Abstract
The tremendous development of knowledge, the accumulation of clinical experience, and the enriching of everyday practice with the results of basic and clinical research created the need for splitting medicine in specialities and sub-specialities. Although this evolution is inevitable in order to meet the complex needs and demands of patients, we have to be aware of the risk of neglecting the holistic approach of a person in distress. Indeed, the organ-focused and pathology-centred approach of a patient may not exempt us of the rudiments of care such as the notion that a human being is more than the sum of its parts. This involves the absolute obligation for intra and inter-disciplinary cooperation.
Recently, the European leading societies in Gynaecology, the European Board Obstetricians and Gynaecologists (EBCOG), the European Society of Human reproduction and Embryology (ESHRE), the European Society for Gynaecological Endoscopy (ESGE) and the European Academy for Gynaecological Surgery (+he Academy), have established some common impressive initiatives to improve women’s health care.
As a result of an intensive research programme coordinated by +he Academy with a multidisciplinary team of gynaecologists and surgeons a unique structured training and certification programme in endoscopic surgery is established. This project is a fine example making the dream of multidisciplinary approach reality and achieving some most impressive results. It is without any doubt a major step forwards in the improvement of the quality assurance in endoscopic surgery in benefit of the patients care and has been accepted by our leading European and national societies.
Recently, ESGE and ESHRE developed a new classification on female genital anomalies. An evidence-based updated new classification published in the official journal of both societies was the ended result.
This creative, successful and uneventful collaboration underlines the need for respecting some crucial points: to clearly outline the topic of common action, to find the working platform, to define the method and to respect independence of each society by clarifying the borders and the responsibilities. Keeping the window of the collaboration open is crucial for keeping the window to medicine of the future unlocked.
Keywords: Basic research, certification programme, classification systems, clinical research, collaboration, gynaecology, multidisciplinary, societies, training
The core business of medicine is patient’s health and well-being
Ever since the Hippocratic oath, that required a new physician to swear upon a number of healing gods that he would uphold certain professional ethical standards in his efforts to cure the diseased, good medical practice has been the guideline through ages of discovery and progress. However, the healing gods have been replaced by mankind and its ever-growing grip on health and disease whereas the needs of patients have become very complex. The World Health Organization (WHO) justly defines health as a state of complete physical, mental and social well-being and not merely as the absence of disease or infirmity. (WHO, 1946)
These evolutions make it impossible nowadays for a physician to solitary keep his vow to the patient and there is an increasing need for support of academic authorities, professional societies and industrial partners. Furthermore, these bodies are bound to collaborate between them in order to reach the final goal which is to restore and preserve patient health as defined by the WHO in this continuously changing world.
The ever-changing world
Without minimizing the merit of Hippocrates and his fellow pioneers, we cannot deny the fact that they practiced primary medicine in a small and homogeneous world. Since then, there has been a tremendous evolution in knowledge, technical possibilities and communication assets in a world with far-reaching environmental changes where furthermore socio-cultural, ethicaland juridical aspects of medicine became more and more prominent.
Apparently unlimited technical possibilities: the peaceful revolution in medicine
In the slipstream of the second industrial revolution (1867-1914), the so-called ‘age of synergy’, medicine benefitted from the numerous technological inventions developed for the industry (Vaclav, 1946). In 1917, Paul Langevin attempted to detect submarines using transducers to generate and detect ultrasonic waves in air and water; that was based on the piezzo-electric phenomenon, already discovered in 1880 by Jacques and Pierre Curie giving birth to the first technological application of ultrasound. The idea to implement this technique in medicine led at first to the exploration of the small ‘intra-uterine submarines’ and was the basis of the later widespread use of ultrasound in obstetrics and gynaecology. Further collaboration with endoscopic companies and their engineers, brought us to the intra-uterine surgery on the foetus.
