Abstract
Five midsagittal pelvic reference lines have been employed to quantify prolapse using MRI. However, the lack of standardization makes study results difficult to compare. Using MRI scans from 149 women, we demonstrate how use of existing reference lines can systematically affect measurements in three distinct ways: in oblique line systems, distances measured to the reference line vary with antero-posterior location; soft issue-based reference lines can underestimate organ movement relative to the pelvic bones; and systems defined relative to the MR scanner are affected by intra- and interindividual differences in the pelvic inclination angle at rest and strain. Thus, we propose a standardized approach called the Pelvic Inclination Correction System (PICS). Based on bony structures and the body axis, the PICS system corrects for variation in pelvic inclination, at rest of straining, and allows for the standardized measurement of organ displacement in the direction of prolapse.
Keywords: Female, MRI, Pelvic floor, Pelvic organ prolapse, Pelvic reference lines, Pelvic tilt
Evaluation of the current measurement systems
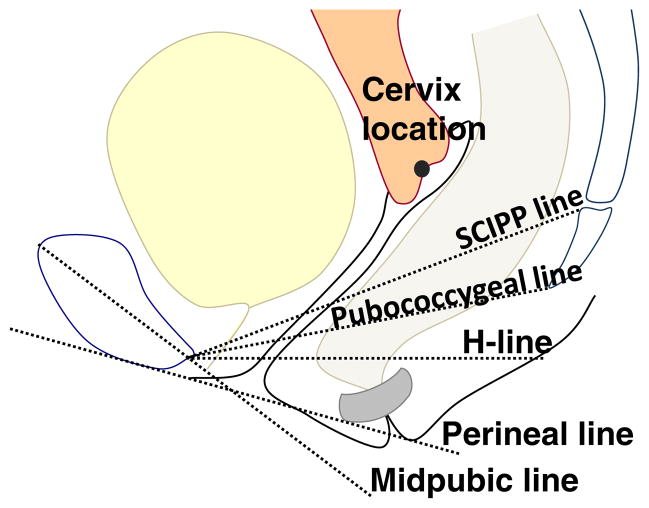
The fundamental nature of pelvic organ prolapse (POP) is a downward displacement of the pelvic organs from their normal location. With advances in soft tissue imaging, it has become possible to record this movement and make measurements of organ location and displacement [1–4], thereby permitting the quantitative assessment of structural relationships [5]. At least five different reference systems have been described (Fig. 1) and used to measure the extent of prolapse, as recently summarized by Broekhuis et al. [5].
Fig 1.
The five most commonly used reference lines. SCIPP sacrococcygeal–inferior pubic point line, H-line horizontal line
The lack of consensus regarding which reference system to use and how they relate to one another makes it difficult to compare data from different studies. Other scientific disciplines, most notably brain imaging, have reached a consensus on reference systems and measurement strategies so that data from different studies can be compared [6]. In this article we analyze the strengths and weaknesses of the current pelvic reference systems and, based on these, suggest a standardized measurement system for evaluating prolapse using MRI.
An optimal pelvic reference system for comparing anatomy in different individuals should allow investigators to make unbiased measurements appropriate to the type of assessment required. To accomplish these goals in prolapse, desirable attributes of the reference system should permit measurements having:
One axis parallel to the direction of prolapse displacement, namely the whole body axis.
One axis perpendicular to the body axis based on bony landmarks that do not change their special relationship with movements of the pelvis during maneuvers known to increase prolapse, such as the Valsalva maneuver.
Landmarks that are easily identifiable in the field of view.
It is widely recognized that the angle of pelvic inclination can change during specific maneuvers such as the Valsalva and Kegel maneuvers. This angle can also be affected by the way that an individual lies in the scanner (e.g., knees supported versus legs extended). The optimal pelvic reference system should allow the investigator to compensate for these variations. In addition, the reference system should allow for measurements that are appropriate to the structure and movement to be studied. Inherently, how “high” or “low” a uterus lies describes a movement in the direction of gravity along the body axis; thus, a reference system based on the body axis has biological meaning.
We will first evaluate the strengths and weaknesses of the five different pelvic reference systems and characterize their attributes before proposing a system that combines positive attributes from several of these systems.
