Abstract
Malignant ascites caused by peritoneal dissemination of gastric cancer is chemotherapy-resistant and associated with poor prognosis. We conducted a pilot study to evaluate the safety of weekly intraperitoneal injections of in vitro expanded Vγ9Vδ2 T cells together with zoledronate for the treatment of such malignant ascites. Patient peripheral blood mononuclear cells were stimulated with zoledronate (5 μmol/L) and interleukin-2 (1000 IU/mL). After 14 days culture, Vγ9Vδ2 T-cells were harvested and administered intraperitoneally in four weekly infusions. The day before T-cell injection, patients received zoledronate (1 mg) to sensitize their tumor cells to Vγ9Vδ2 T-cell recognition. Seven patients were enrolled in this study. The number of Vγ9Vδ2 T-cells in each injection ranged from 0.6 to 69.8 × 108 (median 59.0 × 108). There were no severe adverse events related to the therapy. Intraperitoneal injection of Vγ9Vδ2 T cells allows them access to the tumor cells in the peritoneal cavity. The number of tumor cells in the ascites was significantly reduced even after the first round of therapy and remained substantially lower over the course of treatment. IFN-γ was detected in the ascites on treatment. Computed tomography revealed a significant reduction in volume of ascites in two of seven patients. Thus, injection of these antitumor Vγ9Vδ2 T-cells can result in local control of malignant ascites in patients for whom no standard therapy apart from paracentesis is available. Adoptively transferred Vγ9Vδ2 T-cells do indeed recognize tumor cells and exert antitumor effector activity in vivo, when they access to the tumor cells.
Keywords: Gastric cancer, malignant ascites, peritoneal dissemination, Vγ9Vδ2 T-cell, zoledronate
Introduction
Human T cells carrying γδ T-cell receptors account for 1–5% of peripheral blood T-cells 1,2, the majority expressing the Vγ9Vδ2 receptor 3 that recognizes phosphoantigens 4,5. Recently, much attention has been paid to Vγ9Vδ2 T-cell-based cancer immunotherapy because these cells can secrete cytokines and exert potent cytotoxicity against a wide range of cancer cells 4. Direct in vivo activation of Vγ9Vδ2 T cells by nitrogen-containing bisphosphonates (NBPs) in cancer patients 6,7 as well as adoptive transfer of ex vivo expanded Vγ9Vδ2 T cells have been investigated in several clinical trials 8,9.
We have established a large-scale ex vivo expansion protocol for Vγ9Vδ2 T cells using zoledronate and interleukin-2 (IL-2) 10,11. We found that such cultured T cells retained cytokine secretion capacity and mediated cytotoxicity against a variety of cancer cell lines 10. On the basis of these findings, we conducted a clinical study in patients with advanced or recurrent non-small cell lung cancer resistant to standard therapy 12,13. The adoptive transfer of autologous Vγ9Vδ2 T cells was well-tolerated. Some clinical benefit was observed in some patients in whom Vγ9Vδ2 T-cells were able to survive and expand, and in whom plasma IFN-γ levels were elevated (but without statistical significance) 13. However, it remained to be determined whether transferred Vγ9Vδ2 T cells infiltrated into the tumor, recognized tumor cells and exerted antitumor effector functions in vivo. Therefore, we conducted a clinical study of intraperitoneal (i.p.) Vγ9Vδ2 T-cell transfer therapy for the treatment of malignant ascites caused by peritoneal dissemination of gastric cancer.
Peritoneal dissemination is frequently observed in cases of advanced gastric cancer and occurs as a consequence of direct invasion and/or metastasis 14. The presence of malignant ascites is a severe end-stage manifestation of the disease accompanied by several symptoms including nausea, appetite loss, abdominal tenderness and pain, fatigue and dyspnea, loss of proteins, and electrolyte disorders 15. Recently, systemic chemotherapy with paclitaxel or S-1 plus cisplatin has improved the treatment of unresectable or recurrent gastric cancer 16–18; i.p. chemotherapy 19 and immunotherapy, such as with catumaxomab 20, are also encouraging for the treatment of malignant ascites. However, to date, no options have been established for the management of peritoneal dissemination of ascites for patients' refractory to these treatments 15. In such cases, only palliative therapies, such as paracentesis and diuretics, are available and the prognosis is extremely poor, with a median survival time of 3–4 months 21–23.
Therefore, we undertake adoptive cell therapy by injecting autologous Vγ9Vδ2 T cells expanded ex vivo with zoledronate and IL-2 into the peritoneal cavity of patients with malignant ascites. Direct injection of these cells into the peritoneal cavity allows them access to the tumor cells, bypassing the difficulties of transferred Vγ9Vδ2 T-cell recruitment into solid tumor. Because zoledronate leads to intracellular accumulation of isopentenyl pyrophosphate (IPP)/triphosphoric acid I-adenosine-50-yl ester 3-(3-methylbut-3-enyl) ester (ApppI) in tumor cells that are then recognized by Vγ9Vδ2 T cells by blocking the mevalonate pathway 24,25, the injection of zoledronate preceded the infusion of expanded Vγ9Vδ2 T-cells (Fig. 1). Using this approach, we asked the crucial question of whether zoledronate-expanded Vγ9Vδ2 T-cells can recognize and kill tumor cells in vivo.
Figure 1.
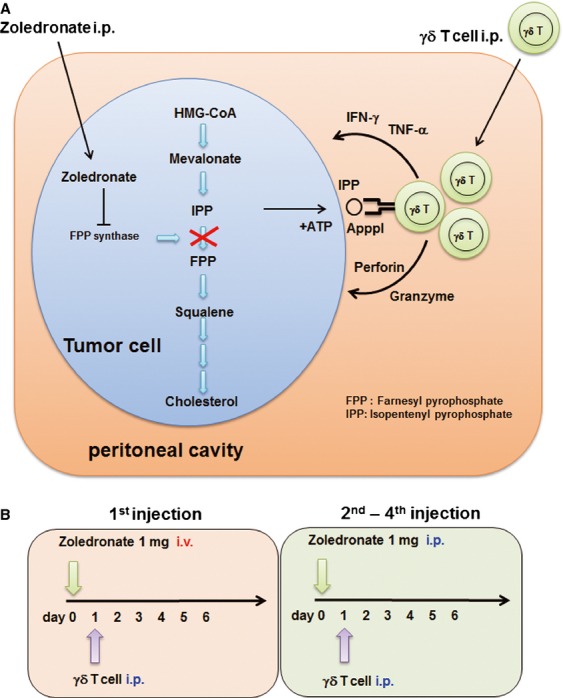
(A) Intraperitoneal administration of zoledronate sensitizes tumor cells to Vγ9Vδ2 T-cell recognition. Isopentenyl pyrophosphate (IPP) is an intermediate metabolite in the mevalonate–cholesterol pathway, recognized by Vγ9Vδ2 T-cells. Zoledronate inhibits farnesyl pyrophosphate (FPP) synthase, thereby causing the accumulation of IPP and triphosphoric acid I-adenosine-50-yl ester 3-(3-methylbut-3-enyl) ester (ApppI) in the tumor cells. When Vγ9Vδ2 T-cells are injected into the peritoneal cavity, they can recognize IPP and respond to tumor cells. (B) The study scheme of weekly i.p. Vγ9Vδ2 T-cell injection. In the first series of injections, zoledronate (1 mg) was administered i.v. on day 0, followed by i.p. Vγ9Vδ2 T-cell injection on day 1. Zoledronate was i.p. injected via a catheter from the second to fourth injection.
Materials and Methods
Study design and patient selection
This was a one-way, open-label, pilot study in patients with symptomatic malignant ascites secondary to gastric adenocarcinoma requiring symptomatic therapeutic paracentesis. The primary objective of this study was to investigate the safety of i.p. injection of autologous Vγ9Vδ2 T-cells. The secondary objectives were to obtain immunological proof-of-concept of antitumor activity of Vγ9Vδ2 T-cells and to evaluate its clinical benefit. The research protocol was approved by the Ethical Committee of our institution (IRB-ID: P2010019-11Z), and registered at the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) (Unique trial number: UMIN000004130) on August 30, 2010. Written informed consent was obtained from each patient before they entered the study. The study was performed in accordance with the Declaration of Helsinki.
