Abstract
Background: In Brazil, access to infertility care, including assisted reproductive technologies (ARTs), is restricted. This is the third report of a study on access to infertility care and ARTs within the public sector, focusing on the barriers to these services.
Methods: The study was anchored on quantitative and qualitative methods. For the quantitative study interviews were conducted with health authorities in each of the 26 states, the Federal District, the state capitals and 16 cities with ≥ 500,000 inhabitants and directors of infertility referral centres within the public sector. Qualitative case studies were conducted in five ART centres.
Results: Overall, 63.5% of the authorities reported that complex infertility treatments were unavailable. Barriers identified consisted of “lack of political decision to implement them”, and “lack of financial resources”. In addition, 75% reported to have “no plans to implement them over the next 12 months”. At the facilities offering ART, the barriers to these procedures were the high costs, long waiting times, complex scheduling processes and lack of initiative to implement low cost ARTs.
Conclusions: Infertile couples’ access to ART procedures is restricted due to the insufficient services and lack of political commitment to support existing and new services..
Keywords: Barriers, inequity, infertility care, IVF, low-income populations, public health
Introduction
For women and men who decide to start a family, difficulties conceiving a child may become a source of strain and cause psychosocial problems. The impact of infertility on women and men’s lives, and on their intrapersonal and interpersonal relationships has already been documented in the literature, reflecting the diversity of the problems faced by individuals confronted with the diagnosis of infertility and the physical and emotional strains of infertility treatments (Brkovich and Fisher, 1998; Daar and Merali, 2002).
Parenthood continuous to constitute an important life project for most women and men, and involuntary childlessness is a major life issue associated with strong psychological consequences. Furthermore, in some settings, infertile individuals, particularly women, are often stigmatized and isolated, and may experience diverse societal problems (Greil, 1997; Brkovich and Fisher, 1998; van Balen and Inhorn, 2002; Ombelet et al., 2008a; Inhorn, 2009; van Balen and Bos, 2009; Dhont et al., 2011).
In addition to the abovementioned challenges, in many developing countries infertile couples with limited resources are confronted with yet another challenge – that of gaining access to infertility services (Van Balen et al., 1996; Makuch et al., 2010, 2011). According to estimates from the World Health Organization (WHO) 180 million people around the world are affected by infertility problems (Rutstein and Iqbal, 2004). In developing countries, infertility is estimated to affect 9% of cohabiting couples and the demand for infertility treatment is estimated at 56% (World Health Organization, 1991; Boivin et al., 2007). Delay in gaining access to the diagnosis of infertility, to infertility services and to services that offer assisted reproductive technologies (ARTs) may negatively affect the possibility and the success of treatment for subfertile couples.
In Brazil, the federal constitution guarantees healthcare as a right for all citizens, and it is mandatory for the state to provide all health-related expenditures within the national health system, which is referred to as the SUS (Sistema Único de Saúde - Unified Health System) (Brasil, 1988, 2005). Despite the significant economic progress made by this country and its present position within the international scenario, inequalities persist between the higher and lower social classes in Brazil. Nevertheless, it has to be taken into account that significant progress has been made in improving and increasing the services covered by the SUS in its 20 years of existence (Viana and Machado, 2008).
Major efforts have been made to achieve reproductive health (RH) goals; however, these efforts have focused on reducing maternal mortality and morbidity, providing universal access to antenatal and obstetric care and family planning. However, there remains a wide gap between available reproductive healthcare, particularly obstetrical and gynaecological care, and access to specialized infertility services involving high-complexity procedures, including ARTs.
