Abstract
The history of sonography in Obstetrics and Gynaecology dates from the classic 1958 Lancet paper of Ian Donald and his team from Glasgow. Fifty years on it is impossible to conceive of practising Obstetrics and Gynaecology without one of the many forms of ultrasound available today. Technological developments such as solid state circuitry, real time imaging, colour and power Doppler, transvaginal sonography and 3/4D imaging have been seized by clinical researchers to enhance the investigation and management of patients in areas as diverse as assessment of fetal growth and wellbeing, screening for fetal anomalies, prediction of pre-eclampsia and preterm birth, detection of ectopic gestation, evaluation of pelvic masses, screening for ovarian cancer and fertility management. Ultrasound guided procedures are now essential components of fetal therapy and IVF treatment. This concise history is written by someone who has witnessed each of these advances throughout the ultrasound era and is able to give perspective to these momentous happenings.
Keywords: sonography, ultrasound, Ian Donald, Real- time ultrasound, 3D ultrasound, Doppler, fetal biometry, fetal abnormalities, preterm birth, pre-eclampsia, fetal chromosome abnormalities, fetal therapy, early pregnancy disorders, pelvic masses, ovarian cancer screening, IVF
Introduction
It is often difficult to know when most developments in medicine actually begin. They tend to evolve and many people will claim the credit of being the first to make the breakthrough. With Ultrasound in Obstetrics and Gynaecology there is no such doubt for it had a very definite beginning with the1958 classic Lancet paper (Donald et al., 1958) by Ian Donald, John McVicar, and Tom Brown “The investigation of abdominal masses by pulsed ultrasound”. Actually this is an unfortunate title because it does not identify what was truly unique about the paper which is that it was entirely devoted to ultrasound studies in clinical obstetrics and gynaecology and contained the first ultrasound images of the fetus and also gynaecological masses. The other unique feature was that these were the first images taken with a compound contact scanner which was the first practical scanning machine.
All developments of ultrasound diagnosis (or Sonography) in Obstetrics and Gynecology date from this seminal paper and this short history is a personal evaluation of the subsequent timeline of key events and breakthroughs up to the present time.
Before Donald
It would be short-sighted to write about the development of medical ultrasound without mentioning some of the great scientists of the 19th and 20th Century whose conceptual advances paved the way for the modern ultrasound machine. Thomas Young in 1801 described “phase shifting” in relation to light waves but this concept is used in ultrasound phased array systems to control interference patterns and is used in the production of 3D images. Christian Doppler in 1842 described what we now call the “Doppler effect” in relation to the motion of stars but this principle is now used as the basis for blood flow studies in pelvic vessels and the fetus. Pierre Curie in 1880 described the piezo electric effect whereby mechanical distortion of ceramic crystals would produce an electric charge; the reverse of this effect is used in all transducers to generate ultrasonic waves. His pupil Paul Langevin in1915 built the first hydrophone which used ultrasonic waves to locate the position and distance of submarines and is the principle behind the measurement of the fetus and abdominal masses by ultrasound. The development of Radar by Watson-Watt and his team using electro-magnetic waves in 1943 was later adapted for ultrasound to produce two dimensional images.
The first simple A-scan metal flaw detectors and modifications of this equipment were used medically in 1949 by George Ludwig at MIT to locate gallstones and John Julian Wild at the Technical Research Institute in Minnesota to detect breast masses. In 1953 Inge Edler and Carl Hertz in Lund University adapted a metal flaw detector to obtain M-mode recordings from the adult heart. Wild together with his engineer John Read published the first 2D images in 1952 but his efforts were directed towards tissue characterisation especially of breast tumours and the accolade for producing the first tomographic images of human anatomy must go to Douglass Howry in Denver who published his landmark paper (Howry, 1952) in the same year.
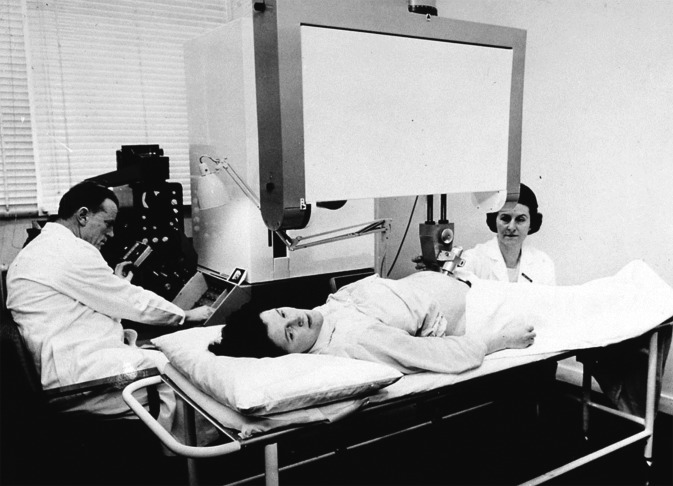
There was a major problem however with the Howry approach which depended on immersing the body part to be examined in degassed water (called water delay scanning) to avoid artifactual echoes from superficial structures. As shown in Figure 1, the equipment was inelegant and uncomfortable for the patient and it seems unlikely that ultrasound diagnosis would have made the breakthrough into becoming the most widespread imaging modality in clinical use was it not for the development of the compound contact scanner by Donald and Brown in the late 1950’s.
Fig. 1. Douglass Howry (a) whose second Tomograph machine called the Pan Scanner (1958) consisted of a semicircular tank with plastic film in contact with the skin of the patient. Note the elegant seating arrangement (b).

Ian Donald
Donald was a tall red haired charismatic Scottish obstetrician gynaecologist with a brilliant mind and a quick temper. He was a most generous and principled man whose anti-abortion stance denied him honours in his own county. He worked feverishly partly because he was a workaholic but principally because he had severe rheumatic heart disease (he needed mitral valve operations on at least three occasions) and every moment was precious to him. It was probably fortunate that Donald knew little of the work being carried out in Denver so armed with some knowledge of radar technology which he learned in the air force, he got together with a very clever engineer called Tom Brown and with help from a local engineering company developed the world’s first contact compound 2D ultrasound scanning machine called the Diasonograph. He and his team published their seminal pioneering paper in the Lancet in 1958. It begins with the physics of ultrasound scanning techniques, safety experiments, ultrasound images of pregnancy, the fetus and gynaecological tumours, and a really detailed description of the strengths, weaknesses and potential of this new technique. The ultrasound images were crude and bistable (i.e. totally lacking grey scale) and static with the image being slowly created on a cathode ray tube by rocking the transducer slowly over the abdomen. But the starting gun had been fired and the ultrasound race had begun.
Fig. 2. Donald in action with the Mark 3 Diasonograph in 1960.
Fig. 3. First page of the most famous paper in Obstetric Ultrasound – the start of the journey.
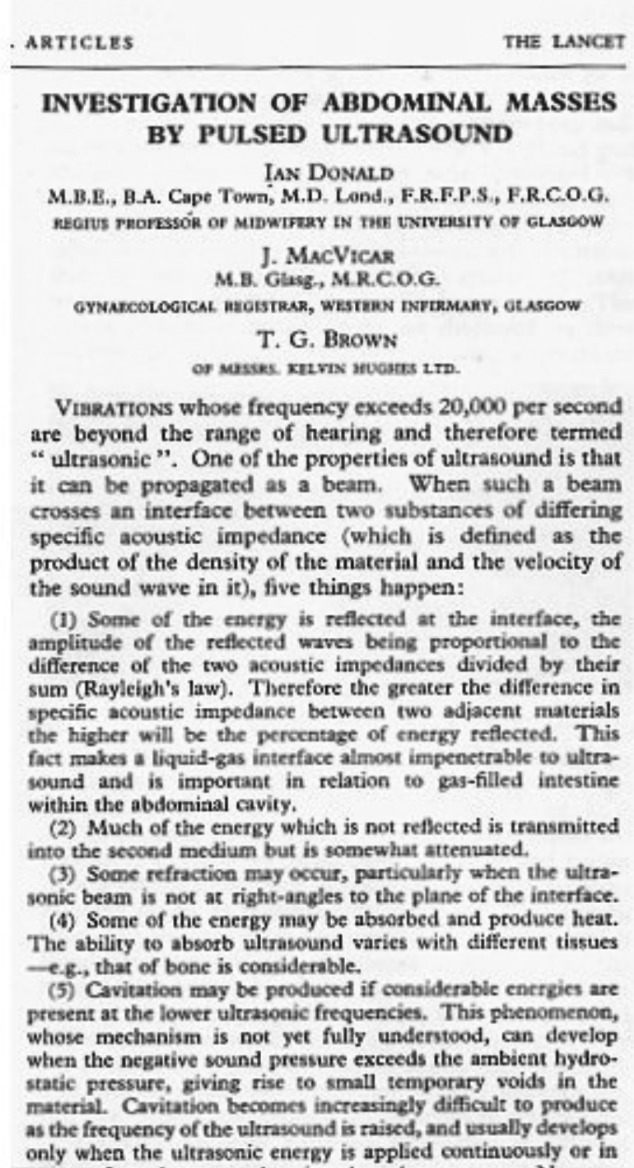
Fig. 4. Images from Donald’s 1958 paper. The picture above (a) is the first ultrasound image of a fetal head. Picture (b) demonstrates malignant ascites in a case of ovarian carcinoma.