To be included, patients aged ≥20 years had to have histologically or cytologically proven gastric cancer, malignant ascites, an expected survival of at least 3 months, an Eastern Cooperative Oncology Group performance status (PS) of 0–2, normal kidney, liver, and bone marrow function, and be resistant to standard therapies. Patients positive for anti-adult T-cell leukemia-associated antigen or anti-human immunodeficiency virus antibody, other primary cancers, uncontrolled infection, active enterocolitis, severe heart disease, severe drug allergy, cryoglobulinemia, or autoimmune disease, were excluded from the study. Those receiving systemic steroid therapy or who were pregnant or lactating were also excluded. Small-scale 10-day Vγ9Vδ2 T-cell culture screening tests were first performed to establish the reactivity of each patient's Vγ9Vδ2 T cells prior to entry into the study. Proliferation was assessed as Vγ9Vδ2 T-cell count on day 10 of culture/Vγ9Vδ2 T-cell count at the initiation of culture. This value had to exceed 100 for the patient to be included in the study.
When the preliminary test fulfilled the criteria described above, leukapheresis was performed to isolate autologous peripheral blood mononuclear cells (PBMCs) and harvest plasma. Small-scale culture tests and leukapheresis were performed prior to chemotherapy; PBMCs and plasma were cryopreserved and stored before use. Patients received standard chemotherapy first; Vγ9Vδ2 T-cell culture was initiated immediately when patients became resistant to the chemotherapy (Table 1). After 14 days culture, Vγ9Vδ2 T-cells were harvested and administered i.p. to the patient. Four infusions were carried out weekly. The day before Vγ9Vδ2 T-cell injection, patients received 1 mg of zoledronate (Novartis, Basel, Switzerland) (Fig. 1A). To ensure safety, zoledronate was administered intravenously (i.v.) on day 0 and i.p. via a catheter on days 7, 14, and 21 (Fig. 1B). Before each zoledronate or Vγ9Vδ2 T-cell infusion and 1 day after cell infusion, blood (10 mL) was collected and ascites fluid (50 mL) was drained from the peritoneal cavity via the indwelling catheter for immunological analysis. When the patient experienced clinical benefit without significant toxicity, additional Vγ9Vδ2 T-cell infusions were permitted.
Table 1.
Summary of patients' background
| Patient ID | Age | Gender | Surgery | Chemotherapy |
|---|---|---|---|---|
| 2305 | 69 | F | Exploratory laparotomy | TS-1/CDDP, TS-1/DOC, CPT-11/CDDP, UFT |
| 2307 | 66 | F | Total gastrectomy Roux-en-Y jejunostomy Cholecystectomy Splenectomy |
5-FU/MTX, UFT, TS-1/CDDP, DOC |
| 2319 | 58 | F | Bypass surgery | TS-1/CDDP |
| 2325 | 62 | M | Total gastrectomy Roux-en-Y jejunostomy Cholecystectomy |
TS-1/CDDP, TS-1/DOC |
| 2334 | 39 | F | Gastroduodenostomy (Billroth I) | DOC, 5-FU+MTX, UFT, TS-1/CDDP |
| 2336 | 47 | F | Bypass surgery | TS-1/CDDP, TS-1/PTX, CPT-11, PTX |
| 2328 | 55 | M | Bypass surgery | TS-1/CDDP, TS-1/DOC |
TS-1, tegafur, gimeracil, and oteracil potassium; CDDP, cisplatin; DOC, docetaxel; PTX, paclitaxel; CPT-11, irinotecan; UFT, tegafur-uracil.
Safety assessment, antitumor effects, and quality of life
Medical history, physical examination, PS, vital signs, chest X ray, electrocardiogram, and routine laboratory monitoring (including biochemistry, hematology, urinalysis, and tumor markers) were recorded at baseline. Thereafter, physical examination, PS, vital signs, and routine laboratory monitoring, as well as any adverse events, were assessed at each visit. Abdominal examination was performed by the investigator to assess ascites signs, such as abdominal distension, dullness to percussion, shifting dullness, fluid thrill, and bulging flanks. Subjective symptoms related to ascites, such as anorexia, nausea, vomiting, abdominal pain, abdominal swelling, dyspnea, fatigue, and heartburn, were also recorded. Adverse events were graded according to National Cancer Institute-Common Terminology Criteria for Adverse Events version 4.0. Clinical responses were assessed by computed tomography performed at baseline and after the fourth infusion. To evaluate the antitumor effects of the treatment on peritoneal metastasis, the amount of malignant ascites and peritoneal cytology was also taken into account 26. Cytology of ascites or peritoneal lavage fluid collected through a peritoneal access catheter was carried out using Diff-Quik staining (Sysmex, Hyogo, Japan) according to the manufacturer's instructions. The cellular components of ascites were evaluated using bright field microscopy (OLYMPUS BX41 with a Canon EOS Kiss X4 digital camera, OLYMPUS, Tokyo, Japan, magnification 200×). The safety assessment and clinical responses were determined by an independent data-monitoring committee after completion of the study.
Isolation of PBMC and Vγ9Vδ2 T-cell culture
Vγ9Vδ2 T-cell culture was performed as previously described 10,27,28. For small-scale 10-day Vγ9Vδ2 T-cell culture tests, whole blood (7.5 mL) was collected in BD Vacutainer Cell Preparation Tubes with sodium heparin (Becton-Dickinson, Franklin Lakes, NJ) and directly centrifuged to isolate PBMC. To prepare Vγ9Vδ2 T-cells for the therapy, patients underwent leukapheresis to isolate PBMC and harvest plasma using Fresenius AS.TEC204 with C4Y white blood cell set (FRESENIUS KABI, Bad Homburg, Germany). Sodium citrate (ACD-A solution; TERUMO, Tokyo, Japan) was used as the anticoagulant. PBMC and plasma were isolated by density gradient centrifugation using Lymphoprep (AXIS-SHIELD Poc AS, Oslo, Norway). Leukapheresis yielded more than 1 × 109 PBMC and 100 mL plasma, both of which were cryopreserved until use. Depending on the data from small-scale 10-day Vγ9Vδ2 T-cell culture tests, the number of PBMCs to set up large-scale Vγ9Vδ2 T-cell cultures was estimated in order to obtain more than 1 × 109 Vγ9Vδ2 T-cells for each injection. PBMC were stimulated with 5 μmol/L zoledronate in AlyS203 Vγ9Vδ2 medium (Cell Science and Technology Institute, Sendai, Japan) containing 1000 IU/mL human recombinant IL-2 (Proleukin™; Chiron, Amsterdam, The Netherlands), and 10% autologous plasma. Fresh medium containing IL-2 (1000 IU/mL) was added every 2–3 days and the cultures were transferred into new flasks or culture bags as necessitated by the degree of cell growth. Cultures were split in two to maintain cell density below 1 × 106/mL. Fourteen days after in vitro stimulation, ex vivo expanded Vγ9Vδ2 T cells were harvested and screened for their sterility (negative for endotoxin, bacteria, fungus, and mycoplasma contamination) and purity (>60%). The cytotoxic activity of the Vγ9Vδ2 T-cell cultures was evaluated against zoledronate (5 μmol/L)-pretreated Daudi cells (z-Daudi cells). Those cultured cells which were approved for use after this examination were washed twice with RPMI-1640 and resuspended in normal saline to administer to the patient.
