Abstract
Background:
Sexual dysfunction is a common complication of diabetes that adversely affects their quality of life. Its prevalence is known to be higher in diabetic men with and it is estimated to affect 20-85% of patients but the problem is probably less common in diabetic women. This study investigated the prevalence of sexual dysfunction and its risk factors among women with diabetes.
Materials and Methods:
This descriptive-analytic study was performed during May 2012 to Feb 2013 at Diabetes clinic of Shahid Beheshti Hospital of Qom and The Female Sexual Function Index (FSFI) was used for evaluation of sexual dysfunction.
Conclusion:
In this study, 59 (53.6%) women had sexual dysfunction. The mean age of patients with sexual dysfunction and healthy people was 48.22 ± 6.61 and 48.14 ± 5.37 years respectively and it was not statistically different in both groups (P = 0.94). Also, there was no significant difference between two groups in average duration of diabetes, fasting blood sugar (FBS), glycosylated hemoglobin (HbA1c) level, insulin resistance, abdominal circumference and body mass index BMI. Although the history of hypertension, coronary artery disease and exercise levels were not significantly associated with sexual dysfunction, but there was a significant association between albuminuria and sexual dysfunction (P = 0.001). Retinopathy and sexual dysfunction had statistically significant relationship (P = 0.007) while no association was found between diabetic neuropathy and sexual dysfunction (P = 0.79).
Results:
Sexual dysfunction is a common complication in diabetic patients which accompanies with some complications of diabetes and should be considered especially in patients with nephropathy or retinopathy.
Keywords: Diabetes mellitus, type 2, sexual dysfunction, the female sexual function index
INTRODUCTION
Nowadays, 246 million people in the world are affected by diabetes and it is expected to affect 380 million by 2025. Moreover, the largest increases in prevalence of diabetes will occur in developing countries by 2025. [1] Among diabetic patients, hyperglycemia can cause several complications from short to long term effects. Sexual problems are common complications of diabetic disease in both men and women. Sexual health is an important, but often neglected. According to the World Health Organization, term “sexual dysfunction” is defined as various ways in which an individual is unable to participate in a sexual relationship as he/she would wish. [2]
Impaired sexual function in men is a common complication of diabetes. It was first mentioned in the 10th century AD by the Persian physician and philosopher Avicenna describing the “collapse of sexual functions” in diabetic males. [3] Previous reports have shown that diabetic men are at increased risk for sexual dysfunction with an incidence ranging from 20-85%. [2] In contrast to male sexual dysfunction, sexual dysfunction has not been well studied among diabetic women and its prevalence in diabetic women seems to be slightly lower (20-80%). [4,5]
Sexual problems in diabetic women mostly include sexual satisfaction and desire, orgasmic and arousal disorder and lubrication. [1] The etiology and risk factors for sexual dysfunction among diabetic patients is still controversial. Several neurological, vascular, endocrine, and psychological factors have been suggested as the etiology of sexual dysfunction among diabetics. [2]
It is stated that infections, hyperglycemia, and vascular, neural, neurovascular and psychosocial disorders are pathogenetic factors of diabetic female sexual dysfunction. [6] In this study, we aimed to evaluate the prevalence of sexual dysfunction in diabetic women in addition to evaluate the association of diabetic parameters including diabetes duration, glycemic control and other parameters with chronic complications of diabetes.
MATERIALS AND METHODS
Participants and data collection
This cross-sectional study was conducted among 110 diabetic women referred to Shahid Beheshti Hospital of Qom. The sample was selected in a consecutive procedure from May 2012 to Feb 2013. The sample size was estimated on the basis of Fatemi and Taghavi's research. [4]
The subjects were assigned into two groups: female with or without sexual dysfunction. The inclusion criteria were identified as registered for two year or longer (these patients had done all their two to three recent HbA1c tests in a year and the mean of their HbA1c was used as HbA1c level), aged 30 years or older and history of diabetes for five years or longer and being married. Exclusion criteria included record of mastectomy, total hysterectomy, pregnancy, existence of sexual disorders in patients' spouse, anemia, presence of sexual disorders before getting diabetes and known history of psychiatric illness.
