Abstract
Posterior cruciate ligament (PCL) injuries are uncommon, and most occur in association with other lesions. The treatment of PCL injuries remains controversial; in addition, PCL injuries have been documented to have a propensity to heal. In the literature several different patterns of PCL injury have been described including midsubstance tears/injuries, tibial bony avulsions, femoral bony avulsions, and femoral “peel-off” injuries. A peel-off injury is a complete or incomplete soft-tissue disruption of the PCL at its femoral attachment site without associated bony avulsion. In recent years arthroscopic repair of femoral avulsion and peel-off lesions of the PCL has been reported. In most of these articles, a transosseous repair with sutures passed through 2 bone tunnels into the medial femoral condyle has been described. We present a case of a femoral PCL avulsion in a 20-year-old collegiate football player with an associated medial collateral ligament injury, and we report about a novel technique for PCL repair using 2 No. 2 FiberWire sutures and two 2.9-mm PushLock anchors (Arthrex) to secure tensioning the ligament at its footprint.
Posterior cruciate ligament (PCL) injuries are uncommon: the estimated incidence ranges from 3% to 37% of all the ligamentous injuries. Isolated PCL lesions are rare, and they have been documented to have the propensity to heal.1,2 In the literature several different patterns of PCL injury have been described including midsubstance injuries, tibial bony avulsions, femoral avulsion with bony fragments, and femoral “peel-off” injuries, with the last 2 types being less common.3 Arthroscopic repair of femoral avulsion and peel-off lesions of the PCL has been reported.4-9 In most of these articles, a transosseous repair with sutures passed through 2 bone tunnels into the medial femoral condyle was described.
We present a case of a femoral peel-off lesion of the PCL in a 20-year-old collegiate football player with an associated medial collateral ligament (MCL) injury, and we report about a novel technique for PCL repair using 2 No. 2 FiberWire sutures and two 2.9-mm PushLock anchors (Arthrex, Naples, FL) to secure the ligament at the footprint.
Case Report and Surgical Technique
A 20-year-old male collegiate football player (body mass index, 34.67 kg/m2) presented to us the day after a right knee injury during a football game. His right knee buckled into valgus when a second player fell onto him. He was not able to walk and complained about medial pain on the right knee. The physical examination of the right lower limb showed intact neurovascular status, full extension of the knee joint, and passive flexion only to approximately 45°. The ligament examination was difficult because of swelling and limitation of motion, but there was complete laxity at full extension and at 30° with a 3+ valgus stress test. The posterior drawer test was positive with grade 1 for posterior sag, and the anterior drawer test had a normal endpoint on testing. The patient had local tenderness along the medial joint line and MCL, and manual muscle examination showed intact motor function in the lower extremity.
On sagittal magnetic resonance imaging, there was a femoral avulsion of the PCL with a normal tibial insertion and an intact anterior cruciate ligament (ACL) (Fig 1). On the coronal view, a detachment of the medial meniscus from the inferior meniscofemoral ligament, complete disruption of the distal MCL, a minimally depressed lateral tibial plateau fracture with contusion versus trabecular microfractures, and a small radial tear of the lateral meniscus were detected (Fig 2). The patient was indicated for an arthroscopic PCL repair, treatment of the meniscal lesions, and open MCL repair of the right knee. The surgery was scheduled 11 days after the injury to allow an arthroscopic technique to be used and minimize the risk of extravasation of fluid.
Fig 1.
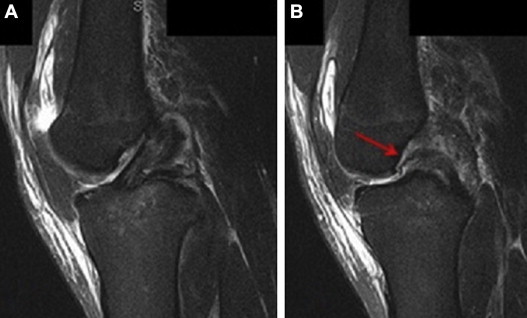
Sagittal magnetic resonance imaging of right knee: (A) intact ACL and (B) femoral avulsion PCL (arrow).