The current situation in Brazil
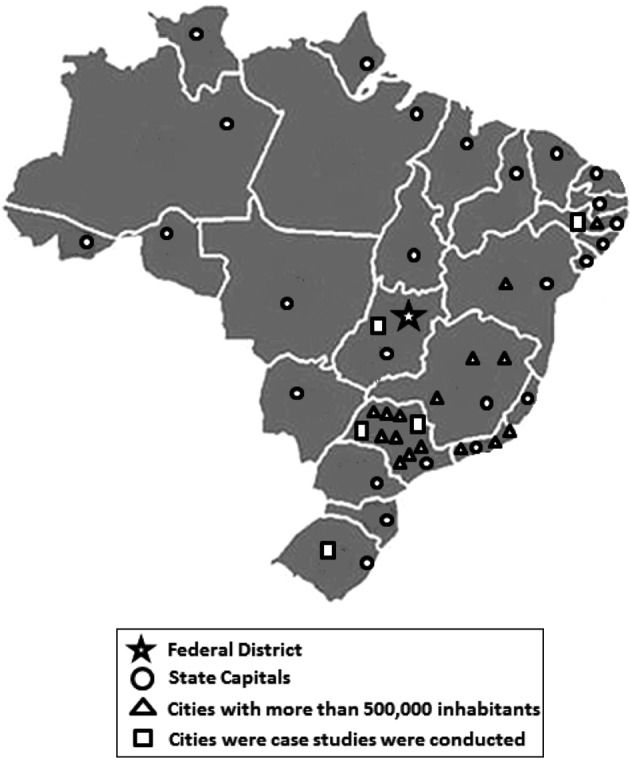
A recent nationwide study, anchored on quantitative and qualitative methods, was conducted in Brazil (Makuch et al., 2010, 2011). This is the third report based on the results of this study. The main objective of this report was to identify barriers that hamper access to infertility care and to ART procedures within the public health services. The first stage of the study was based on a cross-sectional approach. Health authorities in all the 26 State Health Departments and the Department of Health of the Federal District, the 26 Municipal Health Departments in the capital cities of each state and another 16 cities with more than 500,000 inhabitants were contacted. Interviews were scheduled with the Director of the Women’s Health Division or another designated person. In addition, 23 medical directors of referral centres for infertility services and 12 directors of university infertility services offering ART procedures, indicated by the state and municipal health authorities, were contacted for interviews. Based on the results of the first stage, qualitative case studies were conducted in five ART centres located in four of the five regions of the country (one region did not have any ART centres either partially or totally covered by the SUS). Health professionals and patients who had already undergone ART procedures or were waiting to initiate procedures in these centres were interviewed (Fig. 1).
Fig. 1. Brazilian map with indication of the place of interviews conducted.
It should be taken into account that of the total Brazilian population of 193 million, 140 million (72.5%) depend on the public sector healthcare system provided by the SUS (Santos et al., 2008; IBGE, 2011). Considering that there are almost 48 million women of reproductive age (15-49 years of age) in Brazil and around 5 million infertile couples (Santos et al., 2008; IBGE, 2012), it is reasonable to assume that almost 3.6 million infertile women depend on the public healthcare system for infertility care. The above figures show the magnitude of the problem, which is not habitually discussed by governmental authorities, and highlight the importance of improving women and men’s access to services that offer diagnosis and treatment of infertility, including ART procedures.
Main barriers identified
A total of 64 out of 69 (92.7%) health authorities at the state and municipal level were interviewed. Additionally, interviews were conducted with 26 out of the 35 directors of the infertility referral centres identified by the health authorities, including those that had been identified as centres offering government-funded ART procedures.
Health authorities at both the state and municipal levels, 76% and 66.7% respectively, reported that no infertility services were available and that the public health administration had no future political commitment to provide these services. Also, 83% of the interviewed health authorities reported that no ART services were available within the SUS in their administrative region. The most common reason reported for the lack of these procedures within infertility services, both at the state and municipal levels, was lack of political decision to implement them, followed by lack of resources and lack of trained professionals. Furthermore, other important reasons given by the health authorities identified in the interviews for the inexistence of infertility services were “no services were interested in implementing ART” and “the issue had not been discussed by the Health Secretariat”. Likewise, 75% of the authorities reported no plans to implement either infertility services or ART procedures in the 12 months following the interview. Both state and municipal authorities reported that infertile couples, including those who required ART procedures, were referred to centres specializing in women’s healthcare or to university hospitals that are partners with the SUS in health service agreements (Table I).
