Abstract
Empirical research into cross-border reproductive care is scarce and many facets of the phenomenon are unexplored. The objective of this study was to compare Belgian and Dutch patients regarding the way they perceived the treatment they received and regarding the embryo disposition decisions (EDDs) they made.
A questionnaire was sent to patients for whom embryos were cryopreserved at the Ghent University Hospital, Belgium.
The response rate was 79%. Of those who replied the questionnaire, 70.9% was Belgian (n = 231) and 29.1% was from The Netherlands (n = 95). Dutch patients were on average three years older (38.22 years) than Belgian patients (35.30 years). Belgian patients more often considered their last treatment both physically and emotionally burdensome compared to Dutch patients (36.0% versus 25.5%). Half of the Dutch patients wanted to continue the storage of their embryos compared to a third of the Belgian patients. Dutch patients less often considered the EDD difficult to make compared to the local patients and they less often experienced stress or tension regarding the decision. In conclusion, Dutch cross-border patients had more positive experiences regarding to the treatment and the EDD compared to Belgian patients. However, they wanted to hold on longer to their cryopreserved embryos.
Keywords: Belgium, cross-border reproductive care, embryo disposition, infertility, the Netherlands
Introduction
Cross-border reproductive care has attracted considerable attention in recent years. The interest can be largely explained by the potential ethical and health policy implications of the phenomenon (Pennings et al., 2008). However, empirical research about cross-border reproductive care remains scarce. The majority of patients who seek treatment abroad seem to do so for legal reasons (Hudson et al., 2011; Shenfield et al., 2010). The Dutch patients are, however, an exception. In a study in which patients could indicate more than one reason for leaving their country in search for reproductive care, the main reason for Dutch patients was to seek better quality of care (53.0%) while legal reasons only came second (32.2%) (Shenfield et al., 2010). Furthermore, 25.5% crossed the border because of previous treatment failure and 7.4% of Dutch patients complaining about difficulties in access to reproductive care in The Netherlands. For nearly one in four Dutch cross-border patients (23%) the reason for coming to Belgium was related to treatment with donor gametes or embryos.
A recent empirical study that focussed on infertility patients coming to Belgium revealed that 29% of all cross-border patients entering Belgium are Dutch (Pennings et al., 2009). This is the second largest group of cross-border infertility patients entering Belgium, after the French patients (38%). Patients from the Netherlands mainly came to Belgium to obtain ICSI with ejaculated sperm (38%) followed by three other types of treatment (sperm donation, ICSI with non-ejaculated sperm and IVF with own gametes) that each attracted around 15% of the Dutch patients (Pennings et al., 2009).
The Department of Reproductive Medicine of the Ghent University Hospital (Belgium) attracts a considerable number of Dutch patients (De Sutter et al., 2003; Pennings et al., 2009). The centre’s geographical location (32 km from the Dutch border) and the fact that the official language is Dutch are important factors in its attractiveness to these patients. In 2007, the centre treated 1423 Belgian and 366 Dutch patients.
This paper compares Dutch cross-border patients who were treated at the Department for Reproductive Medicine in Ghent with Belgian patients of the department regarding their assessment of treatment burden, their attitudes towards the Embryo Disposition Decision (EDD) and their decisions about their leftover embryos. This study is a secondary analysis of data that was collected to address research questions about patients’ EDDs (Provoost et al., 2011). This means that the patients were not recruited because of their nationality. This paper presents the first empirical data on cross-border patients’ EDD decisions.
Methods
From 1992 to 2008, all patients for whom embryos were cryopreserved at the Department of Reproductive Medicine, Ghent University Hospital (Belgium) received an EDD form by mail every two years following the year in which the embryos were frozen. These patients received an anonymous questionnaire by mail together with the EDD form.
Participants
Patients were included when they spoke Dutch, their embryos were created with the couples’ own gametes and stored for at least two years, and their stored embryos were not transferred before responding to the questionnaire.