Fig 2.

Coronal magnetic resonance imaging of right knee: (a) MCL tibial detachment, (b) minimally depressed lateral tibial plateau fracture, and (c) detachment of medial meniscus from inferior meniscofemoral ligament.
Preoperative Assessment
The patient was positioned supine, and the right leg was positioned with a tourniquet around the thigh in a Canadian leg holder. An examination under anesthesia confirmed laxity with the posterior drawer test, as well as with valgus stress, and no ACL laxity. A superomedial outflow portal was established, and medial and lateral parapatellar portals were used for arthroscopy and instrumentation. An arthroscopic evaluation was performed and confirmed an intact ACL and a femoral avulsion of the PCL without bony fragments, with a few of the posterior fibers still intact (Fig 3). In the medial compartment the cartilage looked mostly healthy, a drive-through sign was present, and the entire meniscus had risen up off of the tibial side, indicating disruption of the coronary ligament; the posterior root was probed and appeared to have a stable attachment (Fig 4). In the lateral compartment we found a small radial tear of the inner rim of the mid body of the meniscus, and on the tibial side, there were 2 small fissures that may have correlated with the subchondral fracture diagnosed on magnetic resonance imaging.
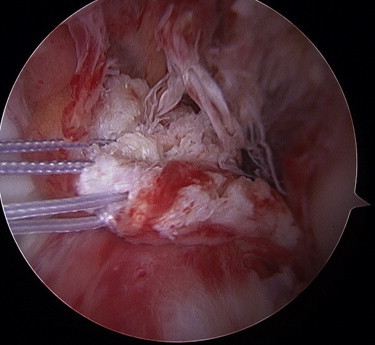
Fig 3.
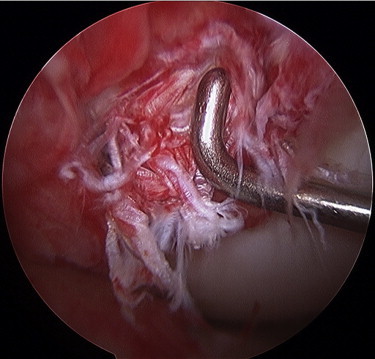
Arthroscopic view of right knee. The probe shows some fibers of the PCL still attached to the footprint.
Fig 4.
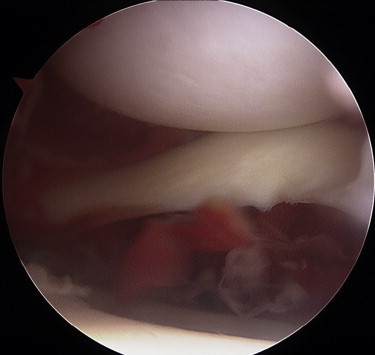
Arthroscopic view of right knee. The entire meniscus had risen up off of the tibial side, indicating disruption of the tibial coronary ligament, and the posterior root was probed and appeared to have a stable attachment.
PCL Repair
First, the PCL was probed and mobilized with a grasper toward to the medial femoral condyle to ensure reparability and reduction before proceeding with the repair (Fig 5). A 5.5-mm PassPort cannula (Arthrex) was placed in the lateral parapatellar portal to easily access the PCL and avoid placing sutures into the anterior fat pad. After the femoral footprint was identified, a 4.0-mm shaver was used to clean off the PCL footprint from a few remnant fibers, and some microfractures were then performed at the femoral insertion with a PowerPick (Arthrex) to obtain bleeding from the subchondral bone, improving healing of the repaired ligament (Fig 6).
Fig 5.
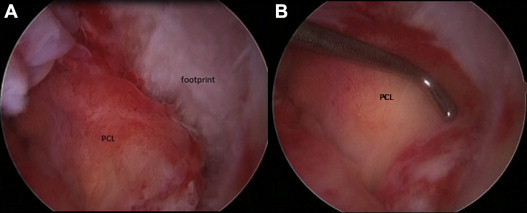
Arthroscopic views of right knee. (A) The PCL was detached from its footprint. (B) Evaluation of the ability to ensure PCL reduction to its footprint with the probe.