Table I. Barriers identified in the interviews with health authorities at the state and municipal levels.
| State | Municipal | |
| Existence of infertility services | ||
| Yes | 8 | 16 |
| No | 17 | 23 |
| Total | 25 | 39 |
| Reasons for not having infertility services | ||
| Lack of political decision | 13 | 10 |
| Lack of resources | 9 | 3 |
| No healthcare facilities interested in implementing them | 4 | 6 |
| Issue not discussed by Health Department | 4 | 6 |
| There is no protocol | 3 | 2 |
| There is no demand | 2 | 3 |
| No plans to implement services in the next 12 months | 17 | 35 |
| Total | 17 | 23 |
The five infertility services visited during the study that offered ART procedures had been set up at the initiative of healthcare professionals interested in implementing services to offer high-complexity infertility treatments. To implement and maintain ART procedures as a component of the treatment offered to infertile couples, these professionals had articulated already existing resources within their institutions such as physical space, technical capacity, equipment, laboratory facilities and personnel dedicated to infertility care whose salaries were paid by their institution. Only one of the services, situated within a public hospital in the most developed region of the country, offered ART procedures completely free of charge to patients. The other four services that offered ARTs were located within public university teaching hospitals through agreements formed with the SUS healthcare system.
The healthcare professionals and the patients interviewed in this study reported that access to infertility services performing ART procedures was limited. Two patterns of access to these services were identified; one was through the SUS referral system, which involves an initial consultation at a primary healthcare unit in order to obtain a referral to a more complex infertility service, while the other route of access consisted of a consultation directly with the ART service. However, the number of couples with an ART referral, who finally have access to these procedures, is restricted due to the low number of procedures performed by these services.
According to the patients and the health professionals of the services visited, scheduling a consultation at an ART centre gave infertile couples access to the initial diagnostic routine. After completing this diagnostic phase couples were able to schedule ART procedures. Those couples that needed additional treatments prior to undergoing ART procedures had an additional delay, principally if the procedure was to be performed at a public service. Patients sometimes had to wait for several months to be able to undergo these additional treatments within the public healthcare network.
These services that offered ARTs determined how many procedures they would perform per month. For example, in the centre in which ARTs were provided free of charge to patients, only 40 couples were scheduled per month. In general, the waiting time for ARTs varied from a few months to up to five years. The healthcare professionals recognized that there was a huge unmet demand; however, they were unable to calculate the magnitude of this demand since they only have contact with those patients who actually managed to gain access to their service.
Another barrier that hampered access to ART procedures was cost. With the exception of one service (subsidized by the government), at all the other centres patients were required to pay for the drugs used for ovarian hyperstimulation. The cost of these drugs is calculated at US$2,000 per cycle for IVF and/or ICSI procedures. Nevertheless, values as high as US$3,000 per cycle have been estimated in cases where additional costs such as anaesthesia, disposables and fees to cover general operating costs were required.
The professionals of the visited centres reported that some costs of ART procedures were performed under SUS coverage, in many cases using alternative diagnostic codes that were recognized by the system as other gynaecological conditions. This was done in the case of hormone measurement, ultrasound scans or ovum pick-ups, which could be performed using existing codes for other gynaecological complaints.
Despite the effort made by the four centres that were not subsidized by public health funds to reduce costs, the services were unable to offer ARTs free of charge to patients or at an accessible cost to the low-income segment of the population. Patients considered costs to be “very high” and one of the greatest impediments to accessing ART procedures. The professionals also reported knowing about low cost ART procedures and, furthermore, they recognized the need to implement simplified ART procedures in order to reduce costs for patients and for the service, and to improve access to more complex infertility treatment.
