Abstract
Background
The objective of this study was to identify important attributes associated with the triad of symptoms (cognition, emotional–behavioral, and motor) of Huntington's disease (HD) from patient, caregiver, and medical provider perspectives to facilitate development of a new disease-specific, health-related quality of life (HRQOL) instrument.
Methods
We conducted a targeted literature review of HD and HRQOL instruments, expert surveys, and patient and caregiver phone-based interviews to extract information on the symptoms and issues most relevant to the HD symptom triad (HD triad). The data collected from these sources were used to generate themes and subdomains and to develop an integrated schema that highlights the key dimensions of the triad.
Results
The search identified the following areas: emotional functioning/behavioral changes (e.g., positive emotions, sadness/depression); cognitive functioning (e.g., memory/learning, attention/comprehension); physical functioning (e.g., motor functioning, medication); social functioning (e.g., leisure, interpersonal relationships); end-of-life concerns/planning; and gene testing. Fifteen individuals diagnosed with HD and 16 HD caregivers, recruited from several Huntington's Disease Society of America support group networks, completed phone interviews. Nineteen US medical providers who specialize in HD completed the online survey. Twenty-six subdomains of the HD symptom triad (seven cognition, 12 emotional–behavioral, and seven motor) emerged relatively consistently across patient, caregiver, and provider samples. These included movements/chorea, memory impairment, depression, and anxiety.
Discussion
Based on an integrated, mixed-methods approach, important HD triad symptom were identified and organized into a guiding schema. These patient-, caregiver-, and provider-triangulated data served as the basis for development of a HD-specific HRQOL instrument, the HD-PRO-TRIAD™.
Keywords: Huntington's disease, quality-of-life scale, psychometric validation, patient-reported outcome, health-related quality of life, HD-PRO-TRIAD™
Introduction
Huntington's disease (HD) is a rare, autosomal dominant, neurologic disorder that affects approximately three in 100,000 individuals worldwide.1 HD is caused by a CAG trinucleotide repeat expansion in the gene encoding the huntingtin protein on the short side of chromosome 4, with affected individuals having at least one allele with 36 or more repeats.2 HD symptoms typically begin subtly and gradually worsen, generally leading to a clinical diagnosis of HD near the age of 40 years, though age of symptom onset is associated with the number of expansions in the longest HD allele.3 Death usually occurs approximately 20 years after initial diagnosis.4
HD is characterized by a triad of insidious and progressive cognitive, emotional–behavioral, and motor symptoms5 (hereafter referred to as the “HD triad”). The symptom presentation for any given individual can include one or all of the HD triad domains. Cognitive symptoms can include forgetfulness, attention difficulties, executive dysfunction, and, at the later stages, dementia.6–9 Emotional–behavioral symptoms may include apathy, depression, aggression, disinhibition, anxiety, and perseverative behaviors.9,10 Motor symptoms generally include chorea, bradykinesia, ataxia, and dystonia.9 In addition to the difficulties associated with the symptoms themselves, the HD triad can have a negative impact on family functioning, other social relationships, and the ability of the patient to work. As a result, HD has a substantial deleterious effect on health-related quality of life (HRQOL).11–13
Recent studies have examined the broader impact of HD on global areas of HRQOL, such as emotional, physical, cognitive, and social health.13–15 Carlozzi et al.13 conducted a series of focus groups with individuals at risk for and with prodromal or symptomatic HD, as well as caregivers and clinical providers for patients with HD, to identify the most important aspects of HD-specific HRQOL. Overall, they reported that emotional, social, and physical areas were discussed relatively evenly across groups (between 26% and 28%), while cognitive health and end-of-life issues were discussed less frequently (9–10%).13
Two HD-specific HRQOL instruments were recently published. The first was based on semi-structured interviews with individuals with pre-symptomatic through late stage HD.15 Findings from these interviews were used to develop the Huntington's Disease Quality of Life questionnaire, a new measure of global HRQOL in HD that focuses on cognitive, emotional, physical, and functional aspects of HD. The second emerged from a European study that employed French and Italian self-reported questionnaires to develop a Huntington Quality of Life Instrument (H-QoL-I) composed of three domains: motor, psychology, and socializing.16
While aspects of the HD triad were explored during development of the two existing HRQOL measures, neither study spanned the HD triad and specifically focused on their direct implications. In other words, they did not fully cover the full HD triad of cognitive, emotional–behavioral, and motor symptoms. The study presented here collected findings from an expert survey and semi-structured patient and caregiver interviews designed to explore the HD symptom triad (HD triad), its impact, and how it may inform new outcome measurement tools. These data were used to design a HD-specific patient-rated outcome (PRO) scale (HD-PRO-TRIAD™) to assess the impacts of the HD triad on HRQOL.17
Methods
A grounded theory qualitative research approach was used to gather data on patient, caregiver, and medical provider experiences with HD triad symptomatology and derive a conceptual understanding of the grounded views of those affected by the HD triad.18 Consistent with this approach, several stages of data collection and modification were employed, each characterized by constant comparison of data with emergent themes and purposive sampling of different perspectives. This included a targeted literature review, expert surveys, and individual phone-based interviews with HD patients and their caregivers. The study was approved by the Northwestern University Institutional Review Board.