Fig 6.

Arthroscopic view of right knee. Using a PowerPick, we performed some microfractures into the footprint to obtain bleeding from the subchondral bone, improving healing of the repaired ligament.
A Scorpion cuff repair instrument (Arthrex) was inserted through the cannula located in the lateral parapatellar portal, and 2 No. 2 FiberWire sutures were passed through the anterolateral and posteromedial bundles of the PCL. Each suture was passed through the tissue twice to obtain a locking figure-of-8 construct to hold the ligament. Ultimately, a very good purchase of the ligament with each suture was obtained (Fig 7).
Fig 7.
With an arthroscopic Scorpion suture passer, 2 No. 2 FiberWire sutures were passed in a figure-of-8 fashion through the posteromedial and anterolateral bundles of the repaired PCL.
To ensure PCL reduction to its footprint, two 2.9-mm PushLock anchors were used. First, 2 holes were drilled with the dedicated instrumentation into the femoral PCL footprint; the 2 limbs of the same suture were then passed in each anchor. Each PushLock was inserted without difficulty through the PassPort cannula in the lateral parapatellar portal (Fig 8). Sutures were carefully tensioned appropriately before final seating of the anchors. In addition, an anterior drawer maneuver was performed as the sutures were tensioned at 90° of flexion and the anchors were inserted into the holes. The suture tails were cut, and a good repair of the PCL back to its footprint was obtained (Fig 9). Video 1 shows all the steps of this technique, which are summarized in Table 1. Table 2 shows indications, contraindications, tips, pearls, pitfalls, and key points.
Fig 8.

Arthroscopic view of right knee. Insertion of a 2.9-mm PushLock was performed to ensure PCL reduction to its footprint.
Fig 9.
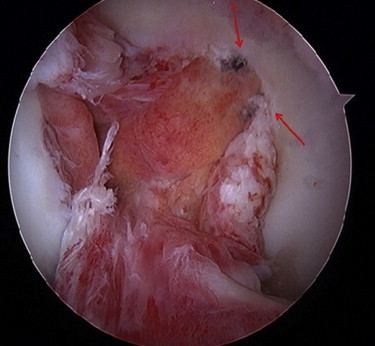
Arthroscopic view of right knee. Final result of PCL repair. The arrows indicate the two 2.9-mm PushLock anchors.
Table 1.
Steps of Surgical Technique
| 1. Perform evaluation of the patient under anesthesia to confirm the posterior laxity. |
| 2. Place the medial and lateral parapatellar portals and a superomedial outflow portal. |
| 3. Probe the PCL and mobilize it with a grasper to ensure reparability and reduction before proceeding with the repair. |
| 4. Place a 5.5-mm PassPort cannula into the lateral parapatellar portal to easily access the PCL and avoid placing sutures into the anterior fat pad. |
| 5. Identify the femoral footprint, and clean off the PCL footprint from the remnant. |
| 6. Perform some microfractures with a PowerPick to obtain bleeding from the subchondral bone, improving healing of the repaired ligament. |
| 7. Insert a Scorpion cuff repair instrument through the cannula, and pass 2 No. 2 FiberWire sutures in a figure-of-8–type fashion in the anterolateral and posteromedial bundles of the PCL. |
| 8. Drill 2 holes with the dedicated 2.9-mm PushLock instrumentation into the footprint. |
| 9. Pass the 2 limbs of the same suture in each anchor, and insert them into the cannula. |
| 10. Carefully tension the suture before final seating of the anchors, and perform an anterior drawer maneuver while inserting the anchors into the holes. |
| 11. Cut the suture tails, and arthroscopically verify the stability of the repair. |
Table 2.