Flow cytometry, immunofluorescence, and cytology
The following monoclonal antibodies (mAbs) were used for flow cytometry: FITC-labeled anti-CD3, -TCRVγ9, and -HLA-ABC, PE-labeled anti-TCR pan αβ, -NKG2D and mouse IgG1 isotype, PC5-labeled anti-CD3, -CD8, -CD27, -CD56, and mouse IgG1 isotype, ECD-labeled anti-CD4, -CD45, -CD45RA, and mouse IgG1 isotype (Beckman Coulter, Immunotech, Marseille, France), PE-labeled anti-CD69 and -TCRVδ2 (BD Bioscience Pharmingen, San Diego, CA), APC-labeled anti-EpCAM (Miltenyi Biotec, Bergisch Gladbach, Germany), and Pacific Blue-labeled anti-CD45 (BioLegend, San Diego, CA). Fixable Viability Dye eFluor 450 and 780 (eBioscience, San Diego, CA) were used to exclude dead cells. The cells were stained with antibodies and analyzed on a Cytomics FC 500 (Beckman Coulter) or Gallios (Beckman Coulter). The data were processed using Kaluza software (Beckman Coulter). Ascites cells were harvested by centrifugation and stained with mAbs described above. Tumor-cell load in ascites fluid (mL) was determined by quantification of EpCAM+ tumor cells in ascites fluid/peritoneal lavage. The cells were also resuspended in PBS and examined by confocal microscopy, FV10i (Olympus, Tokyo, Japan).
Cytotoxicity assay
The cytotoxic activity of Vγ9Vδ2 T-cells was examined by flow cytometry as described previously, with minor modifications 11,29. Daudi cells were obtained from the RIKEN BRC Cell Bank (Ibaraki, Japan) and grown in RPMI-1640 medium (Wako, Osaka, Japan) containing 10% fetal calf serum, streptomycin (100 μg/mL), and penicillin (100 U/mL). Daudi cells were preincubated with 5 μmol/L zoledronate overnight, resuspended in Diluent C (Sigma, St Louis, MO), and incubated for 2 min with 2 μmol/L freshly prepared PKH-26 (Sigma) at room temperature. Daudi cells without zoledronate pretreatment were also used as target cells. After extensive washing, target cells were coincubated with effector cells at the indicated E/T ratio. After 1.5 h of in vitro incubation, cells in 0.1 mL of binding buffer (10 mmol/L HEPES, 140 mmol/L NaCl, 2 mmol/L CaCl2, pH 7.4) were incubated with 5 μL of Annexin-V-FITC (BD Bioscience Pharmingen) and 20 μg/mL of 7-aminoactinomycin D (7-AAD) (Sigma). Data analysis was performed first by gating on PKH-26-positive target cells followed by the analysis of Annexin-V-FITC-and 7-AAD-positive subpopulations. The percentage cytotoxicity in the PKH-26-gated cell population was calculated by subtracting the value of nonspecific Annexin-V-FITC-or 7-AAD-positive target cells, measured in appropriate controls without effector cells.
EpCAM+ cells were enriched from ascites fluid using CD326 (EpCAM) Tumor Cell Enrichment and Detection Kit, human (Miltenyi Biotec) and stained with PKH-26 (Sigma). The labeled cells were plated on 35-mm glass bottom dish (Matsunami Glass Inc., Osaka, Japan) in RPMI-1640 medium containing 10% fetal calf serum with 5 μmol/L zoledronate. Vγ9Vδ2 T cells from same patient were expanded and labeled with 0.5 μmol/L carboxyfluorescein diacetate succinimidyl ester (CFSE; Molecular Probes, Eugene, Oregon) according to the manufacturer's instructions. After EpCAM+ cells adhered to the bottom of the dish, CFSE-labeled Vγ9Vδ2 T-cells were added and cocultured under the confocal microscopy FV10i observation.
CD107 translocation assay
Daudi cells were preincubated overnight with indicated concentration of zoledronate (0, 1, 5, 10, 50, and 100 μmol/L, Novartis, Basel, Switzerland) to accumulate IPP or 10 μmol/L pravastatin sodium (Cayman Chemical, Ann Arbor, MI) to inhibit IPP synthesis. Zoledronate-or pravastatin-treated Daudi cells were used as stimulator cells and incubated with the same number of Vγ9Vδ2 T-cells (5 × 105) for 2 h at 37°C in the presence of GolgiStop (BD bioscience), and anti-CD107a/b mAbs (BD bioscience). Vγ9Vδ2 T cells were also stimulated with 20 ng/mL PMA/2 μg/mL ionomycin (both from Sigma-Aldrich). Cells were then washed in PBS supplemented with 2% FCS, 1 mmol/L EDTA, and stained for 30 min at 4°C with anti-CD3 and -TCRVγ9. CD107 translocation was measured by flow cytometry.
Cytokine measurement
Cytokines, including IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12(p70), TNF-α, TNF-β, and IFN-γ in the plasma and ascites fluid were measured using FlowCytomix human Th1/Th2 11-plex kits (Bender MedSystems, Vienna, Austria) according to the manufacturer's instructions.
Results
patients' characteristics
A total of seven patients underwent adoptive Vγ9Vδ2 T-cell immunotherapy. The characteristics of the enrolled patients are summarized in Table 1. There were two men and five women with a median age of 58 years (range, 39–69). All patients had previously received surgery and chemotherapy. They were resistant to current possible standard chemotherapy, followed by 4-week washout period; then adoptive Vγ9Vδ2 T-cell immunotherapy was reassessed. Malignant lesions were clinically restricted to the peritoneum in two cases (patients 2305 and 2319), while others had metastasized to lymph nodes, ovary, bladder, skin, and bones.
Adoptive transfer of Vγ9Vδ2 T cells
Aliquots of patients' PBMC were thawed and large-scale Vγ9Vδ2 T-cell expansion cultures initiated 14 days prior to each injection. The number and percentage of Vγ9Vδ2 T cells administered differed between individual patients and between separate infusions (Table 2). In most cases, the expansion of Vγ9Vδ2 T cells from cryopreserved PBMCs was successful and >50 × 108 Vγ9Vδ2 T cells were prepared for injections. However, the number of harvested Vγ9Vδ2 T cells from the first large-scale culture was less than expected in patients 2305 and 2334, even though the number of cryopreserved PBMCs used was predetermined by the small-scale culture test. In these cases, more cryopreserved PBMCs were used for the next large-scale expansion culture to ensure the availability of sufficient amounts of cells. The number of Vγ9Vδ2 Tcells in each injection ranged from 0.6 to 69.8 × 108 (median 59.0 × 108) (Table 2). The Vγ9Vδ2 T cells from all of the patients displayed good effector function as assessed by their in vitro cytotoxicity against Daudi cells (Table 2).
Table 2.
Adoptively transferred Vγ9Vδ2 T-cells
| Cell number (×108 cells) (purity of γδ T cells) |
Cumulative number of γδ T cell infusions (×108 cells) | Average number of γδ T cell infusions (×108 cells) | % cytotoxicity against z-Daudi* E/T ratio |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient ID | First | Second | Third | Fourth | 1:1 | 5:1 | 25:1 | ||
| 2305 | 0.6 (27.6%) | 0.6 | 0.6 | 18.1 | 30.3 | 30.1 | |||
| 2307 | 58.8 (81.7%) | 58.8 | 58.8 | 31.4 | 40.9 | 53 | |||
| 2319 | 55.4 (77.0%) | 60.5 (84.0%) | 65.6 (85.2%) | 68.5 (85.6%) | 250 | 62.5 | 41.3 | 58 | 74.6 |
| 2325 | 49.7 (84.3%) | 60 (88.3%) | 69.8 (89.5%) | 40.1 (89.0%) | 219.6 | 54.9 | 14.2 | 39.3 | 60.2 |
| 2334 | 8.6 (71.5%) | 45.1 (77.8%) | 52.7 (82.3%) | 106.4 | 35.5 | 45.1 | 79.7 | 84.6 | |
| 2336 | 64.9 (94.0%) | 64.9 | 64.9 | 28.9 | 57 | 55.4 | |||
| 2328 | 62.4 (90.4%) | 59.2 (92.5%) | 65.7 (93.9%) | 51.7 (92.3%) | 239 | 59.8 | 38.3 | 64.5 | 72.2 |
% cytotoxicity against Daudi cells was provided in Table S2.
Activated Vγ9Vδ2 T cells exert antitumor effector activity through TCR and NK receptors such as NKG2D. NK receptors-dependent or Vγ9Vδ2 TCR-dependent recognition of tumor cell was evaluated by CD107 translocation assay using pravastatin-or zoledronate-pretreated Daudi cells (Fig. 2). When the baseline tumor cell recognition by NK receptors was evaluated against pravastatin-treated Daudi cells, %CD107+ Vγ9Vδ2 T cells was 55%. The proportion of CD107+ Vγ9Vδ2 T cells against Daudi or z-Daudi cells increased from 63.3% to 96.9% according to the concentration of zoledronate, and reached the plateau at 50 μmol/L or higher. These results were consistent with previous reports that the optimum inhibition of FPP synthase activity was achieved by high zoledronate concentration 30. The cytotoxic activities of patients' Vγ9Vδ2 T cells against z-Duadi and Daudi cells were summarized in Table S2.