Although the first endoscope was developed in 1806 by Philipp Bozzini in Mainz with his introduction of a ‘Lichtleiter’ (light conductor) ‘for the examinations of the canals and cavities of the human body’, modern endoscopy became only possible after the manufacturing, in close conjunction with the endoscopic companies, of safe devices for distension of the uterine and abdominal cavity. In the last decades of the 20th century and in the 21th, the development of very performing endoscopic instruments and tools, seems to give us unlimited possibilities to treat our patients in a minimal invasive way.
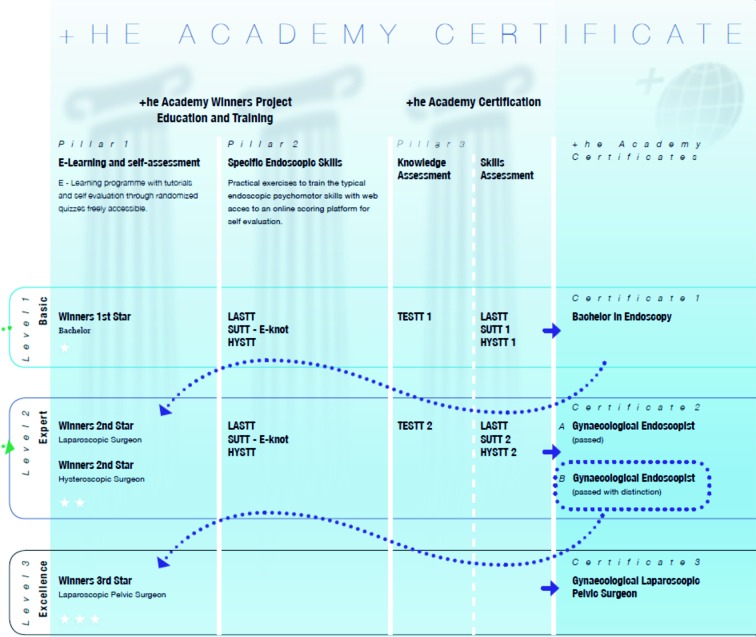
Introduction of novel high techniques such as high definition and 3D endoscopy, 3D ultrasound and Magnetic Resonant Imaging (MRI) represented a ‘peaceful revolution’, changing the diagnostic work-up and the treatment of gynaecological patients so deeply that current management of women has almost nothing to do with the approach before that period (Fig. 1).
1. Power of vision “MRI and laparoscopic image of a pregnancy in a rudimentary horn”.
A tsunami of knowledge: from splitting to the “need” of reconstruction
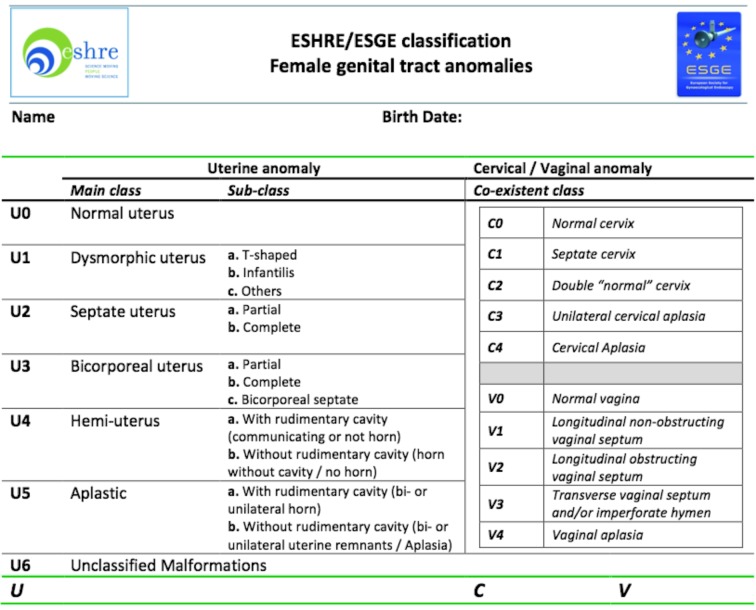
From Leonardo da Vinci to Einstein, man has gathered masses of deeper insights into the fundamentals of nature and life by exploring the boundaries of the human mental and physical potential. Contemporary medicine, starting with Vesalius, who revealed the secrets of anatomy, and da Vinci’s Vitruvian Man (Fig. 2), commonly associated with the science of physiology, is no longer the‘art of healing’ but a scientifically well elaborated and high-technological discipline.