Targeted literature review
A literature search via PubMed/MEDLINE was conducted to identify important HRQOL domains commonly associated with the HD triad. The search identified the following areas: emotional functioning/behavioral changes (positive emotions, sadness/depression, anxiety/fear, anger, self-esteem, and behavioral changes); cognitive functioning (memory/learning, attention/comprehension, executive functioning, and orientation); physical functioning (motor functioning, medication, fatigue, vision changes, sexual functioning, and health promotion); social functioning (leisure, interpersonal relationships, and vocation); end-of-life concerns/planning; and gene testing. These domains were subsequently used as the basis for the development of individual interview guides with patients and caregivers, and expert surveys.
Expert surveys
An online survey for HD medical providers and key opinion leaders was developed after the extensive targeted literature review of HRQOL issues associated with HD and current measures that assess HD-related HRQOL. The survey was hosted online and sought to obtain insights regarding the HD triad of symptoms and their impacts on HRQOL. Experts were asked to free-list cognitive, emotional–behavioral, and motor symptoms issues or concerns that patients with HD experience, and rate their importance and prevalence based on a 4-point Likert scale (1 = not at all common/important to 4 = extremely common/important). Similarly, they were also asked to rate the prevalence and relevance of a list of pre-generated HD triad issues based on the literature review. All data were entered into a relational database and summarized into themes by three study team members (N.C., C.N., A.M.) with qualitative data analysis experience.
Patient and caregiver individual phone-based interviews
Individual telephone-based interviews were conducted to explore the most important issues related to the HD triad, including global life changes, symptoms, adverse effects, and ways of coping. Patients and caregivers were invited to participate through HD Lighthouse and Huntington's Disease Society of America (HDSA) support groups representing California, Texas, New York, Florida, and Illinois. These regions were chosen to ensure a broad US geographic sample distribution and because they offered relatively greater numbers of support groups. Patients were eligible to participate if they met the following inclusion criteria: a) diagnosed with HD; b) ≥18 years of age; c) able to actively participate in an individual phone-based interview; and (d) able to read, write, speak, and understand English. Caregivers were eligible if they self-identified as a caregiver for someone diagnosed with HD. (However, not all caregivers were actively caring for someone with HD. In a few instances, caregivers had cared for family members with HD who had died before the interviews.) General exclusion criteria included: a) physical debilitation such that study participation in an individual interview would not be feasible or would create undue hardship; and b) history of diagnosed severe mental illness or hospitalization for chronic psychiatric reasons.
Interested patients and caregivers provided consent and were called by trained research coordinators to schedule a recorded telephone interview. One week prior to the individual interviews, the research coordinators telephoned participants to remind them of the dates and times. Participants mailed signed consent forms via prepaid return postage sent by the research coordinators prior to the interviews.
As part of the registration process, all participants were asked to complete a demographics form (returned via post with the consent form). This information was summarized to provide a description of sample participant demographics. By tracking participant characteristics throughout the registration process, we modified recruitment as needed to include patients with under-represented attributes, ensuring a sample that accurately reflected the general HD patient population.
Interviews were conducted by trained research team members who followed a semi-structured moderator's guide, which had been developed from guides used in similar previously conducted NIH-funded studies.19 At the conclusion of the individual interviews, participants received a $35 incentive in the form of a gift card. All individual interviews were audio-recorded, and notes taken by the moderator were also recorded within 60 minutes. Digital recordings of the interviews were transcribed verbatim via a professional transcription service. All identifying patient information was excluded from these transcripts.
Analysis
Expert survey and interview response transcriptions and moderator notes were read and examined systematically by at least two study team members (DV, NC) to obtain a general impression of the data, which, supplemented with current literature, allowed two additional raters (C.N., A.M.) to independently generate a mutually agreed upon list of themes and dimensions of major ideas. Through multiple raters, variance was reduced, lending a greater degree of credibility to the analysis. Through open and selective coding approaches and constant comparative methods, an iterative coding process was employed to create coding definitions and rules and, thus, identify and organize common themes. Comments were organized into codes and larger themes, and frequency tables were created to reflect the number of times a given code was applied compared with the rest of the codes. The point of reaching data saturation was noted as patient records were sequentially evaluated. Inter-rater reliability was assessed following the development of the initial code book.
Based on analysis of themes identified from the expert surveys and individual phone-based interviews, preliminary HD-PRO-TRIADTM items were selected and compiled from relevant existing neurology-related HRQOL item banks with content appropriate for the three domains of the HD-PRO-TRIADTM instrument. To this end, cognitive functioning items were selected from the Neuro-QOL Cognition item banks20 and Traumatic Brain Injury-QOL Cognition.21,22 Emotional/behavioral functioning items were selected from the Neuro-QOL Emotional and Behavioral Dyscontrol item bank, and motor functioning items were selected from the HDQLIFE™ chorea items23 and FACIT motor items.24
Results
Expert characteristics
Nineteen medical providers participated in the online survey, all of whom reported being HD specialists. Seventeen providers (90%) were doctors of medicine, one was a registered nurse, and one was a doctor of osteopathic medicine. The majority of medical providers reported having a specialty in movement disorders and treating more than 100 HD patients per year (Table 1).
