Abstract
Peroneus brevis tendon injury is the most common lesion of the peroneal tendons. The initial treatment is conservative, and surgical treatment is indicated if conservative treatment fails. It is often necessary to open the entire upper and lower retinaculum to obtain adequate visualization of the structures. We present a case in which the peroneus brevis tenodesis was used with the aid of tendoscopy. This technique should be used for patients with lesions affecting more than 50% of the tendon diameter. We found that, by making small incisions, the patient recovered well, quickly, with resolution of pain.
Of the lesions that affect the peroneal tendons, peroneus brevis tendon injury is the most common. These lesions frequently may take time to be diagnosed because the symptoms presented are similar to those of lateral-ankle ligament injury.1,2
The clinical condition is usually characterized by pain in the lateral region of the ankle together with swelling and loss of strength for rear-foot eversion.3 Imaging examinations may assist in determining the diagnosis; however, ultrasonography and magnetic resonance imaging are very sensitive and can yield too many false-positive results.4
Initially, conservative treatment is indicated, including nonsteroidal anti-inflammatory agents, rest, immobilization with a spica cast or brace, orthosis use, and physiotherapy. Surgical treatment may be indicated for refractory cases.2
Krause and Brodsky2 proposed a classification to guide treatment. For lesions affecting less than 50% of the tendon diameter, they recommend resection of the injured area and insertion of tubes, whereas for lesions affecting more than 50% of the tendon diameter, tenodesis is indicated.
Conventional surgical treatment includes exposing the peroneal tendons from 1 cm posterior to the end of the lateral malleolus up to 1 cm from the base of the fifth metatarsal. It is often necessary to open the entire upper and lower retinaculum to obtain adequate visualization of structures.5 In this context, tendoscopy has been proposed as a means of accessing the tendons less invasively with fewer complications.6 This study describes a peroneus brevis tenodesis technique using tendoscopy (Video 1).
Case Description
A female patient, aged 68 years, presented in July 2009 complaining of an insidious pain in the lateral rear foot, but she reported no local trauma. Physical examination showed mild symmetric varus of the rear foot and swelling and pain in the region. A complex peroneal brevis tendon was seen on magnetic resonance imaging (Fig 1).
Fig 1.
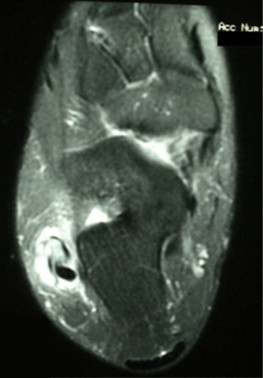
Magnetic resonance imaging (axial section, T2 weighted) of rear foot showing complex lesion of peroneus brevis tendon.
Conservative treatment was initiated with nonsteroidal anti-inflammatory drugs, physiotherapy for analgesia, overall strengthening of the ankle and intrinsic foot muscles, and use of a valgus insole for the rear foot, but these methods were unsuccessful. After 6 months with no improvement, surgical treatment was indicated.
Surgical Technique
The patient is placed in the lateral decubitus position under spinal anesthesia. A pneumatic tourniquet is placed at the base of the thigh. We use a 2.7-mm optical device, at a 30° angle, and an infusion pump at a pressure not higher than 40 mm Hg. As previously described by van Dijk and Kort,6 access to the tendons may be obtained at any point on the optical path. We make the first portal about 3 cm proximal to the end of the lateral malleolus. A skin incision is made with a No. 11 blade, and the tendon sheath is opened by blunt dissection. The second, or distal, portal is made in the same manner, approximately 2 to 2.5 cm distally and plantar to the end of the fibula. We start inspection through the distal portal and through the proximal portal with the blade. As shown in Fig 2, extensive synovectomy is performed, and subsequently, the optical device and blade are switched between portals to improve inspection and synovectomy if necessary (Fig 3).
Fig 2.

Planning of fibular tendoscopy portals, with one portal 3 cm proximal to end of fibula and another portal 2 to 2.5 cm distal and anterior to end of fibula.
Fig 3.
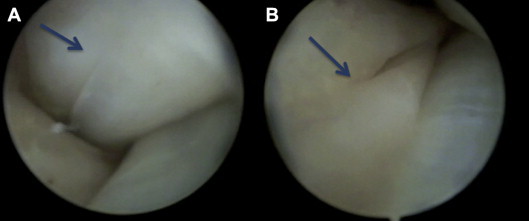
(A) Proximal portal view showing upper limit of lesion (arrow). (B) Distal portal view showing lower limit of lesion (arrow).
The pseudotumor caused by the extensive lesion of the peroneus brevis tendon is demarcated. A U-shaped lateral suture is made between the distal stumps of the peroneus brevis tendon and peroneus longus tendon, with a No. 3-0 nylon suture. Tenotomy is performed proximally to the suture of the peroneus brevis tendon. The latter is pulled through the proximal portal and placed on the skin, as shown in Fig 4. Gentle traction is applied to the degenerated tendon stump, and the new lateral suture is made in the same way but, this time, between the proximal tendon stumps, as shown in the Fig 5. At this point, proximal tenotomy is performed near the stump of the peroneus brevis tendon. This concludes the tenodesis procedure. Through the portals, simple stitches are made for short closure of the proximal and distal retinaculum with No. 4-0 nylon suture. The portals are then closed with the same suture, also with simple stitches, as shown in Fig 6.
Fig 4.