Procedure
Of the initial 448 patients included in the study, 36 (8%) patients moved without notifying the clinic and could not be reached. A total of 412 patients received the questionnaire which was addressed to the female partner of the couples. A detailed description of the questionnaire can be found in another paper on this study (Provoost et al., 2011). Questions were asked about the outcome of the last treatment cycle and how the patients assessed this last treatment cycle (treatment burden). Furthermore, the questionnaire collected data on patient characteristics, the current EDD and the process of decision-making, and patients’ attitudes towards the EDD. Attitude statements to be scored on a five-point Likert-type scale (strongly agree, agree, neutral point, disagree and strongly disagree) were presented to explore several aspects of the patients’ attitude towards cryopreserved embryos, their use for fertility treatment and the decisions regarding these embryos. The statements were placed in a random order to optimize task performance and to reduce unintended order effects. Patients were asked to score the moral status they attached to the embryos on a seven-point semantic differential scale ranging from ‘collection of cells’ to ‘child’. Data were gathered between January 2007 and July 2007. The mailing procedure was based on the Total Design Method (Dillman, 1991) to increase response and was approved by the Ethics Committee of the Ghent University Hospital.
Analysis
Patients were divided into two groups based on their country of origin: Belgian and Dutch patients. Data were analyzed using Predictive Analytics Software (PASW version 18) and StatXact (version 8). Fishers’ Exact test was used to compare the distribution of unordered variables and Kruskal-Wallis Exact test was used for single-order categories. One-way ANOVA was used for continuous data normally distributed (age) and Wilcoxon test was used for data not normally distributed (number of embryos). P < 0.05 was considered statistically significant.
Results
The questionnaire had a response rate of 79% (326/412). Of those who replied to the questionnaire, 70.9% was Belgian (n = 231) and 29.1% was from The Netherlands (n = 95). There were no significant differences in response pattern (response, no response, or could not be reached) between Belgian and Dutch patients (Table 1).
Table 1. Response to the questionnaire according to the patients’ nationality.
| Nationality | p-valueb | Total | ||||
|---|---|---|---|---|---|---|
| Belgian(N = 314) | Dutch(N = 134) | |||||
| N | % | N | % | |||
| Responded | 231 | 73.6 | 95 | 70.9 | 0.814 | 326 |
| Did not respond | 58 | 18.5 | 28 | 20.9 | 86 | |
| Could not be reached | 25 | 8.0 | 11 | 8.2 | 36 | |
Patient characteristics
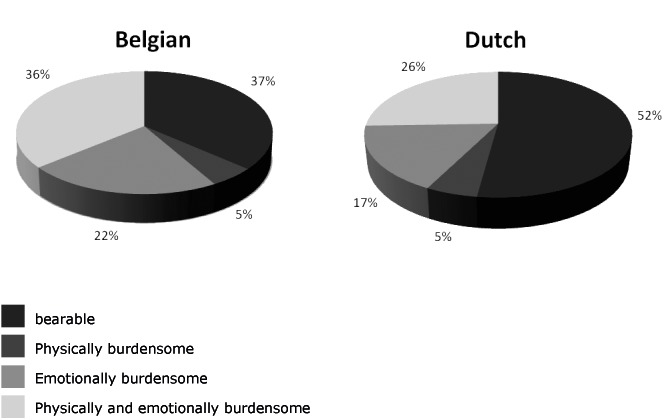
Dutch patients were on average three years older than Belgian patients (mean of 38.22 versus 35.30; p = 0.000). Figure 1 demonstrates the age distribution of the two patient groups, showing a higher proportion of Dutch patients in the older age group. We compared the proportion of both nationalities in two age groups with a cut-off point of 41 years (the age limit according to the Dutch guidelines of 1998) (Table 2). The majority of the patients in the lower age group are Belgian (76.2%) while in the group above 41 years, more than half is Dutch (56.6%) (p < 0.000).
Fig. 1. Age distribution of Belgian and Dutch patients (N = 326).