Table 1. Expert Medical Provider Characteristics (n = 19).
| Specialty in movement disorders | 84.2% |
|---|---|
| Years of practice in HD, mean (range) | 19.5 (5–35) |
| Mean number of patients with HD per year | |
| <12 | 5.3% |
| 12–49 | 31.6% |
| 50–100 | 5.3% |
| >100 | 57.9% |
| Percentage time spent in research and clinic, mean | |
| Research | 40.0% |
| Clinic | 55.3% |
HD: Huntington's disease.
Free-listed HD triad symptoms and issues
Free-listed HD triad symptoms and issues were categorized into three domains—Cognition, Emotional–Behavioral Dyscontrol, and Motor. The most frequently listed Cognition domain symptoms were executive functioning, memory, and concentration (Table 2). The most frequently listed Emotional–Behavioral Dyscontrol domain symptoms were anger, depression, and anxiety. The most frequently listed Motor domain deficits were movements (including chorea), balance, and incoordination.
Table 2. Expert-Identified HD Triad Symptoms.
| Domain | Percentage of Experts who Free-Listed Subdomain (n = 19) | Mean Likert Score1 | |
|---|---|---|---|
| Commonality among Patients | Importance for Patients | ||
| Cognitive symptoms | |||
| Executive function | 21.7% | 3.64 | 3.00 |
| Memory | 21.7% | 2.80 | 2.73 |
| Concentration | 14.5% | 2.70 | 2.50 |
| Attention | 8.7% | 3.33 | 3.00 |
| Learning | 5.8% | 3.50 | 2.75 |
| Perseveration | 5.8% | 3.00 | 2.50 |
| Decision-making | 4.4% | 3.33 | 2.67 |
| Insight/Awareness | 4.4% | 3.33 | 2.33 |
| Judgment | 4.4% | 3.00 | 2.33 |
| Adaptability | 1.4% | 2.00 | 2.00 |
| Communication | 1.4% | 3.00 | 2.00 |
| Job performance | 1.4% | 3.00 | 3.00 |
| Mental fatigue | 1.4% | 2.00 | 3.00 |
| Cognitive-related motor tasks | 1.4% | 3.00 | 3.00 |
| Slowness/Processing speed | 1.4% | 2.00 | 1.00 |
| Emotional/Behavioral Dyscontrol symptoms | |||
| Anger | 22.1% | 2.73 | 2.68 |
| Depression | 16.8% | 3.19 | 2.88 |
| Anxiety | 13.7% | 2.69 | 3.00 |
| Apathy | 8.7% | 3.00 | 2.13 |
| Obsessions/Compulsions | 7.4% | 3.00 | 2.86 |
| Impulsivity | 6.5% | 3.00 | 2.67 |
| Aggression | 4.2% | 2.50 | 3.50 |
| Psychosis | 4.2% | 2.50 | 3.25 |
| Poor coping | 2.2% | 3.50 | 3.00 |
| Behavioral problems | 1.0% | 4.00 | 4.00 |
| Personality change | 1.0% | 3.00 | 2.00 |
| Sleep problems | 1.0% | 4.00 | 3.00 |
| Stigma | 1.0% | 4.00 | 4.00 |
| Motor symptoms | |||
| Movements | 22.7% | 2.88 | 2.59 |
| Balance | 13.5% | 3.10 | 3.40 |
| Incoordination | 12.2% | 3.00 | 2.78 |
| Swallowing | 9.5% | 2.86 | 3.13 |
| Mobility/Locomotion | 8.1% | 2.83 | 2.67 |
| Speech | 8.1% | 3.17 | 2.67 |
| Falls | 6.8% | 3.80 | 4.00 |
| Rigidity | 6.8% | 3.00 | 3.20 |
| Upper extremity/ADL | 5.4% | 2.75 | 3.25 |
| Sleep | 2.7% | 2.00 | 3.00 |
| IADL | 1.4% | 3.00 | 4.00 |
| Pain | 1.4% | 2.00 | 2.00 |
| Socialization | 1.4% | 2.00 | 2.00 |
| Time extension | 1.4% | 3.00 | 4.00 |
4-point Likert scale: 1 = not at all common/important; 2 = somewhat common/important; 3 = very common/important; 4 = extremely common/important.
ADL: Activities of daily Living (e.g., bathing, dressing, eating); HD: Huntington's disease; IADL: Instrumental activities of daily living (e.g., shopping, cooking, driving, finances).
Patient and caregiver characteristics
Fifteen patients and 16 caregivers were enrolled in this study. Data from patient and caregiver interviews reflect nine independent samples of patients, 10 independent samples of caregivers, and six paired dyads. Mean age was 54 years for patients and 63 years for caregivers (Table 3). The majority of patients and caregivers interviewed were white, married, and female. Mean patient CAG trinucleotide repeat lengths reported by patients and caregivers were similar. The reported length of time with symptomatic HD was greater in caregiver reports than in patient reports (mean was 120 months based on caregiver reports vs. 92 months from patient reports), as was the percentage of patients with late-stage HD (47% caregivers vs. 15% patients).
