Abstract
Objectives. We tested hypotheses about the relationship between neighborhood-level food sources and obesity, controlling for individual-level characteristics.
Methods. Data (collected November 2006–April 2008) derived from a random-digit-dial sample of 5688 community-dwelling adults aged 50 to 74 years residing in 1644 census tracts in New Jersey. Using multilevel structural equation models, we created latent constructs representing density of fast-food establishments and storefronts (convenience stores, bars and pubs, grocery stores) and an observed indicator for supermarkets at the neighborhood level, simultaneously modeling obesity and demographic characteristics (age, gender, race, education, household income) at the individual level.
Results. When we controlled for individual-level age, gender, race, education, and household income, densities of fast-food establishments and storefronts were positively associated with obesity. Supermarkets were not associated with obesity.
Conclusions. Because people living in neighborhoods with a higher density of fast food and storefronts are more likely to be obese, these neighborhoods may be optimal sites for interventions.
Rates of obesity increased more than 100% between the 1970s and 2008.1 Although rates have leveled off since 2003and 2004,2 today more than a third of the US population is obese, and estimates indicate that by 2030 between 42% and 51% of the population will be obese.3 People aged 45 to 64 years are more likely to be obese than are those in any other age group.4 If obesity trends continue at their current rate, disability rates among persons aged 50 to 69 years are projected to increase by 1% per year through 2020.5 Because of the relationships between obesity, poor health, and high medical expenditures, obesity is a greater threat to public health than either smoking or drinking.6
Trends in obesity rates are most likely the result of changing environmental factors, including agriculture, food processing and marketing, transportation, and physical demands of work. Because the characteristics of the neighborhoods in which people live can make it easier for them to consume excessive calories and more difficult to expend those calories,7 it is likely that there is an association between obesity and the neighborhoods in which people live. Yet since most existing studies of the relationship between neighborhoods and obesity among older adults focus on the socioeconomic characteristics of neighborhoods8–14 rather than the neighborhood food environment, we lack understanding of how specific characteristics of the neighborhood food environment influence obesity.
The analyses that follow examine the extent to which the local food environment is related to obesity among older adults, controlling for individual characteristics with known associations to obesity, including age, gender, socioeconomic status, and race.
Evidence regarding the extent to which the neighborhood food environment is associated with obesity in the adult population is conflicting, with some studies showing a positive association15–19 and others finding that proximity to fast-food restaurants is not associated with body mass index (BMI).20–23 Similarly, although some studies found that proximity to supermarkets decreased the risk of obesity,18,19,21,24 others found that supermarkets were not associated with BMI.22,23
Although few studies have examined the effects of neighborhood environment and obesity on older people, Yen et al.25 suggest that obesity among older adults may be even more strongly influenced by neighborhood characteristics than is the case for school-aged children and younger adults. Like studies of adults in general, studies linking characteristics of neighborhood food environments and obesity in older people yield conflicting findings. Hanibuchi et al.26 found that better access to supermarkets, fast-food outlets, and convenience stores was positively associated with obesity among older people in Japan, whereas Morland et al.27 found that the presence of supermarkets was associated with a lower prevalence of obesity and that the presence of convenience stores was associated with a higher prevalence of obesity in a large community-dwelling sample of Americans.
Rundle et al.24 suggest that because density measures for food sources such as supermarkets, convenience stores, and fast-food restaurants are correlated with each other, their associations with obesity may be difficult to disentangle. Moreover, because not all studies examine these neighborhood food sources in tandem with one another, findings across studies are difficult to compare. Further adding to the complexity of this issue, most studies do not simultaneously adjust for the inherent nesting of people in neighborhoods and measurement error.
