Abstract
Background
Prediction of severity or complexity of coronary artery disease (CAD) is valuable owing to increased risk for cardiovascular events. Although the association between total coronary artery calcium (CAC) score and severity of CAD, Gensini score was not used, it has been previously demonstrated. There is no information about the association between total CAC score and complexity of CAD.
Objectives
To investigate the association between severity or complexity of coronary artery disease (CAD) assessed by Gensini score and SYNTAX score (SS), respectively, and coronary artery calcium (CAC) score, which is a noninvasive method for CAD evaluation in symptomatic patients with accompanying significant CAD.
Methods
Two-hundred-fourteen patients were enrolled. Total CAC score was obtained before angiography. Severity and complexity of CAD was assessed by Gensini score and SS, respectively. Associations between clinical and angiographic parameters and total CAC score were analyzed.
Results
Median total CAC score was 192 (23.0-729.8), and this was positively correlated with both Gensini score (r: 0.299, p<0.001) and SS (r: 0.577, p<0.001). At multivariate analysis, it was independently associated with age (ß: 0.154, p: 0.027), male gender (ß: 0.126, p: 0.035) and SS (ß: 0.481, p< 0.001). Receiver-operating characteristic (ROC) curve analysis revealed a cut-off value > 809 for SS >32 (high SS tertile).
Conclusion
In symptomatic patients with accompanying significant CAD, total CAC score was independently associated with SS and patients with SS >32 may be detected through high Agatston score.
Keywords: Total coronary calcium score, Gensini score, SYNTAX score, Coronary artery disease
Introduction
Coronary artery disease (CAD) is one of the leading causes of mortality and morbidity1,2. Invasive conventional coronary angiography (CCA) is the gold standard technique for diagnosis and the selection of best treatment options for CAD and reveals the severity and complexity of CAD3. Previous studies have shown that CAD severity and complexity assessed by Gensini score and SYNTAX score (SS), respectively, are associated to increased cardiovascular events (CVE) a factor of mortality and morbidity4,5.
CAD severity and complexity have recently attracted increasing interest for CAD evaluation based on the clinical importance and treatment challenge. Gensini and SS are easy to apply and reproducible scoring systems4,6. SS incorporates morphological features of lesions such as total occlusion, bifurcation, length and localizations of lesions based on the myocardial area at risk7. Therefore, some efforts have been made for the prediction of CAD severity and complexity using non-invasive methods in order to identify the patients at high risk for CVE and treatment challenges before CCA8,9.
Coronary artery calcification (CAC) has a role in atherosclerotic plaque formation10,11. It was quantitated by total CAC score called Agatston score. Multidetector computerized tomography (MDCT) currently represents a noninvasive method for accurate quantification of total CAC score12,13. The association between total CAC score and prognostic information about future cardiac events has been previously demonstrated. Some studies have shown that angiographically proven and significant CAD is related to total CAC score14-16.
The purpose of the present study was to investigate the association of total CAC score and CAD severity and complexity assessed by SS and Gensini score, respectively, and to find which one of the two, CAD severity or complexity, is better associated with total CAC score in symptomatic patients with accompanying significant CAD.
Methods
Data was retrospectively collected between January 2012 and February 2013. We enrolled 923 consecutive patients with symptoms suggestive of CAD who underwent 64 - slice computed tomography coronary angiography (CTA) for assessment of significant CAD. Non- enhanced CT scans were obtained for total CAC score immediately before CTA. Indications for CTA were patients with low to intermediate probability of significant CAD, indeterminate diagnostic test results, high clinical suspicion for CAD and, inability to perform non-invasive tests. 709 patients were not eligible for the study. Reasons for non-inclusion are shown in Table 1. Therefore, the remaining 214 patients with 50% or greater luminal stenosis in any major epicardial coronary artery constituted the study population. All patients underwent CCA within two weeks after CTA and performance of CCA was not influenced by total CAC scores.
Table 1.
Number of ineligible patients and reasons for non-inclusion
| n: 709 | |
| Non-significant CAD in CTA, n (%) | 665 (72.1%) |
| Patients with previous bypass surgery, n (%) | 12 (1.3%) |
| Previous coronary stent implantation, n (%) | 19 (2.1%) |
| End- stage renal failure, n (%) | 4 (0.4%) |
| History of valvular replacement, n (%) | 2 (0.2%) |
| Atrial fibrillation, n (%) | 6 (0.6%) |
| Malignancy, n (%) | 1 (0.1%) |
CAD: coronary artery disease; CTA: computed tomography coronary angiography.
