Abstract
Objective: To describe the postgraduate surgical skills training programme of the Flemish Society of Obstetrics and Gynaecology (VVOG*). Laparoscopic surgical techniques and indications have increased substantially during the past two decades. From surgeons it is expected that they keep up with all techniques and should be able to perform all relevant procedures. Learning new procedures in daily practice is hazardous and difficult to achieve. A training experience with cadaver surgery could improve the course and outcome of surgery on patients. We present the objective, structure, and outcome of the endoscopic postgraduate training course.
Structure: The overall objective of the endoscopic postgraduate training course is to refresh anatomical knowledge and improve general gynaecological laparoscopic surgical skills. The VVOG endoscopic training programme is based on black box training, followed by pig surgery. New is the possibility to perform surgical procedures on specifically prepared human cadavers. The course consists of an anatomical teaching session followed by lectures with videotaped procedures on the anatomical exploration of the pelvis, laparoscopic hysterectomy and pelvic lymphadenectomy. During the hands-on session the participant performs the surgical procedures in a controlled, nonthreatening and interactive way under the guidance of an experienced trainer.
Conclusions: All participants provided feedback on their experiences. The evaluation of the workshop revealed that this course is an opportunity to practise and improve clinical laparoscopic skills of gynaecological procedures and anatomy. Attending the course was regarded as of genuine additional value for surgical practice.
Keywords: Laparoscopy, endoscopy, surgery, training, skills, performance, postgraduate, VVOG, endogent
Introduction
Clinicians should have a good basic knowledge before performing any surgical procedure on a patient. It is difficult for practising gynaecologists and last year trainees to gain adequate experience in new laparoscopic surgical procedures. Postgraduate courses have as goal to improve the knowledge and to increase surgical skills. The traditional training programme is based on simple black box modules, computer models, animal models followed by learning on patients under supervision of a trainer. An additional possibility and extra-step is training on fresh or embalmed human cadavers. Performing surgical procedures in these circumstances is close to real life without the stress of operating on a living patient.
In the present paper, we present the objectives, structure, outcome and acceptance of postgraduates course of the VVOG, specifically aimed to improve the surgical skills and performance of gynaecologists.
Structure
The course was started in June 2010 as an initiative of the BIG GE (‘Bijzondere Interessegroep Gynaecologische Endoscopie’ or ‘the Particular interest group on gynaecological endoscopy’) of the VVOG and had as initial goal to improve the experience with more advanced laparoscopic gynaecological procedures.
Human cadavers
All cadavers were from women who donated their body to medical science. All cadavers were prepared according to the Thiel technique (Thiel, 2002) and procedures were performed at the Laboratory of Human Anatomy Ledganck, Ghent University, Gent, Belgium.
Preparation of the participants
All participants were gynaecologists. Before entering this course they had to attend two other types of courses: the basic course with exercises in the black box (half day) and the advanced course with live surgery on pigs (2 day course).
The cadaveric course started with interactive lectures on the embalming technique and the preparation of the corpses, the pelvic anatomy, the laparoscopic positioning, followed by videos on laparoscopic hysterectomy, pelvic sidewall exploration and pelvic and para-aortic lymphadenectomy.
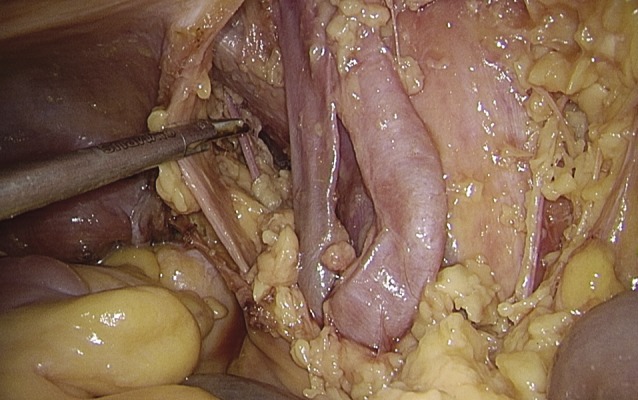
The anatomy of the anterior abdominal wall was reviewed from a surgical point of view with positioning of the trocars (Fig. 1) and the laparoscopic view of the pelvis (Fig. 2). The practical approach of opening the pelvic side wall, with identification of the ureter and its relation to the uterine artery was discussed. The participant should be able to dissect the ureter from the bifurcation of the common iliac artery to the cross of the uterine artery and if possible the bladder, open the pararectal and paravesical spaces (Fig. 3), clamp the uterine artery, dissect the bladder from the isthmus and perform a hysterectomy with ultrascission. Furthermore the pelvic sidewall vessels, and the obturator nerve should be dissected, with the removal of all lymphatic structures surrounding them (Fig. 4). At the end of the procedure an anatomical view of the pelvic sidewall, with clear identification of all structures should be obtained. During the hands-on procedure the trainer’s role is to facilitate the surgical procedures performed by the trainees in a controlled, nonthreatening and interactive way. This approach allows for interactive discussion on the used surgical techniques and points out the possible complications.