The interviewed professionals and patients suggested that the SUS should implement accessible infertility care in a greater number of public institutions or subsidize ART procedures in the institutions that are already offering these procedures in order to facilitate access. In addition, they stated that if more centres would be able to offer these kinds of treatments to infertile couples it would help to reduce the waiting time and waiting lists, and shorten time between screening and the initiation of the ART procedures.
Discussion
This is the third report originating from data of a nationwide study on access to infertility services and ART procedures conducted in Brazil (Makuch et al., 2010, 2011). To the best of our knowledge, this was the first study to be conducted in Brazil and is one of the largest to be conducted on these issues in a developing country. The survey focused on assessing the availability of infertility services within the public healthcare network, including the services that provide ART procedures, the access of patients to these services and the main barriers that hamper access such as the costs of the procedures, the waiting lists and the bureaucracy involved in gaining access to the service.
Brazil has a unique healthcare system in which the federal constitution guarantees that all health-related activities are covered by the state at no cost to patients. Brazil is a cosignatory of the United Nations International Conference of Population and Development (ICPD) and of the Oslo Declaration (United Nations, 1995; Oslo Ministerial Declaration, 2007). By signing these documents, as well as the other participating countries, Brazil recognizes that Reproductive Health (RH) is a human right and that RH care should include infertility care and treatment. Also by signing the Millennium Development Goals of the United Nations 2000, the country has included as one of its targets: “Achieve, by 2015, universal access to reproductive health” (United Nations, 2000).
In most developed and developing countries, parenthood continues to be an important issue in the life of the majority of the population, and in some developing countries infertile women are often stigmatized and are vulnerable to social and economical consequences (Daar and Merali, 2002; Dyer et al., 2002; Dyer, 2007). Access to the diagnosis and treatment of infertility, including ART procedures, contributes to assuring that the right of women and men to decide when they have children is guaranteed, and to enabling infertile couples to have at least one biologically related child (United Nations, 1995, 2000).
Most of the efforts made by Brazil to achieve its RH goals have been concentrated on increasing family planning services and access to contraceptive methods, and on reducing maternal morbidity and mortality (United Nations, 2008). Within this scenario, insufficient attention has been paid to infertility services and to improving the complexity of these services, including the implementation of ART procedures and guaranteeing access to these procedures as in many other settings (Ombelet et al., 2008b).
The present analysis identified and described different levels of barriers within the public sector that hamper the access of infertile couples to infertility care. The barriers described in this report were identified from interviews conducted with health authorities, healthcare providers and patients at ART centres within the public network. According to the information given by the health authorities interviewed for this study, the most important barriers that hamper access to infertility care were the lack of services and the lack of political decision to implement ART services, as well as the lack of resources allocated to infertility care, and no plans for implementing either infertility or ART services within the 12 months following the interviews. At this level, another barrier hampering the implementation of infertility care identified was the fact that in accordance with the norms of the SUS, infertility care was the responsibility of the primary healthcare services which are principally dedicated to primary healthcare. These services do not have the capacity to implement complex infertility care procedures, including at a diagnostic and therapeutic level (lack of technical capacity and trained professionals).
Making infertility services available in low-resource settings often represents a challenge. The nonexistence of these services can be justified by the fact that there are other urgent and life-threatening health problems to be dealt with, including maternal morbidity and mortality, vaccination, malaria, dengue, yellow fever and the arsenal of drugs required for people living with HIV and AIDS (Okonofua, 1996; Hamberger and Janson, 1997; Nachtigall, 2006). An additional factor is that infertility care, particularly complex technologies such as ART procedures, demands expensive equipment and trained professionals within a scenario of budget constraints.