SYNTAX score
All patients gave informed consent before enrollment, and the study protocol was approved by the local Ethical Committee. Baseline clinical and demographic characteristics were obtained from all patients. A detailed physical examination was performed including past medical history. Complete blood count, lipid profile and serum creatinine levels were obtained from all patients before CCA. Cardiovascular risk factors were recorded. Hypertension was identified based on prior prescription of antihypertensive drugs or when blood pressure exceeded 140/90 mmHg in at least three measurements. Dyslipidemia and diabetes were defined as prior prescription of antihyperlipidemic and antidiabetic medications or total cholesterol level > 200 mg/dL and fasting glucose levels above 126 mg/dL, respectively. Current smokers were defined as subjects with a positive history of cigarette smoking. Glomerular filtration rate (GFR) was calculated using the Cockcroft-Gault formula17. Body mass index (BMI) was calculated (kg/m2). Comprehensive two-dimensional transthoracic echocardiography including M-mode and, Doppler echocardiography, were performed by an experienced cardiologist before CCA, using a Vivid-S5, GE (United States) instrument, with a 3.6 MHZ transducer. Measurements were performed according to the American Society of Echocardiography guidelines18. LV end-systolic and end-diastolic volumes and ejection fraction were calculated by the Simpson biplane method.
All patients underwent selective coronary angiography, which was performed using the Judkins technique. Significant lesion was defined as a 50% or greater stenosis in the luminal diameter of any major epicardial coronary artery. The presence of significant lesions was determined based on visual estimation. Basal angiographic characteristics of patients such as diseased vessel, left main coronary artery (LMCA), left anterior descending (LAD) coronary artery; right coronary artery (RCA), circumflex coronary artery (Cx), and diseased vessel number were recorded.
SS is mainly associated with CAD complexity and it was calculated using dedicated software, which integrates two components (a) morphological features of each lesion such as dominance, chronic total occlusion (CTO), bifurcation, trifurcation, tortuosity, heavy calcification, lesion length, presence of thrombus, aorto-ostial and diffuse lesions, and (b) weighting factors of lesions based on myocardial area distal to lesion. Lesions with ≥ 50% luminal obstruction in vessels with a diameter ≥1.5 mm were added to provide SS7,8. SS was calculated using dedicated software (version 2.11, www.syntaxscore.com) and all morphological features of each lesion included in SS were recorded.
The SS was divided into two tertiles as follows: low- intermediate risk tertile was ≤ 32 and high-risk tertile was > 32. All angiograms were scored by two experienced interventional cardiologists who were blinded to CAC measurement data.
Gensini score
CAD severity was assessed by Gensini score, which is based on the percentage of luminal narrowing (25%: 1 point; 50%: 2 points; 75%: 4 points; 90%: 8 points; 99%: 16 points, and total occlusion: 32 points). Each coronary lesion score was calculated using percentage of luminal narrowing multiplied by coefficient of coronary segment: the left main coronary artery (LMCA) x5; the proximal segment of the left anterior descending coronary artery (LAD) x 2.5; the proximal segment of the circumflex artery (CX) x 2.5; themid-segment of the LAD x 1.5; the distal segment of the LAD, all segments of the right coronary artery (RCA) and the obtuse marginal artery x 1; and other segments x 0.5. The Gensini score was calculated by summation of individual coronary segment scores4.
Coronary artery calcification measurement
CAC measurement was performed immediately before CTA in all patients. None of the patients had hyperthyroidism and all patients had sinus rhythm during the procedure. Imaging was performed using a 64 - slice CT scanner (Aquilion 64, Toshiba Medical Systems, Tochigi, Japan). CT scan for total CAC score was obtained by prospective gating with collimation (4 × 3.0 mm) with 3-mm reconstructed slice thickness. Tube current and tube voltage were 300 mA, 120 kV, respectively and gantry rotation time 0.4 s19.
