Abstract
Pseudotumours are rare, occurring in 1–2% of severe haemophiliacs. Osseous locations are far less frequent than soft tissue location. We report a case of a 43-year-old man with haemophilia A, who presented with a gradually enlarging left thigh mass for 8 months. There were no constitutional symptoms. Plain radiograph showed an expansile lytic lesion with ‘soap-bubble’ appearance arising from the left femur diaphysis. On MRI, it appeared as a non-enhancing, multilobulated lesion expanding the medullary and subperiosteal spaces. The mass exhibited concentric ring sign with heterogeneous intermediate signal intensity in the core lesion, reflective of chronic haematoma with blood degradation products of different stages. A diagnosis of haemophilic pseudotumour was made. Hypercalcaemia, however, raised a diagnostic dilemma as bone malignancy needed to be considered. An open excisional biopsy and subsequent amputation confirmed the diagnosis of osseous haemophilic pseudotumour. Nuclear medicine study later revealed a concurrent parathyroid adenoma.
Background
Pseudotumours are rare, occurring in 1–2% of severe haemophiliacs.1 By comparison, an osseous pseudotumour involving the femur is less common in a mild haemophiliac. The aim of this case report is to discuss the role of imaging in the radiological diagnosis of this uncommon entity and to review the radiographic and MRI features of osseous haemophilic pseudotumour.
Case presentation
We present a case of a 43-year-old Chinese man with underlying haemophilia A and who is under follow-up at the authors’ institution. He was diagnosed with haemophilia A at the age of 15 when he underwent screening as his brother developed haemarthrosis after a sports activity. He had three episodes of transfusions of factor VIII in total prior to current presentation. The first two episodes were for the left knee arthroscopies in 1989 and 1997; the former was due to a ligamentous injury in a badminton match the same year and the latter was due to reduced range of movement of the knee. The third episode was for a tongue bleed due to an accidental self-inflicted bite in 2010. He denied any history of spontaneous bleeding. Apart from that, he also had underlying β thalassaemia trait, hypertension, nephrolithiasis and was recently diagnosed with hepatitis C in 2010. He is a chronic smoker with no family history of malignancy.
He presented to the authors’ institution in early 2012 with an 8-month history of a gradually enlarging left thigh mass. He denied history of trauma or surgical procedure to the left thigh prior to the onset of swelling. It was associated with pain on weight-bearing for 2 months prior to presentation. However, the patient did not seek any medical advice nor was on any self-medication as the pain was bearable. Furthermore, he did not experience any constitutional symptoms such as fever, lethargy, poor appetite or loss of weight. There was no associated skin redness or discolouration over the thigh mass. A non-mobile bony mass measuring 20 cm× 12 cm was palpated. There was no calf tenderness bilaterally and the distal pulses were present. There was a full range of movement of both hip and right knee joints. There was, however, limited range of movement of about 10–30° in the left knee joint due to previous ligamentous injury. The rest of the systemic examination was unremarkable.
Investigations
His blood investigations showed mild hypochromic microcytic anaemia (haemoglobin 11.7 g/dL, mean cell volume 68 fL, mean cell haemoglobin 21 pg), normal international normalised ratio (0.98 ratio) and prolonged activated partial thromboplastin time (78.6 s). He had raised corrected calcium concentration of 2.91 (reference range 2.14–2.58) mmol/L but a normal phosphate level of 0.99 mmol/L. His renal function test was normal but the liver function test was deranged due to underlying hepatitis C (alanine aminotransferase 195 U/L, alkaline phosphatase 117 U/L, aspartate transaminase 118 U/L and γ-glutamyl transpeptidase 105 U/L). The serum albumin and total bilirubin levels were normal. Tumour markers were unremarkable.
Plain radiograph (figure 1) revealed an expansile lytic lesion with ‘soap-bubble’ appearance at the diaphysis of the left femur. Cortical thinning and endosteal scalloping were apparent in most parts of the lesion. Some parts of the cortex became imperceptible and interrupted. However, no aggressive periosteal reaction was noted. There were lobulated soft tissue swellings causing cortical erosion of the posterior distal femur. Secondary osteoarthritic changes of the left knee joint were apparent. The differential diagnoses at this point of time were haemophilic pseudotumour, aneurysmal bone cyst (ABC) and malignant bone tumour (in view of elevated serum calcium) in descending order.
Figure 1.

