Abstract
Background:
Automated whole slide imaging (WSI), also known as virtual microscopy is rapidly becoming an important tool in diagnostic pathology. Currently, the primary utilization of the technique is for transmission of digital images, for second opinion consultation, as well as for quality assurance and education. The high-resolution of digital images along with the refinement of technology could now allow for WSI to be used as an alternative to conventional microscopy (CM) as a first line diagnostic platform. However, the accuracy and reproducibility of the technology for the routine histopathologic diagnosis has not been established yet. This study was undertaken to compare the intra-observer variability of WSI and CM in the primary diagnosis of breast biopsies.
Materials and Methods:
One hundred and three consecutive core needle biopsies of breast were selected for this study. Each slide was digitally scanned and the images were stored in a shared file. Three board-certified pathologists independently reviewed the glass slides by CM first, and in an interval of 2-3 weeks for the 2nd time to establish their baseline CM versus CM reproducibility. They then reviewed the digital images of all cases following the same interval of time to compare the reproducibility of WSI versus CM for each observer. The diagnostic categories included the typical range of benign and malignant mammary lesions.
Results:
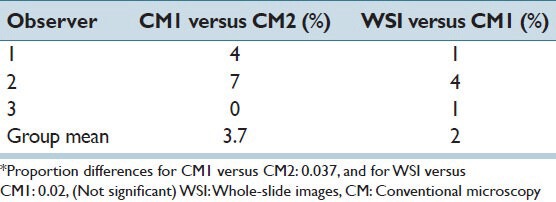
The intra-observer variability for CM versus CM was 4%, 7%, and 0% for observers 1, 2, and 3 respectively. The diagnostic variability for WSI versus CM was 1%, 4%, and 1% for the same observers. All diagnostic disagreements were between ductal hyperplasia and atypical ductal hyperplasia. There was no intra-observer disagreement in the diagnosis of benign versus malignant disease.
Conclusions:
The intra-observer variability in the diagnosis of the core needle biopsies of the breast by high-resolution, WSI was the same as conventional glass slide microscopy. These results suggest that, WSI could be used similar to CM for the initial diagnosis of breast biopsies.
Keywords: Breast biopsy, digital microscopy, reproducibility, whole slide imaging
INTRODUCTION
While digital pathology has been around for more than a decade, its widespread application for primary histologic diagnosis still awaits validation against the traditional glass slide microscopy. Slide digitalization mimics, the use of a microscope with capability of movement along the x and y planes as well as gradual increments in magnification.[1,2,3] Digital microscopy has been shown to have various practical applications including, quality assurance,[4,5,6] teleconsultation for second opinion,[7,8,9,10] education,[11,12] and intra-operative frozen section consultation.[10] It has also been shown that the use of whole slide digital images, improves workflow by eliminating the task of slide distribution and by facilitating filing and retrieving slides.[1]
With the refinement of whole slide imaging (WSI) technology and high-resolution of digital images, the time is ripe to examine the accuracy of WSI as the first line diagnostic tool. There are no current guidelines, however, for the use of WSI as a primary diagnostic tool in pathology and hence, validation is needed before it could be incorporated in the clinical practice.[1,13,14,15] This requires comparison of intra-observer variability for WSI with that of microscopic evaluation of glass slides. In this study, the intrapathologist diagnostic reproducibility of WSI was compared to conventional microscopy (CM) in core needle biopsies of the breast. Determination of inter-observer variability was not the goal of this study.
MATERIALS AND METHODS
One hundred and three consecutive core needle biopsies of the breast from the files of Department of Pathology at the University of Miami, Jackson Memorial Medical Center were subjects of this study. The study coordinator selected one representative slide from each case for both CM and WSI. In some cases where there was more than one level on a single slide, all levels were scanned. The coordinator assigned random numbers to each case. Only H and E, slides were selected for microscopic review and digital imaging. In those cases where immunohistochemical (IHC) staining for diagnostic or predictive markers were performed, the IHC slides were excluded from the review process.