(A) Macroscopic view of pseudotumor-type lesion with longitudinal fissure through proximal portal after distal tenotomy through distal portal. (B) Enlarged view of same lesion.
Fig 5.

Proximal and distal fibular tenodesis after lesion resection.
Fig 6.

Final appearance after portal suturing.
The patient recovered well, and there were no postoperative complications. Because the retinaculum had not been opened extensively, rehabilitation could start sooner than in cases of open surgery.
Early active motion and partial ankle loading were allowed at only 5 days postoperatively to prevent tendon adhesion. Immobilization with an ankle foot brace was maintained for 6 weeks. Strengthening and proprioception exercises were performed for about 4 months after surgery.
The patient complained of discomfort in the distal portal region until about 4 months, which we attribute to the distal-region tenodesis. Six months after surgery, she was completely asymptomatic, and she remains so 3.5 years after surgery.
Discussion
The use of smaller incisions and the limited opening of the retinaculum potentially reduce the chances of scar tissue adhesions and the chance of sural nerve injury.6 Redfern and Myerson5 studied 28 patients with lesions in the short and long fibular tendons who underwent different procedures. Nine patients had complications; in 6 of these patients, the complications were directly related to the surgical access: superficial wound infection (3), sural neuritis (2), and wound dehiscence (1).
Numerous procedures have been described using the endoscopy technique. Van Dijk and Kort6 performed fibular tenosynovectomy in 4 patients, repair of a longitudinal injury to the peroneus brevis through a mini-incision in 1 patient, and peroneal tuberosity resection in 1 patient. Scholten and van Dijk7 described the repair of fibular tendon lesions using mini-incisions in 11 patients and successfully deepened the retromalleolar groove by the endoscopic technique alone in 2 patients. Sammarco8 described debridement of a low insertion of the muscle belly of the peroneus brevis tendon and lower retinaculum decompression.
We conclude that the technique presented avoided the need to open the entire peroneal retinaculum. By using tendoscopy, we were able to demarcate the lesion size and identify the transition from normal to affected tendon, which facilitates locating incisions and performing tenotomy and tenodesis through portals as described without extensive access. The patient improved quickly with resolution of pain.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Peroneal tenodesis technique with the use of tendoscopy.
References
- 1.Dombek M.F., Lamm B.M., Saltrick K., Mendicino R.W., Catanzariti A.R. Peroneal tendon tears: A retrospective review. J Foot Ankle Surg. 2003;42:250–258. doi: 10.1016/s1067-2516(03)00314-4. [DOI] [PubMed] [Google Scholar]
- 2.Krause J.O., Brodsky J.W. Peroneus brevis tendon tears: Pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19:271–279. doi: 10.1177/107110079801900502. [DOI] [PubMed] [Google Scholar]
- 3.Sobel M., DiCarlo E.F., Bohne W.H., Collins L. Longitudinal splitting of the peroneus brevis tendon: An anatomic and histologic study of cadaveric material. Foot Ankle. 1991;12:165–170. doi: 10.1177/107110079101200306. [DOI] [PubMed] [Google Scholar]
- 4.Jerosch J., Aldawoudy A. Tendoscopic management of peroneal tendon disorders. Knee Surg Sports Traumatol Arthrosc. 2007;15:806–810. doi: 10.1007/s00167-006-0227-2. [DOI] [PubMed] [Google Scholar]
- 5.Redfern D., Myerson M. The management of concomitant tears of the peroneus longus and brevis tendons. Foot Ankle Int. 2004;25:695–707. doi: 10.1177/107110070402501002. [DOI] [PubMed] [Google Scholar]
- 6.van Dijk C.N., Kort N. Tendoscopy of the peroneal tendons. Arthroscopy. 1998;14:471–478. doi: 10.1016/s0749-8063(98)70074-x. [DOI] [PubMed] [Google Scholar]
- 7.Scholten P.E., van Dijk C.N. Tendoscopy of the peroneal tendons. Foot Ankle Clin. 2006;11:415–420. doi: 10.1016/j.fcl.2006.03.004. vii. [DOI] [PubMed] [Google Scholar]
- 8.Sammarco V.J. Peroneal tendoscopy: Indications and techniques. Sports Med Arthrosc. 2009;17:94–99. doi: 10.1097/JSA.0b013e3181a3d420. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Peroneal tenodesis technique with the use of tendoscopy.