The Static Scanner Years
Equipment development
During the next decade a large number of static scanning machines were made. They were initially built in research centres where it was essential always to have dedicated physicists on hand for these were pre-transistor days and the equipment was prone to develop electronic faults. Compared to today’s sleek real-time digital scanning machines, the Diasonograph was the equivalent of Babbage’s difference engine to the modern laptop. It was 8 ft in height and occupied about one-third of the scanning room. The gantry that housed the probe was very large and had to be physically shifted with no small effort to alter the scanning plane. Many people, especially the Americans, unkindly called it the Dinosaurograph. However, it had positive features which allowed users to take a lead in the early ultrasound biometry. For example, it had by far the best image resolution compared to its rivals.
The rigid gantry frame meant that reproducible scans could be made at any angle and in any plane, although if the fetus moved it meant beginning the lining up process again which could be time-consuming. The probe was on a pulley system and could be skimmed with ease across the woman’s abdomen as the static image was built up on the oscilloscope. The first contact machine developed in America was the Physionics (to become the Picker machine) which emanated from Howry’s laboratory in Denver and was used for ObGyn scanning by Horace Thomson and Ken Gottesfeld. It had an articulated scanning arm which was easy to manipulate but it made the obtaining of reproducible planes more difficult and the resolution and sensitivity to low level echoes was initially poor.
Similar style machines were built in Vienna by Kretztechnic (used by Alfred Kratochwil), in Copenhagen by Hewlett Packard (used by Jens Bang and Hans Hendrick Holm) and in Japan by Aloka (used by Hsiao Takeuchi). Both Kretztechnic and Aloka developed commercial transvaginal transducers in the mid 1960’s but the potential of transvaginal scanning was not realised until the advent of real time imaging. Two distinctly different machines compared to the static machines described above were also built in the mid 1960’s. In Germany, Richard Soldner an engineer who worked for Siemens developed the first (almost) real time scanner which consisted of a very large fluid filled plastic membrane as the scanning head which housed 3 rotating transducers in front of a parabolic mirror to produce flickering images at 15 frames per second. Compared to the Diasonograph the image resolution was poor yet this machine was purchased widely in German speaking countries and by the late 1960’s was probably the most commonly used machine in Europe. Initially exponents such as Manfred Hansmann from Bonn and Hans Jurgen Hollander from Munster used the machine like a static scanner but eventually the real time facility was found to be useful especially for invasive procedures.
At the Commonwealth Accoustic Laboratories in Australia George Kossoff one of the most brilliant engineers in the history of medical ultrasound built the Octason static scanner in 1962. This machine followed the Howry principle of water delay scanning with the patient lying face down on a plastic tank containing a large amount of degassed water. Although there was an absence of artifactual reverberation echoes beneath the skin surface the images were initially of average quality and it was not until the invention of the scan converter by Kossoff in the late 1960’s that gave this equipment especial prominence. The scan converter allowed the display of scattered reflections in shades of grey thus giving an appearance of tissue texture and introducing the concept of grey scale scanning. The Octason mark 2 images in the late 1960’s were spectacularly good in demonstrating fetal anatomy but the Octason’s time of brilliance was short-lived following the introduction of the scan converter into contact static scanning machines and the convenience of the latter equipment won the day.
Fig. 7. These images were contemporaneous with figure 6 (c. 1970) but taken on the Picker ultrasound machine which was used in the USA. The image resolution was poor and intracranial structures such as the midline echo were difficult to visualise.

Clinical Studies
Donald and his team with the benefit of priority made some early breakthroughs and in 1963 had described the early diagnosis of hydatid mole (with its snowstorm appearance), assessment and growth of the early gestation sac (by the full bladder technique) and the diagnosis of early pregnancy complications (Donald, 1962).
Placentography: Accurate location of the placenta was the holy grail of antenatal diagnosis in the early 1960’s for placenta praevia was the cause of significant maternal mortality due to severe haemorrhage in late gestation. Many radioisotope methods were used at this time but they were unable to accurately define the lower placental edge. In 1966 Ken Gottesfeld and the Denver group published the first paper on ultrasound placentography (Gottesfeld et al., 1966) although they were unable to visualise the posterior placenta (posterior praevia was implied by a space posterior to the fetal head) and it was not till 1968 that Donald and Usama Abdulla in a larger study (Donald and Abdulla, 1968) and with their superior equipment were able to demonstrate placenta in all locations including posterior praevia.
Fetal biometry: The initial studies in fetal biometry began with using a blind A- scan measurement of the biparietal diameter (BPD) and James Willocks from Donald’s department published an interesting paper on head growth in the third trimester showing different rates of growth between growth restricted and normally growing fetuses. The method was intrinsically inaccurate however and precision was needed for meaningful biometry. This was provided by one of Donald’s registrars, Stuart Campbell who described the B mode technique in 1968 where the midline echo of the fetal head was visualised in 2D and then an A-scan measurement was made between the parietal eminences at the widest point. It was not until on-screen callipers were introduced several years later that A-scan was no longer required. Campbell demonstrated that the midline echo could be seen reliably from 13 weeks gestation and soon showed that second trimester cephalometry was an effective method of dating pregnancy in women with uncertain dates introducing the concept of an ultrasound expected date of confinement (EDD) (Campbell, 1969). Following this he developed the first cephalometry graph from 13 to 40 weeks and used this to identify the IUGR fetus by showing a sharp slowing of biparietal diameter growth in the third trimester (Campbell and Dewhurst, 1971). Cephalometry graphs were subsequently produced by Manfred Hansmann, Alfred Kratochwil, Rudi Sabbagha and many others and serial cephalometry became a standard method of measuring fetal growth for many years.
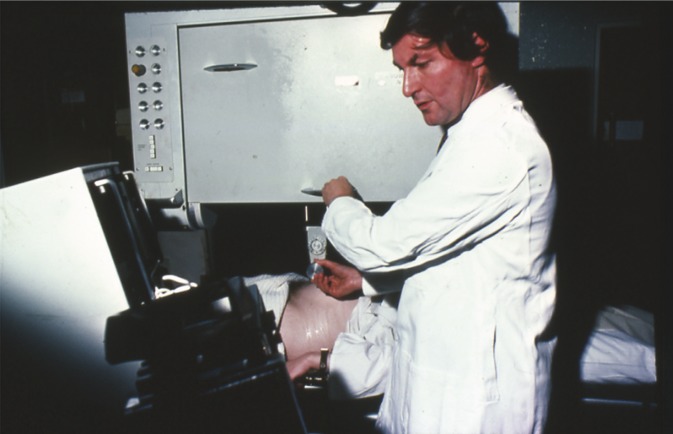
Fig. 5. Campbell using the NE4102, a successor to the Diasonograph with solid state components. The machine remained very large but when the operator stood, the probe could be skimmed across the surface of the abdomen to speed the scanning process.
Fig. 6. Campbell’s improved technique of cephalometry stipulated that the midline echo was always seen on the B-mode scan. Measurements were initially made on the A-scan display before on screen calipers were developed. This image is taken at 20 weeks gestation. In 1970 it was possible to see the midline echo from 13 weeks on the Diasonograph.

The disadvantage of just measuring the fetal head is that brain is the last structure to be affected in growth restriction and Horace Thompson and Ed Makowsky from Denver in 1971 introduced measurement of the thoracic circumference (TC) and the concept of fetal weight prediction using a combination of this measurement and the BPD (Thompson and Makowski, 1971). Manfred Hansmann in Bonn confirmed these results and demonstrated an asymmetry between the BPD measurement and the thoracic circumference in intrauterine growth restricted (IUGR) fetuses. Stuart Campbell who had now moved to Queen Charlotte’s Hospital in London believed there were intrinsic problems with reproducibility with TC measurements as the chest is cone shaped in the fetus and there was no reliable marker to indicate the level of the scan. In 1975 he introduced the abdominal circumference measurement (AC) at the level of the intra abdominal umbilical vein as a more reliable measurement and this has become a standard measurement since (Campbell and Wilkin, 1975). As the AC measurement is at the level of the liver which is the most severely affected organ in IUGR the head circumference to abdomen circumference ratio was introduced as a means of recognising the brain spared IUGR fetus.
The value of routine screening of the obstetric population for accurate dating, early detection of twin gestations and placental location was first demonstrated by Lars Grennert and Per Persson from Malmo (Grennert et al., 1978) who described the evolution of a routine screening programme over a 5 year period; 24% of women had an uncertain EDD and 95% of women were delivered within 12 days of the ultrasound prediction. Also 95% of twins were detected in the second trimester as opposed to 70% before the programme was started.
Early pregnancy: Kratochwil using his transvaginal transducer demonstrated fetal cardiac motion by A-scan from 7 weeks gestation in 1967 but most studies in the 60’s and early 70’s were carried out abdominally by the full bladder technique. For example Bang and Holm from the Copenhagen school reported identifying the fetal heart beat from 10 weeks gestation in 1968 (Bang and Holm, 1968). The seminal work on early pregnancy assessment came from Hugh Robinson from the Glasgow school. In 1973 using an improved Diasonograph he produced the first detailed biometry charts of the fetal crown-rump length from 7 to 16 weeks gestation; his measurements were so meticulous that they are still in use today (Robinson, 1973).
