Abstract
Quality control, training and education in gynaecological surgery are challenged and urgent measures are emerging. The implementation of a structured and validated program for training and quality control seems the most urgent measurement to be taken. The European Academy of Gynaecological Surgery has made a first attempt to do so. Through a practical and theoretical tests system, the skills of an individual surgeon is measured and the conditions to enter the different level of expertise are clearly defined. This certification system based on the best possible level of scientific evidence provides a first practical tool, universally implementable for a decent quality control and structured training program in Gynaecological laparoscopic surgery.
Keywords: Laparoscopy, training, certification, psychomotor skills, education
Introduction
It is unacceptable that the level of care a patient receives would depend on the luck to meet a surgeon with appropriate training in laparoscopic surgery.
Although laparoscopy provides a major improvement of the surgical possibilities and patients comfort, its implementation in gynaecological practice seems to be complex and limited by a variety of factors. Moreover there is vast evidence that the unconditional broad implementation of laparoscopic surgery might be related to an increased patient’s morbidity and mortality (van der Wal, 2007). It seems appropriate, although not yet implemented that, in addition to the surgical skills required for open surgery (manual dexterity and the knowledge of anatomy, pathology and surgical techniques) the laparoscopic surgeon/assistant has proficiency in specific practical skills like the ability of depth appreciation on a two-dimensional screen, camera navigation, hand-eye coordination, handling long instruments from a fixed position and the knowledge of an endoscopic operation room (OR) functioning.
The laparoscopic challenges are significant, like the vision which today is still on a 2D screen, displaying only a representation of the reality challenging the decision making process for the surgeon. Although the laparoscope provides the surgeons a fantastic field of vision it makes him/her also vulnerable and dependent of the skills of the camera navigator. Navigating the camera needs training and laparoscopic surgery demands team work.
That is why, besides the mandatory surgical training, laparoscopic surgery imposes a specific training taking into account that Laparoscopic Psychomotor Skills (LPS) are different from surgical skills.
LPS are skills similar to those required for computer gaming and should be learned and acquired outside the OR on specific and validated training models.
Surgical skills demand a complex educational system with always the need for a one-to-one teaching program in the OR. Surgical skills depend on the theoretical knowledge (anatomy, diseases, etc.) and the practical ability that includes basic sequences like dissection, haemostasis and section, and emergent actions that are realised by the additive synergy of the basic sequences. It is common to say that surgery is 75% cerebral and 25% technical skills, but for laparoscopic surgery this sentence becomes true only after the acquisition of the LPS. The proven improvement of our patient care by using the laparoscope makes it unacceptable that some experienced surgeons without any LPS continue to expose their patient to inadequate laparoscopic surgery as some young laparoscopic surgeons with excellent LPS but limited surgical knowledge and experience are dangerous because they will carry out incomplete surgical actions. This dangerous situation demands an urgent implementation of a structured and validated training and certification program in gynaecological laparoscopic surgery.
Defining the current problem
The efficient implementation of laparoscopy in daily practice is challenged by several critical factors. On one side the exposure to laparoscopic interventions is limited in most teaching hospitals, and on the other side laparoscopy has long learning curves. The classical apprentice-trainer teaching model only seems not very recommendable and teaching hospitals today do not provide the possibility of dry lab training within their facilities. In addition to that, the most important drawback to deal with the problem is the lack of universally accepted and validated system for training and certification.
Excessive long learning curves in the conventional apprentice-tutor model and limited amount of laparoscopic interventions in the teaching hospitals
Historically, the apprentice-trainer model has been used for years as the paradigm for training in surgery. In this model the apprentice first observes, then assists and finally operates under guidance in the OR. Achieving proficiency in both general surgical skills and specific LPS through this model seems ethically unacceptable, because the increased operating time and the higher complication rate. Another drawback of the classical apprentice tutor model is the need of a sufficient number of skilled trainers and the long learning curves reported in laparoscopic surgical training. (large amount of procedures needed to achieve proficiency) (Ascher-Walsh & Capes, 2007; Ghomi et al., 2007).
