Abstract
Background
Metabolic syndrome (MS) is an aggregation of risk factors that increase the incidence of cardiovascular events and diabetes mellitus (DM). Population aging is accompanied by higher prevalence of MS, which varies depending on the population studied and the diagnostic criteria used.
Objective
To determine prevalence of MS in the elderly using four diagnostic criteria and agreement between them.
Methods
Cross-sectional study on 243 patients older than 60 years (180 women) in Niterói, RJ. They were evaluated by clinical examination, fasting glucose, fasting insulin, lipid profile and anthropometric measurements - weight, height, waist circumference and waist/hip ratio. Prevalence of MS was estimated by World Health Organization (WHO) modified, National Cholesterol Education Program - Adult Treatment Panel III (NCEP-ATP III), International Diabetes Federation (IDF) and Joint Interim Statement (JIS) criteria.
Results
Prevalence was high with the four criteria WHO (51.9%), NCEP-ATPIII (45.2%), IDF (64.1%) and JIS (69.1%), and agreement between criteria by kappa was moderate in almost all comparisons WHO vs. IDF (k = 0.47;95% confidence interval (CI), 0.35 to 0.58); WHO vs. NCEP-ATPIII (k = 0.51; 95% CI, 0.40 to 0.61); WHO vs. JIS (k = 0.45; 95% CI, 0.33 to 0.56); IDF vs. NCEP-ATPIII (k = 0.55; 95% CI, 0.45 to 0.65) and NCEP-ATPIII vs. JIS (k = 0.53; 95% CI, 0.43-0.64), except between IDF vs. JIS (K = 0.89;95% CI, 0.83 to 0.95), which was considered good.
Conclusion
Prevalence of MS was high with the four diagnostic criteria, mainly by JIS. There was good agreement between JIS and IDF criteria and moderate among the others.
Keywords: Metabolic Syndrome, Prevalence, Aged, Obesity, Abdominal Circumference, Risk Factors
Introduction
The combination of central obesity, dysglycemia, dyslipidemia and arterial hypertension characterize the so-called Metabolic Syndrome (MS). Several studies1-3 have shown that MS prevalence increases with age, making its diagnosis necessary due to the 2.5-fold increased risk of cardiovascular disease and five-fold increase for the development of diabetes mellitus (DM)4.
In 1988, Reaven5 described a close association between metabolic abnormalities and insulin resistance, calling it "Syndrome X". The World Health Organization (WHO), in 19986, established the first diagnostic criterion, of which hyperglycemia was the important and indispensable component. In 2001, the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII) proposed a new criterion, in which glycemia was no longer considered an indispensable factor, becoming just one of the components. In this criterion, the presence of at least three of the five components of MS - increased Waist Circumference (WC) increased fasting glucose, low HDL cholesterol, hypertriglyceridemia and high blood pressure comprise the diagnosis of MS7. The I Brazilian Guideline for the Diagnosis and Treatment of MS, developed in 2005, used this criterion as the basis for MS diagnosis8.
The prevalence of obesity has increased in recent decades in all age groups, concomitantly with the population aging. Considering the evidence of the association between obesity and cardiovascular risk, the International Diabetes Federation (IDF) in 2005 proposed a new definition of MS taking into account abdominal obesity through the WC, making it essential for the diagnosis9.
In 2009 Alberti et al10 presented a consensus criterion for the diagnosis of MS -the Joint Interim Statement (JIS) - that was endorsed by several societies, which chose the non-mandatory presence of any of the components, but the presence of at least three altered components in five and the WC measurement according to different ethnicities.
Considering that the MS represents a higher risk for cardiovascular disease, DM, mobility alterations11, cognitive deficits12 and depression13 in the elderly, together with the scarcity of data in Brazil, this study aims at determining the prevalence of MS by four different diagnostic criteria and the agreement between them in a population older than 60 years old.
