Abstract
Brain metastases occur in up to 10–30% of patients with cancer. Metastatic lesions are usually diagnosed as multiple mass lesions at the junction of the grey and white matter with associated perilesional vasogenic oedema. Cysticercosis is an endemic disease in underdeveloped countries of Africa, Central and South America and is the most common parasitic infection of the central nervous system. The classical radiological finding of neurocysticercosis is cystic lesions showing the scolex in the brain parenchyma. We report a case of metastatic adenocarcinoma of the lung presenting with cystic brain lesions mimicking neurocysticercosis.
Background
Brain metastases occur in up to 10–30% of patients with cancer.1 Lung cancer is the most common cause of brain metastasis followed by melanoma and renal cell carcinoma. Contrast-enhanced MRI is the preferred method of diagnosis of brain metastasis. It is the most sensitive imaging modality to detect metastatic lesions from lung tumours.2 3 Metastatic lesions are usually diagnosed as multiple mass lesions at the junction of the grey and white matter with associated perilesional vasogenic oedema.4
Cysticercosis is an endemic disease in underdeveloped countries of Africa, Central and South America and is the most common parasitic infection of the central nervous system.5 6 The classical radiological finding of neurocysticercosis is cystic lesions showing the scolex in the brain parenchyma.7 There are rare reports of brain metastasis presenting as cystic lesions which may mimic neurocysticercosis.8–10
We report a case of metastatic adenocarcinoma of the lung presenting with cystic brain lesions mimicking neurocysticercosis.
Case presentation
A 61-year-old woman, non-smoker who was in her usual state of health presented at an outside institution with new onset generalised tonic–clonic seizure. MRI of the brain showed multiple cystic lesions. No chest imaging was performed at the outside facility. She received an 8-day course of albendazole 1400 mg daily along with dexamethasone for probable neurocysticercosis based on imaging findings and its high prevalence in northeast Brazil.
She presented to the emergency room at our institution with subjective dyspnoea, malaise and new neurological symptoms 4 weeks after initial diagnosis of brain cystic lesions and 2 weeks after completion of albendazole treatment at outside facility. No headache, vomiting, visual disturbances were reported on arrival.
On physical examination, her vital signs including respiratory rate were stable. She was found to have right haemiparesis and gait abnormalities. Distal right lower extremity showed right foot drop (strength 3/5) which had been getting progressively worse after completion of albendazole treatment. The patient was alert, attentive, oriented to place, person and time. The lungs were clear to auscultation. The heart rhythm was regular. No cyanosis or clubbing was appreciated on lower extremities. There was no appreciable lymphadenopathy in the cervical, supraclavicular, infraclavicular, inguinal and axillary areas. The abdomen was soft without visceromegaly.
Investigations
Another MRI of the brain was performed showing multiple cystic brain lesions with associated perilesional enhancement (figure 1).
Figure 1.
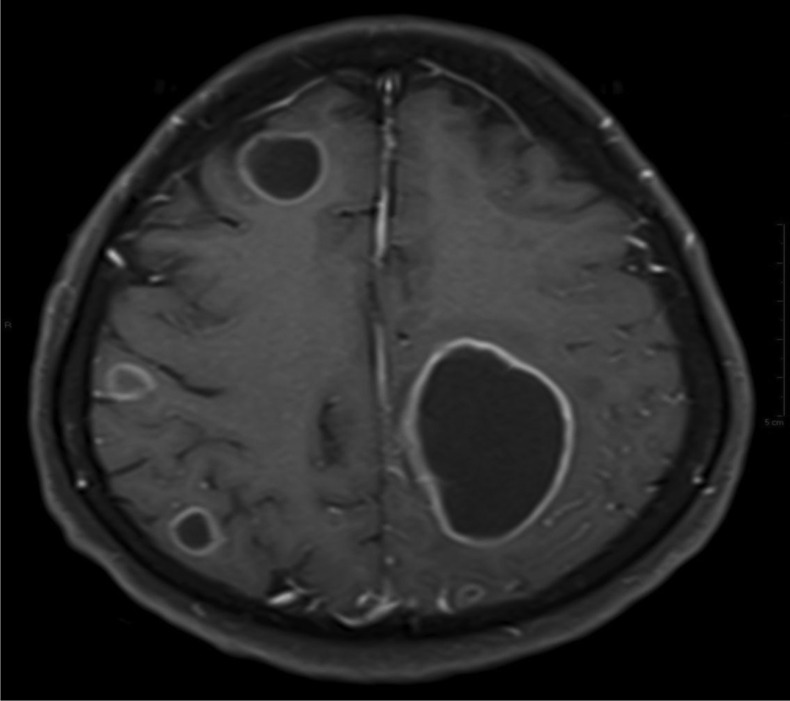
MRI showing multiple brain cystic lesions with associated perilesional enhancement.
