Abstract
Primary chronic osteomyelitis of the jaw is an uncommon non-suppurative, chronic inflammatory disease of unknown origin. It can manifest as early or adult onset and is characterised by lack of pus formation, fistula or bony sequestra formation. A 28-year-old woman presented with swelling on the left side of her mandible. On the basis of clinical, radiological and histological findings, primary chronic osteomyelitis was diagnosed. Surgical decortication and contouring of the affected bone was performed and no signs of recurrence were seen at 2-year follow-up. Hence we emphasise the importance of decortication over peripheral or segmental resection of the jaw for the treatment of primary chronic osteomyelitis since this procedure is less aggressive and more functionally and aesthetically acceptable.
Background
Osteomyelitis is defined as an inflammatory condition of the bone that begins as an infection of the medullary cavity, rapidly spreads to the Haversian systems, and eventually involves the periosteum of the infected areas.1 Primary chronic osteomyelitis (PCO) is a rare but well-known, non-suppurative inflammatory disease of unknown aetiology. Marx and Mercuri defined acute osteomyelitis as lasting for less than 4 weeks and chronic osteomyelitis as lasting for more than 4 weeks.2
PCO exclusively affects the mandible with no special age preference.3 Clinical features range from restricted mouth opening and regional lymphadenopathy to decreased inferior alveolar nerve sensation (Vincent's symptom). The absence of pus, intra- or extra-oral fistula, or sequestration strictly characterises PCO and differentiates primary from acute and secondary chronic osteomyelitis. Sometimes PCO may be associated with chronic recurrent multifocal osteomyelitis and SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis) syndrome.4
Marx in his radiological study showed a mixed radiodensity in the early stages of PCO followed by only sclerotic changes in the later stages.5 In the early stages, mixed radiodensity is suggestive of areas of sclerosis and osteolysis with varying degrees of periosteal reactions. Immununological investigation shows only mild to moderate elevation of C-reactive protein, erythrocyte sedimentation rate and lymphocyte count.6 Histopathological features include the presence of pagetoid bone formation, lymphocytes, plasma cells (suggestive of chronic inflammation) and varying amounts of medullary fibrosis.7 8
We treated PCO of the mandible by decortication of the bone. Although surgical treatment alone cannot guarantee an absolute cure, decortication with removal of necrotic tissue in the early stages is proposed and has a good prognosis.9–11
Case presentation
A 28-year-old woman reported to the department with complaints of recurring episodes of swelling in the left lower jaw (figure 1), intermittent mild pain in the entire left side and paresthaesia of the left lower lip for 1 month. She was apparently asymptomatic 3 years previously when she noticed a small diffuse swelling on the left side of her lower jaw. The swelling had recurred intermittently over the last 3 years. She had no history of trauma, infection or systemic disease. She had undergone drug therapy many times for her complaint but with little benefit. On clinical examination, a firm, hard, diffuse and mildly tender swelling extending from angle of the mouth to the angle of the mandible on the left side was noticed. On intra-oral examination, the buccal cortical plate was increased in size from the left mandibular canine to the second molar region and the buccal vestibule was obliterated. There were no signs of infection, periodontitis or caries.
Figure 1.

Mild extra-oral swelling on the left side of the face.
Investigations
Cone beam CT (CBCT) scans of the region involved revealed a mixed pattern with partial loss of normal bone structure along with sclerosis and subperiosteal bone formation suggestive of chronic osteomyelitis. A large expansion of the mandibular body and periosteal apposition was evident on CBCT (figures 2 and 3).
Figure 2.
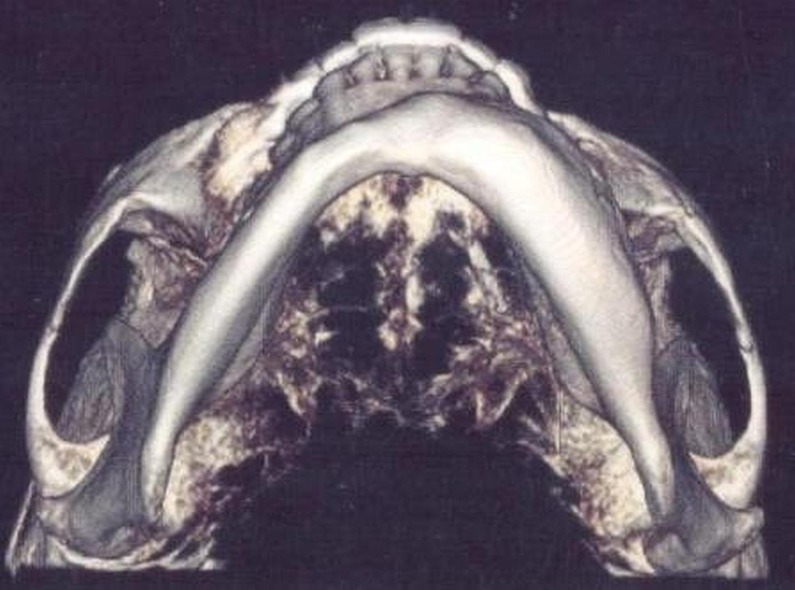
Pre-operative three-dimensional CT scan showing a large increase in the size of the mandible.