Methods
The present is a cross-sectional study including 243 patients, 180 of which females, over 60 years old, volunteers in a convenience sample, all treated at the Outpatient Clinic of Geriatrics and Internal Medicine of Fundação Municipal de Saúde de Niterói (RJ). Patients included the study had different diagnosis and reasons for the treatment received. The project was approved by the Ethics Committee of Faculdade de Medicina, Universidade Federal Fluminense, number 0183.0.258.258.10 and all participants signed a free and informed consent form.
Morbidly obese patients, patients with liver failure and end-stage renal disease, individuals on corticosteroids, immunosuppressants and cognitive disabilities were excluded.
Anamnesis was performed, with collection of social data and information on medication use. Clinical evaluation consisted of blood pressure measurement with an OMRON HEM 742INT automatic sphygmomanometer (Bannockburn, Illinois 60015 USA) in the left arm, with the patient in the sitting position, after at least five minutes of rest, using the average of the last two measurements with a difference < 4 mmHg between them14. Anthropometric measures included weight in kilograms (kg) and height in centimeters (cm) using a Filizola anthropometric scale (São Paulo, SP, Brazil) calibrated by INMETRO. The Body Mass Index (BMI) was calculated by dividing weight in kilograms by the square of height in meters.
The waist circumference (WC) was measured using a SANNY inelastic measuring tape (São Bernardo do Campo, SP, Brazil), at the midpoint between the iliac crest and the last rib, with the patient standing at the end of exhalation15.
Blood samples were obtained after a 12-fast and subsequently analyzed at Laboratório Central de Saúde Pública. Serum fasting glucose, total cholesterol, HDL - cholesterol and TG were measured using Labtest commercial kits (Lagoa Santa, Belo Horizonte, Brazil). LDL - cholesterol was calculated by the Friedewald equation. The samples were analyzed by an enzymatic method in automated Labmax 240 equipment (Belo Horizonte, Brazil).
Insulin measurements were performed on an ELECSYS equipment (Roche, Japan) by the method of electrochemiluminescence. The Homa1-IR was calculated by multiplying fasting glucose (mmol / L) by fasting insulin (μIU / mL) and dividing by 22.5 and a Homa1-IR > 2.7 was considered positive for insulin resistance16. The diagnosis of MS was established according to the modified WHO, NCEP-ATPIII, IDF and JIS criteria as described in Table 1. The cutoff used for WC in IDF and JIS criteria was that of European ethnicity.
Table 1.
Definitions and diagnostic criteria for metabolic syndrome
| WHO (modified)* | NCEP-ATPIII † | IDF ‡ | JIS § | |
|---|---|---|---|---|
| Blood pressure | ≥ 140/90 mmHg or SAH treatment(//) | ≥ 130/85 mmHg | ≥ 130/85 mmHg or SAH treatment | ≥ 130/85 mmHg or SAH treatment |
| Anthropometrics | WHR (¶ ) ♂ > 0.9 and ♀ > 0.85and/or BMI (#) > 30 kg/m2 | WC(§§) ≥ 102 ♂ ≥ 88 ♀ | WC ≥ 94 ♂ ≥ 80 ♀ | WC ≥ 94 ♂ ≥ 80 ♀ |
| Glucose | DM.IGT (**) or Homa-1 IR (††) > 2.7 | ≥ 110 | ≥ 100 | ≥ 100 |
| TG | ≥ 150 ( ‡‡) | ≥ 150 | ≥ 150 | ≥ 150 |
| HDL-col | ♂ < 35 ♀ < 39 | ♂ < 40 ♀ < 50 | ♂ < 40 ♀ < 50 | ♂ < 40 ♀ < 50 |
| MS Criterion | DM, IGT or Homa-1 IR > 2.7 +2 other components | 3 or more components | WC plus 2 components | 3 or more components |
WHO: World Health Organization;
(†)NCEP-ATPIII-Third Report of the National Cholesterol Education Program; (‡)IDF-International Diabetes Federation; (§) JIS: Joint Interim Statement. ( //) SAH: Systemic Arterial Hypertension; (¶ )WHR: waist/hip ratio;(#)BMI: Body Mass Index;
IGT: Impaired glucose tolerance; (††) Homa1-IR: Homeostatic model assessment; (‡‡)Bothaltered TG orlow HDL-c constitute only one factorbyWHO; (§§)WC: waist circumference.