Three board certified pathologists independently reviewed the H and E slides by CM and whole slide digital imaging. The three observers were all general surgical pathologists with experiences ranging from 5 years to 35 years. None of the pathologists had used WSI for primary diagnostic purposes before but had utilized the system for presentation at teaching conferences and tumor boards. Each pathologist initially, evaluated the glass slides of all cases by light microscopy (CM1) without the knowledge of the original pathologic diagnosis. In the next phase of the study, and following an interval period of 2-3 weeks, the glass slides with new random numbers were reviewed for the 2nd time by conventional light microscopy (CM2) to establish each pathologist's baseline reproducibility by CM. In the next step, the slides were assigned another set of random numbers and scanned at ×20 by BioImagene iScan Coreo Au (Ventana Medical System, Tucson, AZ). After a period of 2-3 weeks, each pathologist independently reviewed the digitalized images on his/her PC monitor accessed from the shared file. The diagnosis of the first and the second review by CM (CM1 and CM2) and by the WSI were tabulated for each observer by the study coordinator. The diagnostic disagreements between CM1 versus CM2, and CM1 versus WSI were calculated using the mean proportion differences. The assessment of inter-pathologist reproducibility was not the purpose of this study.
RESULTS
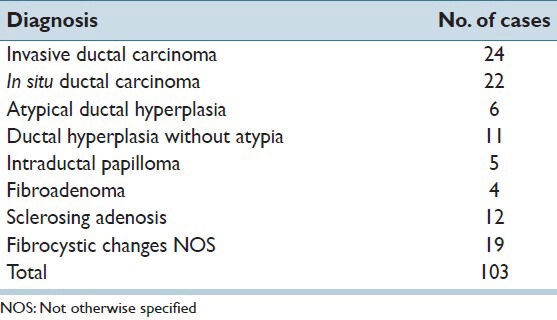
Among the 103 core needle biopsies, were 24 invasive ductal carcinomas, 22 in situ ductal carcinoma, 6 cases of atypical ductal hyperplasia, 11 cases of ductal hyperplasia without atypia, 5 intraductal papillomas, 4 fibroadenomas, 12 cases of sclerosing adenosis and 19 examples of fibrocystic changes not further characterized [Table 1].
Table 1.
The original histologic diagnosis of 103 consecutive core needle biopsies of breast included in this study
The baseline intra-observer variability for the first CM versus the second CM was 4%, 7%, and 0% for pathologist 1, 2, and 3 respectively. When the CM1 diagnoses were compared to the WSI diagnoses, the variability for the observers was 1%, 4%, and 1% [Table 2]. All intra-pathologist disagreements were between the diagnoses of ductal hyperplasia versus atypical ductal hyperplasia. On the basis of H and E slide alone the observers had the same differential diagnostic difficulty with conventional microscope and WSI. No other diagnostic issues were observed that were specific to WSI. Interestingly, most of these cases were originally signed out with the aid of immunohistochemistry for p63 and high molecular weight cytokeratin. There were no significant differences between CM1 versus CM2 compared to WSI versus CM1 for individual observer or for the three pathologists as a group [Table 2].
Table 2.
Intra-observer variability for glass slide and whole-slide images*
DISCUSSION
Although, WSI has been in use for more than a decade, its principal utility has been for telepathology consultation, education, and quality assurance. The application of the technique to primary diagnosis in surgical pathology has been rather slow. Among the reasons for the delayed implementation of WSI in diagnostic surgical pathology one could name technical and regulatory factors as well as hesitation by the pathology community to accept WSI as a viable alternative to conventional glass slide microscopy. Some of the initial technical shortcomings of the WSI such as long scan time and insufficient image resolution have been overcome to a considerable degree in the past few years. What remains is the validation of WSI for primary diagnostic purposes to satisfy the strict requirements by the regulatory bodies and eventually by practicing pathologists.
Recent studies have showed that, WSI could be an acceptable alternative to CM.[14,16,17,18,19,20] Gilbertson et al., showed that using whole slide images in complex cases was sufficient for pathologists to make reliable diagnostic decisions.[14] Two other recent studies have also shown the use of WSI for the diagnosis of prostate specimens. Rodriguez-Urrego, et al. demonstrated that interpretation of prostate needle biopsies by WSI simulates routine microscopy in the assessment of histologic grade, perineural invasion, and tumor volume.[20] Similarly, Chargari, et al., showed that virtual microscopy is comparable to regular microscopy as a primary diagnostic tool for prostate needle biopsies.[21] Interestingly, these authors also reported that, WSI improves the accuracy of Gleason's grading of prostate adenocarcinomas.