2. De humani corporis fabrica libri septem, A. Vesalius and Vitruviusman van Leonardo da Vinci, ca. 1490.
However, the tremendous development of knowledge, the accumulation of clinical experience, and the enriching of everyday practice with the results of basic and clinical research resulted in the need for splitting medicine, at first in specialities and later in sub-specialities. Regarding our discipline, we witnessed in the last decades that the care for a pregnant woman and her newborn child (Obstetrics or Foeto-Maternal Medicine) and the faithful concern for the general welfare of women before and after pregnancy (general gynaecology) went both their own way. Inside these two pillars, subspecialties emerged: perinatology, foetal medicine, reproductive medicine, gynaecological oncology, urogynecology and others. And to these boughs, new branches grew, focusing on an individual technique (endoscopy, ultrasound), organ (breast) or even a single disease (endometriosis).
Although this evolution is inevitable in order to meet the complex needs and demands of patients, we have to be aware of the risk of neglecting the holistic approach of a person in distress. Indeed, the organ-focused and pathology-centred approach of a patient may not exempt us of the rudiments of care such as the notion that a human being is more than the sum of its parts. This involves the absolute obligation for intra and inter-disciplinary cooperation.
The globe has become our back garden: together under the same “flag”
Adaptation of progresses in medicine to the important demographic changes in the last decades remains a very important humanistic challenge. The search for new concepts to help every patient in his/her specific environment has become imperative: a multidisciplinary and global approach is the required basis of any initiative in this regard.
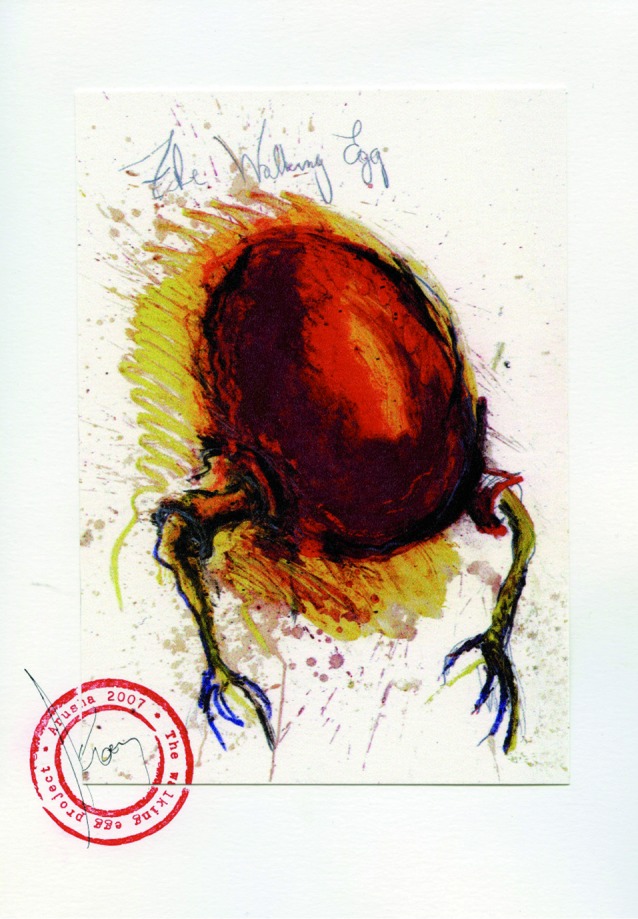
A perfect example of collaboration is the Walking Egg Project (Ombelet, 2013). This non-profit organization strives to raise awareness about childlessness in resource-poor countries. It wants to make reproductive health care, including assisted reproductive technologies, available and accessible to a much larger proportion of the population. The Walking Egg believes that reproductive health care is a neglected aspect of family planning in resource-poor countries. Right from the start in 2010, they opted for a multidisciplinary and global approach to realise affordable and accessible reproductive health care programmes.