Body weight of study participants was measured in light clothing to the nearest 0.1 kg on a bathroom scale (Beurer GmbH and Co, made in Germany). Also, height was measured to the nearest 0.5cm and the participants were standing upright with bared foot, the heels put together and the head in the horizontal plane against a wall-mounted ruler. Body mass index (BMI) was calculated by dividing weight (kg) by the height squared (m2 ). Systolic and diastolic blood pressures were measured by a Richter manometer, made in Germany. Patients were considered hypertensive if they had a diastolic blood pressure of ≥90 mmHg, or systolic blood pressure of ≥140 mmHg. Subjects under antihypertensive medication were obviously considered hypertensive patients. People who exercised at least 150 min aerobic exercise per week in the last two months were considered as exercise positive.
Measures
Sexual dysfunction
Sexual dysfunctions were measured in women using a standard questionnaire. The Female Sexual Function Index (FSFI) is a known instrument that assesses sexual function in women with six domains [6] : Desire, arousal, lubrication, orgasm, satisfaction and pain during sexual intercourse. In women, the minimum and maximum scores are respectively 2 and 36. Women with a score under 26 were classified as presenting sexual dysfunction. [7,8] This cut-off point was the same figure validated by other researchers
Clinical measures
We used available data from Shahid Beheshti Hospital where all patients received routine clinical examination that included recording of diabetes duration, body mass index (BMI), fasting blood sugar, Insulin resistance (Based on Homa-IR), metabolic syndrome criteria, blood pressure, cholesterol and triglyceride levels and diabetes-related complications. Serum total cholesterol, triglyceride, and HDL-cholesterol were measured using enzymatic techniques. Fasting plasma glucose was measured and glycosylated hemoglobin (HbA1c) percentage was determined by ion-exchange method. Insulin level was determined by using kits of Dia Metra (made in Italy), Insulin resistance was calculated by Homeostasis Model of Assessment. Insulin Resistance (HOMA-IR) was calculated using the following US Formula: (Fasting Glucose (mg/dL)×Fasting Insulin (405/μU/mL). All measurements were done under standard conditions by one technician and with the same device.
The micro-vascular complications included recording of retinopathy (ophthalmology visit), nephropathy, (24 h urine analysis) and neuropathy (peripheral, autonomic), monofilament and the diapason therapeutic examination.
Statistical analysis
Data was analyzed using software package used for statistical analysis (SPSS) version 16.0 in a descriptive and analytical fashion. To investigate the associations of demographic and clinical characteristics of the patients with SD, the λ2 test was used. In all statistical tests, a P < 0.05 was considered being significant.
Ethical considerations
All patients enrolled the study after obtaining an informed verbal consent. Diabetic women were assured regarding the confidentiality of the information and the questionnaire was completed by a person with the same gender.
RESULTS
In this study, 110 diabetic women with age range of 30-55 years and the mean age of 48.18 ± 6.04 years were evaluated. The minimum and maximum duration of diabetes was 5 and 25 years respectively with the mean duration of 8.56 ± 4.38 years.
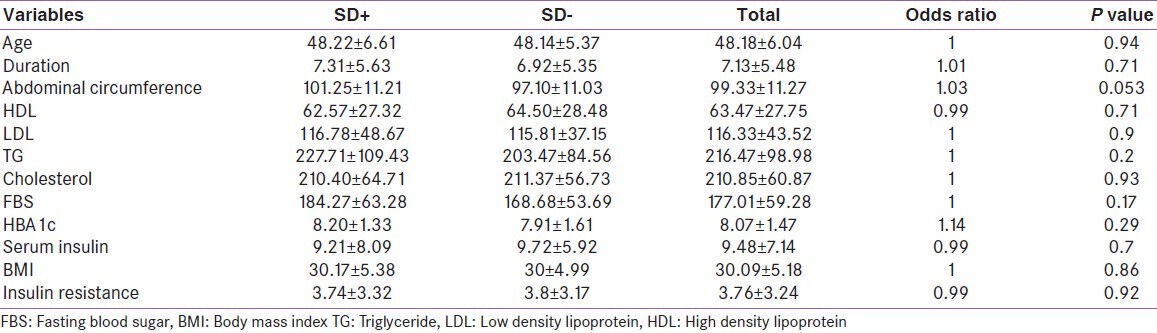
Of these women, 59 (53.60%) had sexual dysfunction. The mean age of women was 48.22 ± 6.61 in sexual dysfunction group and 48.14 ± 5.37 years in healthy patients and it was not statistically significant in both groups (P = 0.94). The mean diabetes duration, FBS, HBA1c and insulin resistance was not statistically significant in both groups [Table 1]. Also, abdominal circumference and BMI were evaluated and were not statistically significant in both groups [Table 1]. Other characteristics of both groups including blood lipid and serum insulin level are shown in [Table 1].