Characteristics of oblique midsagittal pelvic reference line systems
The first reference line to be used in MR imaging study was a line extending from the most inferior portion of the symphysis pubis to the tangent of the last coccygeal joint called the “pubococcygeal line” (PCL) [1] (Fig. 1). Points of interest were measured as a vertical distance1 to the reference line [1, 7]. In choosing this line the authors noted that the coccyx area was the attachment point for important components of the pelvic floor: “Also, components of the pelvic floor, such as the pubococcygeal muscle, puborectal muscle, and pubovesical ligament, attach along this line” [1]. The line approximates the plane of the levator plate. A similar line, the “pubosacral line” (PSL) [8], extending from the inferior pubic symphysis to the tip of the sacrum (S5), was introduced to focus on posterior levator sling insertion. Finally, the sacrococcygeal joint [9] or the anterior margin of the sacrococcygeal junction [10] became the reference point for the “sacrococcygeal inferior–pubic point line” (SCIPP line); a line that had been in use since 1969 for interpreting the voiding lateral cystourethrogram [11]. The sacrococcygeal articulation was suggested rather than the coccyx because of the variability in the angle and length of the coccygeal vertebrae, and also because this landmark is more consistently visible in the sagittal plane. The pubosacral and SCIPP lines use slightly different aspects of the sacrococcygeal articulation for point placement; this fact becomes important when inter-rater reliability is assessed.
These oblique reference lines use bony landmarks that are typically visible on scans containing the pelvic organs. Because they are based on the bony pelvis, rather than the orientation of the scanner, these lines can help compensate for different pelvic angles that can arise when women lie in the scanner with different degrees of pelvic flexion, which can also change during maneuvers such as the Valsalva maneuver. These lines, however, have the disadvantage that the distance measured to a reference line that lies oblique to the body axis will differ depending on the ventro-dorsal location of the organ of interest in the midsagittal plane (Fig. 2a). In addition, studies have reported different conventions in measuring to the oblique reference line with some making measurements perpendicular to the line and others measuring parallel to the body axis (Fig. 2b) [1, 7, 12].
Fig 2.
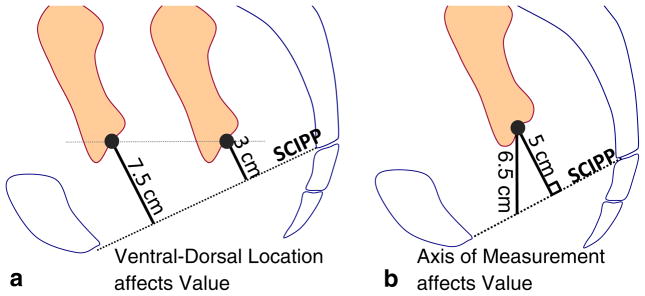
a The “height” of a landmark from an oblique reference line is always affected by ventro-dorsal location. b The difference between a vertically (Yang 1991) and perpendicularly (Agildere 2003) measured distance from an oblique reference line. SCIPP sacrococcygeal–inferior pubic point line
With the advent of the POP-Q system in 1996, clinical measurements of pelvic organ position during pelvic examination used the hymenal ring as a reference line [13]. This led to the development of the “midpubic line” (MPL) [2] in order to correspond more closely to the location of the hymen than earlier systems that used the pubic bone and distal sacrococcygeal landmarks. The MPL is drawn across the midsagittal aspect of the pubic bone through the approximate level of the vaginal hymen. Use of the MPL was shown to correlate with POP-Q staging (in 15 out of 20 cases, or 75 %, the MRI correlated with clinical staging; κ = 0.61) [2]. The problems of using a reference line oblique to the direction of prolapse movement are similar to those outlined above for lines from the pubis to the sacrum.