Table 3. Patient Characteristics as Reported by Patients and Caregivers.
| Patient Characteristics | By Patients (n = 15) | By Caregivers (n = 16) |
|---|---|---|
| Age, mean (SD), years | 54.3 (13.5) | 62.9 (10.7) |
| Female | 66.7% | 56.3% |
| Hispanic | 0% | 12.5% |
| White | 100% | 100% |
| Married | 86.7% | 68.8% |
| College degree or greater | 53.4% | 50.0% |
| Unemployed | 86.7% | NA |
| Income | ||
| $40,000–$74,000 | 40.0% | 28.6% |
| ≥$75,000 | 40.0% | 64.3% |
| CAG repeat length, mean (SD) | 42 (3.1) | 45 (3.9) |
| Patient had gene testing | 92.9% | 68.8% |
| Length of HD symptoms, mean (SD), months | 92.1 (88.6) | 120.1 (76.6) |
| Self-rated HD stage | ||
| Early HD | 61.5% | 33.3% |
| Middle HD | 23.1% | 20.0% |
| Late HD | 15.4% | 46.7% |
| Self-rated health status | ||
| Fair | 6.7% | NA |
| Good | 60.0% | NA |
| Very good | 20.0% | NA |
| Excellent | 6.7% | NA |
| Relationship with patient | ||
| Spouse | NA | 50.0% |
| Parent | NA | 43.8% |
| Friend | NA | 63.0% |
| Length of relationship with patient, mean (SD), months | NA | 383.4 (170.7) |
| Length of role as caregiver, mean (SD), months | NA | 131.1 (128.3) |
HD: Huntington's disease; NA: Not applicable; SD: Standard deviation.
Patient and caregiver comments
Patients and caregivers were asked broad questions about how HD had affected their lives in general, and also about any specific experiences related to cognitive, emotional–behavioral, and motor symptoms. During the coding process, global, unspecified comments about HD triad constructs were encountered, such as, “I couldn't do the mental work” (in reference to cognition effects); “It [HD] tests your emotional skills and asks you questions about your emotional stability and all that” (in reference to emotional–behavioral effects); and “Motor skills in a lot of different things that I do are affected” (in reference to motor effects). Of the three domains (Cognition, Emotional–Behavioral Dyscontrol, and Motor), motor issues were discussed most frequently by patients and caregivers, followed by emotional–behavioral, and cognitive issues. Table 4 presents the HD triad domains and their subdomains, and the frequency with which each subdomain was reported. For a more detailed view of the issues related to the HD triad as reported by patients and caregivers, some typical passages from the transcripts are provided in the following section.
Table 4. Patient- and Caregiver-reported HD Triad Symptoms and Issues, by Domains and Subdomains.
| Code (Domain/Subdomain)1 | Frequency in Patient Reports2 | Frequency in Caregiver Reports2 |
|---|---|---|
| Cognition Domain | ||
| Perseveration | 25.6% | 47.7% |
| Memory | 32.8% | 11.4% |
| Executive functioning | 9.6% | 15.9% |
| Attention/concentration | 11.2% | 12.5% |
| Slowed processing | 12.8% | 6.8% |
| Communication | 4.8% | 2.3% |
| Awareness | 3.2% | 3.4% |
| Emotional–Behavioral Dyscontrol Domain | ||
| Anxiety | 47.9% | 31.9% |
| Depression | 37.0% | 39.7% |
| Anger/Irritability | 4.5% | 6.1% |
| Disinhibition | 1.4% | 7.4% |
| Aggression/behavioral dyscontrol | 3.9% | 3.1% |
| Emotional outbursts | 2.5% | 3.9% |
| Psychosis | 0.3% | 3.9% |
| Impulsivity | 1.1% | 0.9% |
| Apathy | 1.1% | 0.4% |
| Impatience | 0 | 1.3% |
| Legal problems | 0 | 1.3% |
| Obsessions/compulsions | 0.3% | 0 |
| Motor Domain | ||
| Chorea | 10.9% | 12.8% |
| Ambulation | 6.65% | 6.1% |
| ADL | 3.9% | 5.6% |
| Speech | 2.3% | 2.5% |
| Swallowing | 2.2% | 2.0% |
| Fatigue | 3.4% | 0.7% |
| Sleep | 0.6% | 0.8% |
Only HD triad-specific codes are listed here; 1145 total codes were applied to patients and 1,000 total codes were applied to caregivers.
Frequency listed is the frequency at which each subdomain code was applied within its respective HD triad domain.
ADL: Activities of daily living; HD: Huntington's disease.
Cognitive issues
For the Cognition domain, patients and caregivers reported in similar degrees of frequency on attention/concentration problems and HD triad awareness. Attention/concentration problems were characterized by patients as difficulties doing simple calculations or having sustained attention. One patient stated, “If I went to church or went to anything, I couldn't concentrate because I had all these different things going through my head.” One caregiver described her experiences with attention-related problems in a patient for whom she cared, “The first thing that was probably noticeable was that he was not able to count money or make change, and that's been for years now. Just trying to watch him count his change — well, he didn't count his change. I'm like, ‘Don't you ever check your change?’ And he would say ‘No,’ but upon further questioning, I would find out that he really could not count it.”
