Description
Antisynthetase syndrome (ASS) is a lesser recognised idiopathic inflammatory myopathy with nearly 89% showing interstitial lung disease (ILD).1 However, in a small subpopulation without evidence of myositis, the diagnosis may be critically delayed, hindering management of this rapidly progressive disease.
A 58-year-old Caucasian man presented with polyarthritis involving bilateral knees, shoulders, wrists and hand joints. He reported a history of questionable asthma with progressive dyspnoea despite optimal therapy. Examination revealed coarse pulmonary crepitations and diffuse small-joint swelling with rhagadiform skin changes over hands (figure 1). Laboratory studies demonstrated leucocytosis and modest creatinine kinase elevation. Pulmonary function tests showed forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) 76%, diffusing capacity of the lungs for carbon monoxide (DLCO) 63%, FEV1 1.99 L (54%) with 9% (230 mL) reversibility with β-agonists, consistent with restrictive lung disease. High-resolution CT of the chest noted diffuse septal thickening and honeycombing (figures 2 and 3). Inflammatory arthritis, hyperkeratotic ‘mechanic’ hands and ILD prompted a diagnosis of ASS, confirmed by serum anti-Jo1 antibodies, despite the absence of clinical myositis. The patient improved on prednisone and methotrexate, and was later transitioned to mycophenolate mofetil.
Figure 1.

Hyperkeratotic ‘mechanic’ hands.
Figure 2.
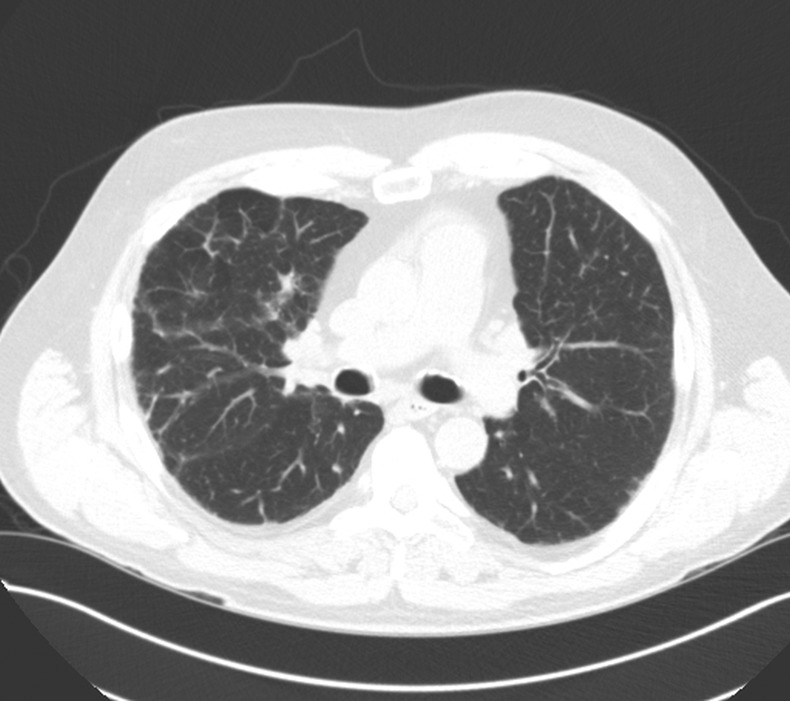
High-resolution CT of the chest demonstrating honeycombing and septal thickening consistent with interstitial lung disease.
Figure 3.
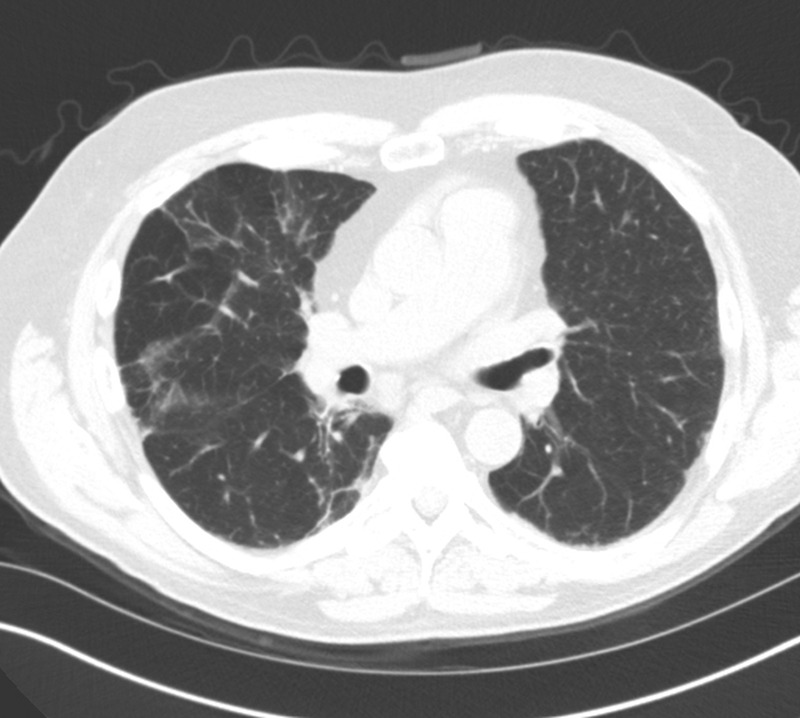
Prominent interstitial thickening consistent with interstitial lung disease.
Only 2–11% patients with ASS present with ILD in the absence of myositis and are diagnosed with anti-Jo1 antibodies in the serum.2 Median interval of development of myositis after ILD is 6 months; however rarely extending up to 2 years.1–3 Anti-Jo1 antibody-positive ILDs cause only modest serum creatine phosphokinase elevation that delays diagnosis in the absence of clinical myositis.1 These patients deteriorate faster in comparison to patients with myositis. However, once diagnosed, they have high steroid-responsiveness, which is postulated to be due to higher non-specific interstitial pneumonia without manifest alveolar damage.2 High-resolution CT scan has replaced lung biopsy in establishing diagnosis. Steroid-resistant cases are treated with azathioprine or cyclophosphamide.1 2
Learning points.
Clinical features and diagnosis of antisynthetase syndrome (ASS) including interstitial lung disease and ‘mechanic’ hands.
Recognising lesser known manifestations of ASS in the absence of clinical myositis.
Footnotes
Contributors: PRS was involved in clinical evaluation, literature search, drafting and finalising the manuscript. SV was involved in literature search, critical analysis, drafting and finalising the manuscript. JPK was involved in clinical evaluation, critical analysis and finalising the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Marie I, Josse S, Hatron PY, et al. Interstitial lung disease in anti-Jo1 patients with antisynthetase syndrome. Arthritis Care Res (Hoboken) 2013;65:800–8 [DOI] [PubMed] [Google Scholar]
- 2.Plastiras SC, Soliotis FC, Vlachoyiannopoulos P, et al. Interstitial lung disease in a patient with antisynthetase syndrome and no myositis. Clin Rheumatol 2007;26:108–11 [DOI] [PubMed] [Google Scholar]
- 3.Patel HC, Lauder NN. The antisynthetase syndrome. Am J Med 2011:124(9):e3–4 [DOI] [PubMed] [Google Scholar]