Fig. 1. Flowchart search strategy of databases .

Fig. 2. Laparoscopic view of the pelvis.
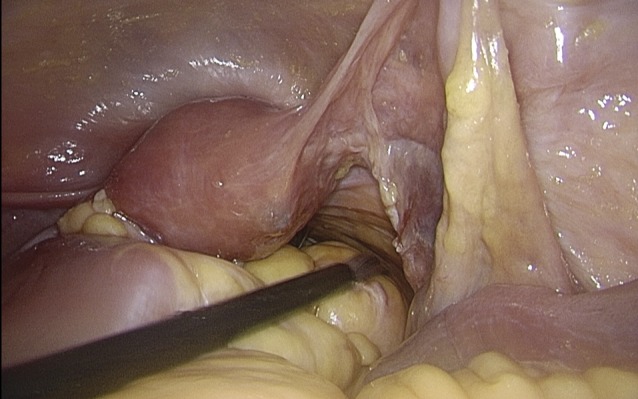
Fig. 3. Opening of the pelvic side wall.
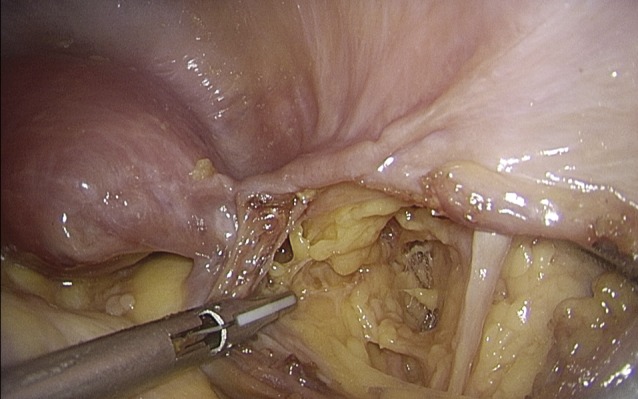
Fig. 4. Dissection of the pelvic side wall with identification of the major vessels, nerves and lymphatic tissue.
Setting
The faculty included 3 to 4 experienced laparoscopic surgeons in order to train simultaneously on three cadavers. Per cadaver there was 1 trainer and two trainees. Figure 3 shows the setting in the Ledeganck laboratory.
Results
The VVOG endoscopic training course was organized for the first time in June 2010 and until now 5 courses have been done with a total of 27 participants (15 female and 12 male gynaecologists). The postgraduate course was initiated as an extension of the existing laparoscopic training programme for trainees of the Flemish Society of Obstetrics and Gynaecology. The program can be found at the website of the VVOG (www.vvog.be/endogent) or at www.endogent.be. Each participant had to fill in an evaluation questionnaire at the end of the course. In table 1 the results are shown. The questionnaire also included the possibility to give free remarks on the course (Table 2).
Table I. Appreciation-score according to the evaluation questionnaire.
| – Anatomy and theory hysterectomy | 95% |
| – Anatomy and theory lymphadenectomy | 93% |
| – Practical exercise hysterectomy | 98% |
| – Practical exercise lymphadenectomy | 95% |
| – Overall score | 99% |
Table II. Feedback remarks of the participant.
| – The small groups have a major advantage in learning |
| – Fantastic course, should be repeated |
| – If possible should be followed by courses in real life |
The average age of the participant was 47 years (range 33-57) and the average lapse of time since certification as a gynaecologist was 17 years (range 3-30). The overall rating of this course was 99%, which is extremely high. The cadaver surgery course was found to be very valuable and all participants would recommend the workshop to their colleagues and trainees. The course not only allowed for a refreshment of anatomy knowledge and surgical procedures, but it also gave the possibility to have an interaction with colleagues and peers regarding daily surgical practice.
Discussion
Laparoscopic gynaecological surgical techniques have increased considerably the last decades. Since laparoscopic surgery tends to be more stressful than open surgery, it is therefore mandatory that laparoscopic surgeons have the opportunity to gain good technical skills (Berguer et al 2001). Laparoscopy has an established place in general gynaecology and in gynaecological oncological surgery. Oncological staging operations in cervical and ovarian cancers have risks but provide considerable opportunities in tailoring the treatment (Tjalma, 2003; Tjalma 2005). Theoretical and practice based knowledge is the keystone in the medical management. For the general gynaecologist it is difficult to keep up with all these new techniques. The principle of ‘see one, do one and teach one’ cannot ethically be justified and from a medical legal point of view it is dangerous to perform operations in which one never has been trained.