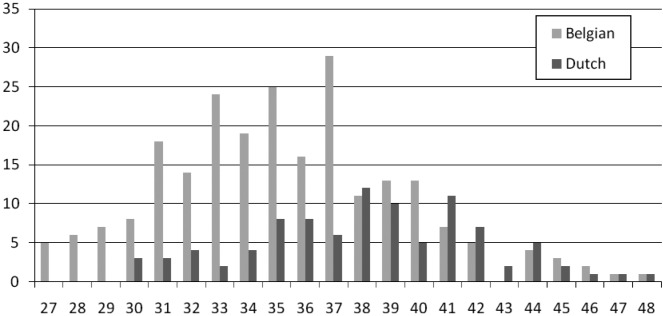
Table 2. Patient characteristics according to their nationality (N = 326) a.
| Nationality | p-valueb | Total | ||||
|---|---|---|---|---|---|---|
| Belgian(N = 231) | Dutch(N = 95) | |||||
| N | % | N | % | |||
| Age (before or from 41 years)c | ||||||
| 27-40 | 208 | 76.2 | 65 | 23.8 | 0.000 | 273 |
| 41-48 | 23 | 43.4 | 30 | 56.6 | 53 | |
| Children | ||||||
| No children | 17 | 7.4 | 14 | 14.7 | 0.064 | 31 |
| Children, but none were conceived through IVF | 29 | 12.7 | 7 | 7.4 | 36 | |
| Children, and at least one child was conceived through IVF | 183 | 79.9 | 74 | 77.9 | 257 | |
| Timing of the last treatment cycle | ||||||
| Less than two years ago | 51 | 22.3 | 30 | 31.6 | 0.023 | 81 |
| Between two years and three years ago | 137 | 59.8 | 41 | 43.2 | 178 | |
| More than three years ago | 41 | 17.9 | 24 | 25.3 | 65 | |
| Assessment of treatment burden of the last treatment cycle | ||||||
| Bearable | 83 | 36.4 | 49 | 52.1 | 0.011 | 132 |
| Physically burdensome | 12 | 5.3 | 5 | 5.3 | 17 | |
| Emotionally burdensome | 51 | 22.4 | 16 | 17.0 | 67 | |
| Physically and emotionally burdensome | 82 | 36.0 | 24 | 25.5 | 106 | |
| Level of education | ||||||
| No upper secondary education | 13 | 5.7 | 9 | 9.6 | 0.000 | 22 |
| Upper secondary education | 67 | 29.3 | 42 | 44.7 | 109 | |
| Tertiary education, short | 93 | 40.6 | 10 | 10.6 | 103 | |
| Tertiary education, long | 56 | 24.5 | 33 | 35.1 | 89 | |
| Life stance and religion | ||||||
| Christian overall | 145 | 63.0 | 38 | 40.0 | 0.000 | 183 |
| Catholic | 87 | 37.8 | 21 | 22.1 | 108 | |
| Protestant | 0 | 0.0 | 7 | 7.4 | 7 | |
| Christian | 58 | 25.2 | 10 | 10.5 | 68 | |
| Muslim | 5 | 2.2 | 5 | 5.3 | 10 | |
| No denomination | 58 | 25.2 | 43 | 45.3 | 101 | |
| Other | 1 | 0.4 | 2 | 2.1 | 3 | |
Row percentages.
aData missing for one patient for ‘Life stance and religion’, for two patients for ‘Timing of the last treatment cycle’ and ‘Children’, for three patients for ‘level of education’, and for four patients for ‘Assessment of treatment of treatment burden’.
bFishers’ Exact test: significance of difference of distribution between Belgian and Dutch patients. Kruskall-Wallis test for ‘Level of education’.
cThe recommended age limit to treat women in the Netherlands.
The proportion of patients who had children conceived through IVF was similar between the two groups. However, although not statistically significant, twice as many Dutch patients were still childless at the time of the questionnaire (14.7% versus 7.4%; p = 0.060). There were no differences between both nationalities in the partners’ child wish or in the proportion of couples that were separated by the time of the questionnaire.