Figure 2.

IPP accumulation by zoledronate was evaluated by the CD107 translocation assay of Vγ9Vδ2 T-cells. Daudi cells were preincubated overnight with indicated concentration of zoledronate (0, 1, 5, 10, 50, and 100 μmol/L) or 10 μmol/L pravastatin sodium and used as stimulator cells. The 5 × 105 Daudi cells were incubated with the same number of Vγ9Vδ2 T-cells for 2 h at 37°C in the presence of GolgiStop and anti-CD107a/b mAbs. Vγ9Vδ2 T-cells were also stimulated with PMA (20 ng/mL)/ionomycin (2 μg/mL). CD107 translocation was measured by flow cytometry. Results were expressed as percentages of positive cells within the Vγ9Vδ2 T-cell population.
Dynamics of zoledronate and Vγ9Vδ2 T-cells injection
Three patients completed the course of four Vγ9Vδ2 T-cell transfers; patient 2328 received an additional two infusions. After each i.p. injection, a large number of Vγ9Vδ2 T cells was observed in the ascites (Fig. 3A); however, Vγ9Vδ2 T cells were not increased in the blood (data not shown), suggesting that they did not enter the systemic circulation from the peritoneal cavity. The number of Vγ9Vδ2 T-cells in ascites rapidly decreased within 7 days except in patient 2319.
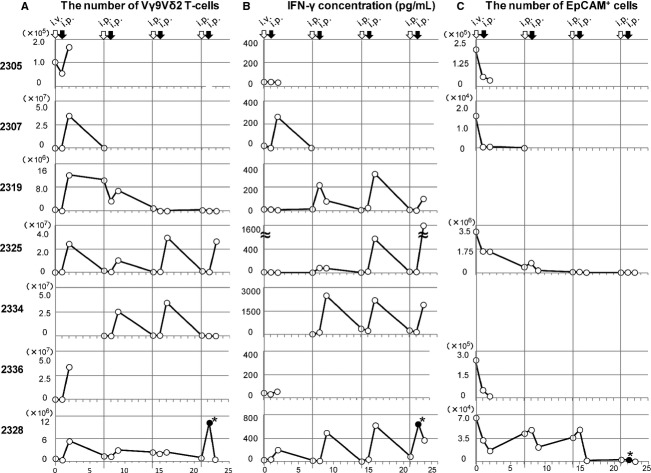
Figure 3.
Dynamics of Vγ9Vδ2 T cells and responses in patients with malignant ascites. (A) The number of Vγ9Vδ2 T cells in ascites. The ascites fluid was drained from the peritoneal cavity via the indwelling catheter before zoledronate and Vγ9Vδ2 T-cell injections and 24 h after Vγ9Vδ2 T-cell injections. The cells were isolated by density gradient centrifugation and stained with anti-CD45, -CD3, and -TCRVγ9. The stained cells were analyzed on flow cytometry and the numbers of Vγ9Vδ2 T cells calculated. (B) IFN-γ concentration (pg/mL) in ascites at the indicated time points was measured by the FlowCytomix bead assay. (C) The cells from ascites were also stained with anti-EpCAM mAb and the numbers of EpCAM+ tumor cells calculated. *Sample was collected 4 h after i.p. Vγ9Vδ2 T-cell injection.
It has been reported that zoledronate declines rapidly from the plasma with half-lives of 0.2 h 31. By systemic injection of zoledronate, the concentration of zoledronate in the ascites might not be sufficient to block the mevalonate pathway and accumulate IPP in the tumor cells. Therefore, we compared the route of zoledronate injection, i.v. or i.p., preceded the infusion of Vγ9Vδ2 T-cell administration. After i.v. zoledronate and i.p. Vγ9Vδ2 T-cell injection, IFN-γ production was detected in patient 2307 and 2328, but not in patients 2305, 2319, 2325, and 2336 (Fig. 3B). Importantly, the IFN-γ production was observed when both zoledronate and Vγ9Vδ2 T cells were i.p. injected. In patient 2334, i.v. zoledronate injection was omitted; she received three courses of i.p. zoledronate injection followed by i.p. Vγ9Vδ2 T-cell injection. IFN-γ was detected in the ascites with each Vγ9Vδ2 T-cell injection.
Consistently, the concentration of zoledronate in the ascites fluid was higher and sustained longer after i.p. zoledronate injection than i.v. injection (Fig. S1). PBMCs from healthy donor were stimulated with indicated amount of zoledronate in AlyS203 medium containing 1000 IU/mL human recombinant IL-2 and 10% pooled human serum. Same donor derived PBMCs were cultured in IL-2 containing medium and in the presence of 10% patient ascites fluid for 14 days. The concentration of zoledronate was estimated by the expansion of Vγ9Vδ2 T cells. While zoledronate was not detectable in the ascites harvested after i.v. zoledornate injection, the zoledronate concentration in the ascites peaked 34.5 ± 20 nmol/L at 2 h, and rapidly declined to 10 nmol/L within 4 h after i.p. injection. The peak concentration reached higher and zoledronate concentration in the ascites sustained longer when zoledronate was i.p. injected than i.v. injected. These results indicated that local administration of zoledronate is important to sensitize tumor cells to Vγ9Vδ2 T-cell recognition.
The cytotoxicity of Vγ9Vδ2 T cells
Because tumor cells from patients 2319 and 2334 were negative for EpCAM, it was difficult to calculate their precise tumor load. In the other five patients, the number of EpCAM+ tumor cells in ascites fluid were significantly reduced after zoledronate and Vγ9Vδ2 T-cell treatment (Fig. 3C). Immunoflueorscence microscopy revealed that Vγ9Vδ2 T cells attached to and surrounded EpCAM+ tumor cells (Fig. 4A). These results are consistent with the cytological data (Fig. 4B). Large tumor cells and many leukocytes were present in the ascites. After Vγ9Vδ2 T-cell injection, a large number of small mononuclear lymphocytes, presumably the Vγ9Vδ2 T cells themselves, were observed in ascites. The number of large tumor cells was gradually reduced by the repetitive injections of Vγ9Vδ2 T cells. In addition, many polymorphonuclear leukocytes were recruited into the ascites after zoledronate injection. The cytotoxic activity of Vγ9Vδ2 T cells was also examined in vitro (Fig. 4D). When Vγ9Vδ2 T cells from patient 2325 were cocultured with autologous EpCAM+ tumor cells in vitro, Vγ9Vδ2 T cells attached and killed tumor cells (movie clip S1). These results indicated that Vγ9Vδ2 T cells indeed recognized tumor cells and exert antitumor activity.
Figure 4.