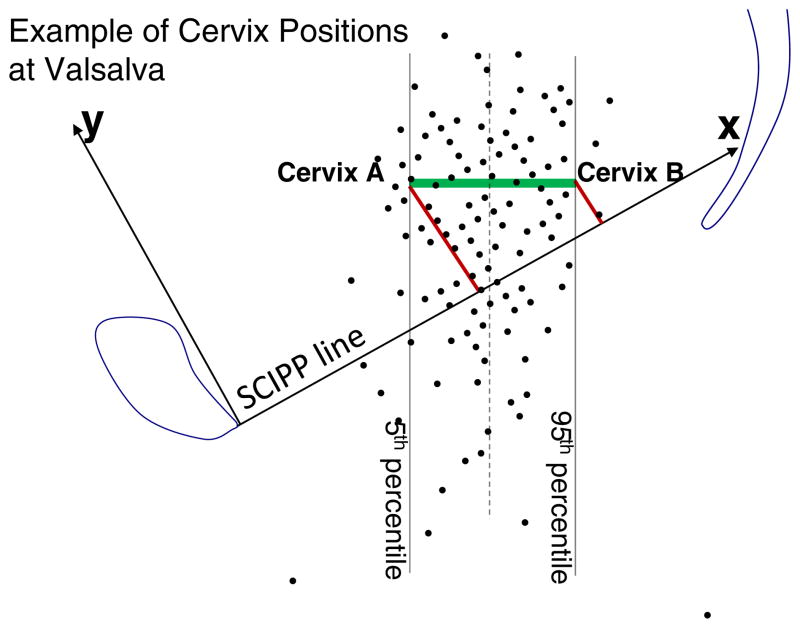
To illustrate the magnitude of measurement bias introduced using an oblique line reference system such as the SCIPP line, we used a sample of 149 MRI scans of women with and without prolapse drawn from a prior study of cervix location during maximal Valsalva maneuver [14] that provides details of the population and technique. To summarize this in brief, the eligible women had a mean age of 53.4±12.6 years, parity of 2.7±1.8, and a BMI of 26.4±4.5. Women had not undergone any prior surgery for POP. All patients had a pelvic magnetic resonance (MR) scan performed in the supine position. MR imaging was performed on a 1.5-Tesla system (Signa; General Electric, Milwaukee, WI, USA) using a four-channel torso phased array coil. For dynamic imaging, a multiphase, single-level image of the pelvis in the midsagittal plane was obtained approximately every second for 23 to 27 s using a T2-weighted single-shot fast spin-echo (SSFSE) sequence (TR: 1,300 ms, TE: 60 ms, slice thickness: 6 mm, field of view 32–36 cm, matrix: 256 × 160, 1 excitation and half-Fourier acquisition). Patients were instructed in straining maneuvers to be performed during the examination starting from minimal to maximal straining. The cervix location was measured in a Cartesian coordinate system using the inferior pubic point as the origin, the SCIPP line as the x-axis, and a line perpendicular to the SCIPP line through the inferior pubic point as the y-axis (Fig. 3). These data show the variation in anterior and posterior locations of the cervix in these women.
Fig 3.
The points represent the distribution of 149 cervix locations at maximum strain for an average θ-SCIPP line strain angle of 29°. Note that two cervices from this sample have the same cranio-caudal location, but different antero-posterior locations, so in the oblique reference system (SCIPP) the y coordinates will vary. The difference (Δ) in the “vertical” distance, v, is given by Δ v=Δ x * sin (θ). In this data set, Δx between the 5th and 95th percentiles of the horizontal cervix distribution was 3.3 cm, which resulted from a 1.6-cm difference in the y coordinate
The bias introduced by measuring to an oblique reference line is demonstrated in Fig. 3. The scatter plot shows the cervix locations at the Valsalva maneuver in our MRI study. The SCIPP and MPL were similarly affected by antero-posterior organ location, but in different directions.