Repair of PCL Peel-Off Avulsion From Femoral Condyle Using 2 Knotless Anchors
| Indications |
| PCL soft-tissue avulsion from femoral footprint (proximal fibers) |
| Adequate PCL tissue length to restore ligament to its footprint |
| Adequate tissue quality to hold sutures |
| Patients in whom PCL reconstruction cannot be performed (e.g., associated tibial plateau fracture) |
| Patients with multiligament injuries that will require concurrent repair or reconstruction of other ligaments |
| Young patients with open physes |
| Contraindications |
| Bony avulsion |
| PCL midsubstance injuries |
| Inadequate tissue/bone quality |
| Tips |
| Good view of footprint from lateral parapatellar portal |
| Ability to mobilize PCL to ensure reducibility to its footprint |
| Use of PassPort cannula to easily place knotless anchors |
| Performance of microfracture on footprint to improve ligament-bone healing |
| Use of sutures in figure-of-8 fashion to ensure good purchase of ligament |
| Pearls |
| Repairing the PCL reduces the morbidity associated with reconstruction. It has been shown that there is no statistical difference in strength or stiffness for a suture anchor and knotless anchor construct compared with a bone tunnel construct for an anatomic repair.10 |
| The most important aspect is to place the anchors at the anterior edge of the footprint so that the ligament will reduce and place tension on the repair. |
| Reduction of the joint by the anterior drawer maneuver should be performed when reducing the ligament by anchor insertion. |
| Pitfalls |
| A divergence between the knotless suture anchor insertion and the drilled hole can damage the anchor. |
| Insufficiently tensioning the ligament or not performing an anterior drawer maneuver during the insertion of the anchors may cause failure of the operation. |
| Key points |
| Place the lateral parapatellar portal while ensuring placement in the correct direction to grab the PCL and to position the anchors. |
| Place a cannula into the lateral parapatellar portal to easily access the PCL and avoid positioning of the sutures into the fat pad. |
| Perform microfracture to obtain bleeding from the bone to improve ligamentous healing. |
| Pass each suture through the tissue twice to obtain a locking figure-of-8 construct to obtain good purchase of the ligament. |
| Place the anchor holes at the anterior border of the footprint to help reduce and tension the PCL to its footprint. |
| Carefully tension the ligament before the final seating of the anchors, and perform an anterior drawer maneuver while inserting the anchors into the predrilled holes. |
Meniscectomy and MCL Repair
A minor resection of the radial tear of the lateral meniscus was also performed arthroscopically. Up to this point, a tourniquet was not used, but for the open repair, the tourniquet was inflated, a longitudinal incision was made over the medial aspect of the knee, and the sartorial fascia was identified and elevated. The medial meniscus was repaired to the coronary ligament (deep MCL off the tibia) with No. 0 Vicryl sutures (Ethicon, Somerville, NJ) in figure-of-8 fashion, as well as horizontal mattress fashion, and it was then reattached just distal to the articular surface of the tibia with two 3.0-mm SutureTak anchors (Arthrex) and one 11.11 × 25.4–mm staple (Smith & Nephew, London, England). At the end of these procedures, the stability of the knee was tested, with both posterior drawer and valgus stress tests in extension and at 30° of flexion, and the knee appeared stable. The wound was copiously irrigated again and closed in a standard fashion.
Postoperative Treatment
Toe-touch weight bearing of the right lower limb was allowed with the knee immobilized into a hinged brace locked in extension for 2 weeks. Subsequently, gentle mobilization to fully recover the range of motion was started. At 7 weeks after surgery, there was no medial laxity at full extension or 30° of flexion, and a slightly positive posterior drawer test was noted but with a very good endpoint and no anterior instability. At that point, use of the brace was discontinued. The athlete returned to full practice and contact by 3 months after surgery, and at the time of this report, 9 months after surgery, he was doing well without any problems.
Discussion
Femoral avulsions and peel-off lesions of the PCL are rare. The first case was reported by O'Donoghue6 in 1950. Subsequently, in 1975, Drucker and Wynne7 reported on a 25-year-old patient with an isolated PCL femoral avulsion; in this case they performed a transosseous repair with sutures.
Wheatley et al.4 reported on 13 cases of arthroscopic repair of a femoral avulsion of the PCL with sutures passed through 2 tunnels on the medial femoral condyle; they concluded that this technique was effective at reducing postoperative instability and improving functional outcomes. Ross et al.5 in 2003 also reported their results with a similar technique for repairing PCL femoral peel-off lesions.