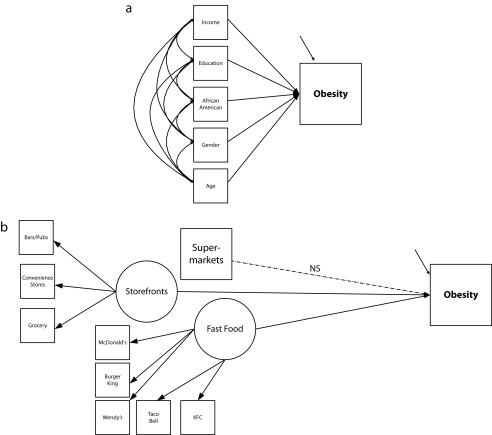
We investigated the relationship between obesity and the local food environment among older adults. We tested the following hypotheses depicted in Figure 1: (1) when age, gender, income, education, and race are controlled for, people living in neighborhoods with more fast-food restaurants and storefronts (small grocery stores, convenience stores, and bars) are more likely to be obese than people living in neighborhoods with fewer of these amenities; and (2) when these same individual-level variables are controlled for, people living in neighborhoods with greater availability of supermarkets will have lower rates of obesity than those living in neighborhoods where supermarkets are less prevalent.
FIGURE 1—
Multilevel structural equation models of individual-level obesity with (a) characteristics at the individual (within) level and (b) food sources at the neighborhood (between) level: Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life (ORANJ BOWL), 2006–2008.
Note. NS = not significant. The 2 arrows pointing to Obesity are indicators for the measurement error associated with the observed variable.
METHODS
Analyses built on data from 5688 people participating in the ORANJ BOWL panel (“Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life”) collected between November 2006 and April 2008. We identified participants by using random-digit-dialing procedures. Eligibility criteria included being between the ages of 50 and 74 years and living in New Jersey. We studied persons in this age range because their high rates of obesity put them at risk for heart disease, cancer, and diabetes. We excluded people unable to participate in a 1-hour English language telephone interview.
ORANJ BOWL staff recruited panel members by telephone cold calling with list-assisted random-digit-dialing procedures. The demographics of the targeted sample made coverage loss from cell phone–only households very small.28 Staff conducted screening interviews with persons aged 18 years and older to determine whether any eligible persons lived in the household. If screening indicated that 2 or more age-eligible persons lived in the household, we listed these people in a Kish table and chose one via computerized gender-weighted random algorithm to participate. No substitutions were permitted.
Of the 151 246 phone numbers in the population, 32 678 households completed the screen. To complete the sample, research staff made 1 060 838 calls, with an average of 7.01 calls made to each phone number. Using standard American Association for Public Opinion Research calculations, ORANJ BOWL achieved a response rate of 58.73% and a cooperation rate of 72.88%.
We linked interview data to administrative data that provided information about neighborhood characteristics. We were able to geocode 5572 of the respondents’ addresses, finding that ORANJ BOWL participants resided in 1644 of New Jersey’s 1912 census tracts. When we compared characteristics of our sample of tracts with census data representing all of New Jersey, we found that there were no significant differences on any variable included in our model, suggesting that our sample of tracts accurately represented the state of New Jersey.
Data Collected From ORANJ BOWL Respondents
Demographic characteristics collected included self-reports of age, gender (1 = male; 2 = female), education (9-point Likert scale; 1 = not high school graduate to 9 = doctoral degree), income (6-point Likert scale; 1 = less than $15 000 to 6 = more than $150 000), and race (African American = 1, not African American = 0). Respondents reported their height and weight, and we used these data to compute BMI (defined as weight in kilograms divided by the square of height in meters). We categorized people with BMIs greater than or equal to 30 as obese.
Neighborhood-Level Data
Information regarding the number of supermarkets, grocery stores, local convenience stores, and fast-food restaurants came from the New Jersey Department of Agriculture, Division of Marketing and Development. We obtained a list of the names of all 12 183 outlets with licenses to distribute milk in New Jersey in 2007 and, following Morland et al.,29 used a modification of the 2007 North America Industry Classification codes to categorize each establishment as a supermarket (large chain store), grocery store (bodega), chain convenience store, local convenience store, gasoline station with convenience store, warehouse club, fruit and vegetable market, pharmacy, full service restaurant, fast-food restaurant (these were further classified by name into groups corresponding to major chains; e.g., Burger King) or snack shop. Three coders established and maintained an interrater reliability of 0.85. We linked these data to the ORANJ BOWL data at the level of the census tract.