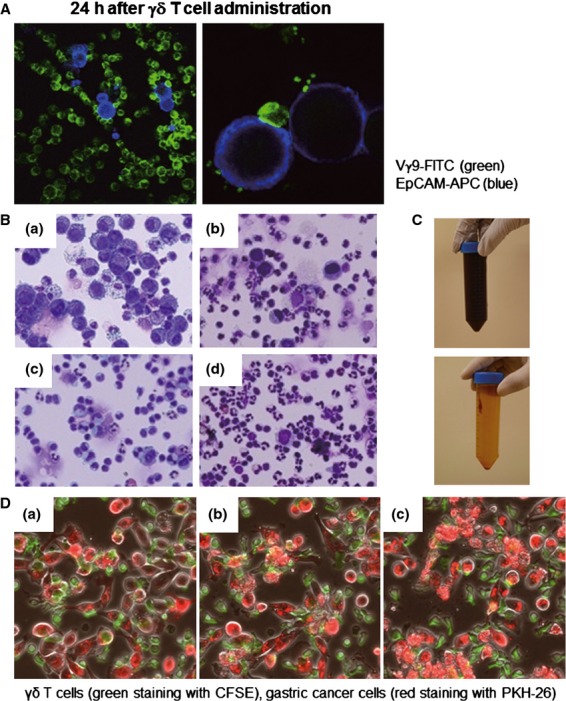
The cellular components and appearance of the ascites fluid. (A) The ascites fluid was harvested 24 h after Vγ9Vδ2 T-cell injection; the cells were stained with anti-TCRVγ9-FITC and anti-EpCAM-APC mAbs and examined by confocal fluorescence microscopy. The EpCAM+ tumor cells (blue) are attached to and surrounded by Vγ9Vδ2 T cells (green) in ascites after Vγ9Vδ2 T-cell injections. Magnification was 150× on the left and 600× on the right. (B) Smears were prepared, air-dried, and stained with Diff-Quik (Sysmex, Kobe, Japan) according to the manufacturer's instructions. Cell morphology was evaluated using bright field microscopy (OLYMPUS BX41 with Canon EOS Kiss X4 digital camera, OLYMPUS, Tokyo, Japan, magnification 200×). Data from patient 2328 on day 0 (a: before zoledronate i.v.), day 9 (b: 24 h after 2nd Vγ9Vδ2 T-cell injection), day 21 (c: before zoledronate i.p.), and day 22 (d: 4 h after Vγ9Vδ2 T-cell injection) are shown. (C) The appearance of ascites from patient 2325 before and after four courses of Vγ9Vδ2 T-cell injections. (D) γδ T cells from patient 2325 (green staining with CFSE) recognized and killed autologous EpCAM+ gastric cancer cells purified from ascites fluid (red staining with PKH-26), by direct contact. Tumor cells were attacked by the γδ T cells; collapse of the cell membranes led to apoptosis. It took approximately 2 h to progress from (a) to (c). Movie clip S1 is also provided.
Clinical outcome
Clinical outcomes are summarized in Table 3. Patients 2305 and 2336 were withdrawn from the study after a single round of injections, due to disease progression. Patients 2307 and 2334 were withdrawn after one and three doses of Vγ9Vδ2 T cells due to aspiration pneumonia and bacterial infection of the central venous catheter, respectively (although both patients experienced relief of their clinical symptoms and showed promising signs of immunological reactivity reflected by induction of IFN-γ and the reduction of tumor cells in ascites). As shown in Figure 4C, bloody ascites of patient 2325 became clear after the treatment. In addition, the massive retention of ascites was no longer present (Fig. 5A). Ascites was also reduced and almost disappeared in patient 2328 (Fig. 5B); therefore he received an additional two rounds of injections. Excellent palliation of symptoms was observed in these patients. However, the clinical benefits of i.p. Vγ9Vδ2 T-cell injection were restricted to the local control of malignant ascites. Patients 2325 and 2328 developed mediastinal lymph node metastasis and bone metastasis, respectively.
Table 3.
Clinical outcome
| Patient ID | Numbers of γδ T-cell injection | Adverse events (Grade, CTCAE v. 4.0) | Clinical outcome |
|
|---|---|---|---|---|
| Ascites | Others | |||
| 2305 | 1 | Rectal obstruction (3)1 | No change | Growth of primary lesion |
| 2307 | 1 | Aspiration (3)1, nausea (3),tumor pain (3), insomnia (2), hypoalbuminemia (2) | No change | Pleural effusion |
| 2319 | 4 | Fatigue (3), weight loss (3), hyponatremia (4), hypocalcemia (3), hypoalbuminemia (3), hypophosphatemia (3), female genital tract fistula (1), urinary tract infection (3), depressed level of consciousness (3), disseminated intravascular coagulation (2), lymphocyte count decreased (3) | No change | Obstructive jaundice due to the growth of primary lesion |
| 2325 | 4 | Fever (2), bloating (2), constipation (2), nausea (2), anemia (1), hypoalbuminemia (3), hypophosphatemia (3), hypocalcemia (3),urinary tract infection (2), insomnia (2), tumor pain (3), central venous catheter-related infection (2) | Disappeared | Mediastinal lymphadenopathy, pleural effusion, carcinomatous lymphangiosis |
| 2334 | 3 | Fever (2), nausea (2), insomnia (2), central venous catheter-related infection (2)1, tumor pain (3), anemia (3), hypocalcemia (3), hypoalbuminemia (3), palmar-plantar erythrodysesthesia syndrome (1) | No change | Metastasis to ovary |
| 2336 | 1 | Tumor pain (3), hypoalbuminemia (3), hypocalcemia (3), hyponatremia (3), hyperkalemia (4) | No change | Poor performance status1, metastasis to bladder, ovary and skin |
| 2328 | 4 (+2) | Fever (2), gastritis (2), constipation (2), hypoalbuminemia (3), lymphocyte count decreased (3) | Reduced | Bone metastasis |
Cause for discontinuance.
Figure 5.
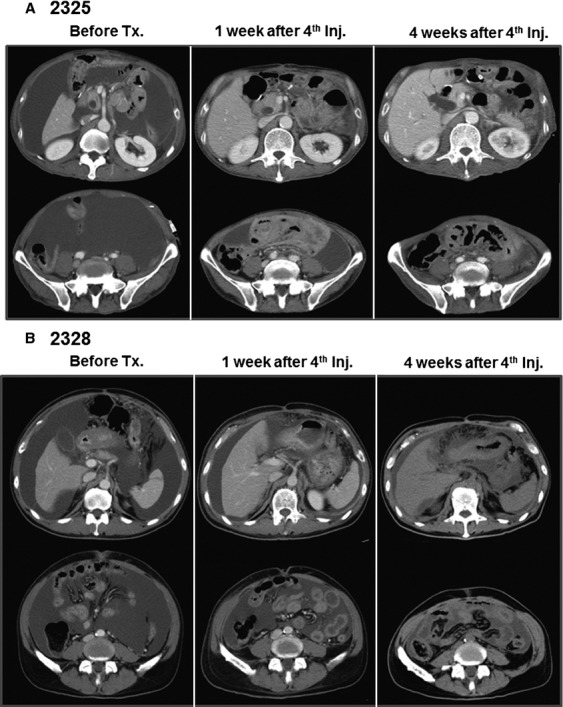
Computed tomography findings in patients 2325 (A) and 2328 (B). Retention of a large amount of ascites was observed before treatment (left panels). The amount of ascites was reduced 1 week (middle panels) and 4 weeks (right panels) after four courses of Vγ9Vδ2 T-cell injections.
Adverse events
None of the patients experienced abdominal pain or any other toxicity related to i.p. injection of Vγ9Vδ2 T cells. The most commonly observed treatment-related adverse events were fever (Grade 2: n = 3) and zoledronate-induced hypocalcemia (Grade 3: n = 4) (Tables 3 and S1). These events were generally mild-to-moderate in intensity and reversible. In contrast, most adverse events and symptoms were due to end-stage gastric cancer with peritoneal dissemination and disease progression, namely, loss of protein (Grade 2: n = 1, and Grade 3: n = 5) and electrolyte disorders (Grade 3: n = 3, and Grade 4: n = 2). Peritoneal dissemination caused serious complications, including intestinal obstruction and massive ascites, associated with weight loss, bloating, constipation, nausea, insomnia, and abdominal pain. Aspiration pneumonia (Grade 3) and disseminated intravascular coagulation (Grade 2) was observed in patients 2305 and 2319, respectively. Central venous catheter infection was detected in patients 2325 and 2334 (Grade 2). None of these adverse events was directly related to the administration of Vγ9Vδ2 T cells and there were no treatment-related deaths.