A chest X-ray showed spiculated opacities at the right parihilar and upper lobe areas (figure 2). A CT of the chest showed right and left superior lobe-spiculated lesions measuring 3.6×3 cm and 2×1.7 cm, respectively, and paratracheal lymphadenopathy (figure 3).
Figure 2.
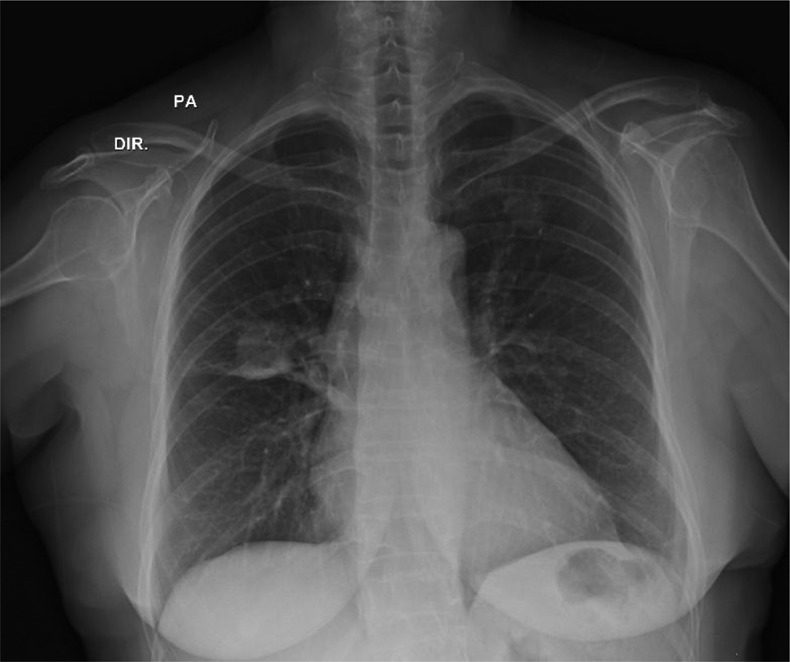
Chest X-ray showing bilateral lung and right parahilar mass. DIR, right side; PA, posteroanterior.
Figure 3.
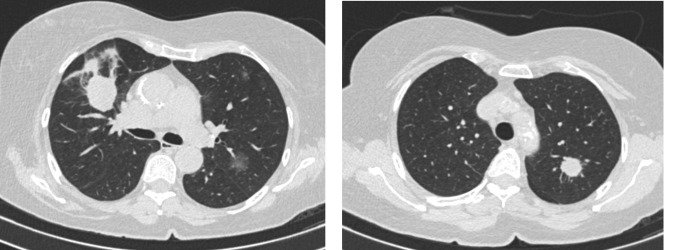
Chest CT showing bilateral lung masses.
In the light of lack of clinical improvement of neurological symptoms and the presence of lung lesions, the patient underwent a left parietal cystic brain lesion resection. Pathological analysis revealed a poorly differentiated adenocarcinoma. Subsequent immunohistochemical evaluation was positive for cytokeratin 40, 48, 50, 5/6 AEA, thyroid transcription factor 1, napsin suggestive of lung primary (figure 4).
Figure 4.
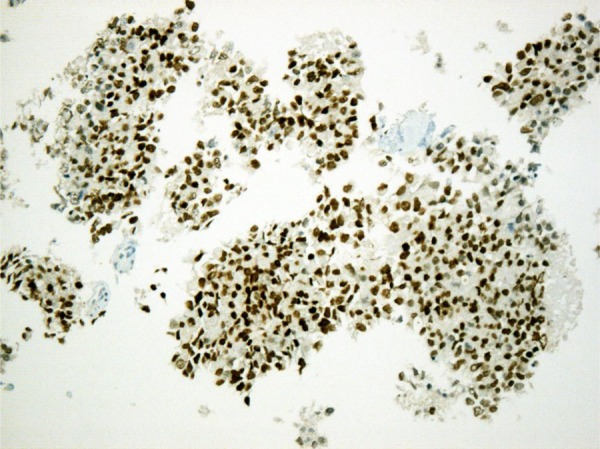
Immunohistochemistry staining of adenocarcinoma involving the brain showing strong expression of thyroid transcription factor 1.
Differential diagnosis
After lack of improvement on albendazole, other entities presenting as cystic brain mass lesions including primary or metastatic brain tumours, tuberculomas, pyogenic brain abscesses and mycotic granulomas were considered as part of the differential diagnoses. The development of respiratory symptoms prompted chest imaging. After results, we decided to pursue tissue biopsy to confirm our suspicion of metastatic lung carcinoma. The other diagnoses seemed less likely to us.