Total CAC score was calculated using dedicated software (Vitrea2 version 3.0.9.1, Vital Images, Minnesota). Calcium based on the Agatston method was defined as the presence of a lesion with an area greater than 1 mm2, and peak intensity greater than 130 Hounsfield Units, which was automatically identified and marked with color by the software. All lesions were added to calculate the total CAC score by the Agatston method.
Statistical analysis
SPSS 17.0 statistical software (SPSS Inc., Chicago, IL, USA) and MedCalc software program, release 12.3.0.0 (MedCalc Software, Belgium) were used for statistical analysis. Continuous variables were expressed as mean ± standard deviation (SD) or median and interquartile range as appropriate. Categorical variables were expressed as percentages. The Kolmogorov Smirnov test was used to test normality of distribution of continuous variables. Group means for continuous variables were compared with the Student's t-test or the Mann-Whitney U test, as appropriate. Pearson's or Spearman's correlation analysis was used for assessing correlation between total CAC score and continuous variables depending on Gaussian distributions.
To find independent associates of total CAC score, variables with a p value of ≤ 0.05 at the bivariate correlation analysis and univariate analysis were selected for multiple linear regression analyses. To account for the non-Gaussian distribution of total CAC scores, a log10 {x+1} transformation was made. Triglyceride, glucose, red cell distribution width (RDW), left ventricle ejection fraction (LVEF), Gensini score and SS were also transformed to the natural logarithmic scale and in order to avoid co-linearity when assessing the multivariate model, independent variables were tested for intercorrelation. A two tailed p < 0.05 was considered statistically significant. The Chi-square test examined the correlation between categorical variables and continuous variables. Inter-observer agreement of SS and Gensini score was calculated by using Bland Altman analysis and the intra class correlation coefficient was used to assess intra observer agreement. Receiver-operating characteristic (ROC) curve analysis was performed to detect the cut-off value of total CAC score in predicting SS >32 (high-risk tertile). A p value of ≤ 0.05 was considered statistically significant.
Results
The study population consisted of 214 patients, 170 (79.4%) were males with mean age of 63.5±10.8. A total of 558 lesions with 50% or greater stenosis in the luminal diameter of major epicardial coronary arteries were detected from the CCA data. Single-vessel disease was present in 44 (20.6%), 23 (10.7%), and 15 (7%) patients for LAD, RCA and Cx, respectively. Two- and three-vessel diseases were present in 37.9% and 23.8% of patients, respectively. Nineteen (8.9%) patients had a total CAC score = 0, among them, two and three-vessel disease were present in 4 (21.1%) and 1 (5.2%), respectively, while single-vessel disease was present in 14 (73.7%). Baseline clinical, laboratory and echocardiographic features of patients are shown in Table 2.
Table 2.
Baseline characteristics of the study population
| Age (years) | 63.5 ± 10.8 |
| Male, n (%) | 170(79.4%) |
| Diabetes mellitus, n (%) | 63(29.4%) |
| Hypertension, n (%) | 130(60.7%) |
| Current smokers, n (%) | 64(29.9%) |
| Dyslipidemia, n (%) | 119(55.6%) |
| Total cholesterol, mg/dL | 206.7 ± 42.8 |
| HDL cholesterol, mg/dL | 40.8 ± 8.8 |
| LDL cholesterol, mg/dL | 144.5 ± 30.9 |
| Triglycerides, mg/dL | 153(110-191.3) |
| GFR, mL/min | 95.7 ± 28.8 |
| BMI, kg/m2 | 27.9 ± 2.7 |
| Glucose, mg/dL | 105(93-124) |
| Hemoglobin, g/dL | 13.8 ± 1.6 |
| RDW | 13.4(12.8-14.1) |
| LVEF, % | 55(48-60) |
| Gensini score | 34(17-64) |
| SS | 13(7.0-26.1) |
| Total CAC score | 192(23.0-729.8) |
| Cardiovascular medications | |
| ACE-I, n (%) | 91(42.5%) |
| Beta-blocker, n (%) | 124(57.9%) |
| Statin, n (%) | 81(37.9%) |
| Ca++ channel blocker, n (%) | 27(12.6%) |
Data are expressed in numbers (percentages), mean or median and (interquartile range). Percentages are rounded. SS: SYNTAX score; BMI: body mass index; GFR: glomerular filtration rate; HDL: high density lipoprotein; LDL: low density lipoprotein; LVEF: left ventricular ejection fraction; ACE-I: angiotensin converting enzyme inhibitor; RDW: red cell distribution width; CAC: coronary artery calcium.