In corporation with the ESHRE and the WHO (World Health Organisation), medical, social and economic scientists and experts were gathered to discuss and work together towards a common goal: strengthen reproductive health care through innovation and research, advocacy and networking, training and capacity building, and service delivery. All scientists involved have agreed to donate the royalties of all inventions made in the frame of this project to the npo, also the founding member and well-known artist Koen Vanmechelen contributes actively to the fundraising of this global project. (Fig. 3).
3. Colored lithography of The Walking Egg from the artist Koen Van Mechelen who supports the project.
Today The Walking Egg has achieved and publish the first results using a simplified culturing system for in vitro fertilisations, baby take home rates seems to be equal to the best high tech IVF laboratories only at significantly reduced cost. The first pregnancy resulted in a term delivery of a healthy baby and today over 16 healthy children are born using this simplified method (Van Blerkom et al., in press).
Education is only a mouse click away
Not only patients, but also physicians can claim their absolute right of access to all available sciences. This implements the obligation for the ‘custodians of knowledge’ such as universities and scientific Societies to provide in every possible way with affordable tools for learning and training. In this perspective, we are blessed with the World Wide Web that brings all information home with only one mouse click. E-learning and e-training are nowadays an essential part of the education of young physicians.
In response to this evolution, WeBSurg has initiated a free of charge World Virtual University that gathers videos, operative techniques, lectures, expert’s opinions, debates and clinical cases of all endoscopic surgical disciplines, providing peer reviewed information to all interested physicians. (http://www.websurg.com/virtual_university).
+he Academy provides at the virtual university a structured e learning programme called Winners Project providing the necessary tutorials, video’s, communication platform and self-evaluation questionnaires giving access to every individual resident or gynaecologist worldwide to the necessary information to learn the endoscopic surgical dimension in a structured way with a validation programme to go from one level to the other. (http://www.websurg.com/winners) (Fig. 4).
4. Winners Project, the first free online educational program for Gynaecological endoscopic Surgery.
Endoscopic Surgery an educational challenge for the benefit of the patient
The apprentice-tutor model was useful for training surgeons during hundreds of years, but the complexity of surgical technology in the 21st Century, especially the endoscopic surgery, has exponentially increased the demands on surgical education. In contrast with this classical model, it has progressively been accepted that endoscopic surgery, demanding specific skills, should be also trained outside the operating theatre (Van der Wal, 2007). Although many systems, including animal models and simulators, have been proposed, an in-house structured and validated method, easily implemented at any place is missing.
Therefore, at the centre of surgical technology of the KULeuven, gynaecologists and surgeons joined forces and developed a training model suitable for the training of the specific laparoscopic skills, monitoring the learning process and measuring the skill level at a particular moment. Exercises related only with the endoscopic dimension of a laparoscopic procedure and also with specific surgical tasks were measured in a specially designed trainer box. The results demonstrated that this model is suitable for both training and measuring laparoscopic skills with face, content and construct validity (Molinas et al., 2008; Campo et al., 2010; Molinas and Campo, 2010). This simple and cost friendly in vitro model can be easily implemented in all educational centres for continuous training and evaluation, which will facilitate the learning process in the operating theatre and preserve the apprentice-tutor model to the essential: to teach surgery.