Figure 3.
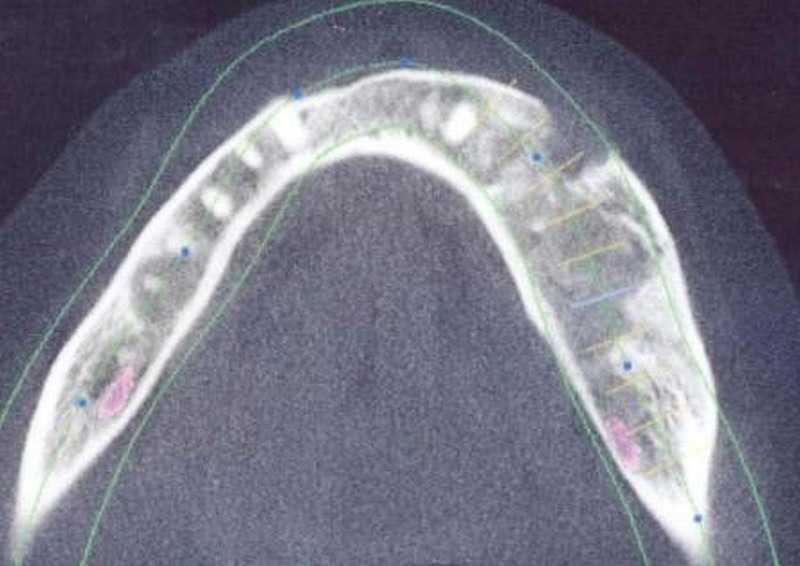
CT scan showing a mixed pattern with absence of any sequestrate.
Blood investigation revealed a raised erythrocyte sedimentation rate. Incisional biopsy was carried out and histopathological finding revealed various stages of chronic inflammation, lymphocytosis and some areas of subperiosteal bone formation.
Differential diagnosis
PCO was diagnosed on the basis of mandibular involvement, the hard swelling, the absence of pus and extra- or intra-oral fistula, the insidious course and the full complement of teeth without any caries or pathology, or any other intra-oral foci of infection. Benign tumours such as ossifying and non-ossifying fibroma, and fibrous dysplasia were ruled out by clinical, radiological and histopathological evaluation.
Treatment
Surgical management was planned and bone decortication was carried out from the left mandibular premolar to the second molar area with extraction of the first and second molars due to poor bone support in the region (figure 4). The patient was prescribed antibiotics and attended regular follow-up visits.
Figure 4.

Intra-operative photograph showing decortication with preservation of the mental nerve.
Outcome and follow-up
The patient was asymptomatic 2 years after surgery and a CBCT scan (figure 5) revealed mild areas of radiolucency and reparative bone formation below the premolar area and comparative normal dense bone in the molar region, suggestive of incomplete bone healing although clinically there was no sign of disease.
Figure 5.
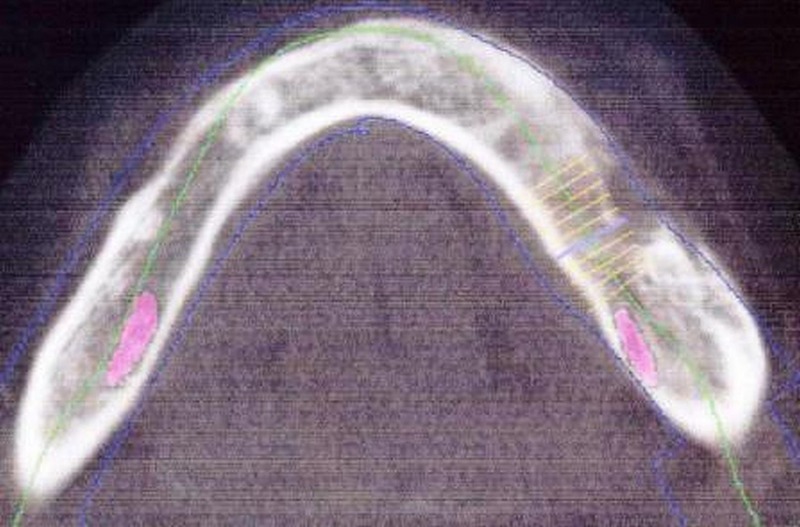
Cone beam CT scan 2 years after surgery demonstrating regression of the pathology.