For HD triad awareness, both patients and caregivers reported that overall patient awareness of deficits and cognitive decline was more or less intact. One patient stated, “The second and third year, I started noticing cognitive issues in myself,” while a caregiver reported, “He knew what was going on around him. He knew who I was till the end. He was aware of what was happening to him.”
Patients and caregivers differed in their frequencies of discussing other cognitive issues. For example, patients spent more time discussing cognitive-related communication challenges, memory problems, and slowed information processing, while caregivers spoke more about executive functioning problems and perseveration (i.e., uncontrollable repetition of a meaningless word or phrase, or a previously appropriate word or phrase that is no longer appropriate). On memory worsening, one patient said, “I used to have all that in my brain — everybody's phone numbers, all the things I had to do for the whole week and the month—and now it's gone.” One caregiver described her experiences with executive functioning problems, “He cannot sequence things. If he was told orally to pick up a pencil, walk over to the next office, sign a document, and bring the document and the pencil back, he might pick up the pencil and not know what to do next, or he might walk to the office and stand there and not know to ask for the document. It's a matter of sequencing things in their proper order.” A patient also described her challenges with initiating tasks, “I just put them off. My husband is great about this. If he's got a doctor's appointment, he makes it, but I just put it off and put it off, where I never used to do that.”
Emotional–Behavioral Dyscontrol issues
Within the Emotional–Behavior domain, patients and caregivers discussed several areas with similar degrees of frequency, including aggression/behavioral dyscontrol, anger/irritability, anxiety, apathy, depression, emotional outbursts, and impulsivity. Anxiety and depression were discussed more often.
For anxiety and depression, exemplary patient comments included the following:
“I ended up checking myself in to the hospital because I was having suicidal thoughts and it was not good.”
“I think I cry probably three times a day or something. I mean it's just not normal the amount of times that I get sad. Things that make me sad probably aren't things that would make other people sad.”
“I worry about what's going to happen, what's really going to happen and how long. I always say, ‘I’ve got 20 years,’ but that's not true. Ten, 15 years, and that makes me worry. That freaks me out.”
“The only thing that is like inside, like totally freaking me out, that I'm really dreading, is when the chorea gets really bad, and I mean you lose your — deformity. You know, your face, what it normally looks like, you lose it. And your body's all twisted up. That's what really, really, really bothers me out of the whole thing. From start to finish, that's the one thing I think about and I dread.”
About anger, aggression, emotional outbursts and behavioral dyscontrol, one patient stated, “I just started noticing a lot more anger, aggression, just like lashing out of nowhere. If somebody did something that would make you angry, you would get angry and walk away. Well, I would break things or just lash out in different ways.” He continued with the following admission, “I break stuff. I’ve broken everything here. I’ve broken the dishwasher because I won't listen to instructions. I broke the stove because the things wouldn't go back on the right way, so I broke the stove.” In addition, patients alone discussed obsessions/compulsions related to fixed schedules/routines, resulting in difficulty adapting to change, or behaviors, such as cleaning.
Caregivers spent more time discussing disinhibition, and only they mentioned impatience, legal problems, and psychosis. One caregiver stated, “He started where he was getting in trouble where he was taking his clothes off and walking around the house without clothes on. He started walking outside and the people in the neighborhood, because we lived behind a school, people in the neighborhood who had children would be calling the police. They would say that he's walking around without any clothes on. He was arrested for indecent exposure.”
Motor issues
Motor symptoms and issues were discussed by patients and caregivers with similar frequency. The most frequently discussed issue was chorea, followed by ambulation, and activities of daily living. One patient described his chorea by stating, “My movement, my chorea has increased. I have tremors.” Another patient described how chorea interferes with her sleep, “I have torso movement all the time that keeps me awake at night because they're going 24 hours, you know, something is moving all the time.”
A caregiver described how chorea contributed to falls and imbalance, “After about 10 years, he was falling a lot in the bathtub, and he couldn't stand up in the bathtub. He would be very, not wanting help, but I would say once he fell out of the tub, you have to get bath bench. I got things like that so that his quality of life would be better so that he wasn't falling and hurting himself. He fell down a staircase twice in his life. That's what the chorea movements did to him.”
In addition to movements and ambulation-related challenges, several patients and caregivers discussed problems with speech and swallowing. The following caregiver describes both issues, “After awhile it got to where he couldn't vocalize his thoughts. I would put together a communication board where I had pictures of things like the word ‘yes,’ the word ‘no,’ a toilet, a TV, and I would ask him ‘yes/no’ questions. Or ask him what do you want, what do you need? He could point to stuff.” She continued by describing his challenges with swallowing, “It was like he was eating one day, and then the next day, he started having trouble where he was choking on stuff, and I started having to purée things. It just got to where he just couldn't get it to go down even when it was puréed. It was like after awhile, it was all going in to his lungs, and then, even after that, they told me he needed a feeding tube, and then when he got the feeding tube, he seemed to gain weight back because he had lost so much weight because he wasn't getting the proper nutrition.”