It is clear that this model only is insufficient and training in laparoscopic surgery needs to be supplemented with a structured pre operation room training program. This issue is especially relevant for gynaecological surgery because the trainees are exposed to fewer and fewer surgical cases in their daily practice. Indeed, in most teaching hospitals it is difficult for a trainee/surgeon to achieve the necessary quantity of laparoscopic procedures (between 40 and 100) to obtain sufficient technical competence (Targarona et al., 2010). This is supported by a literature review that reveals that only 12% of the hysterectomies for benign diseases are performed by laparoscopy (Wu et al., 2007), and by a recent report of the Dutch Ministry of Health that found an unacceptable amount of serious complications in laparoscopic procedures that were damaging patients’ health and costing the community a lot of money (van der Wal, 2007).
Absence of dry labs for LPS training and limited accessibility of specific laparoscopic learning programs
A large variety of inanimate models including trainer boxes and virtual reality models have been developed for training in laparoscopic surgery (Katz, 2006; Undre & Darzi, 2007). In contrast to animal models, these inanimate models have the advantage of allowing for longer training periods, which is crucial to ensuring full LPS acquisition and not only exposure to specific laparoscopic tasks. Both trainer boxes and virtual reality models allow for relaxed and controlled training, and learning curves for different laparoscopic tasks have been reported (Fraser et al., 2005; Vossen et al., 1997; Larsen et al., 2006). Trainer boxes are relatively cheap and accessible (Katz, 2006), whereas virtual reality models provide an objective evaluation of the learning process (Gor et al., 2003), with both being equally effective for acquiring laparoscopic skills (Munz et al., 2004). However, most of these models are not validated and are not used in a standardised way. Moreover, they are not universally available in dedicated dry labs.
Absence of a universal accepted validated system of certification
In spite of the promising data available about evaluation and training of laparoscopic skills (Brunner et al., 2004; Korndorffer et al., 2005), validated and well-structured programs including the pre-clinical training are not universally implemented. Furthermore, due to the variety of strategies and regulations for training in gynaecological laparoscopy there is not a validated system for skills’ certification.
A GLOBAL TRAINING AND CERTIFICATION PROGRAM IN GYNAECOLOGICAL LAPAROSCOPIC SURGERY
The European Academy for Gynaecological Surgery (+he Academy) has elaborated in collaboration with L’Institut de Recherechecontre les Cancers de l’Appareil Digestief (IRCAD) a global program of training and certification in gynaecological laparoscopy taking into account the current necessities, the feasibilities and the existing scientific evidence.
This program has the support and recognition of the European Society for Gynaecological Endoscopy (ESGE), its cooperating member societies and the Standing Committee for Training and Assessment of the European Board of Obstetricians and Gynaecologists (SCTA – EBCOG).
Acquiring the theoretical knowledge
The Virtual University of WeBSurg at the IRCAD in Strasbourg, France, provides free access to a broad e-learning platform covering all surgical disciplines with tutorials on techniques, pathology, experts’ opinions, debates and over 500 surgical videos (http://www.websurg.com). This program provides a direct solution to all individuals who are seeking for information and surgical training and cannot receive it at their local institutions. For trainees in gynaecology a special program is elaborated for learning and training in gynaecological laparoscopic surgery.
The tutorials are divided in the following three different levels of difficulties:
• The laparoscopic basic level provides tutorials to understand the anatomy from a laparoscopic point of view, the ways of entry, technique of exposure, rules of laparoscopic surgery, basic instrumentation and organisation of an endoscopic operation room.
• The laparoscopic gynaecological surgeon level tutorials are concentrating specifically on the ESGE level 2 and 3 surgeries like laparoscopic hysterectomy and myomectomy (Molinas et al., 2008).
• The laparoscopic gynaecological pelvic surgeon level deals with tutorials focusing not only on gynaecological surgery but also on urological, colorectal and vascular surgical procedures
Acquiring the practical basic and advanced laparoscopic psychomotor skills
There is an urgent need of a universally recognized and structured practical training program in laparoscopic surgery with different levels of difficulties and validated tests to guide the individual from one level of expertise to the second and third. Furthermore, the training modalities should be easily accessible and affordable in such a way that the basic training and progression can be accessed at local institutions and is not depending from skilled or expert laparoscopic surgeons or courses.