Statistical Analysis
Student's t test and one-way ANOVA were used to analyze numerical data. Statistical analysis evaluated the concordance in the diagnosis of MS among the criteria used in the survey, WHO, NCEP-ATPIII, IDF and JIS using the Kappa index. Significance level was set at 0.05. S-Plus 8.0 software program was used for these analyses.
Results
A total of 243 elderly individuals participated in study, of which 180 were women (74%). Mean age was 71 ± 7 years when assessing the entire study population and 71 ± 7 years in females and 70 ± 7 in males (p > 0.05). Table 2 shows the mean MS components evaluated by gender.
Table 2.
Metabolic Syndrome componentsaccording togender
| Male (n = 63) | Female (n = 180) | P | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| BMI* (kg/m2) | 28.1 ± 4.4 | 29.2 ± 5.7 | > 0.05 |
| Waist circumference (cm) | 99.9 ± 10.1 | 96 ± 12.7 | < 0.05 |
| Fasting glycemia (mg/dL) | 114 ± 39 | 106 ± 27 | > 0.05 |
| Total cholesterol (mg/dL) | 182 ± 38 | 206 ± 43 | < 0.01 |
| Triglycerides (mg/dL) | 145 ± 74 | 139 ± 74 | > 0.05 |
| HDL - cholesterol (mg/dL) | 47 ± 12 | 57 ± 14 | < 0.05 |
| LDL - cholesterol (mg/dL) | 106 ± 34 | 120 ± 40 | < 0.05 |
BMI: Body Mass Index.
In women, BMI (p > 0.05), total cholesterol (p < 0.01) HDL-c and LDL-c (p < 0.05) values were higher than in males, whereas the WC (p < 0.05), fasting glucose (p >0.05) and triglycerides (p > 0.05) values were higher in men (Table 2).
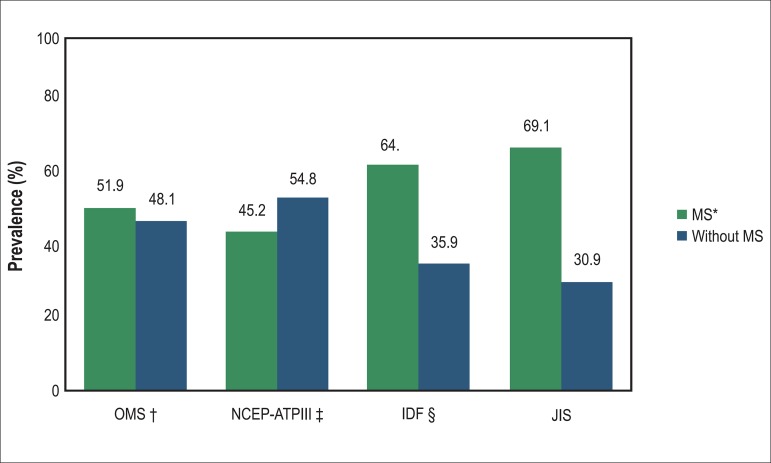
A total of 51.9%, 45.2%, 64.1% and 69.1% of participants were classified as having MS according to WHO criteria, NCEP ATPIII, IDF and JIS, respectively (Chart 1). The prevalence of MS according to gender was 49.4%, 45.6%, 65.6% and 68.9% by WHO, NCEP-ATPIII, IDF and JIS criteria, respectively, in females. In males, the prevalence of MS was 58.7%, 44.4%, 60.3% and 69.8% according to the WHO, NCEP-ATPIII, IDF and JIS criteria, respectively.
Chart 1.