(A and B) Plain radiograph of the left femur shows an expansile multilobulated lytic lesion with ‘soap-bubble’ appearance at the diaphysis of the left femur. Cortical thinning and endosteal scalloping (black arrow) are apparent in most parts of the lesion. Some areas of the cortex are imperceptible and interrupted (white arrowhead). There are lobulated soft tissue swellings causing cortical erosion of the posterior distal femur (asterisk). Secondary osteoarthritis of the left knee is apparent.
An MRI of the left femur was performed (figures 2 and 3). On MRI, the lesion was multilobulated in appearance with involvement of the medullary and subperiosteal spaces. It exhibited heterogeneous intermediate signal intensity on T1-weighted and-T2 weighted images. The lobulated soft tissue mass at the posterior aspect of the distal third femur was attributed to a multilobulated subperiosteal component with extension to the intercondylar notch. The multilobulated lesion was outlined by the hypointense outer rim and hyperintense inner rim on T1-weighted and T2-weighted images, giving rise to concentric ring signs, signifying chronic haematomas. The hypointense outer rims in all sequences represented haemosiderin deposition in the wall. The heterogeneous signal intensity in the core lesion was reflective of the different stages of blood degradation products. The lesion did not show fluid–fluid level or enhancement. The imaging finding was consistent with haemophilic pseudotumour. Bone tumour and ABC were excluded.
Figure 2.

(A and B) MRI axial T1-weighted images show a multilobulated expansile mass with (A) intramedullary and (B) subperiosteal components. Most of the lobulations exhibit concentric ring signs which signify chronic haematomas. The concentric ring sign consists of a hypointense outer rim (white arrow) and hyperintense inner rim (black arrow). The core of the lesion shows heterogeneous intermediate signal intensity reflecting different stages of blood degradation products (asterisk).
Figure 3.
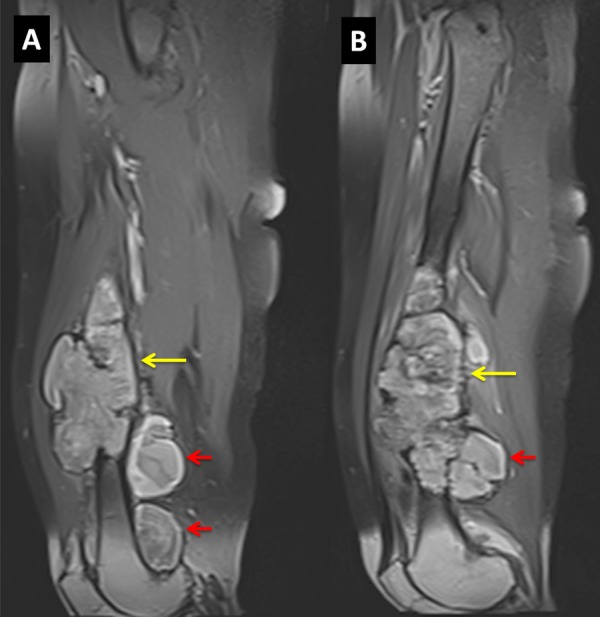
(A and B) MRI postgadolinium T1-weighted fat-saturated sequence on sagittal view shows a non-enhancing, multilobulated, expansile mass with intramedullary component (yellow arrows) in the diaphysis and subperiosteal component (red arrows) at the distal metaphysis.
At the same time, the patient was being investigated and conservatively managed for hypercalcaemia. He was hyperhydrated with 2.5 L of normal saline daily. Multiple myeloma was excluded in view of unremarkable findings in the skeletal survery, urine and serum electrophoresis. No lung lesion was detected on chest radiograph. Ultrasound of the abdomen showed no evidence of malignancy except for bilateral renal calculi. Finally, serum parathyroid hormone revealed hyperparathyroidism (10.4 pmol/L). A diagnosis of osseous haemophilic pseudotumour and concurrent primary hyperparthyroidism was made. However, in view of the risk of concurrent hyperparathyroidism with hypercalcaemia secondary to malignancy, a decision of an open biopsy of the left femur was made to exclude malignancy. Arrangements were made for factor VIII transfusion during the biopsy. The obtained histopathological specimen showed morphological features consisting of blood clot with foci of calcification. There was absence of fibrous capsule or bone trabeculae. No evidence of malignancy was detected.