Characteristics of reference lines systems based on soft tissue landmarks
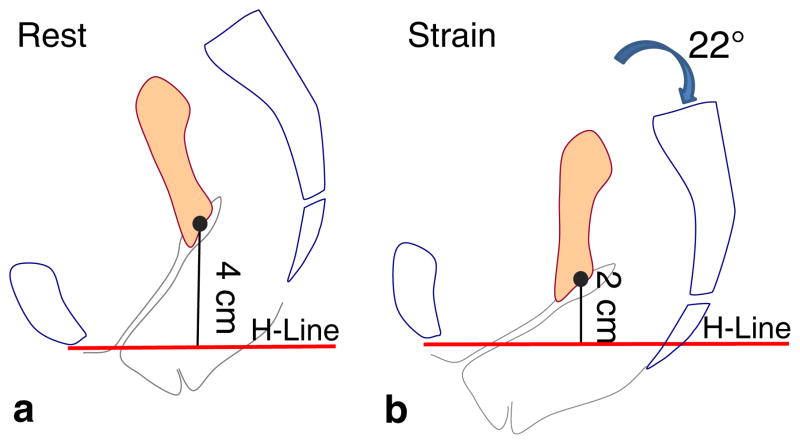
The “perineal line” (PL) system was introduced as an attempt to more closely simulate the reference system used during a POP-Q examination in the clinic [4]. The authors recognized that one source of the differences between POP-Q measurements and the midpubic line lay in the fact that the hymenal ring, used clinically as a landmark, moved with the perineal structures during the Valsalva maneuver. To address this, they employed a tangent from the internal surface of the symphysis pubis to the caudal end of the external anal sphincter (Fig. 1). The Pearson coefficient for correlation of MRI with clinical prolapse in the PL system was 0.74 for point Ba, 0.80 for point C, and 0.49 for perineal body length [4]. However, despite the fact that the PL line method more closely resembles clinical measurements, incorporating a moving soft-tissue landmark as part of the reference system introduces additional variability during maneuvers such as the Valsalva maneuver (Fig. 4) because PL moves relative to the bony pelvis between rest and the Valsalva maneuver. Measurements made relative to the PL are similar to clinical measurements that are also subject to movement of the hymenal ring. In Fig. 4 the location of the cervix relative to the PL system is shown in panel a at rest and Panel b at maximum strain. The difference implies a movement of the cervix measuring 0.5 cm (4.7 cm to 4.2 cm), but the cervix actually moved 2 cm from rest to strain in a caudal direction. Hence, it was the 17° difference in PL orientation between Fig. 4a and b that accounts for the difference between the perceived and real movement of the cervix.
Fig 4.
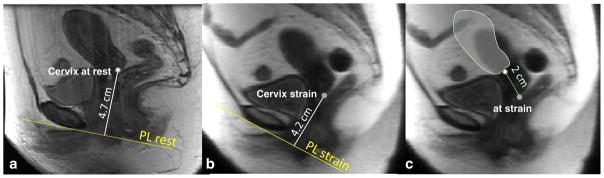
Localization of the cervix using the perineal line system in a woman a at rest and b at maximum strain. The results imply a movement of 0.5 cm (4.7 cm vs 4.2 cm respectively), whereas c the caudal movement of the cervix actually measured 2 cm. PL perineal line
Characteristics of reference line systems based on the MR scanner axis
The “H-line” or “horizontal line” [3] was introduced as a way to measure the distance to the organs of interest from a line parallel to the bottom edge of the MR image and tangential to the inferior rim of the pubic bone (Fig. 1). This line has the advantage that it is roughly perpendicular to the direction in which prolapse occurs and is easy to move. In addition, unlike the oblique lines discussed previously, the ventro-dorsal location of the organs does not affect their measured cranio-caudal location.
When a woman lies on the MR scanner bed her whole-body axis is aligned with the bed and the bore of the machine; the H-line is therefore oriented perpendicular to this axis, allowing measurements to tell how “high” or “low” an organ is relative to the body axis. This fact has biological and functional significance. When a person is standing and the whole-body axis is oriented parallel to the gravity field, the direction in which prolapse occurs, the H-line is then “horizontal” and provides a relevant reference plane for determining how much of the amount a structure has descended is not affected by the oblique line issue.
While the H-line is convenient and relevant to the movement to be studied, it does not take into account the change in the orientation of the pelvis that occurs, for example, between rest and strain. In addition, differences in the pelvic angle can exist if one radiology department places a support under the knees while another does not. As an example, Fig. 5 shows rotation of the pelvis without any change in the position of the uterus relative to the pelvic bones, as might happen in an individual with normal pelvic organ support who rotates her pelvis from rest during a full Valsalva maneuver. Although the pelvic anatomy is identical, it is a shortcoming that pelvic rotation leads to different measurements relative to the H-line during the Valsalva maneuver.
Fig 5.
