisted of 2 BioComposite 2.4 × 12–mm SutureTak anchors (Arthrex, Naples, FL) for the medial row and 2 BioComposite 2.9 × 15.5–mm PushLock anchors (Arthrex) for the lateral row. The patient has done well in his postoperative course and was most recently seen for a 3-month postoperative visit. He was pain free, and his examination showed negative apprehension, intact motor strength, and a full range of shoulder motion without pain. He is now working toward returning to recreational sports, including mixed martial arts, after the sixth postoperative month.
Fig 1.

Example of a case suitable for double-row capsulolabral repair. (A) Internally rotated anteroposterior view of a left shoulder showing a large Hill-Sachs lesion with concomitant periosteal elevation along the anterior glenoid neck. (B) Axial proton density magnetic resonance image of a left shoulder showing a large Hill-Sachs lesion along with a large area of anterior capsulolabral avulsion. (C) Axial, sagittal, and 3-dimensionally reconstructed computed tomography scans of a left shoulder showing an osseous Bankart lesion comprising less than 20% of the glenoid articular surface.
Surgical Technique
Setup and Examination Under Anesthesia
Regional anesthesia is used in all patients. The patient is positioned in the beach-chair position with the use of a beanbag and secured on the operating table (Fig 2A). Shoulder stability and range of motion with the patient under anesthesia are evaluated before arthroscopy (Fig 2B). The arm is then set up in a pneumatic arm holder (Trimano; Arthrex) for the arthroscopic component of the procedure. A bump is prepared to be placed in the axilla after the initial diagnostic arthroscopy to enhance the arthroscopic working space of the glenohumeral joint by providing joint distraction in conjunction with the pneumatic arm holder (Fig 2C).
Fig 2.
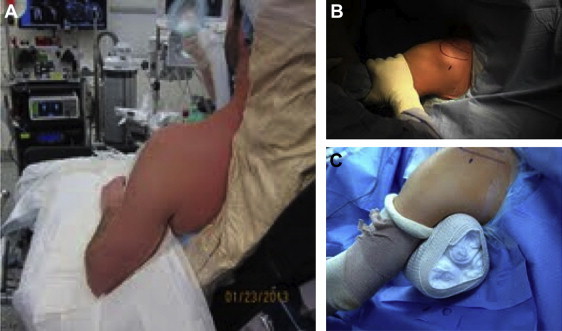
Setup and examination under anesthesia. (A) The patient is placed in the standard beach-chair (modified Fowler) position using a beanbag extending to the medial border of the scapula for support. (B) After surgical preparation and draping, an examination under anesthesia is performed, including range-of-motion and stability testing (e.g., load-and-shift test). (C) A bump is constructed, placed in the axilla after the initial diagnostic arthroscopy, and in conjunction with the pneumatic arm holder, provides distraction at the glenohumeral joint and enhances the arthroscopic working space.
Diagnostic Arthroscopy
Anatomic landmarks of the shoulder are identified and marked, along with portal sites (Fig 3). The markings include the anterior, anterosuperior (rotator interval), anterolateral, and lateral portals. In addition, a mark is made 3 cm inferior to the coracoid, indicating the safe zone for percutaneous placement of the medial-row anchors. A standard posterior portal is established, and a systematic, diagnostic arthroscopic examination of the glenohumeral joint is performed in all cases through this portal by use of a 30° lens followed by a 70° lens. The condition of the anterior labrum, glenoid, humeral head, and capsular tissue is evaluated. A high anterior-superior rotator interval portal is established from outside to inside with a 5-mm cannula. An arthroscopic 3-mm probe is introduced through this portal, and all structures are probed. Volume measurement of any Hill-Sachs lesions is then performed, and the glenoid is evaluated for any bone loss. The extent of the labral tear is recorded based on a clock-face model, with 12 o'clock being superior and 6 o'clock inferior. The tear is graded based on the number of hour segments affected. The surgeon then establishes a working accessory anteroinferior portal, entering the glenohumeral joint just above the subscapularis muscle. An 8.5-mm cannula is used in this portal to aid with instrument passage and suture management. A bump is then placed to allow for improved access to the inferior aspect of the labrum. In the acute situation, the anterior glenoid bony surface can be prepared with a mechanical shaver to debride any remaining soft tissue and create a bed of bleeding bone to enhance later union between the repaired capsulolabral complex and the glenoid neck. In the chronic situation, the detached anterior labrum is elevated sharply with a Samurai Blade (Pivot Medical, Sunnyvale, CA) until the fibers of the subscapularis muscle are visualized (Fig 4). In this manner a sleeve of continuous tissue is elevated off the glenoid neck inferiorly as far as the 6-o'clock position (or beyond in the case of posterior extension of the tear). An arthroscopic shaver is then used to prepare the anterior glenoid surface. If a small osseous Bankart lesion is present, this is mobilized with the attached capsulolabral tissue. The shoulder is then positioned in 45° of external rotation or more (depending on the sport/position of the athlete) before fixation to prevent over-tightening during the stabilization.