Inter-rater agreement and data saturation
Inter-rater agreement for patient and caregiver coding was greater than 90% for all codes applied. In both patient and caregiver code books, a total of 26 HD triad-specific codes were applied (Table 4), of which one was applied only in the patient sample (obsession/compulsion), and two codes were applied only in the caregiver sample (legal problems and impatience). Data saturation (the point at which no new codes were applied) was achieved after the third patient and the third caregiver interviews. All subsequent interviews were analyzed using code books developed from the first three interviews.
Integrating patient, caregiver and provider information
Overall, motor issues were most frequently discussed by patients, caregivers, and medical providers, followed by emotional–behavioral, and then cognitive issues. Of motor issues, chorea and related movements were the most frequently described by patients, caregivers, and medical providers. Anxiety and depression were the most frequently described emotional–behavioral issues by patients and caregivers, while anger was the most frequently listed symptom by medical providers, followed by depression and anxiety. Of cognitive issues, memory and perseveration were the most commonly discussed by patients and caregivers, while executive functioning and memory were most frequently listed by medical providers.
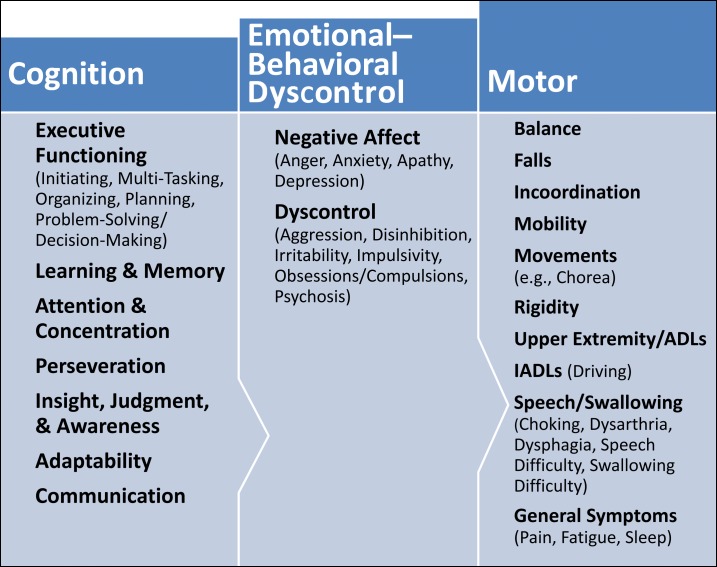
After examining and summarizing the different sources of HD triad data, members of the study team participated in an iterative triangulation exercise to create a conceptual schema that integrated the patient, caregiver, and medical provider perspectives. The result was a unified summary graphic (Figure 1) that represents each HD triad domain in a user-friendly and pragmatic way.
Figure 1. Huntington's Disease Triad Conceptual Schema of Patient, Caregiver, and Provider Report.
ADLs: Activities of daily living; IADLs: Instrumental activities of daily living.
Discussion
Findings from the expert surveys and individual phone-based interviews with HD patients and caregivers offered perspectives on key symptoms and issues most relevant to the HD triad. Although not statistically tested because the number of patient–caregiver dyads was insufficient, findings from the current study suggest that patients and caregivers have different perceptions of the prevalence and importance of various HD-related issues. The two cohorts discussed with varying frequencies many HD-related issues. For example, patients spent more time describing their problems with communication, memory, slower processing, anxiety, and obsessions/compulsions. On the other hand, caregivers spent more time describing problems in executive functioning, perseveration, disinhibition, and psychosis. These observed differences are consistent with other qualitative research examining the perspectives of similar patient populations with neurologic conditions and caregivers across a broad spectrum of HRQOL domains.19,25
It seems natural for patients to focus more on changes or impediments to their communication abilities, as these are their direct connections to the outside world. Even the slightest limitations in these conduits can be perceived as both socially and emotionally devastating. Patients are also likely more aware of deficits in their abilities to remember events, and the longer time needed to process and encode information, as these are often perceptible manifestations that carry significant functional, emotional, and social repercussions. Finally, heightened awareness of anxiety (including obsessions/compulsions) may be characteristic of the relatively earlier stage of the patient sample, as anxiety is linked with feelings of helplessness, which is surely amplified as one learns more about this disease and begins to observe gradual declines in functioning across these domains.
Similarly, it is understandable that caregivers would spend relatively greater amounts of time describing more observable and possibly more severe problems related to an inability to follow instructions, make decisions, and problem solve; or related to bizarre or psychotic presentations. It is important to consider these possible differences in perspective, especially when measuring outcomes related to HD triad domains.
This study is not without limitations. Although efforts were taken to enroll patients and caregivers from several regions across the United States (thus attempting to ensure a more heterogeneous sample), the study sample ultimately lacked racial–ethnic diversity. Future studies that focus on African-American and Hispanic HD patient and caregiver samples may provide additional information on the ways race, ethnicity, and cultural group membership may affect symptom sequelae. In addition, as purposive sampling was used through established support groups, the patient participants described themselves as healthier and earlier in the disease process when compared with caregiver participants. Subsequent studies would benefit from enrollment of more late-stage patients.