Prevalence of metabolic syndrome in the study population according to the four criteria. *MS: Metabolic Syndrome; †WHO: World Health Organization; ‡NCEP- ATP III: Third Report of the National Cholesterol Education Program; § IDF: International Diabetes Federation; ∕∕JIS-Joint Interim Statement.
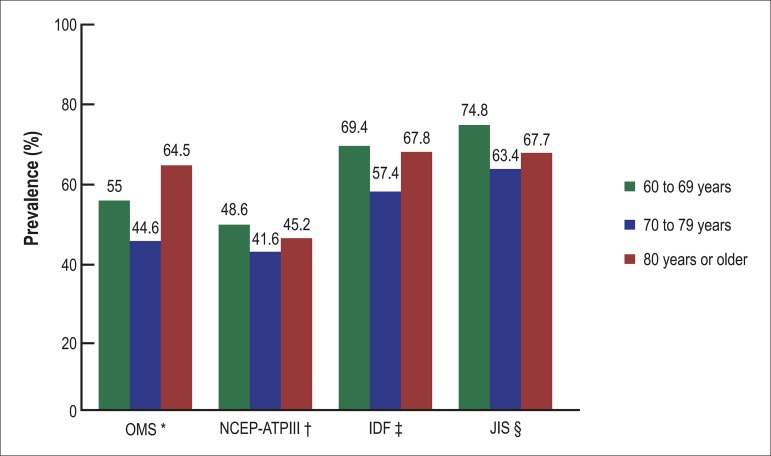
Chart 2 shows the prevalence of MS according to the four diagnostic criteria used, according to age groups (60-69, 70-79 and ≥ 80 years) in both genders.
Chart 2.
Prevalence of metabolic syndrome by age range according to the four criteria. *WHO: World Health Organization; †NCEP - ATP III: Third Report of the National Cholesterol Education Program; ‡IDF: International Diabetes Federation; §JIS: Joint Interim Statement.
The JIS criterion was the one that diagnosed the most MS cases when evaluating all participants (69.1%), in females (68.9%) and in males (69.8%). On the other hand, the NCEP-ATPIII MS criterion diagnosed the least, both in the general population studied (45.2%) and in females (45.6%) and males (44.4%).
The agreement between the criteria used for the definition of MS was analyzed by determining the kappa index, considered moderate between WHO criteria vs. IDF (k = 0.47, 95% CI, 0.35-0.58); WHO vs. NCEP-ATPIII (k = 0.51, 95% CI, 0.40-0.61); WHO vs. JIS (k = 0.45, 95% CI, 0.33-0.56); IDF vs. NCEP-ATPIII (k = 0.55, 95%CI, 0.45 0.65) and NCEP-ATPIII vs. JIS (k = 0.53, 95% CI, 0.43 0.64). The agreement was considered very good between IDF vs. JIS (k = 0.89, 95% CI, 0.83 to 0.95).
Discussion
The population projection study carried out by the Brazilian Institute of Geography and Statistics (IBGE)17 shows that the elderly will have a higher intensity of growth from 2020 on, going from 28.3 million to 52 million elderly individuals in 2040, representing a quarter of the Brazilian population. As for the MS, its prevalence is also on the rise worldwide, which is probably related to the increase in obesity, sedentary lifestyle, changes in dietary habits and the important process of aging. The result of a higher prevalence of MS is the recognized increase in cardiovascular morbimortality18,19.
The literature shows great variability in the prevalence of MS among the elderly, which depends greatly on the criteria used for the diagnosis and also the ethnic and regional characteristics of the study population.
The present study assessed the prevalence and agreement between diagnostic criteria of MS, according to the latest criteria, JIS, compared with the WHO, NCEP-ATP III and IDF criteria in an elderly population treated at the Outpatient Clinic of Internal Medicine and Geriatrics. The prevalence of MS was higher using the JIS criterion (69.1%) followed by the IDF (64.1%), WHO (51.9%) and NCEP-ATPIII (45.2%) criteria. This higher prevalence by JIS and IDF criteria was probably due to the lower cutoff of WC and fasting glycemia established by them20. Alkerwi et al20 found a prevalence of MS of 88% in women and 74% men, aged between 60 and 69 years, using the JIS criterion, with a WC cutoff of 94 cm for men and 80 cm for women.