Table 1.
Characteristics and laboratory findings of both groups
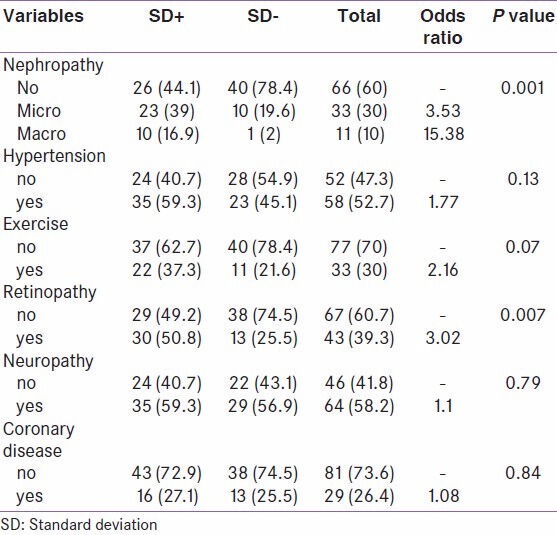
Of the studied patients, 33 ones (33%) had microalbuminuria and 11 ones (10%) had macroalbuminuria and sexual dysfunction was detected in 23 (39%) of microalbuminuria and 10 (16.9%) of macroalbuminuria patients. A significance association was found between albuminuria and sexual dysfunction (P = 0.001) [Table 2]. Also, retinopathy and sexual dysfunction were statistically significant (P = 0.007) [Table 2] but diabetic neuropathy and sexual dysfunction were not associated (P = 0.79). History of hypertension, coronary artery disease and exercise were not associated with sexual dysfunction [Table 2].
Table 2.
The association between sexual dysfunction and complications of diabetes
DISCUSSION
Female sexual dysfunction has several causes including interpersonal, contextual (social), psychological and biological factors. [9] In fact, every factor contributing normal female sexual function can be a potential cause of sexual dysfunction and there is a strong association with psychological health issues such as anxiety, depression, low self-esteem, body image perception disorders, sexual performance anxiety, fear of rejection, traumatic sexual experience in the past, and abuse history. [10,11,12] Quality of the relationship is the second major factor. [10] Biological risk factors include several medical conditions (urogenital, neurological and endocrine disorders, pelvic floor disorders, menopause, pregnancy, obesity) in addition to pharmacological and other therapies (antineoplastic agents, antipsychotic and antidepressant medications, antihypertensive agents, major surgical operations, radiation therapies). [13]
Finally, sociocultural risk factors of sexual dysfunction include limited social relations, financial difficulties, employment status, religious beliefs, educational background and lack of exercise. Diabetes mellitus is one of the important causes of sexual dysfunction. Generally, sexual dysfunction appears to be quite complex in diabetic women, involving neurological, vascular, hormonal, and psychosocial aspects. It is difficult to identify the specific risk factors, including those related to diabetes. [6] It has been hypothesized that hyperglycemia results in poor vaginal lubrication and dyspareunia, by reducing hydration of mucus membrane in the vaginal tissue. Also, hyperglycemia may potentially lead to dyspareunia because of its association with an increased incidence of genitourinary infections. [14]
Diabetes causes vascular and nerve dysfunction which can cause structural and functional changes in female genitalia and may impair sexual response. [6] Moreover, a reduced vibration sense in the genitalia has been observed in diabetic women, but its relationship with sexual problems should be clarified. Vascular changes or diabetic damage may change the local blood flow and inhibition of the clitoris engorgement and vaginal lubrication during arousal, resulting in dyspareunia or decreased arousal during sexual activity. Disorders of arousal, orgasm and sexual pain are the main consequences of the diabetic neuropathy. [15]
Hormonal imbalance accompanying diabetes has been hypothesized to play a potential role in the pathogenesis of the female sexual dysfunction. [6] Additionally, several other endocrinopathies that may accompany diabetes, such as thyroid and hypothalamic-pituitary disorders, and polycystic ovarian syndrome, can contribute to sexual problems in these women. [16] It seems that depression is the most established risk factor for sexual dysfunction in diabetic women. [17]
The prevalence of sexual dysfunction in diabetic women is estimated to be 20-80%. In our study, it was 53.6%. One factor contributing this prevalence is age and some studies consider it as an effective factor in this disorder. [2,4,5] On the contrary, some studies have not confirmed that association. In our study, no association was found between age and risk of sexual dysfunction (P = 0.94).