More recently, Jukic, et al., estimated the intra-pathologist diagnostic discrepancy between glass slides and digital slides in 296 cases from various organ systems.[22] They did not detect any significant differences between the diagnoses that were based on digital images and those on glass slides. Similar studies by Al-Janabi, et al., have showed the feasibility of WSI utilization in the initial diagnosis of gastrointestinal biopsies.[23]
The present study was focused exclusively on the assessment of the intra-observer reproducibility of WSI for the primary diagnosis of breast core biopsies. An initial routine light microscopic review by each of the three pathologists was followed by a second review to establish their respective baseline diagnostic reproducibility. This was followed in 2-3 weeks, by review of the digitalized whole slide images. The reproducibility of each observer was compared to his/her baseline variability established by CM. The result showed that there were no significant differences in the reproducibility rates between the two platforms for each pathologist and for the whole group. In other words, the observers’ performance was same by WSI and CM for the primary diagnosis of breast lesions on core needle biopsies. The diagnostic disagreements for both CM and WSI were between ductal hyperplasia and atypical ductal hyperplasia; a differential that was originally resolved by IHC for basal/myoepithelial cell markers. Although, the pathologists expressed desire to review IHC slides, the study design was for H and E slides only.
In 2012, Al-Janabi, et al., studied the concordance between the light microscopic diagnoses and the whole slide images on 100 breast specimens that included biopsies, resections, and mammoplasty samples. The cases were originally diagnosed by a single breast pathologist who also reviewed the digital images after a washout period of 6 months. The diagnoses were concordant in 93% of cases and slightly discordant, with no clinical significance, in 6% of cases. In the single remaining case with potentially prognostic implications, however, no final consensus could be reached when the slides were reviewed by a panel of breast pathologists.[24]
The possibility of recall bias always exits when pathologists re-review previously examined slides. For the same reason, washout periods ranging from a few weeks to several months have been suggested for the repeat review. Although, we cannot completely rule out the possibility of recall bias in this study we feel that if there was any, it should have been the same for CM1 versus CM2, as the reviews were within similar time spans of WSI versus CM1.
Recently the College of American Pathologists (CAP) assembled a Digital Pathology Work Group, to explore the requirements to validate a WSI system before it is utilized in clinical practice and to reduce the potential risk of misdiagnosis when this technology is used. The CAP group developed a number of statements that were placed online for public comments. Most respondents agreed with the CAP statements for validation of WSI for clinical diagnostic purposes, including adequate storage capacity and interface with the laboratory information systems.[1] In addition to standardization of technical platforms, and establishment of intra-pathologist reproducibility for WSI, other factors that may potentially delay its routine use include the pathologists’ level of comfort and its acceptance as an alternative to CM. Our results and those published by others supports the notion that properly validated WSI platforms could be used for routine first line diagnosis.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2014/5/1/5/127814
REFERENCES
- 1.Pantanowitz L, Valenstein PN, Evans AJ, Kaplan KJ, Pfeifer JD, Wilbur DC, et al. Review of the current state of whole slide imaging in pathology. J Pathol Inform. 2011;2:36. doi: 10.4103/2153-3539.83746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rocha R, Vassallo J, Soares F, Miller K, Gobbi H. Digital slides: Present status of a tool for consultation, teaching, and quality control in pathology. Pathol Res Pract. 2009;205:735–41. doi: 10.1016/j.prp.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein RS, Graham AR, Richter LC, Barker GP, Krupinski EA, Lopez AM, et al. Overview of telepathology, virtual microscopy, and whole slide imaging: Prospects for the future. Hum Pathol. 2009;40:1057–69. doi: 10.1016/j.humpath.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Harnden P, Coleman D, Moss S, Kodikara S, Griffin NR, Melia J. Evaluation of the use of digital images for a national prostate core external quality assurance scheme. Histopathology. 2011;59:703–9. doi: 10.1111/j.1365-2559.2011.03987.x. [DOI] [PubMed] [Google Scholar]