In a study by Ford et al21, carried out in the United States and using the JIS criterion, with a cutoff of 102 cm for men and 88 cm for women, the prevalence of MS was 59.3% in men and 55.4% in women. According to these authors, their findings differ from those found in Europeans, with a lower prevalence of MS, probably due to the higher cutoff used. With aging, there is an increase in WC due to the accumulation of abdominal fat, as seen in the present study both in men and women, which should be taken into account because of its association between this increase and the risk of mortality from all causes22.
In a study carried out in the city of Novo Hamburgo, state of Rio Grande do Sul, Brazil, among 378 elderly individuals evaluated, aged > 60 years, the prevalence of MS was 50.3% and 56.9% by the NCEP-ATPIII and IDF criteria, respectively, with a higher prevalence in women by the two criteria23. In the present study, the prevalence by NCEP-ATPIII and IDF was also higher in women than in men, 45.6% vs. 44.4% by NCEP-ATPIII and 65.6% vs. 60.3% by the IDF. However, when using the WHO and JIS criteria, the result was different, with a higher prevalence in males, 69.8% vs. 68.9% using JIS and 58.7% vs. 49.4% using WHO criteria. A study carried out in Macapa, state of Amapa, Brazil, showed a prevalence of 18.8% according to NCEP-ATP III criterion and 38.9% by the IDF criterion among elderly African descendants and 34% and 43% among elderly non African descendants, with a higher prevalence among women24.
In Italy2, a study in individuals older than 65 years found a prevalence of MS of 20% in women and 33% in men, using the of NCEP-ATP III criterion. In another study carried out in a Geriatrics service in Turkey25, the prevalence of MS in individuals older than 65 years was 24%, also by the NCEP-ATPIII.
When compared with the results of the present study, considering only the NCEP-ATPIII criterion, there was a higher prevalence of MS in the population by this criterion: 45.6% for women and 44.4% for men, similar to the results of the study in Novo Hamburgo (RS), although not so high. This difference probably reflects the ethnic and regional characteristics that predominate in the population of each region. This becomes clearer when considering a French study in which the prevalence of MS was 11.3% in women and 12.5% in men older than 70 years, using the NCEP-ATPIII criterion26. In Finland27, the prevalence of MS in elderly women by the IDF criterion was higher than by the NCEP-ATPIII, similar to what was observed in a Brazilian study carried out in the state of Minas Gerais28.
In China29, where there is a growing change in society's lifestyle, with the incorporation of Western habits and, thus, an increase in metabolic diseases, a study in a population older than 60 years showed a high prevalence of MS, of 54% in women and 35% in men, according to the IDF criterion. When the NCEP-ATPIII criterion was applied to the same population, the prevalence decreased to 39% and 18%, respectively. In Australia30, the prevalence of MS according to the IDF criterion was 46% in women and 36% in men older than 70 years.
The comparison between studies in the elderly population from other countries31,32 and even in other regions of Brazil demonstrates the importance of regional studies, as the different prevalence values for MS found in these studies indicate the need tostrongly consider the population ethnic aspects and regional habits. The findings demonstrate the difficulty in having a diagnostic criterion that is accurate, sensitive and specific and that can be useful for assessing the general population, overcoming the limitations of regional specificities.
The diagnosis of MS itself identifies an increased cardiovascular risk8, but it is unclear which diagnostic criterion for MS would be the best predictor of cardiovascular events. Assmann et al33 compared the diagnostic criteria of IDF and NCEP-ATPIII in adults between 18 and 65 years as predictors of cardiovascular events during ten years of follow-up. Although most cases of MS have been diagnosed by IDF, the NCEP-ATPIII criterion had higher predictive value for cardiovascular risk. A cohort study in a Chinese population older than 50 years showed a prevalence of MS of 28% in men and 48.4% in women diagnosed by the JIS criterion, and it was associated with increased risk of cardiovascular mortality when three or more components of MS were present34.