Treatment
Subsequently, he was arranged for surgery to excise the distal femur as he was unable to walk or bear weight. Reconstruction of the distal femur was performed using a megaprosthesis. The histology of the lesion showed a collection of altered blood surrounded by an inflamed fibrous pseudocapsule. The pseudocapsule contained infiltrates of mild inflammatory cells. Again, there was no evidence of malignancy. The reactive new bone formation was present in the affected zone while the rest of the bone appeared unremarkable. The histopathology evaluation was concluded as a haematoma.
Outcome and follow-up
Postsurgery, the patient recovered well without immediate complications. He was on regular follow-up under the orthopaedic team, the gastroenterology team for antiviral treatment of hepatitis C and the endocrine team for hyperparathyroidism. A technetium-99m sestamibi parathyroid scintigraphy was performed and confirmed a diagnosis of right parathyroid adenoma (figure 4). Consequently, he was referred to the surgical team for excision of the parathyroid adenoma.
Figure 4.

Technetium-99m sestamibi parathyroid scintigraphy with single photon CT fusion images show a right inferior parathyroid adenoma posterior to the lower pole of the right thyroid gland.
Discussion
Haemophilia A is an X linked recessive hereditary disease characterised by clotting factor VIII deficiency and almost exclusively affects men. It results in prolonged bleeding after injury, tooth extraction or surgery.2 Spontaneous bleeding into joints, soft tissue and bones is a feature of severe haemophilia.2 Repetitive haemathrosis is the common presentation which results in haemophilic arthropathy.3 In contrast, intraosseous and subperiosteal bleeding are far less frequent.4 Inadequate resorption of extravasated blood in the extra-articular musculoskeletal system results in an encapsulated area of clotted blood and necrotic tissue.5 With successive haemorrhagic episodes, these lesions expand over time and form a pseudotumour.
Osseous pseudotumours most commonly affect the bones that are susceptible to trauma such as femur, pelvis, tibia and small bones of the hand in decreasing order of frequency.6 Pseudotumour in a mild haemophiliac is far less frequent. In the present case, the patient is a mild haemophiliac who does not have any episode of spontaneous bleeding. A definite episode of precipitating trauma could not be ascertained. However, it is likely that the patient had multiple episodes of minor trauma to the left femur for which he had no recollection. These occurrences had subsequently caused prolonged oozing and repetitive bleeding in the bone.
Osseous pseudotumours can occur in any portion of tubular and flat bones. On conventional radiography, intraosseous/intramedullary pseudotumour appears as a well-defined, unilocular or multilocular expansile lytic lesion of varying size. The lesion may lead to cortical thinning or thickening, endosteal scalloping and peripheral sclerosis.7 Conversely, a subperiosteal pseudotumour would cause pressure erosion to the cortex and give rise to subperiosteal new bone formation.4 It may extend into the adjacent soft tissue. Progressive expansion causes gradual bone loss and subsequently leads to deformity or pathological fracture, mimicking other benign or malignant tumours or infectious processes.7 The differential diagnoses include ABC, giant cell tumour (GCT), low-grade primary bone sarcoma, metastasis and osteomyelitis.8 In the present case, conventional radiography had depicted the combined imaging features of intraosseous and subperiosteal pseudotumour. The diaphyseal location of the bone lesion made the likelihood of ABC, GCT and osteomyelitis to be less likely in this case as these differential diagnoses are commonly centred at the metaphysis.
The appearance on MRI, however, is more specific with an expansile, multiseptated lesion and an invariably peripheral hypointense rim in all sequences representing haemosiderin deposition in the fibrous wall. The concentric ring sign is a feature of chronic haematoma demonstrating a hypointense outer rim and a hyperintense inner rim on T1-weighted image.9 The core of the pseudotumour displays heterogeneous intermediate signal intensity on both pulse sequences owing to the various stages of blood degradation products within. Fluid–fluid levels that were absent in the present case would have suggested acute haematomas.8 In addition, pseudotumours may have peripheral enhancement but are strictly without internal enhancement.
As imaging features of pseudotumours are characteristic and with the given history of haemophilia, radiologists should be aware of these lesions to avoid misinterpretations and unnecessary biopsies. Biopsy was probably best avoided, because of the high likelihood of complications, that is, bleeding, fistula and infection10 and the continued deterioration of the patient necessitating a limb amputation. Despite the aforementioned risk, an excision biopsy was performed in this patient owing to the slim possibility of bone neoplasm in view of concomitant hypercalcaemia.