The cost charged to patients for ART procedures in four of the five centres visited in this study was incompatible with the income of the majority of the population that depends on the public healthcare system. It must be taken into account that the cost of an ART procedure in the public system varies between US$2,000-3,000 per cycle compared to around US$6,000 per cycle in the private sector (Makuch et al., 2010; 2011). However, only 5.3% of the total population in Brazil earns the amount paid per IVF cycle as a monthly income (range 3.8 - 8.1%). While the country has improved its economical position within the world context with a per capita gross domestic product of US$12,917 (Global Property Guide, 2012), it is still estimated that 21% of the population is below the poverty line (Index Mundi, 2012).
Strategies used by the professionals at these centres to minimize the cost barrier of patients consisted of the use of hidden codes through which procedures used for ARTs were charged to the healthcare system, since the same procedures are also used to investigate other gynaecological complaints and are covered by the SUS. In this way, the final costs to patients were reduced (Jones and Allen, 2009). However, despite the strategies used to reduce costs, these services were unable to offer ARTs at no cost or at an affordable cost to lower income patients.
Although the professionals who participated in the present study reported being aware of the need to implement ART procedures at lower costs, to the best of our knowledge, no institutions have implemented procedures using low cost drugs for stimulating follicular development, which also results in a low rate of complications (Ombelet et al., 2008a; Aleyamma et al., 2011; The Low Cost IVF Foundation, 2012), and low cost laboratory procedures (Ombelet and Campo, 2007; Frydman and Ranoux, 2008).
The implantation of the above mentioned approaches represents an excellent opportunity to provide ART procedures within the public sector and to evaluate these new approaches. Additionally, it is worthwhile to note that even though some professionals interviewed in this study mentioned low cost approaches as a possible solution to the cost barrier none of them reported any action towards reducing the cost of infertility diagnosis such as one-day work-up procedures, a strategy that has been previously reported as being effective (Malpani and Malpani, 1992; Ombelet, 2011).
Another barrier identified was the long waiting time for the initial consultation, as well as for the ART procedure, which led to additional emotional suffering and in many cases, particularly in the case of older women, to a reduced possibility of success (Daar and Merali, 2002; Dyer et al., 2002).
To overcome the aforementioned barriers that hamper access to infertility care, health authorities should take into account the needs of the low-income population for the provision of safe and effective ARTs at the lowest cost. This action is not a simple task and cannot depend solely on a voluntary process implemented and maintained by professionals in some services. It should be based on the implementation of appropriate care capable of reducing inequity, avoiding the waste of available funds and improving results (Jones and Allen, 2009). In addition, clear policies and commitments are necessary in order to offer more affordable ART options (Blackwell et al., 2001).
The access to infertility treatments including ARTs in low-resource settings is a challenge and a human right (Ombelet et al., 2011). The fact that developing countries need to allocate restricted resources to life-threatening diseases and other non-life-threatening ailments does not justify the fact that infertility care remains a neglected public health issue. Infertility is still considered a misfortune with negative psychosocial repercussions (Daar and Merali, 2002; Dyer et al., 2002; Dyer, 2007) and in many settings it results in the stigmatization of individuals, principally women. Health authorities can no longer ignore that infertility is a legitimate medical problem.
Acknowledgments
This study was partially supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), grant number 07/00055-9 and the Conselho Nacional de Pesquisa (CNPq), Brazil, grant number 573747/2008-3.