A pelvic rotation of 22° about the pubic symphysis affects measured distances to the H-line between a rest and b maximum strain, even though the relationship between the uterus and pelvic bones is identical in the two images
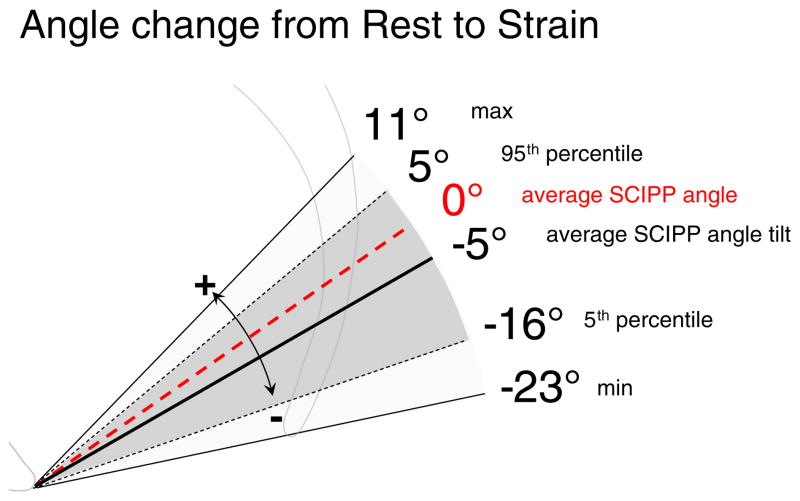
To assess whether or not the magnitude of this shift from rest to strain was of significance, we measured the changes in the angle of the SCIPP line relative to the horizontal at rest and strain from the MRIs of the 149 women described above (Fig. 6). The angle between the SCIPP line and horizontal varied by 29° at rest and by 45° during maximal Valsalva maneuver. In comparing the averages there was a 5° difference between the average location at rest (34°) and at the Valsalva maneuver (29°) resulting in an overall clockwise rotation (i.e., flexion) during straining. The change in pelvic inclination between rest and strain is shown in Fig. 7. Some women exhibited as much as a 23° pelvic flexion from rest to Valsalva maneuver. This indicates a wide range of pelvic angles both at rest and strain as well as changes in pelvic inclination.
Fig 6.
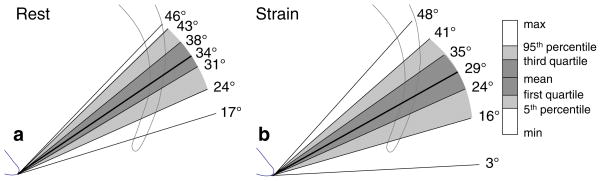
Variation of SCIPP line inclination angles a at rest and b strain in 149 women
Fig 7.
Change in SCIPP line inclination from rest to strain in 149 women performing the Valsalva maneuver. Counterclockwise direction is designated “+” (pelvic extension) and clockwise direction “−” (pelvic flexion)
Proposal for a new reference line system: the Pelvic Inclination Correction System
We propose a Pelvic Inclination Correction System (PICS) that builds on the advantage of a line perpendicular to the whole body axis that allows determination of the cranio-caudal location of an organ along the body axis, while adjusting for changes in pelvic inclination.
We define the PICS as a local pelvic coordinate system with its origin in the mid-sagittal plane on the arcuate pubic ligament. The x-axis points posteriorly along the SCIPP line, but is rotated 34° clockwise (see next paragraph) about its origin (Fig. 8) so that it is, on average, perpendicular to the body axis. The y-axis points cranially. We define the PICS “line” as the x-axis of the system. These conventions are consistent with the use of the whole body axis as well as the internationally accepted use of a right-handed, Cartesian coordinate system when making kinematic measurements [15].