Discussion
We report here the direct evidence that adoptively transferred Vγ9Vδ2 T cells do indeed recognize tumor cells and exert antitumor effector activity in vivo. Previously, we had conducted a clinical trial of adoptive Vγ9Vδ2 T-cell transfer therapy for non-small cell lung cancer in patients who were refractory to other treatments 12,13. Autologous Vγ9Vδ2 T-cells were expanded ex vivo using zoledronate and IL-2, and administered six times at 2-week intervals. The cultured cells were well-tolerated and some clinical benefit was observed in some patients in whom Vγ9Vδ2 T cells were able to survive and expand 12,13. However, it remained to be determined whether transferred Vγ9Vδ2 T cells infiltrated into the tumor and exerted antitumor effector functions in vivo. Therefore, we conducted a trial of adoptive Vγ9Vδ2 T-cell therapy for patients with malignant ascites caused by advanced gastric cancer. PBMC were harvested by apheresis; Vγ9Vδ2 T cells were similarly prepared with zoledronate and IL-2; Vγ9Vδ2 T cells were injected weekly into the peritoneal cavity, four times in total (Fig. 1B). Direct injection of Vγ9Vδ2 T cells into the peritoneal cavity allows them direct access to the tumor cells, bypassing the difficulties of recruitment of transferred Vγ9Vδ2 T-cells into solid tumors.
As shown in Figure 4A, many Vγ9Vδ2 T cells attached to each EpCAM+ tumor cell in the ascites 24 h after their i.p. injection. Concomitantly, IFN-γ was detected in ascites with kinetics similar to the increased number of Vγ9Vδ2 T cells (Fig. 3B). The number of tumor cells in ascites was significantly reduced even after the first cell transfer and remained substantially lower during the course of the treatment (Fig. 3C). These results document tumor cell recognition and antitumor activity of Vγ9Vδ2 T cells in vivo. When autologous tumor cells were isolated by anti-EpCAM magnetic beads and cocultured with autologous zoledronate-expanded Vγ9Vδ2 T cells, Vγ9Vδ2 T cells indeed recognized and killed autologous tumor cells (Fig. 4D and movie clip S1). Such antitumor activity of i.p. Vγ9Vδ2 T cells resulted in some remarkable clinical effects. While the appearance of ascites was initially bloody in patient 2325, it became clear after i.p. Vγ9Vδ2 T-cell treatment (Fig. 4C). The reduction in ascites fluid was confirmed by computed tomography in patients 2325 and 2328 (Fig. 5). These results indicate that i.p. Vγ9Vδ2 T-cell injection combined with zoledronate contributed to the local control of malignant ascites in some patients with gastric cancer for whom no standard therapy apart from paracentesis was available.
NBPs such as zoledronate are widely used in the clinic for the treatment of bone metastases and are known as potent stimulators of Vγ9Vδ2 T cells 32. Zoledronate blocks the mevalonate pathway, leading to intracellular accumulation of IPP, its isomer dimethylallyl pyrophosphate (DMAPP) and ApppI 24,33,34. Because Vγ9Vδ2 T cells recognize these mevalonate metabolites in tumor cells, the high amounts of IPP and ApppI in zoledronate-treated tumor cells contributes to their recognition and lysis 35. In the present study, zoledronate was administered 24 h prior to i.p. Vγ9Vδ2 T-cell injection with the aim of presensitizing the tumor cells. We injected zoledronate either i.v. or i.p. and compared these routes of injection (Fig. 1B). As shown in Figure 3B, smaller amounts of IFN-γ in ascites were detected in two of six patients after i.v. zoledronate injection, while higher amounts were found in ascites of all four patients who received i.p. zoledronate. These results are consistent with pharmacokinetic data for zoledronate, indicating that serum concentrations decline rapidly after infusion 31. When we harvest ascites 2–8 h after i.p. zoledronate injection, ascites fluid contained the sufficient amount of zoledronate to expand Vγ9Vδ2 T cell, suggesting they might inhibit farnesyl pyrophosphate (FPP) synthase activity in the tumor cells at this time point (Fig. S1). However, Vγ9Vδ2 T cell did not respond to the ascites fluid harvested after i.v. zoledronate injection. Therefore, the zoledronate concentration in the ascites might not be sufficient for the inhibition of FPP synthase activity after i.v. administration. While the optimum dose and timing of zoledronate administration remain to be elucidated, the local administration of zoledronate is desired to inhibit FPP synthase and sensitize tumor cells in the abdominal cavity to efficient Vγ9Vδ2 T-cells recognition.
In addition to the direct cytotoxic activity of Vγ9Vδ2 T-cells on the tumor cells, their activation results in release of many cytokines and chemokines that may lead to the recruitment and activation of other immune cells. It has been reported that Vγ9Vδ2 T cells induce dendritic cell maturation 36, B-cell activation 37, and polarization of Th1 immune responses 38. We observed marked recruitment of neutrophils into the peritoneal cavity in this study (Fig. 4B); zoledronate alone induced granulocyte recruitment, suggesting that NBPs induce γδ T cell-independent neutrophil recruitment in humans. Recently, Norton et al. 39 reported that intraperitoneal injection of alendronate, one of the FDA-approved NBPs, induced peritoneal inflammation in mice. In their model, neutrophil recruitment depended on mast cells and IL-1R signaling. As mice lack the counterpart of human Vγ9Vδ2 T cells and thus cannot respond to IPP and NBPs, the mechanism of peritoneal inflammation in mice might be different from our human study. Consistent with a previous reports that Vγ9Vδ2 T-cell activation-induced neutrophil migration and increased their phagocytic potential and release of α-defensins 40, and that γδ T cells rapidly induce CXCL8-mediated migration of neutrophils 41, infiltration of neutrophils was sustained after i.p. Vγ9Vδ2 T-cell injection in this study (Fig. 4B). Despite the recruitment of many neutrophils into the peritoneal cavity, patients did not complain of abdominal pain and did not display any signs of peritonitis except retention of ascites after Vγ9Vδ2 T-cell injection.
The combination of i.p. Vγ9Vδ2 T-cell injection and zoledronate for the treatment of malignant ascites had acceptable tolerability without unexpected severe or long-lasting adverse events. Because patients with severe peritoneal dissemination and malignant ascites are generally in a poor condition, adverse events were frequent; many of them were not associated with cell transfer (Tables 3 and S1). However, pyrexia was probably associated with the release of proinflammatory cytokines induced by zoledronate and Vγ9Vδ2 T-cell injection. The local i.p. injection of zoledronate and Vγ9Vδ2 T cells might reduce the systemic adverse events associated with the release of proinflammatory cytokines. Though the kinetics of IL-1β, IL-8, and TNF-α production in ascites fluid were similar with that of IFN-γ, the changes of these cytokines were not detected in the patients' serum (data not shown). The IL-6 was elevated before the treatment in many of these advanced cancer patients, the changes associated with zoledronate and/or Vγ9Vδ2 T-cells were not clear. The alterations in laboratory parameters were rarely considered clinically relevant to the treatment except for hypocalcemia caused by zoledronate.
The patients in this study received S-1 plus cisplatin, S-1 plus docetaxel, or docetaxel alone as a standard regimen for the treatment of unresectable or recurrent gastric cancer prior to the Vγ9Vδ2 T-cell therapy (Table 1) 17,18. It has been reported that the overall median survival time in treatment-naïve patients with malignant ascites was approximately 5 months irrespective of the regimen received 16,42,43. Once patients have become refractory to these chemotherapies, it is unlikely that they will experience a survival benefit from any treatment. In such cases, paracentesis and diuretics are primarily used in managing malignant ascites, neither of which is an anticancer treatment but solely palliative 15. In contrast, the i.p. injection of Vγ9Vδ2 T cells combined with zoledronate directly affects the tumor cells and reduces their number in the peritoneal cavity, as well as decreasing the amount of ascites fluid, leading to palliation of the symptoms of malignant ascites.
Although the i.p. Vγ9Vδ2 T-cell injection and zoledronate treatment is unlikely to impact overall survival in such advanced disease, especially with metastasis, our results show a clear clinical benefit for the local control of malignant ascites (Fig. 5). We are planning to conduct a new clinical trial for treatment-naïve patients with peritoneal dissemination to evaluate the survival benefit of this treatment. Furthermore, combinations of this newly emerging therapy with established surgical, radiotherapy, and chemotherapy treatments are expected to improve the survival of cancer patients in future.
Acknowledgments
This study was supported in part by a Grant-in-Aid for Scientific Research of the Ministry of Education, Culture, Sports, Science and Technology (K. K.). We thank Makoto Kondo, Takamichi Izumi, and Takuya Takahashi for performing the γδ T cell cultures; Nao Fujieda, Atsushi Kondo, Kaori Kanbara, and Ryuji Maekawa for immunological monitoring and laboratory assistance; Takashige Kondo, Yoko Yamashita, Tomoko Ishida, Haruka Matsushita, Yuki Nagasawa, Hiroki Yoshihara, and Akiko Fukuzawa for administrative supports.