Fig 3.

The surface anatomy (clavicle, acromion, and coracoid) and potential portal sites are marked. From medial to lateral, the portal sites are anterior, anterosuperior (rotator interval), anterolateral, and lateral.
Fig 4.

View of left shoulder through posterior portal in beach-chair position. Elevation of the osseous fragment is performed with the Samurai Blade. In the event that an osseous fragment is identified, the Samurai Blade is used to begin mobilization and develop the plane between the fragment and the remaining glenoid.
Arthroscopic Double-Row Labral Repair
The capsulolabral defect is repaired with a double-row technique. The medial 2.4-mm BioComposite SutureTak anchors (Arthrex) are placed by use of an anterior percutaneous deployment device. During placement of the anchors, the medial row can be viewed from either the anterosuperior or posterior portal using either the 30° or 70° lens. A distance of 3 cm is measured from the tip of the coracoid to avoid percutaneous damage to the musculocutaneous nerve. A needle is then used to percutaneously localize the ideal anchor insertion site and approach angle. The anchor insertion site is approximately 10 to 15 mm medial to the articular surface of the glenoid and lateral to the conjoined tendon. A guidewire is then passed through the needle, followed by removal of the needle and subsequent placement of a dilator and a common guide for both the drill and anchor over the guidewire. The guidewire is removed, and the common drill and anchor guide remains in position throughout this portion of the procedure until all of the anchors are placed from inferior to superior. Keeping the drill guide in the field until all the anchors are placed is a key part of the procedure because correct and safe anchor placement of the medial anchors can be technically challenging using alternative techniques8-10; moreover, the risk of musculocutaneous nerve injury can be minimized by performing only 1 percutaneous puncture. If necessary, the capsulolabral complex may be maintained in an elevated position off the glenoid neck with an elevator passed from the anterosuperior portal to facilitate medial anchor placement. Depending on the size of the defect, 2 to 4 medial anchors are used (Fig 5A). A shuttling technique with a 25° curved SutureLasso (Arthrex) placed through the anteroinferior working portal and then through the medial capsule is used to retrieve the sutures, 1 at a time, from the medial anchors. They are typically brought from inside to outside through separate points in the capsule before being brought out the anteroinferior cannula. Suture management is then optimized by use of a suture claw to bring the pair of suture limbs from each medial anchor—now also passing from in to out through the medial capsule—up and out the anterosuperior portal, where they are parked until lateral fixation is performed. The double-row construct is completed by inserting the medial-row sutures into knotless BioComposite PushLock anchors for lateral-row fixation (Figs 5B and 5C). Approximately 3 to 4 PushLock anchors can be used for the lateral row. The lateral row of anchors is placed approximately 2 mm onto the anterior lip of the glenoid with a medial inclination of approximately 45°. The 2 free limbs from each medial suture anchor are fed into a single lateral PushLock anchor. A superior capsular shift with tensioning of the inferior glenohumeral ligament is performed before fixation of the lateral anchor. This provides a suture-bridge repair of the capsulolabral defect with 2-point fixation. The free limbs are cut flush with the PushLock anchor after lateral fixation. If an osseous Bankart lesion is present, it is usually repaired by the same technique (incorporated into the double-row construct) provided that it is amenable to arthroscopic repair and less than 25% of the glenoid width. The lesion is therefore repaired anatomically between the medial and lateral rows of suture anchors. This has the added benefit of the osseous component being compressed and reduced into the fracture bed on the anteroinferior glenoid.