The number of bars and pubs in each tract was abstracted from the New Jersey Department of Law and Public Safety Division of Alcohol Beverage Control. We obtained a list of the names and addresses of 9261 establishments with alcohol retail licenses in 2007 and coded each establishment as either liquor store; restaurant; bar, pub, or tavern; motel or hotel; social club; or combination bar-grill and restaurant-bar. Coders established and maintained an interrater reliability of 0.85.
Analysis Plan
We computed bivariate correlations among the continuous variables in the analysis using Pearson R. For categorical data, the Spearman statistic is reported.
To test the hypotheses depicted in Figure 1, we used multilevel structural equation models (ML-SEM),30,31 analyzing the data with Mplus 5.21 (Mplus, Los Angeles, CA).32 ML-SEM are uniquely suited for analyzing both measurement and structural relationships among nested data.30,31,33–35 It leverages the strength of multilevel models to decompose variance at the between and within levels and permits explanation of that variance by within and between group predictors.30 The structural equation portion of the model affords an accurate representation of the latent construct by decomposing the variance attributable to the construct from that attributable to measurement error.36–39 It accounts for the clustering of data within neighborhoods that violate the assumption of independence of observations. The amount of dependence in the data is expressed as the intraclass correlation. Prior to model building, we assessed the intraclass correlation to examine the relative importance of neighborhood context to the factors included in the model.40
We developed 2 latent variables at the neighborhood level, one representing fast-food density and the other storefront density. The indicators for fast food were the number of each of 5 different major fast-food chains present in the tract. Indicators for storefronts41 included the number of bars, grocery stores, and convenience stores in the census tract. We operationalized supermarkets as an observed indicator on the basis of the number of supermarkets in each tract. At the individual level, we included income, education, age, race, and gender, variables having well-established relationships with obesity.23
At level 1 (individual level), we regressed obesity on income, education, race (African American), gender, and age. All exogenous variables were free to correlate with one another. At level 2, we regressed fast food, storefronts, and supermarkets on obesity. The model estimation returns the regression parameter values (β and γ) as log odds, which were converted to odds ratios for ease of interpretation. Details regarding the analysis may be found in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org).
RESULTS
The ORANJ BOWL sample included 2067 men and 3621 women whose mean age was 60.7 years (SD = 7.1). More than a third (32.1%) of the sample was obese (BMI ≥ 30.0). Demographic characteristics of the sample are reported in Table 1.
TABLE 1—
Demographic Characteristics of Study Population (n = 5688): Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life (ORANJ BOWL), 2006–2008
| Characteristic | % |
| Race | |
| White | 83.8 |
| African American | 11.8 |
| Asian | 1.6 |
| Other or mixed | 2.8 |
| Household income, $ | |
| < 30 000 | 19.1 |
| 30 000–80 000 | 39.8 |
| > 80 000 | 41.1 |
| Education | |
| < high school | 5.4 |
| High school | 28.3 |
| Some college | 15.0 |
| 2 y of college | 9.3 |
| 4 y of college | 19.5 |
| Some graduate school | 3.9 |
| Master’s degree | 13.1 |
| Some doctoral work | 1.3 |
| Professional degree | 4.2 |
| Current marital status | |
| Married | 56.7 |
| Widowed | 14.2 |
| Divorced | 17.3 |
| Separated | 2.6 |
| Never married | 9.2 |
Note. ORANJ BOWL = Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life.
At the neighborhood level, density of food sources per census tract was as follows: fast-food establishments (range = 0–11; mean = 1.8), storefronts (range = 0–13; mean = 5.4), and supermarkets (range = 0–6; mean = 1.5).
Bivariate correlations (Table 2) revealed significant positive correlations between obesity and fast food and storefronts but not supermarkets. Education and income were negatively associated with obesity, fast food, storefronts, gender (female), and race (African American), but not supermarkets. Race (African American) was positively associated with obesity, storefronts, and gender (female) and negatively associated with supermarkets, education, and income. Substantial within-cluster intraclass correlations existed for race (0.311), household income (0.182), and education (0.125).