About 60% of the Belgian patients had their last treatment between two and three years ago, whereas the time since the last treatment cycle was more varied in the Dutch patients (p = 0.023). There were no differences between the two nationalities in the outcome of this last treatment. When asked about their assessment of the treatment burden, Dutch patients considered their last treatment more often bearable compared to Belgian patients (52.1% versus 36.4% respectively; p = 0.012). Belgian patients more often evaluated their last treatment as both physically and emotionally burdensome (25.5% of Dutch patients versus 36.0% of Belgian patients; p = 0.001) (Fig. 2). More than half of the Belgian patients (58.4%) versus 42.5% of the Dutch patients judged their last treatment cycle emotionally burdensome (whether or not also physically burdensome) (p = 0.014).
Fig. 2. Assessment of treatment burden by Belgian and Dutch patients.
There was a statistically significant difference between the two patient groups in level of education. There are 10% more Dutch patients with a university degree or equivalent (35.1% versus 24.5%; p = 0.056) but also about 20% more patients with a maximum of secondary education.
Nearly two thirds of Belgian patients were Catholic or Christian whereas this was only one third in Dutch patients. In contrast, nearly half of Dutch patients were not religious compared to one in four Belgian patients. We asked the patients how important they considered their personal stance or religion to be for the EDD (scored on a five-point Likert-type scale) and combined that with the type of personal stance or religion. This analysis showed that Dutch patients less often adhered to a religious denomination which they considered important in their decision-making (17.9% versus 31.7% in Belgian patients; p = 0.014).
Attitudes towards embryo disposition decisions
Patients of both nationalities found the EDD equally important (Table 3). However, the percentage of Belgian patients who thought that the EDD was difficult was higher than the percentage of Dutch patients (53.3% versus 40.9%). No differences were found in the patients’ level of concern with their cryopreserved embryos or their anticipated regret about the EDD. An equal proportion of patients from both countries found the EDD an emotionally loaded decision (62%). We asked patients who thought that the EDD was emotionally loaded what type of emotions they felt regarding the EDD, there were no differences in feelings of grieve, relief or other feelings. The only difference was found with regard to stress or tension with Belgian patients more often than Dutch patients reporting stress or tension (52.1% versus 30.4%; p = 0.011).
When looking at the value of the cryopreserved embryo, about a third of both patient groups thought that the embryo was important independent from the probability of using it in a next treatment cycle. However, significantly more Belgian than Dutch patients thought that embryos, once transferred into the womb, were more valuable than those still in storage (40.7% versus 26.4%).
Dutch and Belgian patients had a comparable high confidence in the people caring for them and their embryos (about 90% or more). With regard to the health of children born out of cryopreserved embryos, Dutch patients were worried more than Belgian patients (although not statistically significant). The storage fee was important as a factor in the decision for 10.8% of Dutch patients, compared to twice as many Belgian patients (22.9%).
Looking at their attitudes towards donation for science, about half of the patients from each country preferred their embryos to be used for the improvement of fertility treatments and between 40-50% of the patients thought that the donors should have a say in the selection of projects. More Dutch patients than Belgian patients knew what stem cell research or scientific research with embryos in general was.
Regarding donation to others for reproduction, about 60% in both patient groups compared this option to adoption. There were no significant differences in the patients’ thoughts on the importance of the genetic link between donors and child and on whether donors should have a say in the selection of the recipient couple. However, significantly more Belgian patients indicated that a child resulting from embryo donation should not be able to trace the donors later.
Finally, there were no significant differences in the patients’ attitudes about discarding (e.g. respect for the embryo and the method of discarding). There were also no differences in the moral status that both groups of patients attached to the embryos (data not shown).
Actual decisions
Dutch patients more often wanted to continue the storage of their cryopreserved embryos (49.5% compared to 32.9% of Belgian patients; p = 0.006) (Table 3). There were also significantly more Dutch patients who wanted to continue the storage of their embryos while neither of the partners had a desire for a(nother) child (7.8% versus 1.4%; p = 0.008).