Park and Kim8 reported on a patient with tibial bony avulsion of the ACL and discontinuation of the PCL at the femoral insertion. They performed a PCL repair with 4 transfemoral tunnels: 2 for the anterior bundle and 2 for the posterior bundle. They then passed 2 sutures through the PCL and the tunnels and tied them over a bone bridge on the medial femoral condyle.
Finally, Difelice et al.9 in 2012 reported on 3 patients with PCL peel-off injuries; they performed a PCL repair passing Bunnell-type stitches into the substance of the ligament and then passed the sutures through drill holes into the femoral footprint and tied them over a bony bridge.
To our knowledge, this is the first report of a PCL repair technique using sutures and knotless anchors instead of transfemoral tunnels. In 2012 In et al.10 reported on a biomechanical comparison among suture anchor fixation, screw fixation, and pullout suture fixation for ACL tibial avulsion fractures. They concluded that the initial fixation strength of suture anchor fixation was not less than that of screw fixation or pullout suture fixation and the initial displacement with suture anchor fixation was lower. Besides, it has been shown in some biomechanical studies that there is no statistical difference in strength or stiffness for a suture anchor and PushLock construct compared with a bone tunnel construct for anatomic repair of the lateral ligaments of the ankle.11
The main advantage of the described technique is that it did not require transfemoral tunnels, resulting in a less invasive surgery, less risk of arthrofibrosis, and less morbidity in general compared with a reconstruction, but with no changes in strength or stiffness of the construct. Using an arthroscopic cannula, avoiding placing suture in the fat pad, and using a Scorpion cuff repair instrument allow good purchase of the ligament without any difficulty. In addition, preserving the native tissue results in a theoretic maintenance of the proprioception.12 The main risk with this technique is not to be able to restore the anatomy and strength of the native PCL, so careful evaluation of imaging and careful selection of patients are required. Tips, pearls, and pitfalls of this technique are shown in Table 2.
In summary, we report on a 20-year-old patient with a sport-related injury to the PCL and MCL. The all-arthroscopic PCL repair that allows tensioning and reduction to the footprint of the avulsion or peel-off lesion provides another technique for the treatment of these specific lesions. This is a novel technique with certain advantages over the use of bone tunnels and a bone bridge technique.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.B. receives support from “Enrico ed Enrica Sovena” Foundation, a nonprofit foundation that partially sponsored his fellowship at the Department of Orthopaedics and Rehabilitation of the University of Iowa and all the related publications. A.A. receives support from Arthrex, Arthrosurface, and MTP Solutions. Arthrex for product development.
Supplementary data
Description of mechanism of injury, physical examination, and correlated imaging in our patient. Step-by-step surgical techniques used to perform the PCL repair with knotless sutures anchors are shown. Initially, magnetic resonance imaging and arthroscopy show the medial PCL peel-off lesion, with few of the posterior fibers still intact, and the medial compartment lesions; a drive-through sign was present, and the entire meniscus had risen up off of the tibial side, indicating disruption of the coronary ligament. The femoral footprint was cleaned off with a shaver, and microfractures were then performed at the femoral insertion with a PowerPick. A Scorpion cuff repair instrument was inserted through the cannula, and 2 No. 2 FiberWire sutures were passed through the substance of the PCL. Each suture was passed through the tissue twice to obtain a locking figure-of-8 construct to hold the ligament. Ultimately, a very good purchase of the ligament with each suture was obtained. We secured the PCL reduction to its footprint with two 2.9-mm PushLock anchors, and an anterior drawer maneuver was performed as the sutures were tensioned at 90° of flexion and the anchors were inserted into the holes. At the end of the procedure, an anatomic repair of the PCL back to its footprint was obtained.