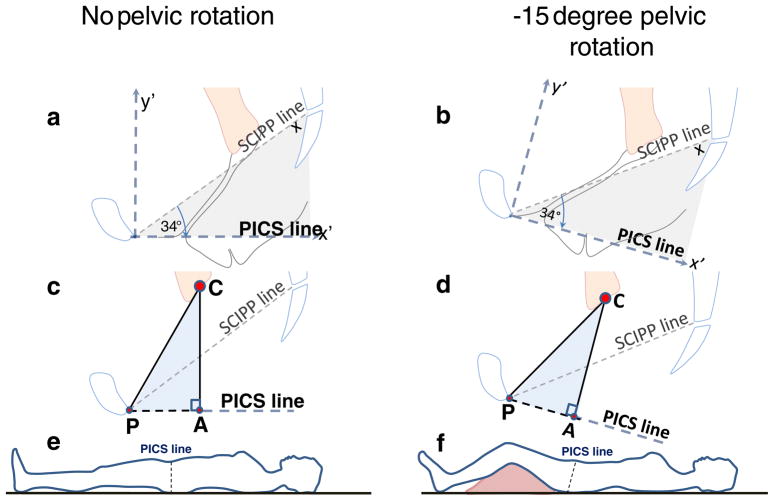
Fig 8.
Example of how the Pelvic Inclination Correction System (PICS) corrects for a −15° pelvic rotation caused by knee support, on the right. a A right-handed local pelvic coordinate system, xy, is located with its origin at the inferior pubic point and its positive x-axis oriented cranio-dorsally along the SCIPP line. A corresponding local coordinate system, x’y’, is defined with the same origin, but with its x-axis rotated −34° from the SCIPP line in the mid-sagittal plane, so that its y’-axis lies along the whole body and scanner axis. b When the pelvis is rotated by a knee support (e to f), the pelvis rotates through −15° carrying the PICS line with it. c, d Note that the dimensions of the triangle PCA do not change because of the pelvic rotation of −15°. P inferior pubic bone point, C cervix, A, intersection of the perpendicular line from the organ to the PICS line. e, f The PICS line rotates when the pelvis rotates
The angle of 34° is based on the average value, measured on the above 149 MRIs, between the SCIPP line and the longitudinal body axis established by the scanner bed (Fig. 6a). As such it approximates the H-line; however, by definition, the PICS line has a fixed angular relationship to the bony pelvis SCIPP line, regardless of the position of the pelvis in the scanner or changes in pelvic inclination that occur between rest and strain. Using this system, the values along the y-axis correspond to how “high” or “low” an organ is along the line of the body axis in which prolapse occurs. Similarly, the x-value corresponds to the anterior–posterior location of the point of interest. In this way, it is possible to determine both of these physiologically relevant measures with a system that adjusts for different degrees of pelvic inclination. This system can also be used as a full three-axis right-handed coordinate system for use in assessing spatial locations in a 3-D volume. In this case, the origin (0, 0, 0) would still pass through the inferior pubic point, the horizontal plane would, again, be 34 degrees below the SCIPP line and a line between the ischial spines or femoral heads would be used to establish transverse plane orientation.
Discussion
The PICS system builds on the advantages of earlier reference systems, and it provides measurements that are not only relevant to the biology of prolapse, but are also salient when considering the action of gravity and increases in abdominal pressure when the individual is upright.
Several factors deserve consideration in evaluating this system. One concerns the assumption that alignment of the pelvic axis with a woman lying on her back in the scanner is similar to that of a standing woman. To test this assumption we compared the pelvic angle in our subjects with published data on pelvic inclination acquired from radiographs made in the standing position [16]. These measures are based on a line from the middle of the sacral promontory to a line between the femoral heads. We computed this angle in 50 women (25 controls, 25 with prolapse) from the Summers cohort [14]. We found our average was 10.6°±5.6° (SD) and compared it with the mean of 160 volunteers in a standardized standing position (12.0°± 6.5°) [16]. The 1.4° difference was not statistically different (p =0.86). In addition, the 34° adjustment we use represents an average value, and individuals can of course vary from this pelvic orientation angle. However, this variation is modest (standard deviation of 6.5°) [16], but, if necessary, the angle of each woman’s pelvis can be determined for research purposes and analyzed separately.
An important issue concerning any reference system is addressing interobserver variability. Broekhuis et al. showed an excellent to good intra- and interobserver reliability of MR imaging measurements for the pubococcygeal line, the H-line, and the midpubic line in a dynamic magnetic resonance imaging study [17]. The pubococcygeal line showed the highest reliability (ICC range 0.70–0.99). It is likely that the reproducibility of the PICS line would be similar to that of the pubococcygeal line as they share some properties.