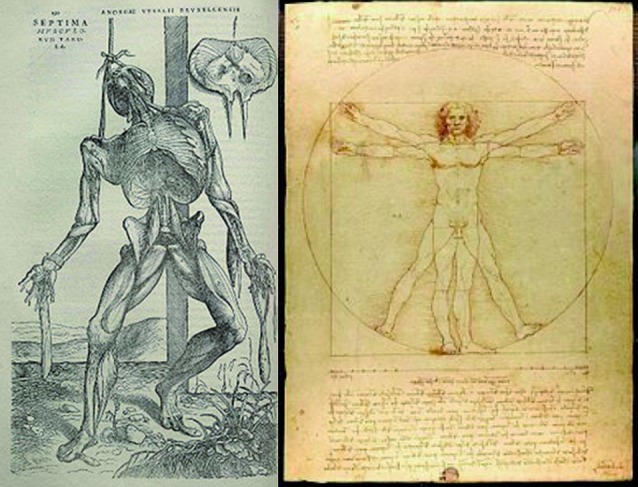
+he Academy certification programme in endoscopic surgery
With the universally accessible Winners project and the accessible training and testing programme of the psychomotor and surgical skills through the Academy web application, both theoretical and practical skills can be acquired in an affordable and accessible way to learn the necessary skills to enter into the different surgical training programmes for endoscopic surgery (Campo et al., 2012a; 2012b).
+ Academy has developed an official evaluation of the theoretical and typical practical endoscopic skills to be able to work in this specific environment resulting in a certificate on 3 different levels (Fig. 5) (European Academy, 2013). The Bachelor certificate expresses the level of the individual which is required to enter the one to one in OR training, whereas the Gynaecological endoscopist gives access to the ESGE advanced endoscopic surgeries and if the individual passes the test cum laude the gate to the expert surgeries is opened.
5. +he Academy certificates in Endoscopic surgery (Pillar 1 – 3 of the GESEA and ECRES program).
This official evaluation consists out of 100 theoretical questions and 9 different endoscopic practical tests. It is worldwide applicable and major interest to implement the system in USA, Asia and Latin America exists.
The GESEA and ECRES programme
Based on the above described certification programme both ESGE as ESHRE have defined their own diploma programme in endoscopic surgery. Each society recognizes the diplomas of the other one and all the diplomas belong to the same European framework of Diplomas in Endoscopic Surgery.
In an effort to improve knowledge and skills in endoscopic surgery, to increase operative efficiency, to reduce unnecessary costs and to enhance patient’s safety and the well-being, the ESGE has officially launched the Gynaecological Endoscopic Surgical Education and Assessment or GESEA programme at its annual congress in Berlin 14-19 October 2013.
The programme is founded on 5 specific pillars of surgical professional competence. Each pillar is defined by a documented educational training route and appropriate stages for assessment. The 5 pillars together give rise to an interesting ESGE diploma programme in which we recognise 3 distinguished levels of surgical expertise (ESGE, 2013).
The first level provides the diploma of Bachelor in Endoscopy, whereas for the second level one can go for the Gynaecological Laparoscopist, Gynaecological Hysteroscopist or for both diplomas expressed as Gynaecological Endoscopist. The third level refers to the expert pelvic surgery with, gastrointestinal, vascular and uro-gynaecological dimension the diploma is called “Laparoscopic Pelvic Surgeon “. A further important evolution of the implementation of the GESEA programme is that standards and criteria are defined for centres who have an accredited training and testing programme in gynaecological endoscopy and centres who will receive the authorisation for Bachelor certification.
Following the same rules, assessing the individual in the five domains of competence and using +he Academy tests for the evaluation of the psycho-motor skills, ESHRE has developed the ESHRE Certification on Reproductive Endoscopic Surgery (ECRES). Although using the same certification platform the ESHRE has elaborated a very nice diploma programme for the recognition of the reproductive surgeons (ESHRE, 2013). After obtaining the diploma of Bachelor in reproductive surgery, the applicant has to pass the ECRES Academy certificate, perform a practical surgical exam through video evaluation and a final theoretical exam on reproductive surgery.