Fig 5.
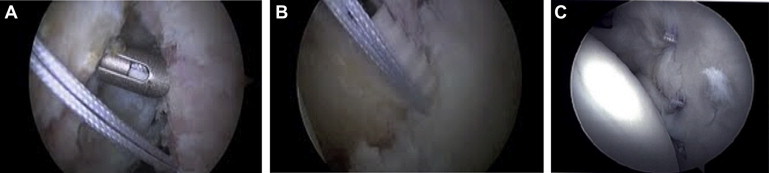
View of left shoulder through posterior portal in beach-chair position. Anchor placement takes place in 2 stages, after one determines the desired configuration. First, (A) the medial row is placed (2.4-mm BioComposite SutureTak), passed through the capsulolabral fragment by use of a 25° curved SutureLasso, and (B) tensioned through the lateral-row anchors (BioComposite PushLock anchors, 2.9 × 15.5 mm). (C) Final inspection shows an anatomic reconstruction.
The final repair construct is inspected from both the posterior and anterosuperior portals using both the 30° and 70° lenses. The subacromial space is also inspected before closure. The entire technique can be viewed in Video 1.
Postoperative Treatment and Rehabilitation
A detailed, supervised physical therapy program is initiated postoperatively. After 3 weeks of immobilization, active-assisted range of motion in the plane of the scapula is progressed to 90°. Active-assisted external rotation is progressed to 25°. Patients wear an immobilizer in internal rotation at all times when not exercising.
At 4 weeks, the immobilizer is discontinued and active-assisted range of motion is progressed in forward flexion and external rotation. From weeks 6 to 12, gradual strengthening is added.
At 12 weeks, upper extremity flexibility and strengthening are continued. Plyometrics, closed-chain strengthening, and proprioceptive exercises are initiated. Sports- or activity-related programs begin and are progressed. A full return to sports is considered after 6 months and predicated on the achievement of previous benchmarks and goals.
Discussion
Recent literature suggests that the outcomes of arthroscopic stabilization approach those of open stabilization in appropriately selected patients.12 Arthroscopic approaches avoid the risk of catastrophic rupture of a subscapularis repair, reduce operative time, improve cosmesis, and are associated with a more normal range of motion postoperatively. Single-row suture anchor constructs have become the preferred methodology for fixation during arthroscopic shoulder stabilization, typically repairing the labrum back to the glenoid rim with point fixation at each anchor.9,12 However, young male patients, contact athletes, and patients who have had a large number of dislocations may be regarded as high-risk populations that may benefit from a more secure anatomic reconstruction than that afforded by traditional arthroscopic single-row stabilization techniques.3-8 Although some surgeons prefer an open approach when performing stabilization procedures in these patients, further optimization of arthroscopic repair techniques with careful attention to the capsulolabral footprint and appropriate selection of cases may allow surgeons to continue to limit the indications for open surgery. Before applying this technique in the arthroscopic setting, we performed it through an open approach.