TABLE 2—
Bivariate Associations Between Obesity, Neighborhood Food Sources, and Demographic Characteristics: Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life (ORANJ BOWL), 2006–2008
| Variable | Obesity | Fast Food | Storefrontsa | Supermarkets | Age | Education | Income | Gender | Race |
| Obesity | 1.000 | ||||||||
| Fast food | 0.038** | 1.000 | |||||||
| Storefronts | 0.102** | 0.308** | 1.000 | ||||||
| Supermarkets | –0.009 | 0.506** | 0.237** | 1.000 | |||||
| Age | 0.020 | 0.005 | 0.013 | 0.018 | 1.000 | ||||
| Education | –0.118** | –0.061** | –0.135** | 0.043** | –0.145** | 1.000 | |||
| Income | –0.102** | –0.079** | –0.24** | 0.029* | –0.267** | 0.462** | 1.000 | ||
| Gender | 0.041** | 0.026* | 0.033* | –0.009 | 0.054** | –0.107** | –0.163** | 1.000 | |
| Race | 0.107** | 0.029* | 0.300** | –0.056** | –0.009 | –0.145** | –0.225** | 0.042** | 1.000 |
Note. ORANJ BOWL = Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life.
Storefronts comprised of: convenience stores, bars and pubs, and small grocery stores.
*P < .05; **P < .001.
Results of the ML-SEM analysis are presented in Table 3. At level 1, gender (female; odds ratio [OR] = 1.1; 95% confidence interval [CI] = 1.05, 1.15), education (lower; OR = 1.1; 95% CI = 1.02, 1.05), and race (African American; OR = 1.2; 95% CI = 1.16, 1.40) were associated with obesity. Income and age were not associated with obesity. There were significant but modest associations among all of the covariates with the exception of race, age, and gender.
TABLE 3—
ML-SEM Parameter Estimates of Association Between Obesity and Food Sources (n = 5572): Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life (ORANJ BOWL), 2006–2008
| Nontandardized Estimates |
Standardized Estimates |
|||
| b (SE) | 95% CI | B (SE) | 95% CI | |
| Individual level 1 (within) | ||||
| Obesity regressed on | ||||
| Age | 0.003 (0.002) | –0.001, 0.007 | 0.023 (0.015) | –0.007, 0.053 |
| Gender | –0.094 (0.023) | –0.14, –0.048 | –0.056** (0.013) | –0.030, –0.082 |
| Education | –0.033 (0.006) | –0.045, –0.021 | –0.085** (0.016) | –0.053, –0.117 |
| Income | –0.004 (0.011) | –0.026, 0.018 | –0.007 (0.018) | –0.029, 0.043 |
| Race | 0.245 (0.050) | 0.145, 0.345 | 0.072** (0.015) | 0.042, 0.102 |
| African American correlated with | ||||
| Age | –0.009 (0.025) | –0.059, 0.041 | –0.005 (0.015) | –0.035, 0.025 |
| Gender | 0.002 (0.002) | –0.002, 0.006 | 0.022 (0.015) | –0.008, 0.052 |
| Education | –0.047 (0.008) | –0.063, –0.031 | –0.096** (0.015) | –0.126, –0.066 |
| Income | –0.050 (0.007) | –0.064, –0.036 | –0.150** (0.019) | –0.188, –0.112 |
| Age correlated with | ||||
| Gender | 0.179 (0.048) | 0.083, 0.275 | 0.053** (0.014) | 0.025, 0.081 |
| Education | –2.178 (0.197) | –2.572, –1.788 | –0.153** (0.014) | –0.181, –0.125 |
| Income | –2.791 (0.145) | –3.084, –2.504 | –0.287** (0.014) | –0.315, –0.259 |
| Gender correlated with | ||||
| Education | –0.115 (0.000) | –0.115, –0.115 | –0.117** (0.014) | –0.145, –0.089 |
| Income | –0.107 (0.000) | –0.107, –0.107 | –0.160** (0.014) | –0.188, –0.132 |
| Education correlated with income | 1.268 (0.049) | 1.176, 1.374 | 0.445** (0.013) | 0.419, 0.471 |
| Neighborhood level 2 (within) | ||||
| Fast food indicated by | ||||
| McDonald's | 1.000 (0.000) | 1.000, 1.000 | 0.780 (0.025) | 0.730, 0.830 |
| Burger King | 0.710 (0.043) | 0.624, 0.796 | 0.750** (0.029) | 0.692, 0.808 |
| Wendy’s | 0.287 (0.034) | 0.219, 0.355 | 0.400** (0.032) | 0.336, 0.464 |
| Taco Bell | 0.089 (0.019) | 0.051, 0.127 | 0.314** (0.055) | 0.204, 0.424 |
| KFC | 0.077 (0.016) | 0.045, 0.109 | 0.231** (0.031) | 0.169, 0.293 |
| Storefronts Indicated by | ||||