The management of osseous pseudotumour would need to suit to each individual case.5 If the pseudotumour is relatively small, factor replacement therapy and immobilisation may be effective. Surgery, however, may be the only option in cases where the lesion is extensive. Amputation of the involved limb may even be necessary.11 12 The main concern associated with surgery is the risk of refractory haemorrhage. The availability of factor VIII, IX and activated prothrombin complex concentrates have now made surgery feasible. Recurrence, however, can occur in the surrounding tissues left behind after removal of the lesion.10
Primary hyperparathyroidism is the commonest cause of hypercalcaemia in outpatients.13 The mainstay of treatment for parathyroid adenoma is surgery.13 Parathyroidectomy is indicated in the presence of hypercalcaemia or when complications of hypercalcaemia such as renal calculi, osteoporosis and fractures occur.
Learning points.
Pseudotumours are a rare entity, seen in only 1–2% of severe haemophiliacs with intraosseous or subperiosteal locations occurring far less frequent than soft tissue location.
Pseudotumour is far less common in mild haemophilia; however, the diagnosis of haemophilic pseudotumour should remain a prime consideration.
On MRI, concentric ring signs on T1-weighted image and absence of internal enhancement on contrast study are highly characteristic of pseudotumours. Radiologists must be aware of these lesions to avoid misinterpretation and unnecessary biopsy.
The treatment of osseous pseudotumour need to suit to each individual case. Factor replacement therapy and immobilisation may be effective for a relatively small pseudotumour. Surgery may be the only option for a large lesion.
Footnotes
Contributors: All of the authors contributed in drafting, writing and revising the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ahlberg AK. On the natural history of hemophilic pseudotumour. J Bone Joint Surg Am 1975;57:1133–6 [PubMed] [Google Scholar]
- 2.Konkle BA, Josephson NC, Nakaya Fletcher SM, et al. Hemophilia A. GeneReviews 2000. http://www.ncbi.nlm.nih.gov/books/NBK1404/ (accessed 10 Dec 2013). [Google Scholar]
- 3.Geyskens W, Vanhoenacker FM, Van der Zijden T, et al. MR imaging of intra-osseous hemophilic pseudotumour: case report and review of literature. JBR-BTR 2004;87:289–93 [PubMed] [Google Scholar]
- 4.Jaganathan S, Gamanagatti S, Goyal A. Musculoskeletal manifestations of haemophilia: imaging features. Curr Probl Diagn Radiol 2011;40:191–7 [DOI] [PubMed] [Google Scholar]
- 5.Pakala A, Thomas J, Comp P. Hemophilic pseudotumour: a case report and review of literature. Int J Clin Med 2012;3:229–33 [Google Scholar]
- 6.Resnick D. Diagnosis of bone and joint disorders. 4th edn Philadelphia, PA: WB Saunders, 2002 [Google Scholar]
- 7.Park JS, Ryu KN. Hemophilic pseudotumour involving the musculoskeletal system: a spectrum of radiologic findings. AJR Am J Roentgenol 2004;183:55–61 [DOI] [PubMed] [Google Scholar]
- 8.Stafford JM, James TT, Allen AM, et al. Hemophilic pseudotumour: radiologic-pathologic correlation. Radiographics 2003;23:852–6 [DOI] [PubMed] [Google Scholar]
- 9.Hahn PF, Saini S, Stark DD, et al. Intraabdominal hematoma: the concentric-ring sign in MR imaging. AJR Am J Roentgenol 1987;148:115–19 [DOI] [PubMed] [Google Scholar]
- 10.Magallon M, Monteaguado J, Altisent C, et al. Hemophilic pseudotumour: multicentre experience over a 25-year period. Am J Hematol 1994;45: 103–8 [DOI] [PubMed] [Google Scholar]
- 11.Hermann G, Gilbert M. Case report 471. Hemophilic pseudotumours (presumptive diagnosis) and hemophilic arthropathy of elbow. Skeletal Radiol 1988;17:152–6 [DOI] [PubMed] [Google Scholar]
- 12.Gaary E, Gorlin JB, Jaramillo D. Pseudotumour and arthropathy in the knees of a haemophiliac. Skeletal Radiol 1996;25:85–7 [DOI] [PubMed] [Google Scholar]
- 13.Eigelberger MS, Cheah WK, Ituarte PH, et al. The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited? Ann Surg 2004;239:528–35 [DOI] [PMC free article] [PubMed] [Google Scholar]