Table 3. Attitudes towards cryopreserved embryos and EDD-making according to the patients’ nationality.
| Belgian(N = 231) | Dutch(N = 95) | p-valueb | |||
|---|---|---|---|---|---|
| % agreeinga | |||||
| Statement | N | % | N | % | |
| (Emotional) response towards the embryo or the decision-making process | |||||
| I find it difficult to choose a disposition for my embryos. | 121 | 53.3 | 38 | 40.9 | 0.049 |
| I rarely think about my embryos. | 67 | 29.9 | 20 | 22.0 | 0.167 |
| Value of the embryo | |||||
| An embryo that was transferred into the womb is more valuable than a cryopreserved embryo. | 92 | 40.7 | 24 | 26.4 | 0.020 |
| Medical and practical considerations | |||||
| I have confidence in the physicians and the laboratory staff who are involved in my treatment and the storage of my embryos. | 203 | 89.4 | 89 | 94.7 | 0.198 |
| I would have more worries about malformations in my child when cryopreserved embryos would be used for the treatment compared to fresh embryos. | 48 | 21.1 | 29 | 30.9 | 0.084 |
| The storage fee is important in my decision to continue storage. | 52 | 22.9 | 10 | 10.8 | 0.013 |
| Donation for science | |||||
| I do not know what scientific research with embryos is. | 148 | 65.5 | 48 | 52.2 | 0.031 |
| I do not know what stem cell research is. | 98 | 43.6 | 33 | 36.3 | 0.258 |
| People who donate embryos for science should have a say in the selection of the project in which they will be used. | 93 | 41.0 | 45 | 48.9 | 0.213 |
| Donation to others | |||||
| People who donate to others should have a say in the selection of the recipient couple. | 68 | 30.2 | 31 | 34.1 | 0.506 |
| A child born from embryo donation should not be able to trace the donors later. | 98 | 43.6 | 25 | 27.2 | 0.008 |
aCombines point one and two of the 5-point Likert scale: strongly or moderately agreeing.
bFishers’ Exact test: significance of difference of distribution of agreeing versus other patients according to their nationality.
In contrast, in the decisions of patients who did not want to keep their embryos, there were no differences between the two patient groups in the options chosen. Also, when looking at the patients’ willingness to consider each of the options (donation for science, donation to others and discarding) in their process of decision-making, there were no significant differences. Answers to questions about the reasons why they were (un)willing to consider certain options, showed that Belgian patients more often refused to consider donation for science because they feared to feel responsible for what would happen to their embryo (82.6% versus 69.5%; p = 0.011). Furthermore, although not statistically significant, Belgian patients who did not want to consider donation to others more often said they did so because they would be too preoccupied with the thought of a possible child (53.0% versus 42.1%; 0.088).
Process of decision-making
Patients of both nationalities were equally satisfied with the information they had received on the different options to dispose of their embryos: 88% of the patients were satisfied.
There were no statistically significant differences in the partner’s roles in the decision-making process or in the number of patients who had consulted someone other than their partner regarding the EDD. However, one in five Dutch patients had discussed the issue with a family member or a close friend, whereas less than half as many Belgian patients had done so (Table 4).
Table 4. Embryo disposition decisions according to nationality.
| Belgian(N = 231) | Dutch(N = 95) | p-valueb | |||
|---|---|---|---|---|---|
| Statement | N | % | N | % | |
| Do you want to continue storage? | |||||
| Undecided | 2 | 0.9 | 1 | 1.1 | |
| Yes | 76 | 32.9 | 47 | 49.5 | 0.006 |
| No | 153 | 66,2 | 47 | 49.5 | |
| Final EDDa (N = 200) | |||||
| Donation to others | 27 | 17.4 | 5 | 10.6 | 0.363 |
| Donation for science | 78 | 50.3 | 23 | 48.9 | 0.868 |
| Discarding | 37 | 23.9 | 17 | 36.2 | 0.133 |
| Consultation of others regarding the decisiona | |||||
| Someone at the fertility center | 2 | 1.4 | 0 | 0.0 | 1.000 |
| Family or close friend | 12 | 8.3 | 9 | 20.0 | 0.052 |
| Someone else | 4 | 2.8 | 0 | 0.0 | 0.574 |
| Nobody | 129 | 89.0 | 36 | 80.0 | 0.133 |
aN = 200 (patients who do not want to continue storage). Data missing for one patient for ‘Final EDD’. Data missing for 10 patients for ‘consultation of others regarding the decision’.
bFishers’ Exact test: significance of difference of distribution of decisions and consultation categories according to patients’ nationality.