+he Academy has recently developed a trainer box called “The Laparoscopic Skills Testing and Training model” (LASTT) aimed to train and measure three specific LPS: laparoscopic camera navigation, hand-eye coordination and bimanual coordination (Figure 1).
Fig. 1. Training box for laparoscopic surgery with the LASTT wooden model.

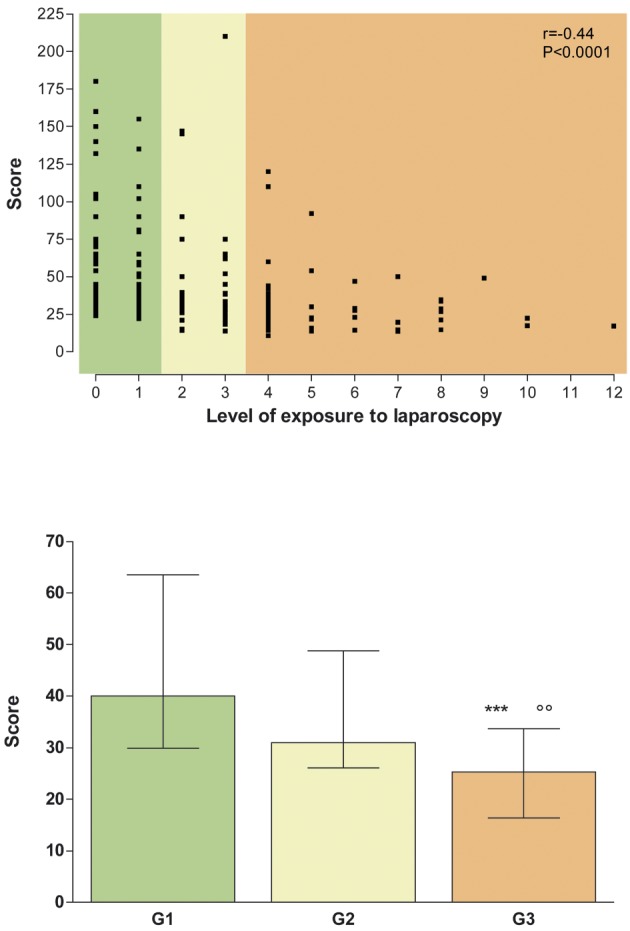
This model was proven to be feasible and its face validity (the realism of the model) and construct validity (the capacity of the model to differentiate between surgeons with different levels of experience) were demonstrated (Molinas et al., 2008; Campo et al., 2010) (Figure 2).
Fig. 2. Construct validity of Bimanual Coordination in the LASTT model. The ability to grasp six pre-defined objects with the dominant hand and re-grasp and transport them with the non-dominant hand to pre-defined targets in the LASTT model was evaluated. Higher scores represent bad performance. The upper graph shows the scores of the participants in function to their exposure to laparoscopic surgery. The lower graph shows the median (interquartile range) scores of the three groups. Group 1 (G1, green): no or little exposure to laparoscopy. Group 2 (G2, yellow): intermediate exposure to laparoscopy. Group 3 (G3, yellow): important exposure to laparoscopy. ***P < 0.001 (G1 vs. G3); °°P < 0.01 (G2 vs. G3). Reproduced with permission from Gynecol Surg 2008; 5(4):281-290.
Supplementary to this model +he Academy has developed a model to train and test more complex and fine LPS: The Suturing and knot tying Training and Testing model (SUTT) (Figure 3).
Fig. 3. The Suturing and knot tying Training and Testing model (SUTT).

The latest development of +he Academy is the E-Knot, a new home trainer to train specifically on the challenging skills of laparoscopic suturing and knot tying. The trainer box is equipped with a video camera which can be connected to a portable computer and with a comprehensive DVD tutorial (Figure 4) so the student can train at home all aspects of laparoscopic suturing and knot tying.
Fig. 4. “E-Knot “. The easy home trainer.