Using the combined A- and B-mode equipment he subsequently produced charts of the fetal heart rate from 7 weeks gestation and showed that the detection rate was 100%. He was the first to point out the prognostic significance of finding a fetal heartbeat at 8 weeks gestation in relation to subsequent fetal demise (Robinson and Shaw-Dunn, 1973). This work had profound influence on the management of patients with threatened abortion.
Fetal abnormalities: Anecdotal reports of the prenatal diagnosis of congenital abnormalities in women with polyhydramnios in the late second or third trimester were made by Bertil Sunden in 1964 (a case of anencephaly) and William Garrett in 1970 who described a case of polycystic kidneys. Ultrasound prenatal diagnosis really began with the Lancet paper by Campbell and his group who in 1972 reported the diagnosis of anencephaly at 17 weeks which resulted in elective termination of pregnancy (Campbell et al., 1972). Subsequent to this he systematically examined the fetal spine in women with raised serum AFP and reported the diagnosis of spina bifida in 1975.
By 1977 he was able to report on 329 high risk pregnancies examined between 16 and 20 weeks in which ultrasound detected 25 of the 28 neural tube defects; 10 of the 13 cases of spina bifida were detected with the false negatives being low sacral lesions (Campbell, 1977). In the USA, John Hobbins and his team at Yale in 1978 described the prenatal diagnosis of several abnormalities including limb reduction defects (Hobbins et al., 1979). The widespread use of ultrasound in prenatal diagnosis came with the invention of the real time scanning machines.
Fig. 8. The Vidoson was the first real time scanner and was popular in Germany. The frame rate was slow, the resolution poor but Manfred Hansmann (a) pioneered ultrasound guided intrauterine therapy (b) with this equipment (c).

Fig. 9. Hugh Robinson (a) pioneered the Fetal Crown-Rump Length (CRL) measurement (b) in 1973. His CRL chart (c) is still used today.

Fig. 10. Second trimester Prenatal Diagnosis by ultrasound began in 1972 with the diagnosis of Anencephaly followed by Spina Bifida in 1975. The picture above (a) shows a cross-section of an intact spine (small circle) and (b) an image of a bifid spine.
The Real Time Revolution
Equipment development
Mechanical sector real time scanners were introduced by several companies such as Aloka and Kretztechnic in the early to mid 70’s but these were quickly superseded by the multi-element linear array and phased array scanners in the mid to late 1970’s. Due to the huge advances in integrated circuit technology occurring at this time, the machines were small and moveable and as they were less expensive, a department would have several instead of the single large static scanner. Movements of the fetus could now be followed and the probe angle instantly adjusted to identify the plane of interest. Sonographers and research fellows could be quickly trained and as complete fetal biometry could be achieved in a matter of minutes, screening the whole obstetric population was now feasible. The first commercial linear array real time scanner was the ADR a small company founded by Martin Wilcox in Tempe Arizona. Initially it had only 64 lines so the resolution was poor but the second version the ADR 2130 in 1975 had over 500 lines and phased focusing and could compete with static scanners in terms of resolution. Most large ultrasound companies produced real time equipment over the next few years leapfrogging each other in degrees of sophistication but the development of the Acuson 128 by Sam Maslak in 1983 with its advanced beam forming software (called “computed sonography”) set new standards in both spatial and contrast resolution. In 1985 Kretztechnic produced the first practical endovaginal mechanical sector transducer which was designed to improve the technique of oocyte collection in IVF. These transducers provided excellent images but probe vibrations were a disadvantage and by the end of the 1990’s most manufacturers had developed small multi-element probes which provided excellent resolution.
By 1985, Aloka had incorporated colour Doppler imaging (originally called colour flow mapping) into their real time equipment and this was quickly followed by other major manufacturers. By 1990 colour was available on the transvaginal probe for gynaecological investigation. By the end of the 1990’s harmonic imaging was introduced which even further improved image resolution. Although early studies on 3D imaging were begun in Japan by Kazunon Baba in 1984, it was not until the production of the third generation 530D Voluson in the mid 1990’s that the world was convinced that 3D/4D ultrasound had a major role to play in both obstetrical and gynaecological imaging. Much of the credit for promoting this new technology must go to Bernard Benoit a French doctor working in Nice who published stunning 3D images of the fetus especially in the first trimester. It could thus be said that (apart from a few refinements) the modern real time scanning machine with high resolution abdominal and endovaginal transducers, harmonic imaging, colour and power Doppler facilities with a 3D/4D option was on the market by the year 2000.
Fig. 11. A typical modern scanning machine complete with high-resolution imaging, colour and power Doppler and a 3D/4D option (GE Voluson Expert).

Clinical Studies in Obstetrics
The development of real time scanning was a great democratising influence in obstetric scanning which was no longer confined to an elite group of experts in a few major centres. Real time scanners being inexpensive were now widely available and many experienced practitioners of static scanning were surprised (and not a little discomfited) at how quickly their junior doctors, midwives and sonographers became experts in scanning almost overnight.
Fetal biometry: The ease with which the probe could be manipulated meant that many fetal structures were measured and a great number of charts of different planes and organs were developed. For example charts of inter-orbital diameter (Mayden et al., 1982), long bones, foot length, ear length, the sizes of virtually every fetal organ and multiple ratios between parameters like femur to foot were produced within a space of a few years. However the standard measurements CRL, BPD, head circumference and abdomen circumference which were developed during the static era remained the standard fetal biometric measurements for assessing growth with only the addition of the femur length (which was now easier to measure) incorporated into equations for fetal weight and growth predictions (Hadlock et al., 1985).
Fetal activity: Studies of fetal behaviour were inspired by leaders in development biology such as Geoffrey Dawes in Oxford and Heinz Prechtl in Nijmegan. The ability to follow fetal movements by ultrasound inspired much interest as to whether quantification of these movements and especially fetal breathing movements might be helpful in assessing fetal wellbeing. In the late 1970’s detailed studies using event markers on a chart recorder were made by groups led by Karel Marsal in Malmo (Marsal et al., 1976), John Patrick in London, Ontario and Alistair Roberts in London. The time, incidence and number of movement episodes or fetal breaths were quantitatively assessed and behavioural states identified. Both fetal breathing movements and fetal activity are episodic and are rarely concordant so the concept of measuring total fetal activity over a 30 minute period was employed. Although there was an association between reduced total activity and IUGR, the test had a low predictive value for a positive test due to the large physiological variation in the incidence of both breathing and motor activity (Marsal, 1978). For this reason in Europe the measurement of fetal activity fell out of favour as a means of assessing fetal well being. In USA however Frank Manning and Larry Platt in 1980 incorporated both of these measures into a 30 minute fetal biophysical profile test (Manning et al., 1980) which also included an assessment of amniotic fluid, fetal tone and a non stress test (CTG) of the fetal heart. This test with minor modifications became the mainstay of fetal wellbeing assessment in the United States for over 20 years. In Europe however researchers turned increasingly to Doppler Ultrasound to solve the problem as to how to effectively assess fetal wellbeing and optimise the timing of delivery when there is fetal compromise.
Doppler Assessment: The demonstration of the umbilical artery waveform using blind continuous wave (CW) Doppler was reported as early as the mid 1960’s from Osaka, Japan and in 1977 by D.E. Fitzgerald and John Drumm from Dublin using 2D static scans to identify where the probe should be placed but neither of these two groups followed up their observations. Two groups initiated pulsed Doppler studies of the fetus. In Australia, Robert Gill working with the Kossoff group measured flow velocity in the umbilical vein (Gill et al., 1981). However the long path length of the Octason prevented the measurement of high velocity arterial flow and this system was impractical for clinical Doppler studies. Sturla Eik-Nes working in Karel Marsal’s department in Malmo described the first duplex linear array system (Eik-Nes et al., 1980) where an offset pulsed Doppler probe was attached at a fixed angle of 52 degrees. He measured flow velocities from the fetal aorta and found that they were reduced in IUGR fetuses. Equipment similar to the Malmo duplex Doppler system was used by workers in several academic units in the early to mid 1980’s across Europe to define the fetal circulatory response to hypoxia. It was found that absolute velocity measurements were inferior to waveform analysis especially the pulsatility index in the assessment changes in the fetal circulation to hypoxia. Yuri Wladimiroff in Rotterdam was the first to draw attention to the compensatory increase in the cerebral circulation or “centralisation of the fetal circulation” associated with IUGR fetuses (Wladimiroff et al., 1986). Wladimiroff also correlated circulatory changes with behavioural states (Wladimiroff 1994) while Campbell, David Griffin and Kypros Nicolaides at King’s College Hospital in London correlated these changes with blood gases obtained by cordocentesis (Bilardo et al., 1990). In Australia Brian Trudinger and Warwick Giles rediscovered the importance of the umbilical artery waveform and established the significance of absent and reversed end diastolic flow (Trudinger et al., 1986). In 1983 Campbell and his group described the uterine artery waveform and the appearance of notching which together with a high resistance index was associated with pre-eclampsia (Campbell et al., 1982). His group subsequently used this finding to screen the pregnant population at 24 weeks gestation to predict the subsequent development of preeclampsia.and IUGR and showed a high sensitivity for the severe forms of these conditions (Harrington et al., 1996).