The course was developed as an extension of the existing training program for gynaecologists. The aim was to learn laparoscopic procedures in a relaxed and safe surrounding in order to improve surgical skills. Pelvic surgery and laparoscopic surgery in particular demands a detailed knowledge of topographical anatomy. Our anatomical knowledge principally depends on lectures and on training in the dissection room during medical school. To learn anatomy by heart is considered old-fashioned and nowadays in medical school the anatomical training programmes and dissection courses are reduced in favour of simulation models. However, up till now computer models haven’t shown to be effective in clinical teaching (Sutherland et al., 2006), while the evidence regarding cadaver dissection as the best way to learn topographical anatomy is growing (Raferty, 1996; Willan et al., 1996; Gordinier et al., 2005; Barton et al., 2009).
In the training program for specialists in Belgium there is no formal anatomical surgical teaching and examination in contrast to other countries. During our training as gynaecologist we gradually increase our knowledge by seeing from our tutors and performing operations under guidance.
The last decades the field of obstetrics and gynaecology has expanded enormously; as a consequence a training of 5 or 6 years is insufficient to gain experience in all fields of expertise. The opportunities to gain practical experience in common surgical procedures like for instance hysterectomies are reduced, also due to the reduction in numbers. Indeed, almost ten years ago it was already established that newly qualified gynaecologists had less surgical skills than their predecessors (Eisenkop and Spirtos, 2004). Furthermore there is a reduction in working hours as a result of the European Working Time Directives, which leads to lesser time to perform surgery. Like colleagues from other disciplines of surgery, we feel that the graduate and postgraduate surgical training is compromised (Monkhouse, 1996; Ger, 1996).
These diminishing opportunities to perform common operative laparoscopic procedures during the training period were acknowledged by the training program committee. Therefore an alternative approach to learn laparoscopic surgical skills based on training in animal models was introduced. These surgical model training have proven to enhance the surgical skills and increase the competence (Taylor and Hammond, 2004; Lentz et al., 2005; Winkelmann, 2007; Goff, 2008 Barton et al., 2009; Larsen et al, 2012). The rabbit and pig models in our training programs allow the resident to develop confidence and experience in surgical handling.
However, these models do not reproduce the anatomical configuration of the human female pelvic viscera. Gynaecologic surgery involves operating near the bowel, bladder, ureter and the major vessels in a well-established fashion. Human cadaver surgery allowed operating in a real-life setting. The surgical approach of dissecting and cutting of the different structures in the pelvis can be practised with the bowel, bladder, ureter, and major blood vessels in the immediate vicinity.
Laparoscopic cadaver dissection sessions are known to improve surgical skills (Levine et al., 2009). Despite the fact that a benefit of integrating cadaver dissection into a resident training program in obstetrics and gynaecology has been proven, cadaver surgery is not yet integrated in our training programme (Corton et al., 2003). However classical enbalming of the cadavers does not allow for laparoscopic surgery: the traditionally formalin-fixed cadavers are less useful because the fixation causes (1) tissue rigidity (2) loss of tissue texture, colour and consistency (3) limited preservation of surgical planes, and spaces, and (4) difficulty in identifying small structures such as autonomic nerves (Barton et al., 2009). The embalmed bodies according to Thiel have a more or less elastic tissue structure, which is completely different from the traditional formalin-fixed cadavers. This results in well preserved organs and tissues with regard to colour, consistency, flexibility and plasticity. The articular joints remain freely movable and the peritoneal cavity can be inflated for laparoscopic procedures. Moreover, in the embalmed bodies it is possible to dissect the thin tissue layers from the underlying structures (Barton 2009, Kerckaert, 2008).
Teaching in a small group, one cadaver per two trainees and an experienced teacher, was regarded as essential in the training session. The opportunity to perform difficult surgical steps in a nonthreatening situation is unique. For instance opening the pelvic sidewall and identifying the ureter is very realistic in these circumstances. The participant hesitated in the beginning but once started, motivated and guided by their private teacher, they were eager to extend their surgical explorations. Furthermore, the direct response and interaction gave the opportunity to learn from each other and practice standard techniques. Anxiousness to create an injury is often the basis for a complication. The principles of safe surgery include the recognition of landmarks. It is only by training that one develops learning points, allowing you to avoid complications.