The PICS line is a new theoretical concept that is aimed at solving problems with oblique reference lines and the pelvic movement. Its practical applicability in comparison to existing lines and the correlation with symptoms or clinical examination in a standardized manner will require careful study. Future directions for research also include confirmation of average SCIPP line angles at rest and strain in larger samples from a more diverse population.
Acknowledgments
We acknowledge the support of Prof. Alejandro Uribe, Department of Mathematics, University of Michigan for his revision of the trigonometry solution and Aimee Summers PhD, Bloomberg School of Public Health, John Hopkins University, Baltimore for the coordinate data for the cervix localization.
Funding NIH Grants RO1 HD 38665 and P50 HD 44406, Grant of the Swiss National Science Foundation.
Appendix
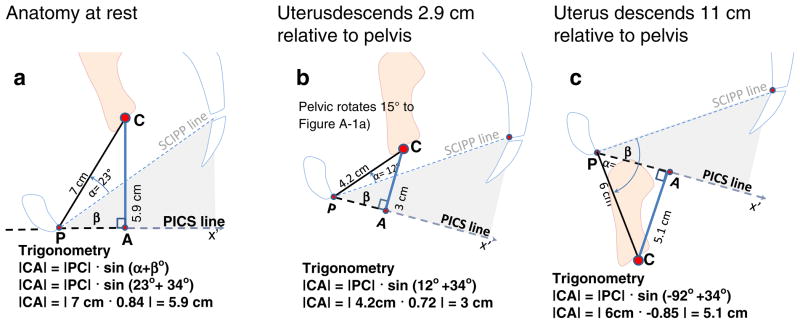
In practice, the distance of an organ to the PICS line is easily established with the absolute value of a trigonometric function. For example, to obtain the distance, |CA|, of an organ, C, to the PICS line (Fig. 8), one distance, |PC| and one angle (α) are needed:
where angle α is the angle from the SCIPP line to the segment PC (Fig. 9).
Fig 9.
Examples of measuring the distance of the cervix from the PICS line at rest and at maximum strain. a Measuring the distance of the cervix, C, to the PICS line at rest, b) with mild descent, and c with severe prolapse. Note that the location of C in PICS has a positive-valued y’ coordinate in a and b, and a negative-valued y’ coordinate in c, as governed by the sign of angle α and the expression y’= |PC| sin (α). β=34°
Similarly, the distance along the PICS line, |PA|, can be found, knowing the distance PC and the cosine of the above angle.
Examples of the measurement are provided in Fig. 9. An easy way to make these calculations is by using the free NIH-sponsored image measurement tool Image J 1.44o. We place x, y coordinates at the points of interest and then calculate the distances and angles. Information about this approach can be obtained from the corresponding author.
Since the PICS line is also the x’ axis of a coordinate system, the PICS offers the option of measuring the rectangular coordinates of an organ within that coordinate system (Figs. 8, 9), while compensating for the intraindividual change in pelvic rotation between rest and strain as well as interindividual differences in pelvic inclination.
Footnotes
By international convention, images made in the sagittal plane are displayed as if an individual were in the upright position, even though the images are made with an individual in the supine position. In this commentary we will continue the established practice of referring to directions in the image, recognizing that they are perpendicular to the way in which the scan is made.
IRB approval IRB University of Michigan 2001-0475.
Conflicts of interest None.