The advent of colour Doppler as an integral part of the ultrasound machine made visualisation of fetal vessels much easier and studies of virtually every fetal artery (such as the renal, splanchnic, cerebral) was investigated and charts made of the gestational changes of PI under different clinical circumstances. In the early 90’s the principal vessels studied to evaluate fetal wellbeing were the umbilical artery and middle cerebral artery. Although these were useful they were no better than the antenatal CTG in determining the optimal time to deliver the compromised fetus. This led to several groups investigating the venous side of the fetal circulation. Initial studies concentrated on the inferior vena cava but in 1991 in a landmark Lancet paper, Torvid Kiserud from the Eik-Nes group in Trontheim, Norway described the measurement of the pulsatility of the ductus venosus (Kiserud et al., 1991) which has become established as a key measure of cardiac function and indicator fetal asphyxia. With modern equipment, Doppler evaluation of the fetal circulation especially umbilical and middle cerebral arteries and ductus venosus is now established as a fundamental requirement in the assessment of fetal wellbeing and the timing of delivery of the compromised fetus. A further important use of Doppler was its use as non-invasive method of diagnosing anaemia in Rh immunised fetuses which was popularised by Giancarlo Mari and the group at Yale University following a paper in the New England journal of Medicine in 2000 (Mari et al., 2000).
The prediction of pre-eclampsia and IUGR by uterine artery Doppler was further explored by Nicolaides in a very large multicentre studies. They showed in 2001 that the uterine artery PI performed at 23 weeks predicted 85% of women who would develop severe pre-eclampsia for only a 5% screen positive rate (Papageorghiou et al., 2001). One of the problems is that prevention by agents such as low dose aspirin does not seem to be effective. Nicolaides and others are now exploring the possibility of screening for pre-eclampsia in the first trimester (when preventive therapy appears to be effective) using uterine artery Doppler and biochemical markers such as PlGF and PAPP-A (Akolekar et al., 2013).
Preterm birth: Preterm labour is the greatest cause of neonatal death and handicap and the care of the preterm baby is hugely expensive. Although the causes of spontaneous pre-term labour are many and not fully understood, a common final pathway is shortening and effacement of the cervix. Several studies in the early 1980’s using transabdominal sonography drew attention to the association between a short cervix and funnelling with cervical incompetence. Frank Andersen from Ann Arbor Michigan was the first to draw attention to the superiority of transvaginal scanning (Andersen et al., 1990) and provided a risk for preterm delivery based on a cervical length. Subsequent studies by Jay Iams from Columbus, Ohio (Iams et al., 1996), Kypros Nicolaides from King’s College, London have confirmed that screening around 23-24 weeks gestation will predict a large percentage of women who will go into preterm labour. For example Nicolaides screened over 32,000 women at 23 weeks and was able to identify 50% of women delivering before 33 weeks gestation by using a cut-off cervical length of 15mm (Heath et al., 1998). Unfortunately cervical cerclage does not appear to be effective in extending gestation in these women but two major studies from the Nicolaides group in London and the group of Robert Romero at Wayne State University, Detroit have demonstrated that following universal screening between 19 and 24 weeks, a significant prolongation of gestation in women with a sonographic shortened cervix can be achieved with daily vaginal progesterone treatment (Romero et al., 2011).
Fetal abnormality screening: Following the introduction of real time scanning there was a large number of review papers documenting the experience of tertiary centres in diagnosing a wide range of abnormalities of virtually every organ of the fetal body. By the mid 1980’s most hospitals had introduced screening for fetal abnormalities as part of the routine 20 week scan. Many of the studies published at this time were invalid because of low ascertainment of anomalies in the newborn (the prevalence should be between 2 and 3 per cent). A controversial American multicentre study (RADIUS) published in 1993 (Ewigman et al., 1993) demonstrated a low detection rate of 17 per cent for the early detection of fetal abnormalities but this was not the experience in European centres. Multicentre studies as a rule had lower detection rates than those from single centres. For example in Salvator Levi’s large Belgian multicentre study conducted between 1990 and 1992 only 40% of fetuses with anomalies were detected before 23 weeks (Levi et al., 1991) while Carrera in a single centre in Barcelona reported an 85% detection rate in a similar time period (Carrera et al., 1995).
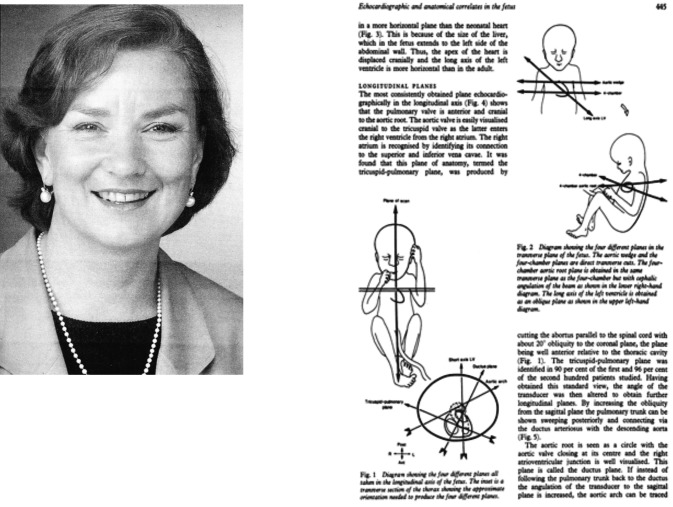
Fetal Cardiac defects: For the first time the diagnosis of cardiac abnormalities was now possible. In 1980, two breakthrough papers on real time fetal echocardiography were published by Lindsey Allan from King’s College Hospital, London and Charles Kleinman from Yale. In her classic study Allan (Allan et al., 1980) was the first to describe the systematic examination of the heart to demonstrate the 4 chamber view and outflow tracts and published images of the 8 classic ultrasound views together with anatomic correlates and was one of the first to promote routine screening for fetal cardiac abnormalities.
Fig. 12. Page from Lindsay Allan’s classic 1980 paper in the British Heart Journal showing 8 classic views of the fetal heart which laid the foundations for fetal echocardiography.
In 1997 S-J Yoo (Yoo et al., 1997) described an additional classic view, namely the 3 vessel view of the outflow tracts. The advent of colour Doppler facilitated studies of intracardiac flow with groups led by Greg DeVore (DeVore et al., 1987), Rabih Chaoui and Ulrich Gembruch making significant contributions.
Fetal Chromosome Abnormalities: before the real time revolution amniocentesis was offered to the “high risk” group of women over the age of 35 years but this policy failed to diagnose the 70 per cent of babies with Down syndrome who were born to younger women. In 1985 Beryl Benacerraf and her group in Boston first described that an increased nuchal skin fold measurement in the second trimester was associated with Down syndrome (Benacerraf et al., 1985) and subsequently described the other classic second trimester markers of shortened femur and pyelectasia. For the first time younger women could be offered amniocentesis on the basis of a combination of markers. The decisive breakthrough came in 1992 when Kypros Nicolaides from King’s in London described the first trimester measurement of nuchal translucency in the diagnosis of Down’s syndrome (Nicolaides et al., 1992). Nicolaides and his group subsequently demonstrated the association of increased nuchal translucency, absence of the nasal bone, tricuspid regurgitation and increased ductus venosus PI with Down’s syndrome. They have combined these ultrasound markers with the measurement of serum PAPP-A and free beta HCG (called combined biomarkers) to provide a likelihood ratio for the presence of Down’s syndrome. With the combined biomarker programme 90 per cent of Down’s syndrome fetuses are detected for a 5 per cent screen positive rate. (Nicolaides, 2011) With CVS being offered as the diagnostic test to women at increased risk, this screening programme has been adopted throughout the world. However this is likely to change with the advent of cell-free DNA testing (Lo et al., 1997). Recent studies have shown that cfDNA screening in a maternal blood sample at 10 weeks gestation (called Non-Invasive Prenatal Testing or NIPT) will detect more than 99% of cases of trisomy 21 for a false positive rate of about 0.1% (Chiu et al., 2011) which is a significant improvement of the combined biomarkers of ultrasound and biochemistry. Furthermore in the future cfDNA is likely to be able to screen for a wide range of chromosome and genetic disorders. At the moment “contingency testing” incorporating biomarkers and cfDNA is recommended to reduce cost but there is little doubt that NIPT will become the method of choice in the not too distant future.