A study by Athyros et al35 showed that the prevalence of cardiovascular disease increased in the presence of MS, regardless of the definition used, but it was more evident when using the NCEP-ATPIII criterion, when compared with the IDF. According to a report by He et al29 in elderly Chinese diagnosed with MS by IDF, but not by the NCEP-ATPIII, it increased the chance of coronary heart disease and cerebral vascular accident.
In the present study, the correlation between the diagnostic criteria for MS was moderate between WHO vs. IDF (k = 0.47), WHO vs. NCEP-ATP III (k = 0.51), WHO vs. JIS (k = 0.45), IDF vs. NCEP-ATPIII (k = 0.55), NCEP-ATPIII vs. JIS (k = 0.53) and very good between IDF vs. JIS (k = 0.89). In Luxembourg20, the agreement between the NCEP-ATPIII, IDF and JIS criteria was excellent (k = 0.89), particularly between IDF vs. JIS (k = 0.93). In the United States36 the agreement was k = 0.92 between the NCEP-ATPIII and IDF criteria in postmenopausal women. A study in Africa37 in individuals between 25 and 64 years found an agreement between WHO vs. IDF of k = 0.61, between WHO vs. NCEP-ATPIII of k = 0.59 and NCEP-ATPIII vs. IDF of k = 0.82.
The difference in concordance between the MS diagnostic criteria in different populations is probably due to ethnic characteristics, dietary habits and lifestyle, thus making it difficult to use a single diagnostic criterion for all populations.
Limitations of this study include the sample size and the likely regional specificity, which somehow prevent the extrapolation of these data to the entire elderly population of Brazil and worldwide.
Conclusion
We observed that the prevalence of MS in the elderly population was high using the four diagnostic criteria, particularly by JIS, and the agreement between the diagnostic criteria was considered very good between JIS and IDF, but only moderate among the others. Due to population characteristics of each region, it is clear the need for further regional studies to better assess the prevalence of MS in the elderly and, therefore, to improve disease diagnosis and treatment with cardiovascular risk reduction.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of Doctoral submitted by Maria Auxiliadora Nogueira Saad from Universidade Federal Fluminense.
Author contributions
Conception and design of the research: Saad MAN, Cardoso GP, Cruz Filho, RA; Acquisition of data: Saad MAN; Analysis and interpretation of the data: Saad MAN, Cardoso GP, Martins WA, Velarde LGC, Cruz Filho, RA; Statistical analysis: Velarde LGC; Writing of the manuscript: Saad MAN, Cardoso GP, Martins WA, Cruz Filho, RA; Critical revision of the manuscript for intellectual content: Cardoso GP, Martins WA, Cruz Filho, RA.