Both programmes uses the same methodology but due to their clearly different natures and surgical domains they issue clearly distinguished diplomas. These unique programmes give, nowadays, for the first time the opportunity to those gynaecologists with special interest in endoscopic surgery to improve their hysteroscopic and laparoscopic surgical abilities and experience, establishing their status as either reproductive or gynaecological endoscopic surgeons and allowing them to become part of an élite of specialists, capable of offering patients all over the World the care they are entitled to.
A new approach to medicine: reconstruction of unity through common initiatives
Although sub-specialization allowed the development of research in depth and made the management of patients more adequate and safe, the ‘reconstruction’ of unity in human knowledge and clinical practice remains a difficult but necessary challenge. In the ideal World, profound collaboration between all those involved in medicine (physicians, scientists, engineers, industrial companies, universities and scientific societies) will overcome all possible hurdles in this process.
When decided and applied, the results of joint efforts are really impressive. Recently, the ESGE, +he Academy and the ESHRE, realizing the need for united action, have established common initiatives thus changing a dream into reality.
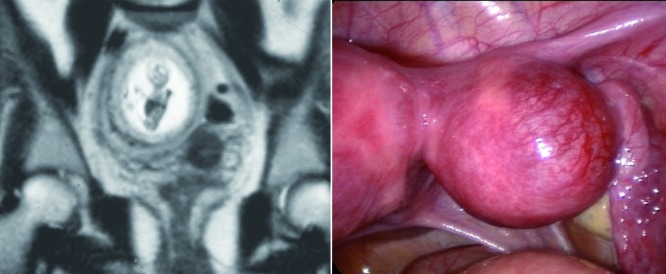
A new, evidence-based classification of congenital uterine anomalies
Female genital anomalies is a topic within the interests of ESHRE and ESGE since they are benign entities affecting reproductive potential of the women but, on the other hand, their treatment is nowadays feasible and effective with endoscopy. An evidence-based updated new classification has been recognized as an urgent priority for their management. EAGS, recognizing this need, has established, quite early, a scientific project on that issue; the characteristics of the new system have been clarified through a systematic and critical re-evaluation of the existing proposals and, thereafter, a proposal for a updated clinical classification of uterine anomalies to be used as the scientific background for a working group of experts in the field has been prepared (Grimbizis et al., 2013a; 2013b).
It was obvious that ESHRE and ESGE, based on that preparative work, could further contribute to this common challenge from a different but supplementary point of view if a common “platform” of action could be found; this was accomplished with the establishment of a common working group under the code name CON(genital)UT(erine)A(nomalies). Once the platform was found, a scientific committee has been appointed to run the project, and DELPHI procedure was adopted as the method to look for a consensus between the scientists and to develop the new system. Once the project came to the end and the classification was ready, after getting approval by the Executive Committees, the new system was published in the official journals of the two Societies at the same time (Grimbizis and Campo, 2010; 2012) (Fig. 6). This was really a very important step forward since the fruitful collaborations of the European Societies interested in the matter created actually a European classification system in a hot issue of clinical interest.
6. New classification on female congenital anomalies (modified from references 9 &10).
The recipe for a smooth and successful collaboration
The examples mentioned above actually gave us an idea of the framework and the crucial points for a successful and uneventful collaboration between scientific Societies.
First point is to outline the topic of common interest and clearly describe the aims of the collaboration. Secondly, it is important to find a platform for collaboration. This can be different depending on the issue and on the priorities, but it should certainly be functional and flexible. To establish the diploma programmes independent Steering Committees for each Society where established as for the new classification the work was performed by a common working group the CONUTA group.
Third point is to define the method to accomplish the aims. This also could be different depending on the issue and the required final result. And last but not least, since it might be the most important point, is to clarify the borders of the cooperation for each Society. The own responsibilities and rights and the respect for each Society’s independence and its distinct scientific entity are key points of any common initiative.