In a cadaveric study, Ahmad et al.9 found that the mean surface area of the native capsulolabral complex footprint was 256 ± 40 mm2, whereas the native footprint of the labrum was 152.3 ± 24.4 mm2. Therefore the labrum attachment comprised 59% of the overall capsulolabral complex. The mean surface area of the single-row repair was 108 ± 27 mm2, whereas that of the double-row repair was 220 ± 39 mm2. This represented 42% and 86% re-creation of the native capsulolabral complex footprint surface area for single- and double-row repairs, respectively. Thus the double-row repair was 103.3% larger than the single-row repair. The native capsulolabral complex footprint surface area was significantly larger than that of either the single- or double-row repair (P < .01 for both), and the double-row repair was significantly larger and re-created more of the native footprint than the single-row repair (P < .01). Kim et al.10 also looked at single-row versus double-row capsulolabral repair in a cadaveric model. They performed a comparative evaluation of contact pressure and surface area at the capsulolabral complex–glenoid bone interface. Instead of computer digitalization as used in the study of Ahmad et al., their study directly measured interface pressure and contact area and observed contact patterns using pressure-sensitive film. In the study of Kim et al., the double-row repair had a significantly higher interface pressure and contact area than the single-row repair. Re-creations of the defined insertion footprint areas based on pressure-sensitive film dimensions were 39.4% for the single-row repair group and 78.4% for the double-row repair group. In addition, regarding contact patterns, the single-row repair produced the shape of a thin line distributed along the anterior glenoid rim and the double-row repair showed a wide band distributed along a significant glenoid bony surface. These cadaveric studies suggest that a double-row repair technique restores a greater percentage of the anatomic footprint than a single-row repair.
Other techniques for double-row repair have also been described. Lafosse et al.12 reported a technique of double-row labral repair, which was performed arthroscopically in 12 patients. They described a double-row fixation technique with 2 suture anchors on the glenoid neck and 3 on the glenoid rim (a W-shaped form resembling the star constellation of Cassiopeia). However, for insertion into the exact position of the medial suture anchors used in that study, it is essential to make a very inferior and medial anterior portal through the subscapularis tendon. When one is using this portal, the neurovascular structures are potentially at greater risk. Furthermore, with an asymmetric number of anchors medially and laterally, diverting suture limbs from 1 medial-row anchor to 2 lateral-row anchors leads to more complex suture management and construct tensioning, which we have found to be less predictable (Fig 6A). In another study Iwaso et al.13 described a series of patients (mean age, 25 years; age range, 17 to 30 years; 12 male and 6 female patients) undergoing a double-row technique with knotless anchors and sutures placed in a V-shaped pattern. They noted no recurrence of dislocation or subluxation in 19 joints followed for 24 months or longer. Millett and Braun14 described a similar technique for fixation of bony Bankart lesions. In their technique a suture anchor is placed medially to the fracture on the glenoid neck, and its sutures are passed around the bony fragment through the soft tissue including the inferior glenohumeral ligament complex.10 The sutures of this anchor are loaded in a second anchor that is placed on the glenoid face. The technique we describe differs from the previously described methods because it is based on percutaneous placement of the medial row of anchors and a 1-to-1 relation between the medial and lateral rows of anchors (Fig 6B). This configuration allows for easier suture management and more consistent suture tensioning (both limbs from each medial-row anchor converge and are tensioned in a single lateral-row anchor), in a manner that we believe is more predictable and less technically demanding than those described earlier.
Fig 6.
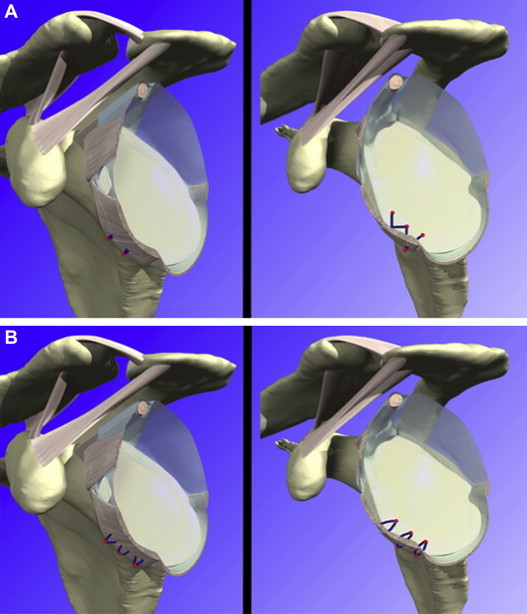
Suture anchor configuration patterns. (A) The Cassiopeia (“W”) divergent technique uses an asymmetric number of anchors (1 more laterally than medially), and the suture limbs diverge from a single point in the capsule to 2 different anchors in the lateral row. (B) The convergent (“M”) technique uses a symmetric number of anchors medially and laterally, and the suture limbs converge to a single medial-row anchor, through 2 different points in the capsule, and converge to a single lateral-row anchor. By use of a 1:1 anchor configuration, suture management and tensioning are more predictable and straightforward.