References
- Aleyamma TK, Kamath MS, Muthukumar K, et al. Affordable ART: a different perspective. Hum Reprod. 2011;26:3312–3318. doi: 10.1093/humrep/der323. [DOI] [PubMed] [Google Scholar]
- Blackwell RE, Hammond KR, Steinkampf MP. A one year experience with a capitated health care plan for infertility. Fertil Steril. 2001;75:749–753. doi: 10.1016/s0015-0282(01)01673-9. [DOI] [PubMed] [Google Scholar]
- Boivin J, Bunting L, Collins JA, et al. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–1512. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- Brasil. Republica Federativa. Constituição Brasília Senado Federal. 1988 [Google Scholar]
- Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. . Área Técnica de Saúde da Mulher. Direitos sexuais e direitos reprodutivos: uma prioridade do governo. Brasília: Ministério da Saúde; 2005. [Google Scholar]
- Brkovich AM, Fisher WA. Psychological distress and infertility: Forty years of research. J Psychosom Obst Gyn. 1998;19:218–228. doi: 10.3109/01674829809025700. [DOI] [PubMed] [Google Scholar]
- Daar AS, Merali Z. Vayena E, Rowe PJ, Griffin PD (eds) Current Practices and Controversies in Assisted Reproduction. Geneva, Switzerland: World Health Organization; 2002. Infertility and social suffering: the case of ART in developing countries; pp. 15–21. [Google Scholar]
- Dhont N, van de Wijgert J, Coene G, et al. ‘Mama and papa nothing’: living with infertility among an urban population in Kigali, Rwanda. Hum Reprod. 2011;26:623–629. doi: 10.1093/humrep/deq373. [DOI] [PubMed] [Google Scholar]
- Dyer SJ, Abrahams N, Hoffman M, et al. ‘Men leave me as I cannot have children’: women’s experiences with involuntary childlessness. Hum Reprod. 2002;17:1663–1668. doi: 10.1093/humrep/17.6.1663. [DOI] [PubMed] [Google Scholar]
- Dyer SJ. The value of children in African countries: insights from studies on infertility. J Psychosom Obstet Gynaecol. 2007;28:69–77. doi: 10.1080/01674820701409959. [DOI] [PubMed] [Google Scholar]
- Frydman R, Ranoux C. INVO: a simple, low cost effective assisted reproductive technology. Hum Reprod. 2008;(ESHRE Monographs):85–89. [Google Scholar]
- Global Property Guide. http://www.globalpropertyguide. com/Latin-America/Brazil/gdp-per-capita 2012 [Google Scholar]
- Greil AL. Infertility and psychological distress: A critical review of the literature. Soc Sci Med. 1997;11:1506–1512. doi: 10.1016/s0277-9536(97)00102-0. [DOI] [PubMed] [Google Scholar]
- Hamberger L, Janson PO. Global importance of infertility and its treatment: role of fertility technologies. Int J Gynaecol Obstet. 1997;58:149–158. doi: 10.1016/s0020-7292(97)00286-5. [DOI] [PubMed] [Google Scholar]
- IBGE. http://www.ibge.gov.br/series_estatisticas/exibedados.php?idnivel=BR&idserie=POP327 2011 [Google Scholar]
- IBGE. http://www.ibge.gov.br/series_estatisticas/exibedados.php?idnivel=BR&idserie=POP3277 2012 [Google Scholar]
- Index Mundi. http://www.indexmundi.com/ brazil/percentage-of-population-below-national-poverty-line.html 2012 [Google Scholar]
- Inhorn MC. Right to assisted reproductive technology: overcoming infertility in low-resource countries. Int J Gynaecol Obstet. 2009;106:172–174. doi: 10.1016/j.ijgo.2009.03.034. [DOI] [PubMed] [Google Scholar]
- Jones HW, Jr, Allen BD. Strategies for designing an efficient insurance fertility benefit: a 21st century approach. Fertil Steril. 2009;91:2295–2297. doi: 10.1016/j.fertnstert.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Makuch MY, Petta CA, Osis MJ, et al. Low priority level for infertility services within the public health sector: a Brazilian case study. Hum Reprod. 2010;25:430–435. doi: 10.1093/humrep/dep405. [DOI] [PubMed] [Google Scholar]