In this study, the perspectives of patients, caregivers, and medical providers were used to describe their personal experiences with cognitive, emotional–behavioral, and motor symptoms and issues related to HD. Using qualitative methods and analysis, we synthesized these findings into a conceptual schema that expounds each major concept of the HD triad to offer a better understanding of which aspects are most common and/or most important to those affected. This field may benefit from future mechanism of action research studies that attempt to disentangle conceptually similar concepts (e.g., executive function and perseveration; impulsivity, and disinhibition) and their unique relevance to HD triad–specific sequelae. Additional studies designed to compare and contrast clinician and patient concerns would also help to clarify potential disparities in patient–physician communication (and its role on future treatment trial selection) to ensure that treatments are ultimately best serving patients' needs and interests. For example, in our study, under behavioral concerns, “anger” was listed most frequently by clinician experts. The most important behavioral symptoms for patients were “behavioral problems” (which, in fact, may overlap with anger), and “stigma.” Similarly, in evaluation of motor concerns, “movements” were most frequently noted by clinicians, but “falls,” “IADLs,” and “time extension” were rated most important among patients.
These findings offer valuable information to HD researchers and clinicians regarding the HD triad and its specific make up. The HD-PRO-TRIAD™ provides an advantage over more generic instruments of HRQOL that do not fully capture the behavioral characteristics of HD. In addition, to date, based on a thorough literature search, we have found no other study that has focused specifically on cognitive, motor, and emotional–behavioral issues from patients, “caregivers,” and medical providers' perspectives. Furthermore, the HD-PRO-TRIAD™ does not have some of the limitations of previous patient-reported outcome measures developed for HD. The HD-QOL-I16 is available in French and Italian, but not English. The HD-QoL14 did not assess accepted norms for minimum sample patient sizes for the analyses it employed.26
This conceptual schema was used as the basis of a new patient-reported outcome measure to assess the HD triad impact on HRQOL — the HD-PRO-TRIAD™.17 This instrument may be used to measure clinical or supportive care intervention to manage disease and treatment-related burden in both clinical and research settings.
Acknowledgements
Writing assistance and editorial support during manuscript preparation were provided by Neva West, PhD, of Prescott Medical Communications Group (Chicago, IL), and Michael A. Nissen, ELS, Lundbeck LLC (Deerfield, IL). The copyright for the HDQLIFE and its individual items are held by the Regents of the University of Michigan (Ann Arbor, MI). The copyright for the PROMIS/NQ is held by the PROMIS Health Organization. The copyright for the Neuro-QOL items is held by David Cella, on behalf of the NINDS. The copyright for FACIT items are held by David Cella. The copyright for the TBI-QOL is held jointly by the Kessler Foundation and David Tulsky.
Footnotes
Funding: This research was funded by Lundbeck LLC, Deerfield, IL.
Financial Disclosures: Wendy Cheng, Brian Gorin, Mei Sheng Duh, and David Samuelson are employees of the Analysis Group, Inc., a contract research organization funded by Lundbeck LLC to conduct the research and develop the new PRO instrument, and engage the remainder of the HD-PRO-TRIAD™ research consortium. Noelle E. Carlozzi, Jennifer L. Beaumont, David Victorson, Victor Sung, David Tulsky, Sandra Gutierrez, Cindy Nowinski, Allison Mueller, and Samuel Frank were funded by the Analysis Group. Vivienne Shen is a full-time Lundbeck employee.
Conflict of Interests: S.F. has received research support from the Michael J Fox Foundation and Auspex, as well as consulting fees from Merz.