Independent associates of total CAC score
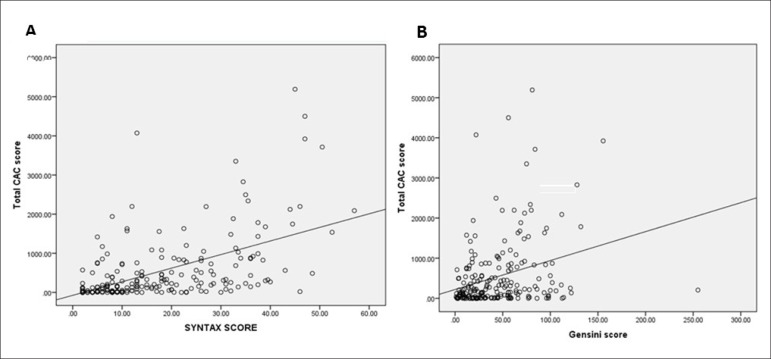
Spearman's correlation analysis showed a significant correlation between total CAC score and SS (r: 0.577, p < 0.001) and Gensini score (r: 0.299, p < 0.001) (Figure 1). Univariate analysis showed that male patients and patients with hypertension had significantly higher total CAC score, (p: 0.004 and p: 0.048), respectively. Total CAC score was significantly higher among patients taking angiotensin converting enzyme inhibitors (ACE-I) (p: 0.013). Bivariate correlation analysis showed that total CAC score was associated with age (r: 0.320, p < 0.001), GFR (r: -0.236, p: 0.001), hemoglobin (r: -0.181, p: 0.008), LVEF (r: -0.268, p < 0.001) and RDW (r: 0.186, p: 0.006).
Figure 1.
A and B show the association between total CAC score and SYNTAX score and Gensini score, respectively. (CAC: coronary artery calcium).
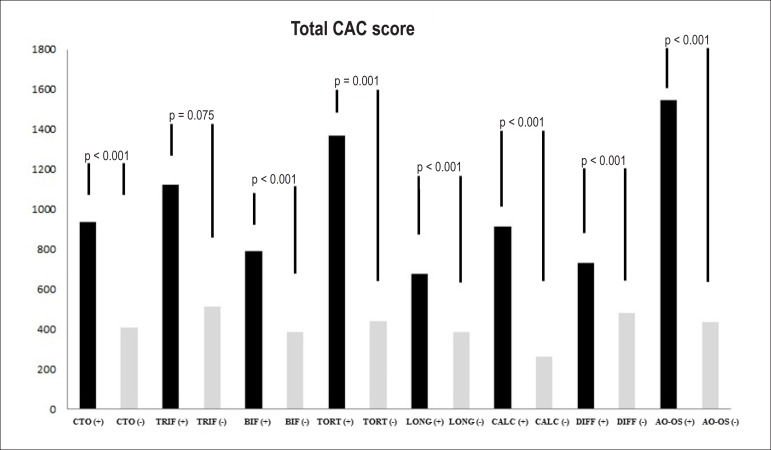
Multiple linear regression analysis was performed to find independent associates of total CAC score. Age (β: 0.154, p: 0.027), male gender (β: 0.126, p: 0.035) and SS (β: 0.481, p < 0.001) were independent predictors of total CAC score. Independent associates of total CAC score are shown in Table 3. Results of correlation analysis between total CAC score and morphological features of lesions included in SS are shown in Table 4. The mean values of total CAC scores based on presence or absence of morphological features of lesions is shown in Figure 2.
Table 3.
Association of total CAC score in multivariate linear regression analysis
| Variables | Standardized β -regression coefficients | p value |
| Age (years) | 0.154 | 0.027 |
| GFR, mL/min | -0.064 | 0.330 |
| Hemoglobin, g/dL | -0.070 | 0.253 |
| RDW | 0.105 | 0.071 |
| LVEF, % | -0.001 | 0.988 |
| Gensini score | 0.030 | 0.666 |
| SS | 0.481 | <0.001 |
| Male | 0.126 | 0.035 |
| Hypertension | 0.038 | 0.516 |
| ACE-I | 0.039 | 0.504 |
SS: SYNTAX score; GFR: glomerular filtration rate; LVEF: left ventricular ejection fraction; ACE-I: angiotensin converting enzyme inhibitor; RDW: red cell distribution width; CAC: coronary artery calcium.