(Reprinted with permission of Primal Pictures Ltd.)
The double-row suture-bridge technique for repair of soft-tissue Bankart lesions combines the advantages of arthroscopic Bankart repair with its ability to improve the anatomic reconstruction of the capsulolabral complex. Limitations of the procedure relate to appropriate patient selection. Those patients who have significant bone loss, who have poor-quality tissue, or are undergoing a revision surgical stabilization will still likely benefit from an open approach. The risk profile of the procedure is similar to that of traditional single-row capsulolabral repair. We have found this technique to be reproducible, with very predictable and straightforward suture management and tensioning, and believe that it may have a role to play in the treatment of shoulder instability in high-risk athletes without significant bone loss or other related pathology.
Footnotes
The authors report the following potential conflict of interest or source of funding: F.A.C. receives royalties from CONMED Linvatec and is a consultant for Arthrex, Inc.
Supplementary Data
Arthroscopic double-row capsulolabral repair.
References
- 1.Dodson C.C., Cordasco F.A. Anterior glenohumeral joint dislocations. Orthop Clin North Am. 2008;39:507–518. doi: 10.1016/j.ocl.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Marans H.J., Angel K.R., Schemitsch E.H., Wedge J.H. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg Am. 1992;74:1242–1244. [PubMed] [Google Scholar]
- 3.Brophy R.H., Marx R.G. The treatment of traumatic anterior instability of the shoulder: Nonoperative and surgical treatment. Arthroscopy. 2009;25:298–304. doi: 10.1016/j.arthro.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Balg F., Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 5.Porcellini G., Campi F., Pegreffi F., Castagna A., Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009;91:2537–2542. doi: 10.2106/JBJS.H.01126. [DOI] [PubMed] [Google Scholar]
- 6.Voos J.E., Livermore R.W., Feeley B.T. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 7.Castagna A., Delle Rose G., Borroni M. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy. 2012;28:309–315. doi: 10.1016/j.arthro.2011.08.302. [DOI] [PubMed] [Google Scholar]
- 8.Wasserstein D., Dwyer T., Veillette C. Predictors of dislocation and revision after shoulder stabilization in Ontario, Canada, from 2003 to 2008. Am J Sports Med. 2013;41:2034–2040. doi: 10.1177/0363546513492952. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad C.S., Galano G.J., Vorys G.C., Covey A.S., Gardner T.R., Levine W.N. Evaluation of glenoid capsulolabral complex insertional anatomy and restoration with single- and double-row capsulolabral repairs. J Shoulder Elbow Surg. 2009;18:948–954. doi: 10.1016/j.jse.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Kim D.S., Yoon Y.S., Chung H.J. Single-row versus double-row capsulolabral repair: A comparative evaluation of contact pressure and surface area in the capsulolabral complex-glenoid bone interface. Am J Sports Med. 2011;39:1500–1506. doi: 10.1177/0363546511399863. [DOI] [PubMed] [Google Scholar]
- 11.Tjoumakaris F.P., Bradley J.P. The rationale for an arthroscopic approach to shoulder stabilization. Arthroscopy. 2011;27:1422–1433. doi: 10.1016/j.arthro.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Lafosse L., Baier G.P., Jost B. Footprint fixation for arthroscopic reconstruction in anterior shoulder instability: The Cassiopeia double-row technique. Arthroscopy. 2006;22:231.e1–231.e6. doi: 10.1016/j.arthro.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Iwaso H., Uchiyama E., Sakakibara S., Fukui N. Modified double-row technique for arthroscopic Bankart repair: Surgical technique and preliminary results. Acta Orthop Belg. 2011;77:252–257. [PubMed] [Google Scholar]
- 14.Millett P.J., Braun S. The “bony Bankart bridge” procedure: A new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy. 2009;25:102–105. doi: 10.1016/j.arthro.2008.07.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic double-row capsulolabral repair.