References
- 1.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 2.Ravaglia G, Forti P, Maioli F, Bastagli L, Chiappelli M, Montesi F, et al. Metabolic syndrome: prevalence and prediction of mortality in elderly individuals. Diabetes Care. 2006;29(11):2471–2476. doi: 10.2337/dc06-0282. [DOI] [PubMed] [Google Scholar]
- 3.Hildrum B, Mykletun A, Hole T, Midthjell K, Dahl AA. Age-specific prevalence of the metabolic syndrome defined by the International Diabetes Federation and the National Cholesterol Education Program: the Norwegian HUNT 2 study. BMC Public Health. 2007;7:220–220. doi: 10.1186/1471-2458-7-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28(9):2289–2304. doi: 10.2337/diacare.28.9.2289. [DOI] [PubMed] [Google Scholar]
- 5.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 6.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 7.Expert Panel on Detection.Evaluation.and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 8.Brandão AP, Brandão AA, Nogueira AR, Suplicy H, Guimarães JI, Oliveira JE, et al. Sociedade Brasileira de Cardiologia I Diretriz brasileira de diagnóstico e tratamento da síndrome metabólica. Arq Bras Cardiol. 2005;84(supl 1):1–28. [PubMed] [Google Scholar]
- 9.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome - a new worldwide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 10.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiologic and Prevention; National Heart, Lung and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 11.Blazer DG, Hybels CF, Fillenbaum GG. Metabolic syndrome predicts mobility decline in a community-based sample of older adults. J Am Geriatr Soc. 2006;54(3):502–506. doi: 10.1111/j.1532-5415.2005.00607.x. [DOI] [PubMed] [Google Scholar]
- 12.Dik MG, Jonker C, Comijs HC, Deeg DJ, Kok A, Yaffe K, et al. Contribution of metabolic syndrome components to cognition in older individuals. Diabetes Care. 2007;30(10):2655–2660. doi: 10.2337/dc06-1190. [DOI] [PubMed] [Google Scholar]
- 13.Koponen H, Jokelainen J, Keinanen-Kiukaanniemi S, Kumpusalo E, Vanhala M. Metabolic syndrome predisposes to depressive symptoms: a population-based 7-year follow-up study. J Clin Psychiatry. 2008;69(2):178–182. doi: 10.4088/jcp.v69n0202. [DOI] [PubMed] [Google Scholar]
- 14.Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Hipertensão. Sociedade Brasileira de Nefrologia VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1) supl. 1:1–51. [PubMed] [Google Scholar]
- 15.Organização Mundial de Saúde (OMS) Obesidade: prevenção e gestão da epidemia global. Relatório de uma Consulta da OMS. Genebra; 2000. [Google Scholar]
- 16.Geloneze B, Vasques AC, Stabe CF, Pareja JC, Rosado LE, Queiroz EC, et al. HOMA 1-IR and HOMA 2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS) . Arq Bras Endocrinol Metab. 2009;53(2):281–287. doi: 10.1590/s0004-27302009000200020. [DOI] [PubMed] [Google Scholar]
- 17.Instituto Brasileiro de Geografia e Estatística (IBGE) Projeção da população do Brasil por sexo e idade. 1980-2050. Rio de Janeiro: 2008. [Google Scholar]
- 18.Wang J, Ruotsalainen S, Moilanen L, Lepisto P, Laakso M, Kuusisto J. The metabolic syndrome predicts cardiovascular mortality: a 13-year follow-up study in elderly non-diabetic Finns. Eur Heart J. 2007;28(7):857–864. doi: 10.1093/eurheartj/ehl524. [DOI] [PubMed] [Google Scholar]
- 19.Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci. 2004;19(2):195–201. doi: 10.3346/jkms.2004.19.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alkerwi A, Donneau A, Sauvageot N, Lair ML, Scheen A, Albert A, et al. Prevalence of the metabolic syndrome in Luxembourg according to the Joint Interim Statement definition estimated from the ORISCAV-LUX study. BMC Public Health. 2011;11(1):4. doi: 10.1186/1471-2458-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes. 2010;2(3):180–193. doi: 10.1111/j.1753-0407.2010.00078.x. [DOI] [PubMed] [Google Scholar]