The direct feedback at the surgical table of participants revealed that cadaver dissection enhanced their understanding of pelvic surgical anatomy and gave confidence in performing standard and new procedures.
The structured evaluation afterwards confirmed that all participants found it a valuable learning experience, which improved their surgical capabilities. The approach was called refreshing, something they never had done before. Participants would encourage their colleagues and trainees to attend this postgraduate surgical workshop.
Since no validated tools were available to measure the surgical performance before and after the course, it is impossible to assess what the long-term impact would be on the surgical development of the attendees. Hammond et al reported that the participants of a surgical workshop, being contacted 6 months after the workshop, all reported an increased confidence in their surgical ability in less common surgical situations, which they ascribed to attending the workshop (Hammond et al., 2004).
Live surgery by experienced surgeons has been done since mankind. However live surgery does not provide the possibility for the trainees to get hands-on experience. From a medical legal point of view it would be a major step forward if we could learn new techniques on embalmed bodies.
Regardless how one looks at surgical training it is largely based on ‘bed-side’ teaching and remains an apprenticeship. The last two decades several complex new techniques like radical trachelectomy or sentinel node procedures have been introduced. Without shame we have to acknowledge that the majority of us learned these new techniques by performing them (under supervision) on patients.
The next step in this course could be the availability of internet databases with video presentations demonstrating standard procedures as well as atypical situations, including the management of complications (Cibula and Kesic, 2009; Hoffman and Bodurka, 2009). Moreover we should consider to organize, as the attendees mentioned, live surgical teaching sessions in our hospital.
Conclusion
Human cadaver surgery in small groups, consisting of two trainees and one teacher, is a useful model for gynaecologists. This model provides the opportunity to gain more knowledge in anatomy and get acquainted with laparoscopic procedures in a close to real life situation, this without the stress of operating on a living patient. It allows the participants to perform a surgical procedure in a controlled, nonthreatening and interactive way under the guidance of an experienced trainer. Short-term evaluation of the course yielded appreciation scores of more than 90 %. It provoked the desire to do more. What the long-term impact will be on managing patients is difficult to measure. Maintaining surgical skills is essential for a good performance. The Flemish Society of Obstetrics and Gynecology will offer this workshop twice yearly to their members in order to improve and extend laparoscopic procedures. For the future this approach should be incorporated in the training program of gynaecologists.
Acknowledgments
We would like to pay tribute to all the women who donated their bodies to science. Due to them we can take better care of women tomorrow. We thank the technical staff of the anatomical laboratory of the Ledeganck of the University of Gent for their support. In particular we would like to thank Mr. Aron De Smet and his staff for all preparations. Gratitude to the Flemish Society of Obstetrics and Gynecology (VVOG), and in particular the interest group gynaecological endoscopy (BIG gynaecological endoscopy) for their support to extend the endoscopic training program. Thanks to the logistic and enthusiastic support of Marleen Parisis and Christa Grootaert, secretaries of the VVOG. The support from the pharmaceutical industry Ethicon Endo-Surgery, Inc a Johnson-Johnson company and Ethicon Women’s Health & Urology, The Olympus Company Belgium provider of the endoscopic hardware and laparoscopic instruments for sponsoring the course with their material en educational knowledge. Thanks to the faculty and all participants.