- 5.Ho J, Parwani AV, Jukic DM, Yagi Y, Anthony L, Gilbertson JR. Use of whole slide imaging in surgical pathology quality assurance: Design and pilot validation studies. Hum Pathol. 2006;37:322–31. doi: 10.1016/j.humpath.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Koch LH, Lampros JN, Delong LK, Chen SC, Woosley JT, Hood AF. Randomized comparison of virtual microscopy and traditional glass microscopy in diagnostic accuracy among dermatology and pathology residents. Hum Pathol. 2009;40:662–7. doi: 10.1016/j.humpath.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Leong FJ, McGee JO. Automated complete slide digitization: A medium for simultaneous viewing by multiple pathologists. J Pathol. 2001;195:508–14. doi: 10.1002/path.972. [DOI] [PubMed] [Google Scholar]
- 8.Singson RP, Natarajan S, Greenson JK, Marchevsky AM. Virtual microscopy and the internet as telepathology consultation tools. A study of gastrointestinal biopsy specimens. Am J Clin Pathol. 1999;111:792–5. doi: 10.1093/ajcp/111.6.792. [DOI] [PubMed] [Google Scholar]
- 9.Wilbur DC, Madi K, Colvin RB, Duncan LM, Faquin WC, Ferry JA, et al. Whole-slide imaging digital pathology as a platform for teleconsultation: A pilot study using paired subspecialist correlations. Arch Pathol Lab Med. 2009;133:1949–53. doi: 10.1043/1543-2165-133.12.1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winokur TS, McClellan S, Siegal GP, Redden D, Gore P, Lazenby A, et al. A prospective trial of telepathology for intraoperative consultation (frozen sections) Hum Pathol. 2000;31:781–5. doi: 10.1053/hupa.2000.8452. [DOI] [PubMed] [Google Scholar]
- 11.Dee FR. Virtual microscopy in pathology education. Hum Pathol. 2009;40:1112–21. doi: 10.1016/j.humpath.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Kumar RK, Velan GM, Korell SO, Kandara M, Dee FR, Wakefield D. Virtual microscopy for learning and assessment in pathology. J Pathol. 2004;204:613–8. doi: 10.1002/path.1658. [DOI] [PubMed] [Google Scholar]
- 13.Dee FR, Lehman JM, Consoer D, Leaven T, Cohen MB. Implementation of virtual microscope slides in the annual pathobiology of cancer workshop laboratory. Hum Pathol. 2003;34:430–6. doi: 10.1016/s0046-8177(03)00185-0. [DOI] [PubMed] [Google Scholar]
- 14.Gilbertson JR, Ho J, Anthony L, Jukic DM, Yagi Y, Parwani AV. Primary histologic diagnosis using automated whole slide imaging: A validation study. BMC Clin Pathol. 2006;6:4. doi: 10.1186/1472-6890-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molnar B, Berczi L, Diczhazy C, Tagscherer A, Varga SV, Szende B, et al. Digital slide and virtual microscopy based routine and telepathology evaluation of routine gastrointestinal biopsy specimens. J Clin Pathol. 2003;56:433–8. doi: 10.1136/jcp.56.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Janabi S, Huisman A, Nap M, Clarijs R, van Diest PJ. Whole slide images as a platform for initial diagnostics in histopathology in a medium-sized routine laboratory. J Clin Pathol. 2012;65:1107–11. doi: 10.1136/jclinpath-2012-200878. [DOI] [PubMed] [Google Scholar]
- 17.Cornish TC, Swapp RE, Kaplan KJ. Whole-slide imaging: Routine pathologic diagnosis. Adv Anat Pathol. 2012;19:152–9. doi: 10.1097/PAP.0b013e318253459e. [DOI] [PubMed] [Google Scholar]
- 18.Isaacs M, Lennerz JK, Yates S, Clermont W, Rossi J, Pfeifer JD. Implementation of whole slide imaging in surgical pathology: A value added approach. J Pathol Inform. 2011;2:39. doi: 10.4103/2153-3539.84232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nelson D, Ziv A, Bandali KS. Going glass to digital: Virtual microscopy as a simulation-based revolution in pathology and laboratory science. J Clin Pathol. 2012;65:877–81. doi: 10.1136/jclinpath-2012-200665. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Urrego PA, Cronin AM, Al-Ahmadie HA, Gopalan A, Tickoo SK, Reuter VE, et al. Interobserver and intraobserver reproducibility in digital and routine microscopic assessment of prostate needle biopsies. Hum Pathol. 2011;42:68–74. doi: 10.1016/j.humpath.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Chargari C, Comperat E, Magné N, Védrine L, Houlgatte A, Egevad L, et al. Prostate needle biopsy examination by means of virtual microscopy. Pathol Res Pract. 2011;207:366–9. doi: 10.1016/j.prp.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Jukiæ DM, Drogowski LM, Martina J, Parwani AV. Clinical examination and validation of primary diagnosis in anatomic pathology using whole slide digital images. Arch Pathol Lab Med. 2011;135:372–8. doi: 10.5858/2009-0678-OA.1. [DOI] [PubMed] [Google Scholar]
- 23.Al-Janabi S, Huisman A, Vink A, Leguit RJ, Offerhaus GJ, ten Kate FJ, et al. Whole slide images for primary diagnostics of gastrointestinal tract pathology: A feasibility study. Hum Pathol. 2012;43:702–7. doi: 10.1016/j.humpath.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Al-Janabi S, Huisman A, Willems SM, Van Diest PJ. Digital slide images for primary diagnostics in breast pathology: A feasibility study. Hum Pathol. 2012;43:2318–25. doi: 10.1016/j.humpath.2012.03.027. [DOI] [PubMed] [Google Scholar]