Discussion
Most studies on cross-border reproductive care focus on the difficulties the patients experience or their reasons for travelling (Blyth, 2010; Hughes and Dejean, 2010; Pennings et al., 2009; Shenfield et al., 2010). Moreover, most existing studies are based on small samples of selected patients. The present study performs a secondary analysis of data on patients that were not selected on the fact that they travelled to receive treatment.
Dutch patients were on average three years older than the Belgian inhabitants. This confirms findings of an earlier study on the results of in vitro fertilization in Dutch couples at the Department of Reproductive Medicine, Ghent University Hospital (De Sutter et al., 2003). This study also showed that the duration of infertility was longer for the Dutch than for the Belgian couples. This age difference is also in line with the recent finding that one of the reasons for Dutch patients to come to Belgium was to seek better care after previous treatment failure (Shenfield et al., 2010). The finding that the proportion of Dutch cross-border patients increased from a fourth in the group up to the age of 41 to more than half in the older group can be explained by a guideline in The Netherlands that discourages the application of IVF above the age of 41 (Pennings et al., 2009). Although this guideline has been relaxed in practice in recent years, many Dutch patients still feel unfairly treated and prefer to go to Belgian clinics. It also shows that a considerable number of Dutch patients do not accept the judgement of the Dutch professionals that the success rate is too low above 41.
Significantly more Belgian patients indicated that a child born after embryo donation should not be able to trace the donors later. In Belgium, embryo donation is anonymous by law (Pennings, 2010). The difference in appreciation of the anonymity rule is difficult to explain. There are no data on the attitude of Dutch and Belgian patients in the past but it seems reasonable to assume that the long-lasting debate in the Netherlands preceding the law in 2004 has had an impact on the general acceptance of donor identifiability. However, this suggestion has to be made with caution since all Dutch patients needing donor material were excluded from the study and since 35% of the Dutch patients who go abroad for donor gametes explicitly indicate that they want anonymous donation (Pennings, 2010).
Patients who consider cross-border reproductive care largely rely on their own resources when searching and processing information about fertility centers (which they mostly find through the Internet) (Blyth, 2010; De Sutter, 2011). Also in the Netherlands, the Internet was the first source of information to select a clinic (42.3%) but it was followed very closely by the patients’ local gynaecologist (39.6%) (Shenfield et al., 2010). Most Dutch patients had a fairly long history of fertility treatment at home. As a consequence, they know what to look for, they are familiar with the medical procedures and they know what to expect. Culley et al. (2010) mentioned similar characteristics of the British patients who went abroad.
In contrast to what could be expected, Dutch patients assessed their treatment burden lower than the local patients. The general idea behind the negative evaluation of cross-border care is that these patients have to deal with extra practical issues such as travelling, different culture, language and communication difficulties etc. These issues are generally very limited for Dutch patients when they stay within the Flemish community in Belgium since they share the same language. In addition, other elements, such as the gratefulness for the extra chance they did not get at home, or feeling more in control because of their choice to travel abroad, may weigh heavier in the balance than the practical issues related to crossing the border. The cross-border patients in other studies also reported a high degree of satisfaction and very positive experiences (Blyth, 2010; Culley et al., 2010).
This general positive experience may determine other aspects of the treatment. It may, for instance, make them see the EDD as less difficult. Other explanations are possible here. One could be the self-selection of the foreign patients: are patients who go abroad for medical treatment emotionally stronger patients? Another explanation might be that patients who go abroad invest more in their treatment, financially as well as emotionally, leading to a more positive assessment of their treatment and the decisions that come with it.