Another finding of this research was considering the impact of diabetes duration on sexual dysfunction. Some studies confirmed it while others did not confirm it. [1,4,5,18] In our study, the association between duration of diabetes and sexual dysfunction was observed (P = 0.71).
Effect of glycemic control on rates of sexual dysfunction is also controversial. Some studies have shown that glycemic control has no effect on the incidence of sexual dysfunction in women with diabetes. [5] In contrast, some comments are opposite. [1] In our study, we found no significant association between blood sugar and sexual dysfunction (P = 0.29). Of course, our measure of glycemic control was the mean HBA1c within last year but due to chronic nature of sexual dysfunction, prolonged evaluation of glycemic control, may provide more reliable results. Other personal factors such as weight may also affect this disorder. Some believe that overweight is another factor, [2,5] but we found no association between BMI and abdominal circumference with sexual dysfunction (P = 0.86 and P = 0.053 respectively) and it was similar to Fatemi and Taghavi's study. [4]
Of course, as it can be seen, the very close relationship between the abdominal circumference and sexual dysfunction is close to the significant amount. One of the discussed issues is the effect of other chronic diabetic complications like retinopathy and nephropathy on sexual dysfunction and considering them as risk factors for this complication. Some studies considered some diabetic complications as risk factor for sexual dysfunction [18,19] and some others consider them independent to the other diabetic complications. [20,21]
Neuropathy is one such complication. Theoretically, diabetic neuropathy affects sexual dysfunction, but clinical studies are contradictory. [6] This relationship has not been observed in some studies, [5] but some studies have shown this association. [22]
In our study, no significant association was found between sexual dysfunction and diabetic neuropathy (P = 0.79). The criterion for the diagnosis of diabetic neuropathy was therapist's examination and the patients have not undergone Nerve conduction velocity (NCV).
One of the significant correlations was detected between sexual dysfunction and diabetic nephropathy (P = 0.001) and it appears that there is a significant relationship between these two disorders, [5,18,22] It is notable that due to this statistically significant association, albuminuria can be considered as an important risk factor in the development of sexual dysfunction. It was evaluated in a study on men and albuminuria was considered as an important risk factor in the development of sexual dysfunction (14) and it seems that further prospective studies are needed for this evaluation. [19]
Another finding of this study was the association between sexual dysfunction and retinopathy (P = 0.007), which was confirmed in Abu Ali et al's study. [5] Also no significant association was found between hypertension and sexual dysfunction in our study, (P = 0.13) which was the same as Abu Ali et al's study. [5] However, other studies have not confirmed these findings. [23]
CONCLUSION
Sexual dysfunction is a common complication in patients with diabetes that should be considered by clinicians. The very meaningful relationship of this disorder with diabetic nephropathy reminds that in patients with diabetes, sexual dysfunction should be considered.