Finally, although rules are always the basis for an uneventful collaboration, the persons involved in each process are of equal importance. Open-minded, inventive, team-workers, opinion makers and bearing new ideas scientists are the ideal candidates for these initiatives.
Collaboration (between societies) is not always an easy task to be achieved but it is certainly worthwhile because it creates the opportunities to explore new horizons in research and clinical practice. It is our assignment to collaborate in the pursuit of the best possible care for every patient worldwide and, now that the window to the medicine of the future is unlocked, it is our common responsibility to keep it open.
References
- Campo R, Reising C, Van Belle Y, et al. A valid model for testing and training laparoscopic psychomotor skills. Gynecol Surg. 2010;7:133–141. [Google Scholar]
- Campo R, Molinas CR J, De Wilde RL, et al. Are you good enough for your patients? The European certification model in laparoscopic surgery. FV&V in ObGyn. 2012;4:95–101. [PMC free article] [PubMed] [Google Scholar]
- Campo R, Wattiez A, De Wilde R. Training in Laparoscopic Surgery: From the Lab to the OR. Zdrav Var. 2012;51:285–298. [Google Scholar]
- European Academy Of Gynaecological surgery. www.europeanacademy.org Certification Project 2013.
- ESGE. www.esge.org European Diploma in Gynecological Endoscopic Surgery: Gynecological Endoscopic Surgical Education and Assessment (GESEA) Project. 2013
- ESHRE. www.eshre.eu ESHRE Certification for Reproductive Endoscopic Surgery (ECRES) 2013
- Grimbizis GF, Campo R. Congenital malformations of the female genital tract: the need for a new classification system. Fertil Steril. 2010;94:401–407. doi: 10.1016/j.fertnstert.2010.02.030. [DOI] [PubMed] [Google Scholar]
- Grimbizis GF, Campo R, on behalf of the SC of the CONUTA ESHRE. Brucker S, Gergolet M, Tanos V, Li T, De Angelis C, Di Spiezio SA. Clinical approach for the classification of congenital uterine malformations. Gynecol Surg. 2012;9:119–129. doi: 10.1007/s10397-011-0724-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimbizis GF, Gordts G, Di Spiezio SA, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital malformations. Hum Reprod. 2013;28:2032–2044. doi: 10.1093/humrep/det098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimbizis GF, Gordts G, Di Spiezio SA, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital malformations. Gynecol Surg. 2013;10:199–212. doi: 10.1007/s10397-013-0800-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molinas CR, De Win G, Ritter O, et al. Feasibility and construct validity of a novel laparoscopic testing and training model. Gynecol Surg. 2008;5:281–290. [Google Scholar]
- Molinas CR, Campo R. Defining a structured training program for acquiring basic and advanced laparoscopic psychomotor skills in a simulator. Gynecol Surg. 2010;7:427–435. [Google Scholar]
- Ombelet W. The Walking Egg Project: Universal access to infertility care – from dream to reality. FV&V in ObGyn. 2013;5:161–175. [PMC free article] [PubMed] [Google Scholar]
- Vaclav S. Creating the Twentieth Century: Technical innovations of 1867–1914 and their lasting impact signed on 22 July 1946 by the representatives of 61 States. Official Records of the World Health Organization, 1946; No 2: 100; entered into force on 7 April 1948. Oxford; New York: Oxford University Press; 2005. [Google Scholar]
- Van Blerkom J, Ombelet W, Klerkx E, et al. First Births with a Simplified Culture System for Clinical IVF and ET. RBM Online : doi: 10.1016/j.rbmo.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Van der Wal G. http://www.igz.nl/publicaties/rapporten/2007/mic Risico’s minimaal invasieve chirurgie onderschat. 2007
- World Health Organization. Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. June 19-22. New York: 1946. [Google Scholar]