The data gathered so far by the Academy confirm that training improves laparoscopic skills and indicates that many repetitions are required for reaching proficiency. Because prior full acquisition of basic LPS facilitates the acquisition of more advanced skills, the evidence strongly suggest that an individual should start training basic LPS for both the dominant and the non-dominant hand, and only when proficiency is achieved s/he should continue with training for more advanced tasks, such as laparoscopic suturing and knotting (Molinas & Campo, 2010). Investment in training to acquire full proficiency in both basic and advanced LPS certainly is recommended prior to enter the one-to-one training in the OR; moreover because those skills remain for longer periods, as we have observed over a period of 18-24 month (unpublished observations). It seems that we are dealing with skills like biking, piano playing or gaming: once you know how to do it, you keep the ability.
Assessing theoretical knowledge and practical skills
For testing practical laparoscopic skills we are currently using the LASTT and the SUTT models. The LAST+T and SUT+T are standardized methods to test basic and advanced LPS, respectively and are trademarks of +he Academy.
The face and construct validity of the SUT+T method are still under evaluation, but today we already have sufficient individuals tested to be able to provide a bench mark data base for individual scoring.
To train and test the theoretical knowledge we are in the process of establishing a website with the tutorials and a theoretical test system that in analogy to the LAST+T and SUT+T will represent a specific method to differentiate the trainees in one of the three levels of expertise. This method will use the trade name TEST+T.
• The LAST+T method uses the LASTT model to measure three basic LPS.
The first exercise measures the ability of a person to navigate the camera and to handle the 30° optic, 14 targets have to be identified in a precise order. The second exercise measures the hand eye coordination by positioning 6 small rings over a nail and the last exercise measures the bimanual coordination by transporting 6 objects from one hand to the other and then in a corresponding hole. Test proficiency should guarantee the perfect laparoscopic instrument handling capabilities.
• The SUT+T method uses the SUTT model to test advanced LPS (i.e., laparoscopic stitching and intra-corporeal knot tying). The test consists out of four stitching exercises in which the individual is tested to position the needle correctly through a well-defined location, and one intra corporeal knot in which the individual has to perform a correct flat knot with two locking sequences. Test proficiency should guarantee the sufficient skills for laparoscopic suturing and intra corporeal knotting.
• The TEST+T method uses 50 multiple choice questions to test an individual on his/hers knowledge about laparoscopic anatomy, basic surgical principles, laparoscopic instrumentation, OR organization and functioning, recognition and management of complications. Exam proficiency should guarantee the sufficient theoretical knowledge to enter into the OR to assist or perform laparoscopic surgery.
On line scoring platform
+he Academy has developed an online scoring platform to register participants’ data and test results in a central database. For each participant the previous exposure to gynaecological laparoscopy is registered and documented according to the previously published scoring system (Campo et al., 2010). At the time of data analysis, participants are classified either as no or very little exposure to laparoscopy, limited exposure to laparoscopy or important exposure to laparoscopy (final score ≥ 4). The central data base provides an online calculation of the results and an appreciation of the skills of the participant with a colour code system similar to the traffic lights colour code. The green code indicates an excellent level of proficiency, similar to the very experienced laparoscopist. The yellow code indicates fair skills. The red code indicates that there is still a lot of room for improvement.
All tested individuals with an exposure score to laparoscopy equal or higher than 6 are used as reference values to calculate the group allocation. The green code is assigned to results within 2 SD of the reference values, the yellow code is assigned to results between 2 and 4 SD, whereas the red code is assigned to results over 4 SD.
The benchmark data base is continuously supplied with test results of the first test of an individual and saved in relation to its score of exposure to laparoscopy at the time of the test procedure. Follow up or second test do not enter the benchmark data base. As such, this data base is unique, dynamic and cut off values can change over the time.
For the LAST+T this online scoring engine is already in practical use in different teaching centres with a high satisfaction rate. A major advantage is that it provides automatically the mentors and mentees the results and group allocation. Information on the position of the individual in his/her group of experience is also given. For the SUT+T and TEST+T we follow the same philosophy and the establishment of the reference values is in process.
CERTIFICATION
After performing the practical and theoretical exam the participant will receive an overall score giving the possibility to receive +he Academy Card Certification. The aim is that any institution with training and/or a fellowship program uses the card system as entry criteria to improve the effect of their teaching programs. According to the results obtained on the LAST+T, SUT+T and TEST+T the participant will receive one of the 3 cards seen as a “license for different in OR training programs”.