- Makuch MY, Simônia de Padua K, Petta CA, et al. Inequitable access to assisted reproductive technology for the low-income Brazilian population: a qualitative study. Hum Reprod. 2011;26:2054–2060. doi: 10.1093/humrep/der158. [DOI] [PubMed] [Google Scholar]
- Malpani A, Malpani A. Simplifying assisted conception techniques to make them universally available – a view from India. Hum Reprod. 1992;7:49–50. doi: 10.1093/oxfordjournals.humrep.a137555. [DOI] [PubMed] [Google Scholar]
- Nachtigall RD. International disparities in access to infertility services. Fertil Steril. 2006;85:871–875. doi: 10.1016/j.fertnstert.2005.08.066. [DOI] [PubMed] [Google Scholar]
- Okonofua FE. The case against new reproductive technologies in developing countries. Br J Obstet Gynaecol. 1996;103:957–962. doi: 10.1111/j.1471-0528.1996.tb09542.x. [DOI] [PubMed] [Google Scholar]
- Ombelet W, Campo R. Affordable IVF for developing countries. Reprod Biomed Online. 2007;15:257–265. doi: 10.1016/s1472-6483(10)60337-9. [DOI] [PubMed] [Google Scholar]
- Ombelet W, Cooke I, Dyer S, et al. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14:605–621. doi: 10.1093/humupd/dmn042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ombelet W, Devroey P, Gianaroli L, et al. ESHRE Special Task Force on ‘Developing Countries and Infertility’. 2008;1(ESHRE Monogr):1–117. [Google Scholar]
- Ombelet W. Global access to infertility care in developing countries: a case of human rights, equity and social justice. FV&V in ObGyn. 2011;3:257–266. [PMC free article] [PubMed] [Google Scholar]
- Oslo Ministerial Declaration. Global health: a pressing foreign policy issue of our time. Lancet. 2007;369:1373–1378. doi: 10.1016/S0140-6736(07)60498-X. [DOI] [PubMed] [Google Scholar]
- Rutstein SO, Iqbal HS. DHS comparative Reports. WHO; 2004. Infecundity, infertility, and childlessness in developing countries. [Google Scholar]
- Santos IS, Ugá MAD, Porto SM. The public-private mix in the Brazilian Health System: financing, delivery and utilization of health services. Ciência e Saúde Coletiva. 2008;13:1431–1440. doi: 10.1590/s1413-81232008000500009. [DOI] [PubMed] [Google Scholar]
- The Low Cost IVF Foundation. http://www.lowcost-ivf.org 2012 [Google Scholar]
- United Nations. Report of the International Conference on Population and Development, Cairo, Egypt, 5-13 September 1994. New York: United Nations Population Fund; 1995. [Google Scholar]
- United Nations. The Millennium Development Goals. New York: United Nations; 2000. [Google Scholar]
- United Nations. World contraceptive use, 2007. USAID, Population Reference Bureau. World Population Data Sheet. 2008 [Google Scholar]
- Van Balen F, Kemper T, Verdurmen J. Perception of diagnosis and openness of patients about infertility. Patient Educ Counsel. 1996;28:247–252. doi: 10.1016/0738-3991(95)00852-7. [DOI] [PubMed] [Google Scholar]
- Van Balen F, Inhorn MC. nhorn MC and Van Balen F (eds). Infertility around the globe, new thinking on childlessness, gender and reproductive technologies. Berkeley, Los Angeles, London: UCLA-press; 2002. Interpreting infertility a view from the social sciences; pp. 3–32. [Google Scholar]
- Van Balen F, Bos HMW. The social and cultural consequences of being childless in poor-resources areas. FV&V in ObGyn. 2009;1:106–121. [PMC free article] [PubMed] [Google Scholar]
- Viana ALA, Machado CV. Vol. 18. Rio de Janeiro: Physis – Revista de Saúde Coletiva; 2008. Health Care Security: 20 years of the Unified Health System; pp. 645–684. [Google Scholar]
- World Health Organization. Geneva: Division of family health, World Health Organization; 1991. Infertility: a tabulation of available data on prevalence of primary and secondary infertility. Geneva programme on maternal and child health and family planning. [Google Scholar]