Treatment
The patient started systemic chemotherapy with carboplatin area under the curve (AUC) 5 and paclitaxel 150 mg/m2 every 21 days after surgical recovery. Her brain metastases are being closely observed while on systemic treatment.
Outcome and follow-up
The patient has been tolerating treatment well with stable disease on follow-up MRI of the brain performed after two cycles of systemic chemotherapy.
Discussion
There are very few reports of lung cancer presenting with metastatic cystic brain lesions.10–12 Neurocysticercosis is the most common parasitic infection of the central nervous system. Imaging studies along with serological testing are the basis for diagnosis of neurocysticercosis when biopsy is not indicated.7 In endemic areas, cystic brain metastasis can be misdiagnosed for neurocysticercosis, even when in the presence of seropositive markers.13 For those in other areas of the globe, brain metastases would have been considered at the time of initial imaging. However, this patient did meet the criteria for probable neurocysticersosis in that geographical region. In an area of limited resources, the initial course of action was appropriate. The lack of improvement led to further evaluation, diagnosis and definitive treatment. In retrospect, the patient could have undergone a less invasive diagnostic procedure such as lung biopsy for tissue diagnosis.
In summary, physicians as well radiologists, especially those practicing in endemic areas for cysticercosis, should be aware of the rare presentation of cystic brain metastasis of lung tumours.
Learning points.
Cystic lesions are an uncommon presentation of brain metastases of lung adenocarcinoma.
Treatment with antiparasitics is a reasonable first step for patients with definite or probable neurocysticercosis.
Other causes for brain cystic lesions should be investigated in case of initial treatment failure in areas where cysticercosis is endemic.
Lung cancer should always be considered as a possible diagnosis in patients with brain lesions given its high prevalence.
Footnotes
Contributors: All the authors were involved in the conception and design of the manuscript, acquisition and interpretation of the data, drafting the article or revising it critically for important intellectual content. All the authors gave final approval of the version published.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Johnson JD, Young B. Demographics of brain metastasis. Neurosurg Clin N Am 1996;7:337–44 [PubMed] [Google Scholar]
- 2.Yokoi K, Kamiya N, Matsuguma H, et al. Detection of brain metastasis in potentially operable non-small cell lung cancer: a comparison of CT and MRI. Chest 1999;115:714–19 [DOI] [PubMed] [Google Scholar]
- 3.Davis PC, Hudgins PA, Peterman SB, et al. Diagnosis of cerebral metastases: double-dose delayed CT vs contrast-enhanced MR imaging. AJNR Am J Neuroradiol 1991;12:293–300 [PMC free article] [PubMed] [Google Scholar]
- 4.Strugar J, Rothbart D, Harrington W, et al. Vascular permeability factor in brain metastases: correlation with vasogenic brain edema and tumor angiogenesis. J Neurosurg 1994;81:560–6 [DOI] [PubMed] [Google Scholar]
- 5.Willingham AL, III, Engels D. Control of Taenia solium cysticercosis/taeniosis. Adv Parasitol 2006;61:509–66 [DOI] [PubMed] [Google Scholar]
- 6.Montano SM, Villaran MV, Ylquimiche L, et al. Neurocysticercosis: association between seizures, serology, and brain CT in rural Peru. Neurology 2005; 65:229–33 [DOI] [PubMed] [Google Scholar]
- 7.Del Brutto OH, Rajshekhar V, White AC, Jret al. Proposed diagnostic criteria for neurocysticercosis. Neurology 2001;57:177–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Troiani C, Lopes CC, Scardovelli CA, et al. Cystic brain metastases radiologically simulating neurocysticercosis. Sao Paulo Med J 2011;129:352–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surov A, Hainz M, Kornhuber M. Multiple cystic metastases in the brain from adenocarcinoma of the lung. Am J Med 2009;122:e3–4 [DOI] [PubMed] [Google Scholar]
- 10.Mota PC, Reis C, Pires NF, et al. Lung cancer: atypical brain metastases mimicking neurocysticercosis. Int J Clin Oncol 2011;16:746–50 [DOI] [PubMed] [Google Scholar]
- 11.Choi HJ, Choi SK. Multiple cystic brain metastases from adenocarcinoma mimicking cysticercosis. Case report. Clin Neuroradiol 2012;22:105–7 [DOI] [PubMed] [Google Scholar]
- 12.De Shields MS, Ruether J. Lung carcinoma presenting as multiple cystic lesions in the brain. Del Med J 1998;70:77–80 [PubMed] [Google Scholar]
- 13.Coulibaly B, Gautier G, Fuentes S, et al. [Degenerating neurocysticercosis cysts: differential diagnosis with cerebral metastasis]. Rev Neurol 2008;164:948–52 [DOI] [PubMed] [Google Scholar]