Contributor Information
C. Betschart, Email: cornelia.betschart@gmx.ch, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, USA, Department of Gynecology, University Hospital of Zurich, Frauenklinikstrasse 10, 8091 Zurich, Switzerland
L. Chen, Department of Mechanical Engineering, University of Michigan, Ann Arbor, MI, USA
J. A. Ashton-Miller, Department of Mechanical Engineering, University of Michigan, Ann Arbor, MI, USA
J. O. L. DeLancey, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, USA
References
- 1.Yang A, Mostwin JL, Rosenshein NB, Zerhouni EA. Pelvic floor descent in women: dynamic evaluation with fastMR imaging and cinematic display. Radiology. 1991;179:25–33. doi: 10.1148/radiology.179.1.2006286. [DOI] [PubMed] [Google Scholar]
- 2.Singh K, Reid WM, Berger LA. Assessment and grading of pelvic organ prolapse by use of dynamic magnetic resonance imaging. Am J Obstet Gynecol. 2001;185:71–77. doi: 10.1067/mob.2001.113876. [DOI] [PubMed] [Google Scholar]
- 3.Lienemann A, Sprenger D, Janssen U, Grosch E, Pellengahr C, Anthuber C. Assessment of pelvic organ descent by use of functional cine-MRI: which reference line should be used? Neurourol Urodyn. 2004;23:33–37. doi: 10.1002/nau.10170. [DOI] [PubMed] [Google Scholar]
- 4.Fauconnier A, Zaeski E, Abichedid J, Bader G, Falissard B, Fritel X. Dynamic magnetic resonance imaging for grading pelvic organ prolapse according to the International Continence Society Classification: which line should be used? Neurourol Urodyn. 2007;27:191–197. doi: 10.1002/nau.20491. [DOI] [PubMed] [Google Scholar]
- 5.Broekhuis SR, Fütterer JJ, Barentsz JO, Vierhout ME, Kluivers KB. A systematic review of clinical studies on dynamic magnetic resonance imaging of pelvic organ prolapse: the use of reference lines and anatomical landmarks. Int Urogynecol J. 2009;20(6):721–729. doi: 10.1007/s00192-009-0848-3. [DOI] [PubMed] [Google Scholar]
- 6.Kall BA, Kelly PJ, Goerss S, Frieder G. Methodology and clinical experience with computed tomography and a computer-resident stereotactic atlas. Neurosurgery. 1985;17(3):400–407. doi: 10.1227/00006123-198509000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Unterweger M, Marincek B, Gottstein-Aalame N, Debatin JF, Seifert B, Ochsenbein-Imhof N, Perucchini D, Kubic-Huch RA. Ultrafast MR Imaging of the pelvic floor. AJR Am J Roentgenol. 2001;176:959–963. doi: 10.2214/ajr.176.4.1760959. [DOI] [PubMed] [Google Scholar]
- 8.Goodrich MA, Webb MJ, King BF, Bampton AE, Cameau NG, Riederer SJ. Magnetic resonance imaging of pelvic floor relaxation: dynamic analysis and evaluation of patients before and after surgical repair. Obstet Gynecol. 1993;82:883–891. [PubMed] [Google Scholar]
- 9.Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M. Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol. 1997;7:1309–1317. doi: 10.1007/s003300050294. [DOI] [PubMed] [Google Scholar]
- 10.Hodroff MA, Stolpen AH, Denson MA, Bolinger L, Kreder KJ. Dynamic magnetic resonance imaging of the female pelvis: the relationship with the pelvic organ prolapse quantification staging system. J Urol. 2002;167:1353–1355. doi: 10.1016/s0022-5347(05)65298-6. [DOI] [PubMed] [Google Scholar]
- 11.Noll LE, Hutch JA. The SCIPP line—an aid in interpreting the voiding lateral cystourethrogram. Obstet Gynecol. 1969;33:680–689. [PubMed] [Google Scholar]
- 12.Agildere AM, Tarhan NC, Ergeneli MH, Yologlu Z, Kurt A, Akgun S, Kazahan EM. MR rectography evaluation of rectoceles with oral gadopentetate dimeglumine and polyethylene glycol solution. Abdom Imaging. 2003;28:28–35. doi: 10.1007/s00261-002-0023-5. [DOI] [PubMed] [Google Scholar]
- 13.Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Obstet Gynecol. 1996;175(1):10–17. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 14.Summers A, Winkel LA, Hussain HK, DeLancey JO. The relationship between anterior and apical compartment support. Am J Obstet Gynecol. 2006;194(5):1438–1443. doi: 10.1016/j.ajog.2006.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu G, Cavanagh PR. ISB recommendations for standardization in the reporting of kinematic data. J Biomech. 1995;28:1257–1261. doi: 10.1016/0021-9290(95)00017-c. [DOI] [PubMed] [Google Scholar]
- 16.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 17.Broekhuis SR, Kluivers KB, Hendriks JC, Vierhout ME, Barentsz JO, Fütterer JJ. Dynamic magnetic resonance imaging: reliability of anatomical landmarks and reference lines used to assess pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:141–148. doi: 10.1007/s00192-008-0760-2. [DOI] [PubMed] [Google Scholar]