Conflict of Interest
Dr. Kazuhiro Kakimi received research support from Medinet Co. Ltd. (Yokohama, Japan). The costs of the entire γδ T cell culture production and part of the immunological assays were covered by Medinet Co. Ltd. The study sponsors had no involvement in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication. All other authors have declared there are no financial conflicts of interest related to this work.
Funding Information
This study was supported in part by a Grantin-Aid for Scientific Research of the Ministry of Education, Culture, Sports, Science and Technology (K. K.).
Supporting Information
Additional Supporting Information may be found in the online version of this article:
The concentration of zoledronate was estimated by the Vμ9Vδ2 T-cell bioassay. PBMCs from healthy donor were stimulated with indicated amount of zoledronate in AlyS203 medium containing 1000 IU/mL human recombinant IL-2 and 10% pooled human serum. After 14 day-culture, expansion of Vμ9Vδ2 T cell was measured by flow cytometry to prepare the standard curve. Same donor-derived PBMCs were cultured in IL-2 containing medium and in the presence of 10% patient ascites fluid for 14 days. The concentration of zoledronate was estimated by the expansion of Vμ9Vδ2 T cell using the standard curve.
Patient's Vμ9Vδ2 T cells recognize and kill autologous tumor cells.
Adverse events.
% Cytotoxicity of Vμ9Vδ2 T cells against Daudi cells w/o zoledronate treatment.
References
- 1.Hayday AC. γδ cells: a right time and a right place for a conserved third way of protection. Annu. Rev. Immunol. 2000;18:975–1026. doi: 10.1146/annurev.immunol.18.1.975. [DOI] [PubMed] [Google Scholar]
- 2.Carding SR, Egan PJ. γδ T cells: functional plasticity and heterogeneity. Nat. Rev. Immunol. 2002;2:336–345. doi: 10.1038/nri797. [DOI] [PubMed] [Google Scholar]
- 3.Triebel F, Hercend T. Subpopulations of human peripheral T γδ lymphocytes. Immunol. Today. 1989;10:186–188. doi: 10.1016/0167-5699(89)90321-6. [DOI] [PubMed] [Google Scholar]
- 4.Bonneville M, Scotet E. Human Vgamma9Vdelta2 T cells: promising new leads for immunotherapy of infections and tumors. Curr. Opin. Immunol. 2006;18:539–546. doi: 10.1016/j.coi.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Riganti C, Massaia M, Davey MS, Eberl M. Human gammadelta T-cell responses in infection and immunotherapy: common mechanisms, common mediators? Eur. J. Immunol. 2012;42:1668–1676. doi: 10.1002/eji.201242492. [DOI] [PubMed] [Google Scholar]
- 6.Wilhelm M, Kunzmann V, Eckstein S, Reimer P, Weissinger F, Ruediger T, et al. γδ T cells for immune therapy of patients with lymphoid malignancies. Blood. 2003;102:200–206. doi: 10.1182/blood-2002-12-3665. [DOI] [PubMed] [Google Scholar]
- 7.Dieli F, Vermijlen D, Fulfaro F, Caccamo N, Meraviglia S, Cicero G, et al. Targeting human γδ T cells with zoledronate and interleukin-2 for immunotherapy of hormone-refractory prostate cancer. Cancer Res. 2007;67:7450–7457. doi: 10.1158/0008-5472.CAN-07-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennouna J, Bompas E, Neidhardt EM, Rolland F, Philip I, Galea C, et al. Phase-I study of Innacell gammadelta, an autologous cell-therapy product highly enriched in gamma9delta2 T lymphocytes, in combination with IL-2, in patients with metastatic renal cell carcinoma. Cancer Immunol. Immunother. 2008;57:1599–1609. doi: 10.1007/s00262-008-0491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kobayashi H, Tanaka Y, Yagi J, Minato N, Tanabe K. Phase I/II study of adoptive transfer of gammadelta T cells in combination with zoledronic acid and IL-2 to patients with advanced renal cell carcinoma. Cancer Immunol. Immunother. 2011;60:1075–1084. doi: 10.1007/s00262-011-1021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondo M, Sakuta K, Noguchi A, Ariyoshi N, Sato K, Sato S, et al. Zoledronate facilitates large-scale ex vivo expansion of functional gammadelta T cells from cancer patients for use in adoptive immunotherapy. Cytotherapy. 2008;10:842–856. doi: 10.1080/14653240802419328. [DOI] [PubMed] [Google Scholar]
- 11.Sato K, Kondo M, Sakuta K, Hosoi A, Noji S, Sugiura M, et al. Impact of culture medium on the expansion of T cells for immunotherapy. Cytotherapy. 2009;11:936–946. doi: 10.3109/14653240903219114. [DOI] [PubMed] [Google Scholar]
- 12.Nakajima J, Murakawa T, Fukami T, Goto S, Kaneko T, Yoshida Y, et al. A phase I study of adoptive immunotherapy for recurrent non-small-cell lung cancer patients with autologous γδ T cells. Eur. J. Cardiothorac. Surg. 2010;37:1191–1197. doi: 10.1016/j.ejcts.2009.11.051. [DOI] [PubMed] [Google Scholar]
- 13.Sakamoto M, Nakajima J, Murakawa T, Fukami T, Yoshida Y, Murayama T, et al. Adoptive immunotherapy for advanced non-small cell lung cancer using zoledronate-expanded gammadeltaTcells: a phase I clinical study. J. Immunother. 2011;34:202–211. doi: 10.1097/CJI.0b013e318207ecfb. [DOI] [PubMed] [Google Scholar]
- 14.Dupont JB, Jr, Lee JR, Burton GR, Cohn I., Jr Adenocarcinoma of the stomach: review of 1,497 cases. Cancer. 1978;41:941–947. doi: 10.1002/1097-0142(197803)41:3<941::aid-cncr2820410323>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 15.Cavazzoni E, Bugiantella W, Graziosi L, Franceschini M, Donini A. Malignant ascites: pathophysiology and treatment. Int. J. Clin. Oncol. 2013;18:1–9. doi: 10.1007/s10147-012-0396-6. [DOI] [PubMed] [Google Scholar]
- 16.Imamoto H, Oba K, Sakamoto J, Iishi H, Narahara H, Yumiba T, et al. Assessing clinical benefit response in the treatment of gastric malignant ascites with non-measurable lesions: a multicenter phase II trial of paclitaxel for malignant ascites secondary to advanced/recurrent gastric cancer. Gastric Cancer. 2011;14:81–90. doi: 10.1007/s10120-011-0016-6. [DOI] [PubMed] [Google Scholar]
- 17.Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–221. doi: 10.1016/S1470-2045(08)70035-4. [DOI] [PubMed] [Google Scholar]
- 18.Lenz HJ, Lee FC, Haller DG, Singh D, Benson AB, III, Strumberg D, et al. Extended safety and efficacy data on S-1 plus cisplatin in patients with untreated, advanced gastric carcinoma in a multicenter phase II study. Cancer. 2007;109:33–40. doi: 10.1002/cncr.22329. [DOI] [PubMed] [Google Scholar]
- 19.Ishigami H, Kitayama J, Kaisaki S, Hidemura A, Kato M, Otani K, et al. Phase II study of weekly intravenous and intraperitoneal paclitaxel combined with S-1 for advanced gastric cancer with peritoneal metastasis. Ann. Oncol. 2010;21:67–70. doi: 10.1093/annonc/mdp260. [DOI] [PubMed] [Google Scholar]
- 20.Heiss MM, Murawa P, Koralewski P, Kutarska E, Kolesnik OO, Ivanchenko VV, et al. The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: results of a prospective randomized phase II/III trial. Int. J. Cancer. 2010;127:2209–2221. doi: 10.1002/ijc.25423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glimelius B, Hoffman K, Haglund U, Nyren O, Sjoden PO. Initial or delayed chemotherapy with best supportive care in advanced gastric cancer. Ann. Oncol. 1994;5:189–190. doi: 10.1093/oxfordjournals.annonc.a058778. [DOI] [PubMed] [Google Scholar]