References
- 1.Pringsheim T, Wiltshire K, Day L, et al. The incidence and prevalence of Huntington's disease: a systematic review and meta-analysis. Mov Disord. 2012;27:1083–1091. doi: 10.1002/mds.25075. [DOI] [PubMed] [Google Scholar]
- 2.ACMG/ASHG statement Laboratory guidelines for Huntington disease genetic testing. The American College of Medical Genetics/American Society of Human Genetics Huntington Disease Genetic Testing Working Group. Am J Hum Genet. 1998;62:1243–1247. doi: 10.1086/301846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JM, Ramos EM, Lee JH, et al. CAG repeat expansion in Huntington disease determines age at onset in a fully dominant fashion. Neurology. 2012;78:690–695. doi: 10.1212/WNL.0b013e318249f683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paulson HL, Albin RL. Huntington's disease: Clinical features and routes to therapy. In: Lo DC, Hughes RE, editors. Neurobiology of Huntington's disease: Applications to Drug discovery Frontiers in Neuroscienc. Boca Raton: CRC Press; 2011. (Chapter 1. PM1D 21882418) [Google Scholar]
- 5.Singer C. Comprehensive treatment of Huntington disease and other choreic disorders. Cleve Clin J Med. 2012;79:S30–S34. doi: 10.3949/ccjm.79.s2a.06. [DOI] [PubMed] [Google Scholar]
- 6.Peavy GM, Jacobson MW, Goldstein JL, et al. Cognitive and functional decline in Huntington's disease: Dementia criteria revisited. Mov Disord. 2010;25:1163–1169. doi: 10.1002/mds.22953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirkwood SC, Su JL, Conneally P, et al. Progression of symptoms in the early and middle stages of Huntington disease. Arch Neurol. 2001;58:273–278. doi: 10.1001/archneur.58.2.273. [DOI] [PubMed] [Google Scholar]
- 8.Cleret de Langavant L, Fenelon G, Benisty S, et al. Awareness of memory deficits in early stage Huntington's disease. PLoS One. 2013;8:e61676. doi: 10.1371/journal.pone.0061676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harper P. Huntington's disease: a historical background. In: Bates G, Harper P, Jones L, editors. Huntington's disease. New York: Oxford University Press; 2002. pp. 3–27. p. [Google Scholar]
- 10.Thompson JC, Snowden JS, Craufurd D, et al. Behavior in Huntington's disease: Dissociating cognition-based and mood-based changes. J Neuropsychiatry Clin Neurosci. 2002;14:37–43. doi: 10.1176/appi.neuropsych.14.1.37. [DOI] [PubMed] [Google Scholar]
- 11.Ho AK, Hocaoglu MB. Impact of Huntington's across the entire disease spectrum: The phases and stages of disease from the patient perspective. Clin Genet. 2011;80:235–239. doi: 10.1111/j.1399-0004.2011.01748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams J, Downing N, Vaccarino AL, et al. Self-Reports of day-to-day function in a small cohort of people with prodromal and early HD. PLoS Curr. 2011;3:RRN1254. doi: 10.1371/currents.RRN1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carlozzi NE, Tulsky DS. Identification of health-related quality of life (HRQOL) issues relevant to individuals with Huntington disease. J Health Psychol. 2013;18:212–225. doi: 10.1177/1359105312438109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hocaoglu MB, Gaffan EA, Ho AK. Health-related quality of life in Huntington's disease patients: A comparison of proxy assessment and patient self-rating using the disease-specific Huntington's disease health-related quality of life questionnaire (HDQoL) J Neurol. 2012;259:1793–1800. doi: 10.1007/s00415-011-6405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hocaoglu MB, Gaffan EA, Ho AK. The Huntington's Disease health-related Quality of Life questionnaire (HDQoL): A disease-specific measure of health-related quality of life. Clin Genet. 2012;81:117–122. doi: 10.1111/j.1399-0004.2011.01823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clay E, De Nicola A, Dorey J, et al. Validation of the first quality-of-life measurement for patients with Huntington's disease: The Huntington Quality of Life Instrument. Int Clin Psychopharmacol. 2012;27:208–214. doi: 10.1097/YIC.0b013e3283534fa9. [DOI] [PubMed] [Google Scholar]
- 17.Carlozzi N, Victorson D, Sung V, et al. Tremor Other Hyperkinet Mov (N Y) HD-PRO-TRIAD™ Validation: A patient-reported instrument for the symptom triad of Huntington disease. 2014;4 doi: http://dx.doi.org/10.7916/D8PN93NZ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker D, Myrick F. Grounded theory: An exploration of process and procedure. Qual Health Res. 2006;16:547–659. doi: 10.1177/1049732305285972. [DOI] [PubMed] [Google Scholar]
- 19.Perez L, Huang J, Jansky L, et al. Using focus groups to inform the Neuro-QOL measurement tool: Exploring patient-centered, health-related quality of life concepts across neurological conditions. J Neurosci Nurs. 2007;39:342–353. doi: 10.1097/01376517-200712000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Cella D, Lai JS, Nowinski CJ, et al. Neuro-QOL: Brief measures of health-related quality of life for clinical research in neurology. Neurology. 2012;78:1860–1867. doi: 10.1212/WNL.0b013e318258f744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlozzi NE, Tulsky DS, Kisala PA. Traumatic brain injury patient-reported outcome measure: Identification of health-related quality-of-life issues relevant to individuals with traumatic brain injury. Arch Phys Med Rehabil. 2011;92:S52–S60. doi: 10.1016/j.apmr.2010.12.046. [DOI] [PubMed] [Google Scholar]
- 22.Tulsky DS, Kisala P, Victorson D, Carlozzi NE, Cella D. Development of tailored outcomes measures for traumatic brain injury and spinal cord injury. Proceedings of the 61st annual meeting of the American Academy of Neurology. April 25–May 2, 2009, Seattle, WA. [Google Scholar]
- 23.Carlozzi NE, Tulsky DS. Identification of health-related quality of life (HRQOL) issues relevant to individuals with Huntington disease. J Health Psych. 2013;18:212–225. doi: 10.1177/1359105312438109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: Properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lynch EB, Butt Z, Heinemann A, et al. A qualitative study of quality of life after stroke: The importance of social relationships. J Rehabil Med. 2008;40:518–523. doi: 10.2340/16501977-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paulsen JS, Nance M, Kim JI, et al. A review of quality of life after predictive testing for and earlier identification of neurodegenerative diseases. Prog Neurobiol. 2013;110:2–28. doi: 10.1016/j.pneurobio.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]