Whereas the score on the different tests performed uses the traffic light codes, we decided for the certification cards to use a neutral and different set of colours mainly because the colour should not reflect any negative allocation to one of the tree certified skill levels.
• Bronze card
– Basic theoretical knowledge and LPS
– Score: LAST+T and TEST+T at least yellow code, SUT+T indifferent
– Access to in OR training as an observer or for ESGE class 1 surgeries
• Silver Card
– Excellent theoretical knowledge and basic LPS
– Score: LAST+T , TEST+T and SUT+T at least yellow code
– Access to in OR surgical training for ESGE class 1 - 3 surgeries
• Gold Card
– Excellent theoretical knowledge and LPS
– Score: LAST+T, SUT+T and TEST+T green code
– Access to in OR training for ESGE class 1-4 surgeries
Discussion
The current education methods for training in gynaecological surgery are being challenged by different forces and influences, such as the boundaries of traditional apprentices-trainer model, the ethical objectives to limit patient morbidity and the error rate during laparoscopic surgical procedures and the continuous pressure on the cost effectiveness of procedures.
The increased incidence of serious (lethal) complications in common laparoscopic procedures within general surgery and gynaecology has given lead to major investigations by the Dutch Ministry of Health.
Training in laparoscopic techniques was found to be variable and inadequately structured. It was expressed as a matter of concern that the standards, which a future laparoscopist must meet in order to operate, either independently or under supervision, have not been adequately established. Seen those challenges, it becomes without saying that a structured training program in gynaecological laparoscopic surgery is necessary and should be established with objective measurable levels of competencies.
+he Academy has defined the skills which can be learned outside the OR and which do not need the presence of an expert laparoscopist for the evaluation. The established test method uses objective parameters, it provides access to an online scoring platform and is affordable, and therefore it can easily be implemented in each teaching institution.
There is scientific evidence that large exposure to laparoscopic surgery correlates with proficiency in instrument handling (Campo et al., 2010). Technical skills, like instrument handling and laparoscopic intra-corporeal suturing, are only acquired by specific training and surgeons who receive psychomotor skill training show significantly greater improvement in performance in the OR (Grantcharov et al., 2004). Currently, in vitro training in a simple pelvic-trainer seems the most appropriate method to acquire the technical skills. The online scoring platform and the simple objective scoring system make this methodology accessible for every institution responsible for training trainees. Furthermore, those laparoscopic technical skills last over long periods and can be compared with skills like piano playing or biking. It seems then logic and obvious, but not yet implemented, that each training centre should put an in vitro training station at the disposal of their trainees and implement a qualification program.
+he Academy certification card system provides and defines the individual capacity to comply with theoretical and practical skills in different levels of expertise and is the prerequisite to enter different levels of training programs.
Especially the introduction of the card system as a license for OR activity could be a major step forward in the quality control of our clinical teaching programs in laparoscopic surgery.
Defining minimal standards with objective testing systems will increase patient safety and increase the quality of a one-to-one clinical training program in laparoscopic procedures.
We are performing a study to evaluate to what extent this is relevant and to assess the predictive validity of the LASTT and SUTT models for live animal surgery. Preliminary data confirm the predictive validity of the proper training in the LASTT and SUTT models (unpublished observations), because trainees who followed a complete and structured training program for LPS are performing much better than those who did not follow this training. It is still too early to elucidate which specific psychomotor task is more relevant and more important. In addition to answer these questions, the study will also define the relevance of training with or without trainers, which is crucial not only for educational but also for administrative purposes. Furthermore, all these data will allow us to evaluate learning curves in order to define the minimum training recommended to reach the plateau and to be able to organize the duration of training according to the program to be followed. Nevertheless, the predictive validity for real human surgery still has to be evaluated in a proper study.
Conclusions
Training in laparoscopic surgery is a real challenge. The actual pressure surrounding the surgical practice imposes evidently a validated quality control program. This control starts by a standardization of the surgical training. The European Academy succeeded to elaborate a program of training and certification dealing with both the theoretical knowledge on instrumentation, OR organisation, anatomy and complication management, and the practical laparoscopic psychomotor skills, including suturing and knot tying skills.