Discussion
PCO of the jaws is a complex clinical entity which presents both a diagnostic and a therapeutic challenge, especially in young patients. The Zurich classification system subdivides PCO into adult onset, early onset (depending upon age at presentation) and syndrome associated. It is characterised as a strictly non-suppurative chronic inflammation of the jaw bones with the absence of pus formation, extra- or intra-oral fistula, or sequestration. The absence of these symptoms clearly differentiates primary from acute and secondary chronic osteomyelitis in most cases. Our case perfectly fits into the early onset subcategory of PCO. Mandibular involvement, a hard swelling, the absence of pus and extra- or intra-oral fistula, the insidious course and full complement of teeth without any caries or pathology, or any other intra-oral foci of infection strongly suggested PCO. Benign tumours such as ossifying and non-ossifying fibroma, and fibrous dysplasia were ruled out by clinical, radiological and histopathological evaluation.
Both orthopantomogram and CBCT showed mixed radiodensity in the early stages followed by only sclerotic changes in the later stages. Immununological investigation revealed only mild to moderate elevation of C-reactive protein, erythrocyte sedimentation rate and lymphocyte count, which was similar to the findings of the study by Erich.12 On histopathological examination, variable amounts of chronic inflammatory cells were seen with numerous lymphocytes and absence of sequestrum. Surgical treatment in conjunction with antibiotics and non-steroid anti-inflammatory drugs is beneficial and considerably improves the patient's quality of life.13 In our case, intra-oral decortication was carried out, antibiotics were prescribed and the patient was called for routine follow-up examinations. The patient was completely relieved of symptoms and had no complaint after 2 years of follow-up. We recommend that surgical decortication and empirical antibiotic therapy should be considered as the treatment of choice as compared to antibiotics alone or peripheral/segmental osteotomy. Patients should be followed up as recurrence is common.
Learning points.
Surgical decortication and empirical antibiotic therapy should be considered as the treatment of choice for primary chronic osteomyelitis since this is less aggressive and more functionally and aesthetically acceptable.
Following decortications, implants can be used for the rehabilitation of patients.
Patients should be followed up as recurrence is common.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Prasad KC, Prasad SC, Mouli N, et al. Osteomyelitis in the head and neck. Acta Otolaryngol 2007;127:194–205 [DOI] [PubMed] [Google Scholar]
- 2.Mercuri LG. Acute osteomyelitis of the jaw. Oral Maxillofac Surg Clin North Am 1991;3:355–65 [Google Scholar]
- 3.Eisenbud L, Miller J, Roberts IL. Garré's proliferative periostitis occurring simultaneously in four quadrants of the jaws. Oral Surg Oral Med Oral Pathol 1981;51:172–8 [DOI] [PubMed] [Google Scholar]
- 4.Baltensperger M, Gratz K, Bruder E, et al. Is primary chronic osteomyelitis a uniform disease? Proposal of a classification based on a retrospective analysis of patients treated in the past 30 years. J Craniomaxillofac Surg 2004;32:43–50 [DOI] [PubMed] [Google Scholar]
- 5.Marx RE. Chronic osteomyelitis of the jaws. Oral Maxillofac Clin North Am 1991;3:367–81 [Google Scholar]
- 6.Chamot AM, Kahn MF. Das Sapho-syndrome. Z Rheumatol 1994;53:234–42 [PubMed] [Google Scholar]
- 7.Malmström M, Fyhrquist F, Kosunen TU, et al. Immunological features of patients with chronic sclerosing osteomyelitis of the mandible. Int J Oral Surg 1983;12:6–13 [DOI] [PubMed] [Google Scholar]
- 8.Van Merkesteyn JP, Groot RH, Bras J, et al. Diffuse sclerosing osteomyelitis of the mandible: clinical radiographic and histologic findings in twenty-seven patients. J Oral Maxillofac Surg 1988;46:825–9 [DOI] [PubMed] [Google Scholar]
- 9.Farnam J, Griffin JE, Schow CE, et al. Recurrent diffuse sclerosing osteomyelitis involving the mandible. Oral Surg 1984;57:374–8 [DOI] [PubMed] [Google Scholar]
- 10.Suei Y, Tanimoto K, Taguchi A, et al. Possible identity of diffuse sclerosing osteomyelitis and chronic recurrent multifocal osteomyelitis: one entity or two. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:401–8 [DOI] [PubMed] [Google Scholar]
- 11.Suei Y, Tanimoto K, Taguchi A, et al. Chronic recurrent multifocal osteomyelitis involving the mandible. Oral Surg Oral Med Oral Pathol 1994;78:156–62 [DOI] [PubMed] [Google Scholar]
- 12.Kuhn E, Wu J, Karl J, et al. Quantification of C-reactive protein in the serum of patients with rheumatoid arthritis using multiple reaction monitoring mass spectrometry and 13C-labeled peptide standards. Proteomics 2004;4:1175–86 [DOI] [PubMed] [Google Scholar]
- 13.Theologie-Lygidakis N, Schoinohoriti O, Iatrou I. Surgical management of primary chronic osteomyelitis of the jaws in children: a prospective analysis of five cases and review of the literature. Oral Maxillofac Surg 2011;15:41–50 [DOI] [PubMed] [Google Scholar]