Invasive procedures: The importance of identifying the position of the needle during amniocentesis was first highlighted by Jens Bang in Copenhagen in 1973 (Bang and Northeved, 1972) during the static scan era but few practitioners used his transducer with a central hole and scans at this time were usually used to identify a placenta-free accessible pool of fluid prior to the procedure. The advent of real time scanning allowed the performance of invasive procedures under continuous vision thus reducing bloody taps and avoiding placental, cord or fetal injury. In 1974 fetoscopy was introduced by John Hobbins and Maurice Mahoney at Yale for the prenatal diagnosis of haemoglobinopathies (Hobbins and Mahoney, 1974) from fetal red blood cells obtained from the chorionic plate. Many believed that this technique would supersede ultrasound guided methods especially when Rodeck and Campbell at King’s in London described the obtaining of pure fetal blood from the umbilical vein by this method and Niels Hahnemann and Jan Mohr with a similar instrument obtained chorionic tissue trancervically for genetic diagnosis. However in 1983 Fernand Daffos and co-workers from Paris introduced pure fetal blood sampling from the cord insertion by direct ultrasound guided needling using two operators (Daffos et al., 1983) and subsequently Nicolaides from King’s perfected the single operator two hands method and called it cordocentesis. He and his team used this technique to assess the severity of fetal anaemia in rhesus disease thus supplanting the old method based on bilirubin measurements in the amniotic fluid (Nicolaides et al., 1988). Nicolaides and others such as Giorgio Pardi in Milan also used this technique to assess aspects of fetal acid base status and biochemistry in the IUGR fetus (Pardi et al., 1987). Another nail in the coffin for fetoscopy came with the introduction of transabdominal first trimester fine needle aspiration of chorionic villi(CVS) by Steen Smidt-Jensen and Hahnemann in 1984 (Smidt-Jensen et al., 1984), a technique which has been adopted universally for the prenatal diagnosis of fetal genetic and karyotype defects.
Fig. 13. Fetoscopic intravascular transfusion was introduced by Rodeck (a) in 1981 but 5 years later this was superseded by the cordocentesis method (b) introduced by Nicolaides.
Fetal Therapy: The treatment of severe rhesus disease in the fetus by intraperitoneal transfusion under x-ray guidance was pioneered by Lilley in 1959. Hansmann in 1968 used the Vidoson’s “real time” capability to simplify the technique into an ultrasound guided procedure (Hansmann and Lang, 1971). Access to the fetal circulation however prompted the development of therapeutic procedures firstly by fetoscopy (Rodeck et al., 1981) and then by cordocentesis such as fetal blood transfusion in severe rhesus disease (Nicolaides et al., 1986) and platelet transfusion for alloimmune thrombocytopenia. Ultrasound controlled needling procedures were also used to insert shunts to decompress obstructions in the urinary tract and cerebral ventricles or to drain fluid from pleural effusions but none of these procedures were found to significantly improve outcome and in the case of ventriculomegaly, the condition was frequently made worse. Two prenatal surgical procedures that have been shown to be useful involve the combined use of ultrasound and fetoscopy. In 1995 Yves Ville and Nicolaides from King’s College in London demonstrated the effectiveness of laser ablation to the communicating placental vessels in the treatment of twin-to-twin transfusion syndrome (Ville et al., 1992) and this technique has been shown to be superior to therapeutic amniocentesis in terms of fetal survival. In 1998 Harrison’s group in San Francisco described occlusion of the fetal trachea by ultrasound guided fetoscopic surgery for the treatment of severe diaphragmatic hernia and subsequently Jan Deprest in Leuven, Eduard Gratacos in Barcelona and Kypros Nicolaides in London described temporary endoscopic balloon occlusion for this condition resulting in a significant improvement in outcome.
Clinical Studies in Gynaecology
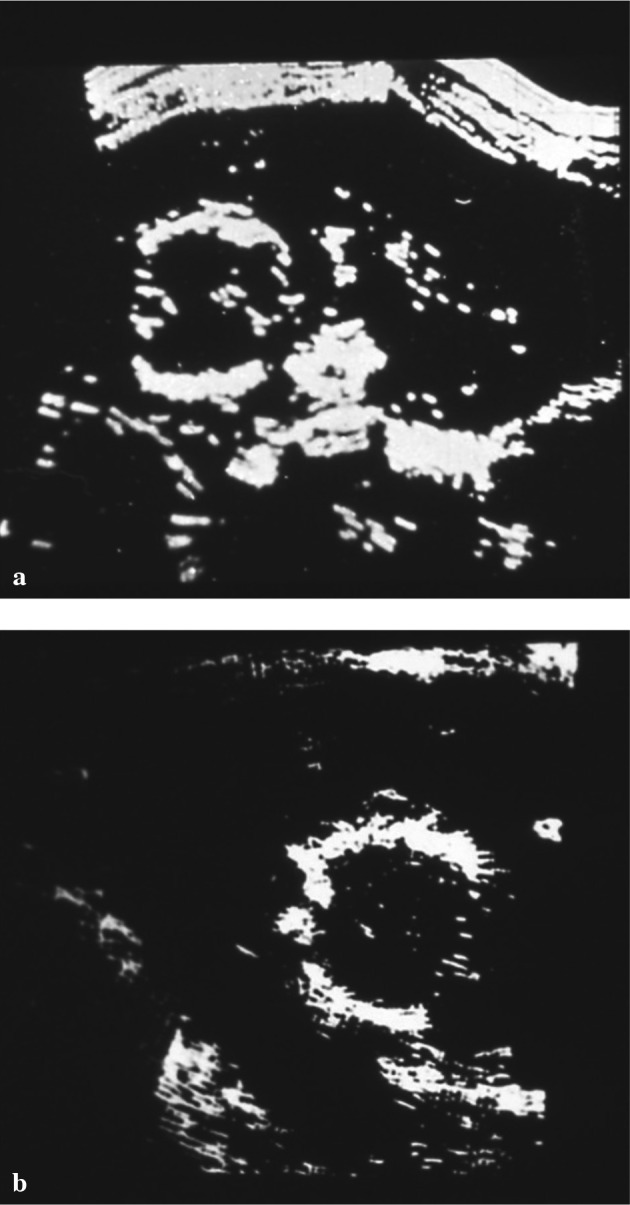
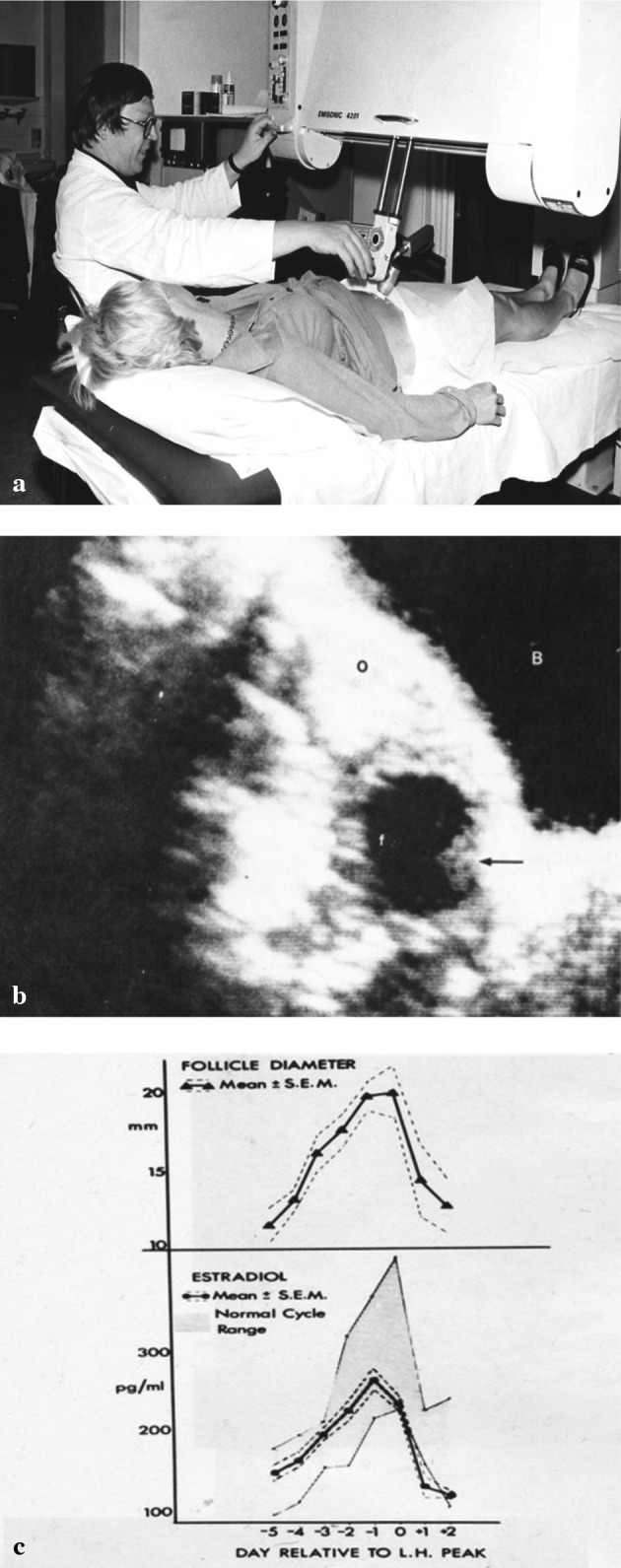
Advances in gynaecological scanning were rapid following the introduction of the real time transvaginal probe in the mid 1980’s. Before this visualisation of the pelvic organs required the patient to have a distended bladder which not only frequently caused her distress but often pushed the structure of interest beyond the focal distance of the transducer. Despite this important studies were made with the static scanners. Following on Donald’s original observations of the characteristics of malignant ovarian tumours Patricia Morley and Ellis Barnett from Glasgow described in 1970 the ultrasound differential diagnosis of ovarian masses. In 1981 Nick Kadar and Roberto Romero from Yale (Kadar et al., 1981) described the discriminatory zone (i.e. the minimal hCG level that should be associated with an intrauterine sac) for the diagnosis of ectopic gestation. In 1979 Joachim Hackeloer a German doctor working on sabbatical in Glasgow published his classic paper on the tracking of ovarian follicular growth (Hackeloer and Robinson, 1978) and showed a correlation between follicular size and serum oestradiol. In 1985 Judith Adams working in Howard Jacobs Unit in London determined the classic ultrasound parameters for the diagnosis of polycystic ovaries and subsequently showed that PCO affected 23% of the female population during their reproductive years. However the advent of transvaginal sonography changed the diagnostic impact of ultrasound in gynaecology.