Dutch patients tended to keep their cryopreserved embryos longer, despite being older than the Belgian patients. However, once they decided to discontinue storage, there were no significant differences in the type of EDD. Two explanations are possible. First, as patients who are coming from abroad are overall financially better off than the average local patient, the storage fee could be less important in their EDD compared to Belgian patients. For cross-border patients, who mostly do not benefit from reimbursement by their health insurance, the storage fee will be proportionally lower, in light of the totality of their expenses. However, although we have no specific information on this point for our respondents, Dutch patients benefit much more than other foreign patients from financial support from their insurance. In the study of Shenfield et al. (2010), only 16.8% of the Dutch patients indicated that they received no reimbursement while the mean percentage of no reimbursement for the 6 European countries was 71.7%. More than 20% of the Dutch patients received full reimbursement and 44% partial refund. Although patients who look for treatment abroad are most likely financially better off than those who stay at home, the financial threshold clearly is much less relevant for Dutch patients than for other patients.
Second, patients who had invested more in their treatment, both financially and emotionally, could have more difficulties choosing a final disposition for their embryos which may represent their investment, as was found in a qualitative study (Provoost et al., 2009).
Many of the differences between the Belgian and Dutch patients in this study probably stem from a priori population differences between these two groups. Further research should examine these differences more closely in order to make correct interpretations of variations in these patients’ perceptions and decisions. In these studies, cultural differences will have to be taken into account. We know, for instance, that differences between Belgian and Dutch patients regarding the use of antibiotics, can be influenced by differences in religious traditions (Deschepper et al., 2002). However, a priori differences between Belgian and Dutch patients in general may not explain all differences found between local patients and Dutch cross-border patients as there is also a degree of self-selection in the cross-border patients. The latter differ from both the local Belgian patients and Dutch patients who stay in the Netherlands for their treatment in that they apparently do not accept local treatment restrictions or advise. Furthermore, they had a longer treatment history, are very well informed about their own case and about differences between clinics (De Sutter, 2011), and are probably also more conscious of their medical rights.
In conclusion, Dutch cross-border patients had more positive experiences regarding to the treatment and the EDD compared to Belgian patients. However, they wanted to hold on longer to their cryopreserved embryos.
Acknowledgments
Acknowledgement of financial support
VP and PDS are holders of a Postdoctoral Fellowship (VP) and a Fundamental Clinical Research Mandate (PDS) by the Flemish Foundation for Scientific Research (FWO-Vlaanderen).
References
- Blyth E. Fertility patients’ experiences of cross-border reproductive care. Fertil Steril. 2010;94:11–15. doi: 10.1016/j.fertnstert.2010.01.046. [DOI] [PubMed] [Google Scholar]
- Culley L, Hudson N, Blyth E, et al. Travelling abroad for fertility treatment: an exploratory study of UK residents seeking cross-border care. Hum Reprod. 2010;25:s1–i78. [Google Scholar]
- Deschepper R, Vander Stichele RH, Ruskamp FM. Cross-cultural differences in lay attitudes and utilisation of antibiotics in a Belgian and a Dutch city. Patient Educ Couns. 2002;48:161–169. doi: 10.1016/s0738-3991(02)00017-4. [DOI] [PubMed] [Google Scholar]
- De Sutter P. Considerations for clinics and practitioners treating foreign patients with assisted reproductive technology: lessons from experiences at Ghent University Hospital, Belgium. RBM Online. 2011;23:652–656. doi: 10.1016/j.rbmo.2011.07.016. [DOI] [PubMed] [Google Scholar]
- De Sutter P, van der Elst J, Dhont M. Results of in vitro fertilization in Dutch subfertile couples in Ghent, Belgium, 1993-2002: no patient group with decreased prognosis. (article in Dutch) Ned Tijdschr Geneeskd. 2003;147:1741–1746. [PubMed] [Google Scholar]
- Dillman DA. The design and administration of mail surveys. Annu Rev Sociol. 1991;17:225–249. [Google Scholar]
- Pennings G. The rough guide to insemination: cross-border travelling for donor semen due to different regulations. FVVinObGyn. 2010;(Monograph):55–60. [Google Scholar]