References
- Barton DPJ, Davies DC, Mahadevan V, et al. Dissection of soft-preserved cadavers in the training of gynaecological oncologists: Report of the first UK workshop. Gynaecol Oncol. 2009;113:352–356. doi: 10.1016/j.ygyno.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Berguer R, Smith WD, Chung YH. Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc. 2001;15:1204–1207. doi: 10.1007/s004640080030. [DOI] [PubMed] [Google Scholar]
- Cibula D, Kesic V. Surgical education and training in gynaecological oncology I: European perspective. Gynecol Oncol. 2009;114:S52–55. doi: 10.1016/j.ygyno.2009.02.021. [DOI] [PubMed] [Google Scholar]
- Corton MM, Wai CY, Babak V, et al. A compre-hensive pelvic dissection course improves obstetrics and gynecology resident proficiency in surgical anatomy. Am J Obstet Gynecol. 2003:647–651. doi: 10.1067/s0002-9378(03)00881-0. [DOI] [PubMed] [Google Scholar]
- Eisenkop SM, Spirtos NM. The relative importance of surgical training and laboratory research in a gynaecological oncology fellowship. Int J Gynecol Cancer. 2004;14:23–34. doi: 10.1111/j.1048-891x.2004.014164.x. [DOI] [PubMed] [Google Scholar]
- Ger R. Basic surgical training. 4: American and British scenes compared. Clin Anat. 1996;9:173–174. doi: 10.1002/(SICI)1098-2353(1996)9:3<173::AID-CA8>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- Goff BA. Changing the paradigm in surgical education. Obstet Gynecol. 2008;112:328–332. doi: 10.1097/AOG.0b013e3181802163. [DOI] [PubMed] [Google Scholar]
- Gordinier ME, Granai CO, Jackson ND, et al. The effects of a course in cadaver dissection on resident knowledge of pelvic anatomy: an experimental study. Obstet Gynecol. 2005;86:137–139. doi: 10.1016/0029-7844(95)00076-4. [DOI] [PubMed] [Google Scholar]
- Hammond I, Taylor J, Obermair A, et al. The anatomy of complications workshop: an educational strategy to improve the training and performance of fellows in gynecologic oncology. Gynecol Oncol. 2004;94(3):769–773. doi: 10.1016/j.ygyno.2004.06.022. [DOI] [PubMed] [Google Scholar]
- Hoffman MS, Bodurka DC. Gynecol Oncol. 2009;114:S47–51. doi: 10.1016/j.ygyno.2008.12.023. [DOI] [PubMed] [Google Scholar]
- Kerckaert I, Van Hoof T, Pattyn P, Herde K. Proceeding ENDOGENT: centre for anatomy and invasive techniques. Anatomy (International journal of Experimental and Clinical Anatomy) 2007;1:1–2. [Google Scholar]
- Larsen CR, Oestergaard J, Ottesen BS, et al. The efficacy of virtual reality simulation training in laparoscopy: a systematic review of randomized trials. Acta Obstet Gynecol Scand. 2012;91:1015–1028. doi: 10.1111/j.1600-0412.2012.01482.x. [DOI] [PubMed] [Google Scholar]
- Lentz GM, Mandel LS, Goff BA. A six-year study of surgical teaching and skills evaluation for obstetric/gynecologic residents in porcine and inanimate surgical models. Am J Obstet Gynecol. 2005;193:2056–2061. doi: 10.1016/j.ajog.2005.07.064. [DOI] [PubMed] [Google Scholar]
- Levine RL, Kives S, Cathey G, et al. The use of lightly embalmed (fresh tissue) cadavers for resident laparoscopic training. J Minim Invasive Gynecol. 2006;13:451–456. doi: 10.1016/j.jmig.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Monaghan JM, De Barros Lopes T. BBC; 2001. NCOG Newcastle Live Surgery. [Google Scholar]
- Monkhouse S. Basic surgical training. 3: A view from Ireland. Clin Anat. 1996;9:171–172. doi: 10.1002/(SICI)1098-2353(1996)9:3<171::AID-CA7>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Raftery AT. Basic surgical training.1: Postgraduate surgical examinations in the UK and Ireland. Clin Anat. 1996;9:163–166. doi: 10.1002/(SICI)1098-2353(1996)9:3<163::AID-CA5>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- Sutherland LM, Middleton PF, Anthony A, et al. Surgical stimulation: a systematic review. Annal Surg. 2006;243:291–300. doi: 10.1097/01.sla.0000200839.93965.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JD, Hammond IG. The freshly killed pig: a model for surgical training in gynecologic oncology. Aust NZ J Obstet Gynecol. 2004;44:146–148. doi: 10.1111/j.1479-828X.2004.00219.x. [DOI] [PubMed] [Google Scholar]
- Thiel W. Erg inzung fiir die Konservierung ganzer Leichen nach W. Thiel. Ann Anat. 2002;184:267–269. doi: 10.1016/s0940-9602(02)80121-2. [DOI] [PubMed] [Google Scholar]
- Tjalma WA. Three pathognomonic signs of a laparoscopic complication. Acta Obstet Gynecol Scand. 2005;84:101–102. doi: 10.1111/j.0001-6349.2005.0423c.x. [DOI] [PubMed] [Google Scholar]
- Tjalma WA. Cervical cancer and laparoscopic staging lymphadenectomy. Int J Gynecol Cancer. 2003;13:391. doi: 10.1046/j.1525-1438.2003.13183.x. [DOI] [PubMed] [Google Scholar]
- Willan P. Basic surgical training. 2: Interactions with the undergraduate medical curriculum. Clin Anat. 1996;9:167–170. doi: 10.1002/(SICI)1098-2353(1996)9:3<167::AID-CA6>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Winkelmann A. Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ. 2007;41:15–22. doi: 10.1111/j.1365-2929.2006.02625.x. [DOI] [PubMed] [Google Scholar]