It remains without doubt that this is only the first but an important step in a professional training program in laparoscopic gynaecological surgery but it certainly helps to answer the question:
“Are you good enough to offer your patient the laparoscopic approach for her surgery?”
References
- Walsh CJ, Capes T. An evaluation of the resident learning curve in performing laparoscopic supracervical hysterectomies as compared with patient outcome: five-year experience. J Minim Invasive Gynecol. 2007;14:719–723. doi: 10.1016/j.jmig.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Brunner WC, Korndorffer JR, Jr. , Sierra R. Determining standards for laparoscopic proficiency using virtual reality. Am Surg. 2005;71:29–35. doi: 10.1177/000313480507100105. [DOI] [PubMed] [Google Scholar]
- Brunner WC, Korndorffer JR, Jr. , Sierra R. Laparoscopic virtual reality training: are 30 repetitions enough? J Surg Res. 2004;122:150–156. doi: 10.1016/j.jss.2004.08.006. [DOI] [PubMed] [Google Scholar]
- Campo R, Reising C, Van Belle Y. A valid model for testing and training laparoscopic psychomotor skills. Gynecol Surg. 2010;7:133–141. [Google Scholar]
- Fraser SA, Feldman LS, Stanbridge D. Characterizing the learning curve for a basic laparoscopic drill. Surg Endosc. 2005;19:1572–1578. doi: 10.1007/s00464-005-0150-5. [DOI] [PubMed] [Google Scholar]
- Ghomi A, Littman P, Prasad A. Assessing the learning curve for laparoscopic supracervical hysterectomy. 11. 2007:190–194. [PMC free article] [PubMed] [Google Scholar]
- Gor M, McCloy R, Stone R, Smith A. Virtual reality laparoscopic simulator for assessment in gynaecology. BJOG. 2003;110:181–187. [PubMed] [Google Scholar]
- Grantcharov TP, Kristiansen VB, Bendix J. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91:146–150. doi: 10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- Katz R. Methods of training using pelvic trainers. Curr Urol Rep. 2006;7:100–106. doi: 10.1007/s11934-006-0067-0. [DOI] [PubMed] [Google Scholar]
- Korndorffer JR Jr., Scott DJ, Sierra R. Developing and testing competency levels for laparoscopic skills training. Arch Surg. 2005;140:80–84. doi: 10.1001/archsurg.140.1.80. [DOI] [PubMed] [Google Scholar]
- Larsen CR, Grantcharov T, Aggarwal R. Objective assessment of gynecologic laparoscopic skills using the LapSimGyn virtual reality simulator. Surg Endosc. 2006;20:1460–1466. doi: 10.1007/s00464-005-0745-x. [DOI] [PubMed] [Google Scholar]
- Molinas CR, Campo R. Defining a structurated training program for acquiring basic and advanced laparoscopic psychomotor skills in a simulator. Gynecol Surg. 2010;7:427–435. [Google Scholar]
- Molinas CR, De Win G, Ritter O. Feasibility and construct validity of a novel laparoscopic testing and training model. Gynecol Surg. 2008;5:281–290. [Google Scholar]
- Munz Y, Kumar BD, Moorthy K. Laparoscopic virtual reality and box trainers: is one superior to the other? Surg Endosc. 2004;18:485–494. doi: 10.1007/s00464-003-9043-7. [DOI] [PubMed] [Google Scholar]
- Targarona EM, Salvador Sanchis JL, Conde S. Advanced training in laparoscopic surgery: what is the best model? Cir Esp. 2010;87:1–3. doi: 10.1016/j.ciresp.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Undre S, Darzi A. Laparoscopy simulators. J Endourol. 2007;21:274–279. doi: 10.1089/end.2007.9980. [DOI] [PubMed] [Google Scholar]
- van der Wal G. Den Haag, the Netherlands: Prof. Dr. G. van der Wal; 2007. Risico’s minimaal invasieve chirurgie onderschat. [Google Scholar]
- Vossen C, Van BP, Shaw RW. Effect of training on endoscopic intracorporeal knot tying. Hum Reprod. 1997;12:2658–2663. doi: 10.1093/humrep/12.12.2658. [DOI] [PubMed] [Google Scholar]
- Wu JM, Wechter ME, Geller EJ. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–1095. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]