- 22.de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallashofski H, Guallar-Casttillon PG, et al. WC elderly collaborators The association between waist circumference and risk of mortality considering body mass index in 65- to 74- year-olds: a meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41(3):805–817. doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rigo JC, Vieira JL, Dalacorte RR, Reichert CL. Prevalência de síndrome metabólica em idosos de uma comunidade: comparação entre três métodos diagnósticos. Arq Bras Cardiol. 2009;93(2):85–91. doi: 10.1590/s0066-782x2009000800004. [DOI] [PubMed] [Google Scholar]
- 24.Medeiros CL. Síndrome metabólica em idosos quilombolas e não quilombolas no Estado do Amapá. Brasília [Mestrado] Brasília: Universidade Católica de Brasília; 2009. [Google Scholar]
- 25.Cankurtaran M, Halil M, Yavuz BB, Dagli N, Oyan B, Ariogul S. Prevalence and correlates of metabolic syndrome (MS) in older adults. Arch Gerontol Geriatr. 2006;42(1):35–45. doi: 10.1016/j.archger.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Guize L, Thomas F, Pannier B, Bean K, Danchin N, Benetos A. [Metabolic syndrome: prevalence, risk factors and mortality in a French population of 62 000 subjects]. Bull Acad Natl Med. 2006;190(3):685–697. [PubMed] [Google Scholar]
- 27.Saukkonen T, Jokelainen J, Timonen M, Cederberg H, Laakso M, Härkönen P, et al. Prevalence of metabolic syndrome components among the elderly using three different definitions: A cohort study in Finland. Scand J P Health Care. 2012;30(1):29–34. doi: 10.3109/02813432.2012.654192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paula HA, Ribeiro RC, Rosado LE, Pereira RS, Franceschini Sdo C. Comparação de diferentes critérios de definição para diagnóstico de síndrome metabólica em idosas. Arq Bras Cardiol. 2010;95(3):346–353. doi: 10.1590/s0066-782x2010005000100. [DOI] [PubMed] [Google Scholar]
- 29.He Y, Jiang B, Wang J, Feng K, Chang Q, Fan L, et al. Prevalence of the metabolic syndrome and its relation to cardiovascular disease in an elderly Chinese population. J Am Coll Cardiol. 2006;47(8):1588–1594. doi: 10.1016/j.jacc.2005.11.074. [DOI] [PubMed] [Google Scholar]
- 30.Adams RJ, Appleton S, Wilson DH, Taylor AW, Dal Grande E, Chitleborough C, et al. Population comparison of two clinical approaches to the metabolic syndrome: implications of the new International Diabetes Federation consensus definition. Diabetes Care. 2005;28(11):2777–2779. doi: 10.2337/diacare.28.11.2777. [DOI] [PubMed] [Google Scholar]
- 31.Qiao Q. Comparison of three different definitions for the metabolic syndrome in non-diabetic Europeans. The Decode Study Group. Br J Diabetes Vascular Dis. 2005;5:161–168. [Google Scholar]
- 32.Athyros VG, Ganotakis ES, Elisaf M, Mikhailidis DP. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr Med Res Opin. 2005;21(8):1157–1159. doi: 10.1185/030079905x53333. [DOI] [PubMed] [Google Scholar]
- 33.Assmann G, Guerra R, Fox G, Cullen P, Schulte H, Willett D, et al. Harmonizing the definition of the metabolic syndrome: comparison of the criteria of the adult treatment Panel III and the International Diabetes Federation in United States American and European Populations. Am J Cardiol. 2007;99(4):541–548. doi: 10.1016/j.amjcard.2006.08.045. [DOI] [PubMed] [Google Scholar]
- 34.Sun DL, Wang JH, Jiang B, Li LS, Li LS, Wu L, et al. Metabolic syndrome vs. its components for prediction of cardiovascular mortality: a cohort study in Chinese elderly adults. J Geriatr Cardiol. 2012;9(2):123–129. doi: 10.3724/SP.J.1263.2012.01172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Athyros V, Ganotakis E, Elisaf M, Liberopoulos E, Goudevenos L, Karagiannis A. Prevalence of vascular disease in metabolic syndrome using three proposed definitions. Int J Cardiol. 2007;117(2):204–210. doi: 10.1016/j.ijcard.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 36.Brown T, Vaidya D, Rogers W, Waters D, Howard B, Tardif J, et al. Does prevalence of the metabolic syndrome in women with coronary artery disease differ by the ATPIII and IDF criteria? J Womens Health (Larchmt) 2008;17(5):841–847. doi: 10.1089/jwh.2007.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelliny C, William J, Riesen W, Paccaud F, Bovet P. Metabolic syndrome according to different definitions in a rapidly developing country of the African region. Cardiovasc Diabetol. 2008;7:27–27. doi: 10.1186/1475-2840-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]