Table 4.
Association between total coronary artery calcium (CAC) score and morphological features of lesions
| r | p value | ||
| Chronic total occlusion | 0.313 | <0.001 | |
| Trifurcation | 0.137 | 0.045 | |
| Bifurcation | 0.202 | 0.002 | |
| Tortuosity | 0.335 | <0.001 | |
| Long lesion | 0.420 | <0.001 | |
| Calcification | 0.751 | <0.001 | |
| Diffuse disease | 0.101 | 0.139 | |
| Aorto-ostial lesion | 0.355 | <0.001 | |
Figure 2.
Mean values of total coronary artery calcium (CAC) score according to presence or absence of morphological features of lesions that were included in SYNTAX score (SS) such as chronic total occlusion (CTO), trifurcation (TRIF), bifurcation (BIF), tortuosity (TORT), long lesion (LONG), calcification (CALC), dıffuse disease (DIFF), aorto-ostial lesion (AO-OS).
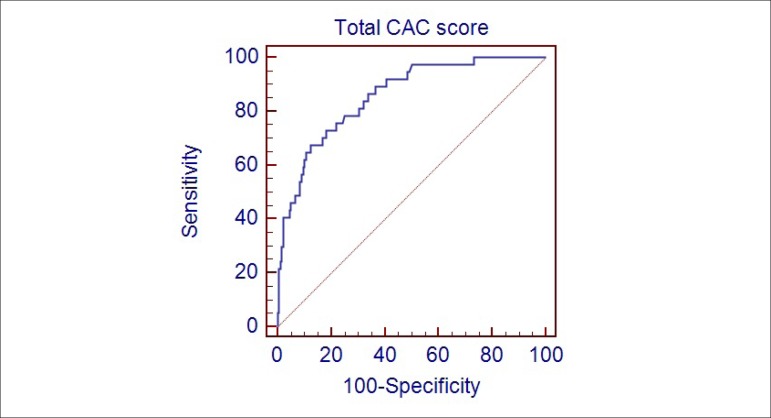
Assessment of cut-off point of total CAC score for patients with SS>32 (high SS tertile)
ROC curve analysis was performed to detect the cut off value of total CAC score in predicting patients with SS > 32 (high SS tertile) (Figure 3). Total CAC score identified patients with SS >32 (high SS tertile) with a specificity of 87.6% (95% CI: 81.8%-92%) and a sensitivity of 67.6% (95% CI: 50.2%-82%) and with a cut-off value of > 809 (AUC: 0.857, 95% CI: 0.803 - 0.901, p < 0.001).
Figure 3.
Receiver–operating characteristic (ROC) curves for total coronary artery calcium (CAC) score in prediction by SYNTAX score (SS) > 32 (high risk tertile).
Analysis of inter- and intra-observer agreement for SS and Gensini score measurements revealed high agreement. Bland-Altman analysis and intra-class correlation for SS and Gensini score showed a mean difference of 0.1 (95% limit of agreement 3.2, -3.2) and a mean difference of -5.1 (95% limit of agreement 30.4, -40.6) as well as an intra-class correlation coefficient of 0.977 (95% CI 0.970 - 0.983) and 0.955 (95% CI 0.942 - 0.966), respectively.
Discussion
The present study showed that Gensini score and SS were significantly correlated with total CAC score. However, age, male gender and SS were independently associated with total CAC score in symptomatic patients with accompanying significant CAD. For total CAC score, a cut-off value > 809 with a specificity of 87.6% and a sensitivity of 67.6% were found for the identification of patients with SS > 32 (high SS tertile).