References
- 1.Fanelli G., Beck J.D., Edson C.J. Current concepts review: The posterior cruciate ligament. J Knee Surg. 2010;23:61–72. doi: 10.1055/s-0030-1267466. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne K.D., Clark M., Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41:1526–1533. doi: 10.1177/0363546513486771. [DOI] [PubMed] [Google Scholar]
- 3.Giordano B.D., Dehaven K.E., Maloney M.D. Acute femoral “peel-off” tears of the posterior cruciate ligament: Technique for arthroscopic anatomical repair. Am J Orthop (Belle Mead NJ) 2011;40:226–232. [PubMed] [Google Scholar]
- 4.Wheatley W.B., Martinez A.E., Sacks T. Arthroscopic posterior cruciate ligament repair. Arthroscopy. 2002;18:695–702. doi: 10.1053/jars.2002.32836. [DOI] [PubMed] [Google Scholar]
- 5.Ross G., Driscoll J., McDevitt E., Scheller A., Jr. Arthroscopic posterior cruciate ligament repair for acute femoral “peel off” tears. Arthroscopy. 2003;19:431–435. doi: 10.1053/jars.2003.50134. [DOI] [PubMed] [Google Scholar]
- 6.O’Donoghue D.H. Surgical treatment of fresh injuries to the major ligaments of the knee. J Bone Joint Surg Am. 1950;32:721–738. [PubMed] [Google Scholar]
- 7.Drucker M.M., Wynne G.F. Avulsion of the posterior cruciate ligament from its femoral attachment: An isolated ligamentous injury. J Trauma. 1975;15:616–617. doi: 10.1097/00005373-197507000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Park I.S., Kim S.J. Arthroscopic fixation of avulsion of the posterior cruciate ligament from femoral insertion. Arthroscopy. 2005;21:1397. doi: 10.1016/j.arthro.2005.08.030. [DOI] [PubMed] [Google Scholar]
- 9.Difelice G.S., Lissy M., Haynes P. Surgical technique: When to arthroscopically repair the torn posterior cruciate ligament. Clin Orthop Relat Res. 2012;470:861–868. doi: 10.1007/s11999-011-2034-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.In Y., Kwak D.S., Moon C.W., Han S.H., Choi N.Y. Biomechanical comparison of three techniques for fixation of tibial avulsion fractures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2012;20:1470–1478. doi: 10.1007/s00167-011-1694-7. [DOI] [PubMed] [Google Scholar]
- 11.Giza E., Nathe R., Nathe T., Anderson M., Campanelli V. Strength of bone tunnel versus suture anchor and PushLock construct in Broström repair. Am J Sports Med. 2012;40:1419–1423. doi: 10.1177/0363546512443947. [DOI] [PubMed] [Google Scholar]
- 12.Kim S.J., Kim S.H., Chun Y.M., Hwang B.Y., Choi D.H., Yoon J.Y. Clinical comparison of conventional and remnant-preserving transtibial single-bundle posterior cruciate ligament reconstruction combined with posterolateral corner reconstruction. Am J Sports Med. 2012;40:640–649. doi: 10.1177/0363546511428068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of mechanism of injury, physical examination, and correlated imaging in our patient. Step-by-step surgical techniques used to perform the PCL repair with knotless sutures anchors are shown. Initially, magnetic resonance imaging and arthroscopy show the medial PCL peel-off lesion, with few of the posterior fibers still intact, and the medial compartment lesions; a drive-through sign was present, and the entire meniscus had risen up off of the tibial side, indicating disruption of the coronary ligament. The femoral footprint was cleaned off with a shaver, and microfractures were then performed at the femoral insertion with a PowerPick. A Scorpion cuff repair instrument was inserted through the cannula, and 2 No. 2 FiberWire sutures were passed through the substance of the PCL. Each suture was passed through the tissue twice to obtain a locking figure-of-8 construct to hold the ligament. Ultimately, a very good purchase of the ligament with each suture was obtained. We secured the PCL reduction to its footprint with two 2.9-mm PushLock anchors, and an anterior drawer maneuver was performed as the sutures were tensioned at 90° of flexion and the anchors were inserted into the holes. At the end of the procedure, an anatomic repair of the PCL back to its footprint was obtained.