- 22.Pyrhonen S, Kuitunen T, Nyandoto P, Kouri M. Randomised comparison of fluorouracil, epidoxorubicin and methotrexate (FEMTX) plus supportive care with supportive care alone in patients with non-resectable gastric cancer. Br. J. Cancer. 1995;71:587–591. doi: 10.1038/bjc.1995.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang JH, Lee SI, Lim DH, Park K-W, Oh SY, Kwon H-C, et al. Salvage chemotherapy for pretreated gastric cancer: a randomized phase III trial comparing chemotherapy plus best supportive care with best supportive care alone. J. Clin. Oncol. 2012;30:1513–1518. doi: 10.1200/JCO.2011.39.4585. [DOI] [PubMed] [Google Scholar]
- 24.Gober HJ, Kistowska M, Angman L, Jeno P, Mori L, De Libero G. Human T cell receptor gammadelta cells recognize endogenous mevalonate metabolites in tumor cells. J. Exp. Med. 2003;197:163–168. doi: 10.1084/jem.20021500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clézardin P. Bisphosphonates' antitumor activity: an unravelled side of a multifaceted drug class. Bone. 2011;48:71–79. doi: 10.1016/j.bone.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 27.Kondo M, Izumi T, Fujieda N, Kondo A, Morishita T, Matsushita H, et al. Expansion of human peripheral blood gammadelta T cells using zoledronate. J. Vis. Exp. 2011:e3182. doi: 10.3791/3182. doi: 10.3791/3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Izumi T, Kondo M, Takahashi T, Fujieda N, Kondo A, Tamura N, et al. Ex vivo characterization of gammadelta T-cell repertoire in patients after adoptive transfer of Vgamma9Vdelta2 T cells expressing the interleukin-2 receptor beta-chain and the common gamma-chain. Cytotherapy. 2013;15:481–491. doi: 10.1016/j.jcyt.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Fischer K, Andreesen R, Mackensen A. An improved flow cytometric assay for the determination of cytotoxic T lymphocyte activity. J. Immunol. Methods. 2002;259:159–169. doi: 10.1016/s0022-1759(01)00507-5. [DOI] [PubMed] [Google Scholar]
- 30.Idrees ASM, Sugie T, Inoue C, Murata-Hirai K, Okamura H, Morita CT, et al. Comparison of γδ T cell responses and farnesyl diphosphate synthase inhibition in tumor cells pretreated with zoledronic acid. Cancer Sci. 2013;104:536–542. doi: 10.1111/cas.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen T, Berenson J, Vescio R, Swift R, Gilchick A, Goodin S, et al. Pharmacokinetics and pharmacodynamics of zoledronic acid in cancer patients with bone metastases. J. Clin. Pharmacol. 2002;42:1228–1236. doi: 10.1177/009127002762491316. [DOI] [PubMed] [Google Scholar]
- 32.Kunzmann V, Bauer E, Feurle J, Weissinger F, Tony HP, Wilhelm M. Stimulation of gammadelta T cells by aminobisphosphonates and induction of antiplasma cell activity in multiple myeloma. Blood. 2000;96:384–392. [PubMed] [Google Scholar]
- 33.Roelofs AJ, Jauhiainen M, Monkkonen H, Rogers MJ, Monkkonen J, Thompson K. Peripheral blood monocytes are responsible for gammadelta T cell activation induced by zoledronic acid through accumulation of IPP/DMAPP. Br. J. Haematol. 2009;144:245–250. doi: 10.1111/j.1365-2141.2008.07435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monkkonen H, Auriola S, Lehenkari P, Kellinsalmi M, Hassinen IE, Vepsalainen J, et al. A new endogenous ATP analog (ApppI) inhibits the mitochondrial adenine nucleotide translocase (ANT) and is responsible for the apoptosis induced by nitrogen-containing bisphosphonates. Br. J. Pharmacol. 2006;147:437–445. doi: 10.1038/sj.bjp.0706628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benzaid I, Monkkonen H, Stresing V, Bonnelye E, Green J, Monkkonen J, et al. High phosphoantigen levels in bisphosphonate-treated human breast tumors promote Vgamma9Vdelta2 T-cell chemotaxis and cytotoxicity in vivo. Cancer Res. 2011;71:4562–4572. doi: 10.1158/0008-5472.CAN-10-3862. [DOI] [PubMed] [Google Scholar]
- 36.Ismaili J, Olislagers V, Poupot R, Fournie JJ, Goldman M. Human gamma delta T cells induce dendritic cell maturation. Clin. Immunol. 2002;103:296–302. doi: 10.1006/clim.2002.5218. [DOI] [PubMed] [Google Scholar]
- 37.Brandes M, Willimann K, Lang AB, Nam KH, Jin C, Brenner MB, et al. Flexible migration program regulates gamma delta T-cell involvement in humoral immunity. Blood. 2003;102:3693–3701. doi: 10.1182/blood-2003-04-1016. [DOI] [PubMed] [Google Scholar]
- 38.Poccia F, Gougeon ML, Agrati C, Montesano C, Martini F, Pauza CD, et al. Innate T-cell immunity in HIV infection: the role of Vgamma9Vdelta2 T lymphocytes. Curr. Mol. Med. 2002;2:769–781. doi: 10.2174/1566524023361880. [DOI] [PubMed] [Google Scholar]
- 39.Norton JT, Hayashi T, Crain B, Cho JS, Miller LS, Corr M, et al. Cutting edge: nitrogen bisphosphonate-induced inflammation is dependent upon mast cells and IL-1. J. Immunol. 2012;188:2977–2980. doi: 10.4049/jimmunol.1100830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agrati C, Cimini E, Sacchi A, Bordoni V, Gioia C, Casetti R, et al. Activated Vγ9Vδ2 T cells trigger granulocyte functions via MCP-2 release. J. Immunol. 2009;182:522–529. doi: 10.4049/jimmunol.182.1.522. [DOI] [PubMed] [Google Scholar]
- 41.Caccamo N, Orlando C, La Mendola V, Meraviglia S, Todaro M, Stassi G, et al. Differentiation, phenotype, and function of interleukin-17-producing human Vγ9Vδ2 T cells. Blood. 2011;118:129–138. doi: 10.1182/blood-2011-01-331298. [DOI] [PubMed] [Google Scholar]
- 42.Yamao T, Shimada Y, Shirao K, Ohtsu A, Ikeda N, Hyodo I, et al. Phase II study of sequential methotrexate and 5-fluorouracil chemotherapy against peritoneally disseminated gastric cancer with malignant ascites: a report from the Gastrointestinal Oncology Study Group of the Japan Clinical Oncology Group, JCOG 9603 Trial. Jpn. J. Clin. Oncol. 2004;34:316–322. doi: 10.1093/jjco/hyh063. [DOI] [PubMed] [Google Scholar]
- 43.Oh SY, Kwon HC, Lee S, Lee DM, Yoo HS, Kim SH, et al. A phase II study of oxaliplatin with low-dose leucovorin and bolus and continuous infusion 5-fluorouracil (modified FOLFOX-4) for gastric cancer patients with malignant ascites. Jpn. J. Clin. Oncol. 2007;37:930–935. doi: 10.1093/jjco/hym131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The concentration of zoledronate was estimated by the Vμ9Vδ2 T-cell bioassay. PBMCs from healthy donor were stimulated with indicated amount of zoledronate in AlyS203 medium containing 1000 IU/mL human recombinant IL-2 and 10% pooled human serum. After 14 day-culture, expansion of Vμ9Vδ2 T cell was measured by flow cytometry to prepare the standard curve. Same donor-derived PBMCs were cultured in IL-2 containing medium and in the presence of 10% patient ascites fluid for 14 days. The concentration of zoledronate was estimated by the expansion of Vμ9Vδ2 T cell using the standard curve.
Patient's Vμ9Vδ2 T cells recognize and kill autologous tumor cells.
Adverse events.
% Cytotoxicity of Vμ9Vδ2 T cells against Daudi cells w/o zoledronate treatment.