CAC is mainly limited to the subintimal space of coronary arteries and may occur around the second decade of life. Calcification of atherosclerotic plaque increases according to aging and atherosclerotic progression. CAC is therefore regarded as a marker of coronary atherosclerosis20. Previous studies have considered the association between coronary artery disease and CAC, especially in asymptomatic patients. The prognostic value of CAC in asymptomatic patients has been shown to be independent of traditional risk factors in studies such as the Multi-Ethnic Study of Atherosclerosis (MESA)20. In symptomatic patients, the association between presence of CAC and obstructive CAD has been demonstrated with high sensitivity and low specificity. Therefore, more efforts have been performed for CAC utilization as a useful filter for obstructive CAD before CCA21,22. A limited numbers of studies have examined the value of CAC for prediction of CAD severity and complexity beyond prediction of obstructive CAD in patients with symptoms suggestive of the disease9,23.
Schmermund et al9 reported that CAC score determined through the Agatston method predicts the angiographic extent of CAD in symptomatic patients. Extent of CAD was interpreted as the percentage of flow-limiting luminal narrowing. Likewise, Budoff et al16 reported similar results in symptomatic patients. In the present study, total CAC score was not independently associated with CAD severity assessed by Gensini score, although it was significantly correlated with Gensini score. Our study results did not contradict the results of these two previous studies, because of the different methods used. Our explanations about the results of the present study are: first of all, Gensini score is based on the percentage of luminal narrowing and coefficient of coronary segment that was affected. The percentage of luminal narrowing had a considerable impact on the scoring system and all lesions with ≥ 25% luminal narrowing that were included in the calculation. Previous studies have reported that not all coronary plaques are calcified and CAC score was weakly correlated with severity of luminal stenosis24,25. Therefore, Gensini score may not be associated with total CAC score. Secondly, the association between Gensini score and total CAC score was decreased depending on the effects of traditional risk factors and SS on the Gensini score. Intercorrelation was tested in order to avoid collinearity.
Our study results were compatible with previous reports that age and male gender are independently associated with total CAC score20. The association between total CAC score and SS was evaluated first by Stähli et al23, who previously demonstrated higher Agatston scores in patients treated by complex percutaneous coronary interventions (PCIs) defined as use of the buddy wire technique, kissing balloon, necessity of high pressure balloon, pre or post-dilation and use of a rotablator23. In contrast to the definition of complex PCI by Stähli et al., the SS we used to define complex PCI has been shown in previous studies to be associated with cardiovascular mortality and treatment challenges5,7. SS incorporates a number of morphological features of lesions, such as CTO, bifurcation, trifurcation, tortuosity, heavy calcification, lesion length, aorto-ostial and diffuse lesions. Presence of calcification in CTO and right coronary ostial lesions was demonstrated by Srivatsa et al26 and Popma et al27, respectively. These findings support our study results. Additionally, calcification of lesions adds two points to the scoring system. All morphologic features of lesions were significantly correlated with total CAC score, except for diffuse disease. An association between coronary calcification and endothelial dysfunction and impaired myocardial blood flow in patients with angiographically normal coronary has been previously demonstrated28-30. Altered coronary blood flow in the presence of coronary calcification may affect atherosclerotic plaque progression and formation, which constitute the main determinants of complex CAD formation. Altered coronary blood flow may cause lesion formations including tortuosity, bifurcation or ostial lesion depending on impaired flow dynamics.
Conclusion
Total CAC score was independently associated with complexity of CAD assessed by SS. Studies have shown that SS is associated with increased cardiovascular mortality and treatment challenge5,7. Total CAC score measurement represents a non-invasively anatomical imaging of coronary arteries with a relatively small radiation exposure. Therefore, in clinical practice, total CAC score measurement may predict cardiovascular mortality and treatment challenge before CCA in symptomatic patients with accompanying significant CAD.
Limitations
The study population was relatively small. Quantification of lesions was performed according to visual estimation. However, all angiograms were scored by two experienced interventional cardiologists. Analysis of our study was based on per-patient, rather than per-vessel levels. Therefore, CAC score per-coronary artery was not included in the study. Some large-scale studies, such as MESA, have reported that CAC was less predictive on a per-vessel than on a per patient level. 64-slice MDCT determines coronary calcium with a slice thickness of 3-mm, which may result in missing low levels of coronary calcium. However, many authors concluded that MDCT is equivalent to electron beam tomography for CAC scoring. In our study, the Agatston method was used for CAC scoring, while other methods such as mass score and calcium volume score were not included. However, many published studies have been based on the Agatston method and we continue to use this method in clinical practice.