Fig. 14. Joachim Hackeloer (a) introduced ovarian follicular monitoring and correlated follicle size (b) with oestradiol levels (c). This revolutionised fertility management and paved the way for IVF.
Early pregnancy disorders: The importance of understanding normal embryogenesis was emphasised by Ilan Timor-Tritch from Columbia University, New York who pioneered the concept of transvaginal “sono-embryology” in the late 1980’s (Timor-Tritsch et al., 1992) and subsequently he and other workers described the diagnosis of early embryonic abnormalities. The direct diagnosis of ectopic pregnancy was also revolutionised by transvaginal probe. David Nyberg and Roy Filly from San Francisco (Nyberg et al., 1987) and Bruno Cacciatore from Finland in the late 1980’s described the many sonographic manifestations of this condition and reported diagnostic success rates of over 90 per cent. In the 1990’s virtually every hospital had an emergency diagnostic unit where women with pelvic pain and bleeding were assessed by an expert transvaginal scan and a sensitive beta hCG blood test.
Pelvic masses: TVS allowed greater discrimination between benign and malignant masses and there were several attempts to create a scoring system of morphological parameters to better define the differential diagnosis. Sassone and Timor Tritch in New York Hospital first described such a scoring system. The advent of colour Doppler allowed the detection of angiogenesis in tumours and in 1989 Tom Bourne and Campbell at King’s demonstrated high vascularity with increased peak velocity flow was associated with malignant masses. Anil Tailor from the same group developed a multiple regression model incorporating morphological and blood flow criteria. More recently a European multicentre trial (IOTA) led by Dirk Timmerman from Leuven and Lil Valentin from Lund has developed sophisticated models to discriminate benign from malignant masses (Timmerman et al., 2005). While these models have provided useful information they have not been shown to be superior to the subjective evaluation by an experienced observer in differentiating benign from malignant tumours.
Screening for malignancy: Ovarian cancer has the highest mortality rate of all gynaecological cancers because it is symptom free in its early stages. Campbell and his team at King’s in London in 1989 (Campbell et al., 1989) and John Van Nagell in Lexington, Kentucky in 1991 using transvaginal ultrasound both reported a high detection rate for ovarian cancer most of which were at stage1 but due to the high number of benign cysts the operation rate per cancer detected was unacceptably high. In 1999 Ian Jacobs at University College London introduced the concept of multimodal ovarian cancer screening in which serial CA125 measurements were used as the screening test backed up by TVS in screen positive cases to reduce the false positive rate. He has since set up a large UK multicentre randomised screening programme (UKCTOCS) which is at present ongoing but initial published data (Menon et al., 2009) indicates a high detection rate for epithelial cancer with only 2.7 operations per cancer detected.
Reproductive medicine: The advent of TVS transformed reproductive medicine especially the monitoring and procedures associated with IVF. Traditionally following on the pioneer work of Patrick Steptoe oocyte collection was made by laparoscopy but in 1990 Susan Lenz from Jens Bang’s unit in Copenhagen described the ultrasound guided transvesical aspiration of oocytes (Lenz, 1981). At King’s John Parsons used the Copenhagen technique to make IVF a totally out patient procedure. In 1995 Wilfred Feichtinger and Pieter Kemeter from Vienna described transvaginal oocyte aspiration with a needle guide attached to the transvaginal probe (Feichtinger and Kemeter, 1986) and this has now become the standard technique. Transvaginal ultrasound has proved to be reliable in assessing ovarian reserve through measurement of the antral follicle count which was first described by Reuss and colleagues in 1996 in Columbia University, New York (Reuss et al., 1996). Doppler has also been used to assess ovarian reserve by measurement of stromal flow and follicular competence and maturity by measurement of peri-follicular blood flow (Nargund et al., 1996).
Clinical Studies in 3D/4D Ultrasound
The advent of 3D ultrasound imaging has led to a flurry of publications extolling the virtues of this new modality yet substantial evidence of definitive benefit is hard to obtain. Most fetal anomalies can be detected by high resolution 2D ultrasound and most practitioners report that the addition of 3D is rarely required. Almost all 3D studies have been carried out with the Voluson originally introduced by Kretztechnic and now made by General Electric. Early workers in the field and strong advocates of 3D ultrasound are Dolores Pretorius from Los Angeles, Kazunori Baba from Japan and Eberhard Merz from Germany. 3D ultrasound is superior in demonstrating superficial fetal defects such as facial clefts and studies from several groups have shown that the technique has a high sensitivity for diagnosing defects of the secondary palate which are rarely detected by 2D ultrasound (Campbell, 2007). In fetal echocardiography the capture of a volume of the beating fetal heart (called spatio-temporal image correlation or STIC) allows the study of tomographic slices of cardiac anatomy and movement in slow motion. Proponents of this technology are Greg DeVore in the USA and Rabih Chaoui in Germany. In gynaecology Davor Jurkovic from King’s in London demonstrated that 3D imaging of the uterus was superior to 2D imaging in recognising and classifying congenital abnormalities of the uterus (Jurkovic et al., 1995). Volumetric quantification of vascularity and flow (3D flow indices) offers an alternative to Doppler velocimetry in the assessment of flow within an organ. Nick Raine Fenning from Nottingham has shown interesting data on endometrial flow and implantation of the embryo but as yet the technique has not been shown to be clinically useful. However this group have shown that 3D software that generates automated follicle volume measurement (SonoAVC) permits faster measurement of antral follicle counts and tracking of follicular growth during and an IVF cycle (Raine-Fenning et al., 2009).
Real Time 3D ultrasound imaging (i.e. 4D) is most useful in showing fetal movements and there is evidence that this has real benefit in improving maternal-fetal bonding. 3D/4D ultrasound is very much “work in progress” and further technical developments such as the matrix probe will undoubtedly pave the way for further advances in obstetrical and gynaecological imaging in the future.
Fig. 15. It is believed that a 3D moving sequence (i.e. 4D ultrasound) demonstrating the “humanity” of the fetus can encourage maternal-fetal bonding.
Postscript
When a former president of the Royal College of Obstetricians and Gynaecologists was asked what were the three most important advances in his specialty in the 20th century he replied ultrasound, ultrasound and ultrasound. The brief overview given above can not do full justice to the huge range of beneficial effects of ultrasound examination in improving the health of women and babies in the second half of the 20th Century. Ultrasound scanning features in almost everything we do in obstetrics and gynaecology. The great advances described in this chapter have come about because of a symbiotic relationship between brilliant engineers and the doctors who exploited each new development for the benefit of their patients and then fed back to the engineers what was next required. Ultrasound is unique in that it is safe even for the smallest embryo and that the examination is convenient and causes no discomfort. Indeed for most patients the ultrasound examination is both enjoyable and instructive. The greatest problem with ultrasound is that the results are still very much dependent on the skill of the operator. Space does not permit me to praise the great teachers of ultrasound or the organisations such as the International Society of Ultrasound in Obstetrics and Gynaecology (ISUOG) and the Fetal Medicine Foundation (FMF) which are dedicated to improve the knowledge and performance of the clinicians, sonographers and nurses who use ultrasound equipment in everyday practice. Without these teachers and trainers the advances described in this chapter could never have been introduced into clinical practice.