ACKNOWLEDGEMENTS
The authors would like to thank all participants who cooperated during the study. We would also appreciate the Deputy of Research and Education of Qom University of Medical Sciences for financial support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ziaei-Rad M, Vahdaninia M, Montazeri A. Sexual dysfunctions in patients with diabetes: A study from Iran. Reprod Biol Endocrinol. 2010;8:50. doi: 10.1186/1477-7827-8-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owiredu WK, Amidu N, Alidu H, Sarpong C, Gyasi-Sarpong CK. Determinants of sexual dysfunction among clinically diagnosed diabetic patients. Reprod Biol Endocrinol. 2011;9:70. doi: 10.1186/1477-7827-9-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giraldi A, Kristensen E. Sexual dysfunction in women with diabetes mellitus. J Sex Res. 2010;47:199–211. doi: 10.1080/00224491003632834. [DOI] [PubMed] [Google Scholar]
- 4.Fatemi SS, Taghavi SM. Evaluation of sexual function in women with type 2 diabetes mellitus. Diab Vasc Dis Res. 2009;6:38–9. doi: 10.3132/dvdr.2009.07. [DOI] [PubMed] [Google Scholar]
- 5.Abu Ali RM, Al Hajeri RM, Khader YS, Shegem NS, Ajlouni KM. Sexual dysfunction in Jordanian diabetic women. Diabetes Care. 2008;31:1580–1. doi: 10.2337/dc08-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bargiota A, Dimitropoulos K, Tzortzis V, Koukoulis GN. Sexual dysfunction in diabetic women. Hormones. 2011;10:196–206. doi: 10.14310/horm.2002.1309. [DOI] [PubMed] [Google Scholar]
- 7.Santos PR, Capote JR, Cavalcanti JU, Vieira CB, Rocha AR, Apolônio NA, et al. Quality of life among women with sexual dysfunction undergoing hemodialysis: A cross-sectional observational study. Health Qual Life Outcomes. 2012;10:103. doi: 10.1186/1477-7525-10-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 9.Berman JR. Physiology of female sexual function and dysfunction. Int J Impot Res. 2005;17:S44–51. doi: 10.1038/sj.ijir.3901428. [DOI] [PubMed] [Google Scholar]
- 10.Bancroft J, Loftus J, Long JS. Distress about sex: A national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32:193–208. doi: 10.1023/a:1023420431760. [DOI] [PubMed] [Google Scholar]
- 11.Cyranowski JM, Bromberger J, Youk A, Matthews K, Kravitz HM, Powell LH. Lifetime depression history and sexual function in women at midlife. Arch Sex Behav. 2004;33:539–48. doi: 10.1023/B:ASEB.0000044738.84813.3b. [DOI] [PubMed] [Google Scholar]
- 12.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 13.Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635–42. [PubMed] [Google Scholar]
- 14.Rockliffe-Fidler C, Kiemle G. Sexual function in diabetic women: A psychological perspective. Sex Relat Ther. 2003;18:143. [Google Scholar]
- 15.Park K, Ahn K, Chang JS, Lee SE, Ryu SB, Park YI. Diabetes induced alteration of clitoral hemodynamics and structure in the rabbit. J Urol. 2002;168:1269–72. doi: 10.1016/S0022-5347(05)64638-1. [DOI] [PubMed] [Google Scholar]
- 16.Bhasin S, Enzlin P, Coviello A, Basson R. Sexual dysfunction in men and women with endocrine disorders. Lancet. 2007;369:597–611. doi: 10.1016/S0140-6736(07)60280-3. [DOI] [PubMed] [Google Scholar]
- 17.Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: A systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009;5:112–9. doi: 10.2174/157339909788166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chernyshova TE, Sitnikov VA, Martirosov IuK. The effect of diabetic nephropathy on the function of the hypophyseal-gonadal system in men. Urol Nefrol (Mosk) 1991;1:54–7. [PubMed] [Google Scholar]
- 19.Chuang YC, Chung MS, Wang PW, Lee WC, Chen CD, Chang HW, et al. Albuminuria is an independent risk factor of erectile dysfunction in men with type 2 diabetes. J Sex Med. 2012;9:1055–64. doi: 10.1111/j.1743-6109.2011.02586.x. [DOI] [PubMed] [Google Scholar]
- 20.Doruk H, Akbay E, Cayan S, Bozlu M, Acar D. Effect of diabetes mellitus on female sexual function and risk factors. Arch Androl. 2005;51:1–6. doi: 10.1080/014850190512798. [DOI] [PubMed] [Google Scholar]
- 21.Enzlin P, Mathieu C, Van den Bruel A, Bosteels J, Vanderschueren D, Demyttenaere K. Sexual dysfunction in women with type 1 diabetes: A controlled study. Diabetes Care. 2002;25:672–7. doi: 10.2337/diacare.25.4.672. [DOI] [PubMed] [Google Scholar]
- 22.Copeland KL, Brown JS, Creasman JM, Van Den Eeden SK, Subak LL, Thom DH, et al. Diabetes mellitus and sexual function in middle-aged and older women. Obstet Gynecol. 2012;120:331–40. doi: 10.1097/AOG.0b013e31825ec5fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olarinoye J, Olarinoye A. Determinants of sexual function among women with type 2 diabetes in a Nigerian population. J Sex Med. 2008;5:878–86. doi: 10.1111/j.1743-6109.2007.00649.x. [DOI] [PubMed] [Google Scholar]