Acknowledgements
The authors wish to thank Dr İbrahim H. Tanboğa for his constructive comments and assistance to statistical analysis.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
Author contributions
Conception and design of the research: Gökdeniz T, Kalaycıoğlu E, Aykan AÇ, Boyacı F, Turan T, Gül I, Çavuşoğlu G; Acquisition of data: Gökdeniz T, Kalaycıoğlu E, Aykan AÇ, Boyacı F, Turan T, Gül I, Çavuşoğlu G, Dursun I; Analysis and interpretation of the data: Aykan AÇ, Gül I; Statistical analysis: Gökdeniz T, Gül I; Writing of the manuscript: Gökdeniz T, Kalaycıoğlu E, Aykan AÇ; Critical revision of the manuscript for intellectual content: Kalaycıoğlu E.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stoke statistics 2010 update: a report from the American Heart Association. Circulation. 2010;121(7):948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. Erratum in Circulation. 2010;121(12):e259. [DOI] [PubMed] [Google Scholar]
- 2.Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low-and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Higgins CB. Coronary angiography a decade of advances. Am J Cardiol. 1988;62(18):7K–10K. doi: 10.1016/0002-9149(88)90099-9. [DOI] [PubMed] [Google Scholar]
- 4.Ndrepepa G, Tada T, Fusaro M, Cassese S, King L, Hadamitzky M, et al. Association of coronary atherosclerotic burden with clinical presentation and prognosis in patients with stable and unstable coronary artery disease. Clin Res Cardiol. 2012;101(12):1003–1011. doi: 10.1007/s00392-012-0490-9. [DOI] [PubMed] [Google Scholar]
- 5.Farooq V, Serruys PW, Bourantas C, Vranckx P, Diletti R, Garcia Garcia HM, et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) trial. Eur Heart J. 2012;33(24):3105–3113. doi: 10.1093/eurheartj/ehs367. [DOI] [PubMed] [Google Scholar]
- 6.Tanboga IH, Ekinci M, Isik T, Kurt M, Kaya A, Sevimli S. Reproducibility of syntax score: from core lab to real world. J Interv Cardiol. 2011;24(4):302–306. doi: 10.1111/j.1540-8183.2011.00645.x. [DOI] [PubMed] [Google Scholar]
- 7.Ong AT, Serruys PW, Mohr FW, Morice MC, Kappetein AP, Holmes DR, Jr, et al. TheSYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J. 2006;151(6):1194–1204. doi: 10.1016/j.ahj.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Gökdeniz T, Turan T, Aykan AC, Gül I, Boyaci F, Hatem E, et al. Relation of epicardial fat thickness and cardio-ankle vascular index to complexity of coronary artery disease in nondiabetic patients. Cardiology. 2013;124(1):41–48. doi: 10.1159/000345298. [DOI] [PubMed] [Google Scholar]
- 9.Schmermund A, Denktas AE, Rumberger JA, Christian TF, Sheedy 2nd PF, Bailey KR, et al. Independent and incremental value of coronary artery calcium for predicting the extent of angiographic coronary artery disease: comparison with cardiac risk factors and radionuclide perfusion imaging. J Am Coll Cardiol. 1999;34(3):777–786. doi: 10.1016/s0735-1097(99)00265-x. [DOI] [PubMed] [Google Scholar]
- 10.Gussenhoven EJ, Essed CE, Lancée CT, Mastik F, Frietman P, van Egmond FC, et al. Arterial wall characteristics determined by intravascular ultrasound imaging: an in vitro study. J Am Coll Cardiol. 1989;14(4):947–952. doi: 10.1016/0735-1097(89)90471-3. [DOI] [PubMed] [Google Scholar]
- 11.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Jr, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1995;92(5):1355–1374. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 12.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 13.Knez A, Becker C, Becker A, Leber A, White C, Reiser M, et al. Determination of coronary calcium with multi-slice spiral computed tomography: a comparative study with electron-beam CT. Int J Cardiovasc Imaging. 2002;18(4):295–303. doi: 10.1023/a:1015536705455. [DOI] [PubMed] [Google Scholar]
- 14.Raggi P, Callister TQ, Cooil B, He ZX, Lippolis NJ, Russo DJ, et al. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000;101(8):850–855. doi: 10.1161/01.cir.101.8.850. [DOI] [PubMed] [Google Scholar]