References
- Akolekar R, Syngelaki A, Poon L, et al. Competing Risks Model in Early Screening for Preeclampsia by Biophysical and Biochemical Markers. Fetal Diagn Ther. 2013;33:8–15. doi: 10.1159/000341264. [DOI] [PubMed] [Google Scholar]
- Allan LD, Tynan MJ, Campbell S, et al. Echocardiographic and anatomical correlates in the fetus. Br Heart J. 1980;44:444–51. doi: 10.1136/hrt.44.4.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen HF, Nugent CE, Wanty SD, et al. Prediction of risk for preterm delivery by ultrasonography measurement of cervical length. Am J Obstet Gynec. 1990;163:859–67. doi: 10.1016/0002-9378(90)91084-p. [DOI] [PubMed] [Google Scholar]
- Bang J, Holm HH. Ultrasonics in the demonstration of fetal heart movements. Am J Obstet Gynecol. 1968;102:956–60. doi: 10.1016/0002-9378(68)90454-7. [DOI] [PubMed] [Google Scholar]
- Bang J, Northeved A. A new method for transabdominal amniocentesis. Am J Obstet Gynecol. 1972;114:599–601. doi: 10.1016/0002-9378(72)90835-6. [DOI] [PubMed] [Google Scholar]
- Benacerraf BR, Barss VA, Laboda LA. A sonographic sign for the detection in the second trimester of the fetus with Down’s syndrome. Am J Obstet Gynecol. 1985;151:1078–9. doi: 10.1016/0002-9378(85)90385-0. [DOI] [PubMed] [Google Scholar]
- Bilardo CM, Nicolaides KH, Campbell S. Doppler measurements of fetal and uteroplacental circulations: relationship with umbilical venous blood gases measured at cordocentesis. Am J Obstet Gynecol. 1990;162:115–20. doi: 10.1016/0002-9378(90)90833-s. [DOI] [PubMed] [Google Scholar]
- Campbell S. Prediction of fetal maturity by ultrasonic measurement of the biparietal diameter. J Obstet Gynaec Br Commonw. 1969;76:603–9. doi: 10.1111/j.1471-0528.1969.tb06146.x. [DOI] [PubMed] [Google Scholar]
- Campbell S, Dewhurst CJ. Diagnosis of the small-for-dates fetus by serial ultrasonic cephalometry. Lancet. 1971;2(7732):1002–6. doi: 10.1016/s0140-6736(71)90324-2. [DOI] [PubMed] [Google Scholar]
- Campbell S, Johnstone FD, Holt EM, et al. Anencephaly: early ultrasonic diagnosis and active management. Lancet. 1972;2(7789):1226–7. doi: 10.1016/s0140-6736(72)92273-8. [DOI] [PubMed] [Google Scholar]
- Campbell S, Wilkin D. Ultrasonic measurement of the fetal abdomen circumference in the estimation of fetal weight. Br J Obstet Gynaecol. 1975;82:687–9. doi: 10.1111/j.1471-0528.1975.tb00708.x. [DOI] [PubMed] [Google Scholar]
- Campbell S. Early prenatal diagnosis of neural tube defects by ultrasound. Clin Obstet Gynecol. 1977;20:351–9. doi: 10.1097/00003081-197706000-00015. [DOI] [PubMed] [Google Scholar]
- Campbell S, Diaz-Recasens J, Griffin DR, et al. New Doppler technique for assessing uteroplacental blood flow. Lancet. 1983;26:675–7.. doi: 10.1016/s0140-6736(83)91970-0. [DOI] [PubMed] [Google Scholar]
- Campbell S, Bhan V, Royston P, et al. Transabdominal ultrasound screening for early ovarian cancer. Brit Med J. 1989;299:1363–7. doi: 10.1136/bmj.299.6712.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S. Prenatal ultrasound examination of the secondary palate. Ultrasound Obstet Gynecol. 2007;29:124–7. doi: 10.1002/uog.3954. [DOI] [PubMed] [Google Scholar]
- Carrera JM, Torrents M, Mortera C, et al. Routine prenatal ultrasound screening for fetal abnormalities: 22 years’ experience. Ultrasound Obstet Gynecol. 1995;5:174–9. doi: 10.1046/j.1469-0705.1995.05030174.x. [DOI] [PubMed] [Google Scholar]
- Chiu RW, Akolekar R, Zheng YW, et al. Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validity study. Brit Med J. 2011;342:c7401. doi: 10.1136/bmj.c7401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daffos F, Pavlovsky M, Forestier F. Fetal blood sampling via the umbilical cord using a needle guided by ultrasound. Report of 66 cases. Prenat Diagn. 1983;3:271–7. doi: 10.1002/pd.1970030402. [DOI] [PubMed] [Google Scholar]
- DeVore GR, Horenstein J, Siassi B, et al. Fetal echocardiography. Doppler color flow mapping: a new technique for the diagnosis of congenital heart disease. Am J Obstet Gynecol. 1987;156:1054–64. doi: 10.1016/0002-9378(87)90110-4. [DOI] [PubMed] [Google Scholar]
- Donald I, MacVicar J, Brown TG. Investigation of abdominal masses by pulsed ultrasound. Lancet. 1958;1:1188–95. doi: 10.1016/s0140-6736(58)91905-6. [DOI] [PubMed] [Google Scholar]
- Donald I. Clinical applications of ultrasonic techniques in obstetrical and gynaecological diagnosis. Br J Obstet Gynaecol. 1962;69:1036. [PubMed] [Google Scholar]
- Donald I, Abdulla U. Placentography by sonar. J Obstet Gynaecol Br Commonw. 1968;75:993–1006. doi: 10.1111/j.1471-0528.1968.tb02871.x. [DOI] [PubMed] [Google Scholar]
- Eik-Nes SH, Marsal K, Brubakk AO, et al. Ultrasonic measurement of human fetal blood flow. J Biomed Eng. 1982;4:28–36. doi: 10.1016/0141-5425(82)90023-1. [DOI] [PubMed] [Google Scholar]
- Ewigman BG, Crane JP, Frigoletto FD, et al. Effect of prenatal ultrasound screening on perinatal outcome. RADIUS Study Group. N Engl J Med. 1993;329:821–7. doi: 10.1056/NEJM199309163291201. [DOI] [PubMed] [Google Scholar]
- Feichtinger W, Kemeter P. Transvaginal sector scan sonography for needle guided transvaginal follicle aspiration and other applications in gynecologic routine and research. Fertil Steril. 1986;45:722–5. doi: 10.1016/s0015-0282(16)49349-0. [DOI] [PubMed] [Google Scholar]
- Gill RW, Trudinger BJ, Garrett WJ, et al. Fetal umbilical venous flow measured in utero by pulsed Doppler and B-mode ultrasound. I. Normal pregnancies. Am J Obstet Gynecol. 1981;139:720–5. doi: 10.1016/0002-9378(81)90495-6. [DOI] [PubMed] [Google Scholar]
- Gottesfeld KR, Thompson KE, Holmes JH, et al. Ultrasonic placentography-a new method for placental localisation. Am J Obstet Gynec. 1966;96:538–47. doi: 10.1016/s0002-9378(16)34691-9. [DOI] [PubMed] [Google Scholar]
- Grennert L, Persson P, Gennser G. Benefits of ultrasound screening of a pregnant population. Acta Obstet Gynecol Scand Suppl. 1978;78:5–14. doi: 10.3109/00016347809162696. [DOI] [PubMed] [Google Scholar]
- Hackeloer BJ, Robinson HP. Ultrasound examination of the growing ovarian follicle and of the corpus luteum during the normal physiologie menstrual cycle. Geburtshilfe Frauenheilkd. 1978;38:163–8. [PubMed] [Google Scholar]
- Hadlock FP, Harrist RB, Sharman RS, et al. Estimation of fetal weight with the use of head, body and femur measurements-a prospective study. Am J Obstet Gynecol. 1985;151:333–7. doi: 10.1016/0002-9378(85)90298-4. [DOI] [PubMed] [Google Scholar]
- Hansmann M, Lang N. Intrauterine transfusion controlled by ultrasound. Klin Wochenschr. 1972;50:930–2. doi: 10.1007/BF01487926. [DOI] [PubMed] [Google Scholar]
- Harrington K, Cooper D, Lees C, et al. Doppler ultrasound of the uterine arteries: the importance of bilateral notching in the prediction of pre-eclampsia, placental abruption or delivery of a small-for-gestational-age baby. Ultrasound Obstet Gynecol. 1996;7:182–8. doi: 10.1046/j.1469-0705.1996.07030182.x. [DOI] [PubMed] [Google Scholar]
- Heath VC, Southall TR, Souka AP, et al. Cervical length at 23 weeks of gestation: prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12:312–7. doi: 10.1046/j.1469-0705.1998.12050312.x. [DOI] [PubMed] [Google Scholar]
- Hobbins J, Mahoney MJ. In utero diagnosis of hemoglobinopathies; technic for obtaining fetal blood. New England J Med. 1974;290:1065–7. doi: 10.1056/NEJM197405092901908. [DOI] [PubMed] [Google Scholar]
- Hobbins JC, Grannum PA, Berkowitz RL, et al. Ultrasound in the diagnosis of congenital anomalies. Am J Obstet Gynecol. 1979;134:331–45. doi: 10.1016/s0002-9378(16)33043-5. [DOI] [PubMed] [Google Scholar]
- Howry DH. The ultrasonic visualization of soft tissue structures and disease processes. J Lab Clin Med. 1952;40:812–3. [PubMed] [Google Scholar]
- Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–72. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- Jurkovic D, Geipel A, Gruboeck K, et al. Three-dimensional ultrasound for the assessment of uterine anatomy and detection of congenital anomalies: a comparison with hysterosalpingography and two-dimensional sonography. Ultrasound Obstet Gynecol. 1995;5:233–8. doi: 10.1046/j.1469-0705.1995.05040233.x. [DOI] [PubMed] [Google Scholar]
- Kadar N, DeVore G, Romero R. Discriminatory hCG zone: its use in the sonographic evaluation of ectopic pregnancy. Obstet Gynecol. 1981;58:156–61. [PubMed] [Google Scholar]
- Kiserud T, Nes SH, Blaas HG, et al. Ultrasonographic velocimetry of the fetal ductus venosus. Lancet. 1991;338:1412–4. doi: 10.1016/0140-6736(91)92720-m. [DOI] [PubMed] [Google Scholar]
- Lenz S, Lauritsen JG, Kjellow M. Collection of Human Oocytes in IVF by ultrasonically guided follicular puncture. Lancet. 1981;1:1163–4. doi: 10.1016/s0140-6736(81)92335-7. [DOI] [PubMed] [Google Scholar]
- Levi S, Hyjazi Y, Schaapst J, et al. Sensitivity and specificity of routine antenatal screening for congenital anomalies by ultrasound: The Belgian Multicentric Study. Ultrasound Obstet Gynecol. 1991;1:102–10. doi: 10.1046/j.1469-0705.1991.01020102.x. [DOI] [PubMed] [Google Scholar]
- Lo YM, Corbetta N, Chamberlain PF, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350:485–7. doi: 10.1016/S0140-6736(97)02174-0. [DOI] [PubMed] [Google Scholar]
- Manning FA, Platt LD, Sipos L. Antepartum fetal evaluation: development of a biophysical profile. Am J Obstet Gynecol. . 1980;136:787–95. doi: 10.1016/0002-9378(80)90457-3. [DOI] [PubMed] [Google Scholar]
- Mari G, Deter RL, Carpenter RL, et al. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative Group for Doppler Assessment of the Blood Velocity in Anemic. N Engl J Med. 2000;342:9–14. doi: 10.1056/NEJM200001063420102. [DOI] [PubMed] [Google Scholar]
- Marsal K, Gennser G, Lindstrom K. Real-time ultrasonography for quantified analysis of fetal breathing movements in man. Lancet. 1976;2(7988):718–9. doi: 10.1016/s0140-6736(76)90011-8. [DOI] [PubMed] [Google Scholar]
- Marsal K. Fetal breathing movements-characteristics and clinical significance. Obstet Gynecol. 1978;52:394–401. [PubMed] [Google Scholar]
- Mayden K, Tortora M, Berkowitz RL, et al. Orbital diameters: a new parameter for prenatal diagnosis and dating. Am J Obstet Gynec. 1982;144:289–97. doi: 10.1016/0002-9378(82)90581-6. [DOI] [PubMed] [Google Scholar]
- Menon U, Maharaj A, Hallett R, et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) Lancet Oncol. 2009;10:327–40. doi: 10.1016/S1470-2045(09)70026-9. [DOI] [PubMed] [Google Scholar]
- Nargund G, Doyle PE, Bourne TH, et al. Ultrasound derived indices of follicular blood flow before HCG administration and the prediction of oocyte recovery and preimplantation embryo quality. Hum Reprod. 1996;11:2512–7. doi: 10.1093/oxfordjournals.humrep.a019150. [DOI] [PubMed] [Google Scholar]
- Nicolaides KH, Soothill PW, Rodeck CH, et al. Disease: intravascular fetal blood transfusion by cordocentesis. Fetal Therapy. 1986;1:185–92. doi: 10.1159/000262267. [DOI] [PubMed] [Google Scholar]
- Nicolaides KH, Soothill PW, Clewell WH, et al. Fetal haemoglobin measurement in the assessment of red cell isoimmunization. Lancet. 1988;1(8594):1073–5. doi: 10.1016/s0140-6736(88)91896-x. [DOI] [PubMed] [Google Scholar]
- Nicolaides KH, Azar GB, Byrne D. Nuchal translucency: ultrasound screening for chromosomal defects in the first trimester of pregnancy. Brit Med J. 1992;304:867–9. doi: 10.1136/bmj.304.6831.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaides KH. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat Diagn. 2011;31:7–15. doi: 10.1002/pd.2637. [DOI] [PubMed] [Google Scholar]
- Nyberg DA, Filly RA, Laing FC, et al. Ectopic pregnancy: Diagnosis by sonography correlated with hCG levels. J Ultrasound Med. 1987;6:145–50. doi: 10.7863/jum.1987.6.3.145. [DOI] [PubMed] [Google Scholar]
- Papageorghiou AT, Yu CK, Bindra R, et al. Multicenter screening for pre-eclampsia and fetal growth restriction by transvaginal uterine artery Doppler at 23 weeks of gestation. Ultrasound Obstet Gynecol. 2001;18:441–9. doi: 10.1046/j.0960-7692.2001.00572.x. [DOI] [PubMed] [Google Scholar]
- Pardi G, Buscaglia M, Ferrazzi E, et al. Cord sampling for the evaluation of oxygenation and acid-base balance in growth-retarded human fetuses. Am J Obstet Gynecol. 1987;157:1221–8. doi: 10.1016/s0002-9378(87)80298-3. [DOI] [PubMed] [Google Scholar]
- Raine-Fenning N, Jayaprakasan K, Deb S, et al. Automated follicle tracking improves measurement reliability in patients undergoing ovarian stimulation. Reprod Biomed Online. 2009;18:658–63. doi: 10.1016/s1472-6483(10)60010-7. [DOI] [PubMed] [Google Scholar]
- Robinson HP. Sonar measurement of fetal crown-rump length as means of assessing maturity in the first trimester of pregnancy. Br Med J. 1973;4(5883):28–31. doi: 10.1136/bmj.4.5883.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson HP, Dunn J. Fetal heart rates as Determined by Sonar in Early Pregnancy. J Obstet Gynaecol Br Commomw. 1973;80:805–9. doi: 10.1111/j.1471-0528.1973.tb11222.x. [DOI] [PubMed] [Google Scholar]
- Rodeck CH, Kemp JR, Holman CA, et al. Direct Intravascular Fetal Blood transfusion by Fetoscopy in Severe rhesus isoimmunisation. Lancet. 1981;1(8221):625–7. doi: 10.1016/s0140-6736(81)91549-x. [DOI] [PubMed] [Google Scholar]
- Romero R, Nicolaides K, Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: a systematic review and meta-analysis of individual patient data. Am J Obstet Gynecol. 2012;206:124.e1–19. doi: 10.1016/j.ajog.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruess ML, Kline J, Santos R, et al. Age and the ovarian follicle pool assessed with transvaginal ultrasonography. Am J Obstet Gynecol. 1996;174:624–7. doi: 10.1016/s0002-9378(96)70439-8. [DOI] [PubMed] [Google Scholar]
- Smidt-Jensen S, Hahnemann N, Jensen PKA, et al. Transabdominal fine needle biopsy from chorionic villi in the first trimester. Prenat Diagn. 1984;4:163–9. doi: 10.1002/pd.1970040302. [DOI] [PubMed] [Google Scholar]
- Thompson, Makowski Estimation of birthweight and gestational age. Obstet Gynecol. 1971;37:44–7. [PubMed] [Google Scholar]
- Timor-Tritsch IE, Monteagudo A, Peisner DB. High frequency transvaginal sonographic examination for the potential malformation assessment of the 9 week to 14 week fetus. J Clin Ultrasound. 1992;20:231–8. doi: 10.1002/jcu.1870200403. [DOI] [PubMed] [Google Scholar]
- Timmerman D, Testa AC, Bourne T, et al. Logistic regression model to distinguish between the benign and malignant adnexal mass before surgery: a multicenter study by the International Ovarian Tumor Analysis Group. J Clin Oncol. 2005;23:8794–801. doi: 10.1200/JCO.2005.01.7632. [DOI] [PubMed] [Google Scholar]
- Trudinger BJ, Cook CM, Jones L, et al. A comparison of fetal heart rate monitoring and umbilical artery waveforms in the recognition of fetal compromise. Br J Obstet Gynaecol. 1986;93:171–5. doi: 10.1111/j.1471-0528.1986.tb07882.x. [DOI] [PubMed] [Google Scholar]
- Ville Y, Hecher K, Ogg D, et al. Successful outcome after Nd-YAG laser separation of chorioangiopagus-twins under sonoendoscopic control. Ultrasound Obstet Gynecol. 1992;2:429–31. doi: 10.1046/j.1469-0705.1992.02060429.x. [DOI] [PubMed] [Google Scholar]
- Wladimiroff JW, Tonge HM, Stewart PA. Doppler ultrasound assessment of cerebral blood flow in the human fetus. Br J Obstet Gynaecol. 1986;93:471–5. [PubMed] [Google Scholar]
- Wladimiroff JW. Behavioural states and cardiovascular dynamics in the human fetus; an overview. Early Hum Dev. 1994;37:139–49. doi: 10.1016/0378-3782(94)90072-8. [DOI] [PubMed] [Google Scholar]
- Yoo SJ, Lee YH, Kim ES, et al. Three- vessel view of the upper mediastinum: an easy means of detecting abnormalities of the ventricular outflow tracts and great arteries during obstetric screening. Ultrasound Obstet Gynecol. 1997;9:173–82. doi: 10.1046/j.1469-0705.1997.09030173.x. [DOI] [PubMed] [Google Scholar]