- 15.Haberl R, Becker A, Leber A, Knez A, Becker C, Lang C, et al. Correlation of coronary calcification and angiographically documented stenoses in patients with suspected coronary artery disease: results of 1,764 patients. J Am Coll Cardiol. 2001;37(2):451–457. doi: 10.1016/s0735-1097(00)01119-0. [DOI] [PubMed] [Google Scholar]
- 16.Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ, et al. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation. 2002;105(15):1791–1796. doi: 10.1161/01.cir.0000014483.43921.8c. [DOI] [PubMed] [Google Scholar]
- 17.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 18.Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17(10):1086–1119. doi: 10.1016/j.echo.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 19.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography); Society of Atherosclerosis Imaging and Prevention; Society of Cardiovascular Computed Tomography. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. . J Am Coll Cardiol. 2007;49(3):378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Alexopoulos N, Raggi P. Calcification in atherosclerosis. Nat Rev Cardiol. 2009;6(11):681–688. doi: 10.1038/nrcardio.2009.165. [DOI] [PubMed] [Google Scholar]
- 21.Becker A, Leber A, White CW, Becker C, Reiser MF, Knez A. Multislice computed tomography for determination of coronary artery disease in a symptomatic patient population. Int J Cardiovasc Imaging. 2007;23(3):361–367. doi: 10.1007/s10554-006-9189-1. [DOI] [PubMed] [Google Scholar]
- 22.Berman DS, Wong ND, Gransar H, Miranda-Peats R, Dahlbeck J, Hayes SW, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol. 2004;44(4):923–930. doi: 10.1016/j.jacc.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 23.Stähli BE, Bonassin F, Goetti R, Küest SM, Frank M, Altwegg LA, et al. Coronary computed tomography angiography indicates complexity of percutaneous coronary interventions. J Invasive Cardiol. 2012;24(5):196–201. [PubMed] [Google Scholar]
- 24.Simons DB, Schwartz RS, Edwards WD, Sheedy PF, Breen JF, Rumberger JA. Noninvasive definition of anatomic coronary artery disease by ultrafast computed tomographic scanning: a quantitative pathologic comparison study. J Am Coll Cardiol. 1992;20(5):1118–1126. doi: 10.1016/0735-1097(92)90367-v. [DOI] [PubMed] [Google Scholar]
- 25.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study . Circulation. 1995;92(8):2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 26.Srivatsa S, Holmes D., Jr The histopathology of angiographic chronic total coronary artery occlusions ñ changes in neovascular pattern and intimal plaque composition associated with progressive occlusion duration. J Invasive Cardiol. 1997;9(4):294–301. [PubMed] [Google Scholar]
- 27.Popma JJ, Dick RJ, Haudenschild CC, Topol EJ, Ellis SG. Atherectomy of right coronary ostial stenoses: initial and long-term results, technical features and histologic findings . Am J Cardiol. 1991;67(5):431–433. doi: 10.1016/0002-9149(91)90057-r. [DOI] [PubMed] [Google Scholar]
- 28.Lavi S, Bae JH, Rihal CS, Prasad A, Barsness GW, Lennon RJ, et al. Segmental coronary endothelial dysfunction in patients with minimal atherosclerosis is associated with necrotic core plaques. Heart. 2009;95(18):1525–1530. doi: 10.1136/hrt.2009.166017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kullo IJ, Malik AR, Bielak LF, Sheedy 2nd PF, Turner ST, Peyser PA. Brachial artery diameter and vasodilator response to nitroglycerine, but not flow-mediated dilatation, are associated with the presence and quantity of coronary arterycalcium in asymptomatic adults. Clin Sci (Lond) 2007;112(3):175–182. doi: 10.1042/CS20060131. [DOI] [PubMed] [Google Scholar]
- 30.Sekiya M, Mukai M, Suzuki M, Ohtani T, Abe M, Matsuoka H, et al. Clinical significance of the calcification of coronary arteries in patients with angiographically normal coronary arteries. Angiology. 1992;43(5):401–407. doi: 10.1177/000331979204300505. [DOI] [PubMed] [Google Scholar]