| Convenience stores | 1.000 (0.000) | 1.000, 1.000 | 0.886** (0.012) | 0.862, 0.910 |
| Bars or pubs | 0.706 (0.021) | 0.664, 0.748 | 0.809** (0.013) | 0.783, 0.835 |
| Small grocery stores | 1.457 (0.041) | 1.375, 1.539 | 0.870** (0.012) | 0.846, 0.894 |
| Obesity indicated by BMI ≥ 30 kg/m2 | 1.000 (0.000) | 1.000, 1.000 | 0.921** (0.254) | 0.413, 1.429 |
| Obesity regressed on | ||||
| Fast food | 0.827 (0.087) | 0.653, 1.001 | 0.338** (0.102) | 0.134, 0.542 |
| Storefronts | 2.262 (0.940) | 0.382, 4.142 | 0.568** (0.241) | 0.086, 1.050 |
| Supermarkets | 0.273 (0.674) | –1.075, 1.621 | 0.066 (0.162) | –0.258, 0.390 |
Note. BMI = body mass index; CI = confidence interval; ML-SEM = multilevel structural equation models; ORANJ BOWL = Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life.
**P < .001.
Fast food was well measured at level 2, with standardized loadings ranging from 0.23 to 0.78. Likewise, storefronts were well measured, with standardized loadings ranging from 0.81 to 0.89. At level 2, obesity was significantly associated with fast food (OR = 2.29; 95% CI = 1.93, 2.71) and storefronts (OR = 9.60; 95% CI = 1.52, 26.60) but not supermarkets (OR = 1.31; 95% CI = 0.35, 4.40), indicating that people living in areas having greater densities of convenience food sources were more likely to be obese.
DISCUSSION
These analyses revealed that the presence of fast-food restaurants and storefronts (convenience stores, bars, and small grocery stores) has significant associations with older adults’ obesity that are independent of individual-level characteristics with known associations to obesity, including age, race, and socioeconomic status. Fast-food restaurants, convenience stores, bars, and small grocery stores offer prepared, zero high-calorie foods and little fresh produce.42 Others have found that the availability of fast-food restaurants has a positive relationship to intake of fat, sodium, and soft drinks and a negative relationship with nutrient-dense foods such as fruit, vegetables, and milk.17,19,29 Although our findings are consistent with those reported elsewhere,15,17–19,27 these results move the field forward because they control for individual-level characteristics with known associations with obesity that have obscured understanding of the relationships between characteristics of individuals and of place.
Although evidence regarding the association between obesity and supermarket density is contradictory, our analysis found no significant association between supermarket density and obesity. Supermarkets sell a wide variety of high-quality products at low cost, but they also sell a variety of unhealthy foods. Because we did not have data about either the choices people made about where to shop or their purchasing decisions, our conclusions are limited. Future studies examining whether older people eat in local fast-food restaurants and shop in local supermarkets will add important information to our understanding of the relationship between neighborhood characteristics and obesity. Our findings regarding supermarket density and obesity are consistent with those reported by Wang et al.43 and Stafford et al.,22 but they differ from those finding that proximity to supermarkets decreased the risk of obesity.18,19,21,24,27 These discrepancies may be explained by the age of people studied (our sample was significantly older) as well as by the complexity of the sampled food environment.
Our study, which included information about multiple food environments in a single analysis, supports the finding of Rundle et al.24 that densities of supermarkets, convenience stores, small groceries, bars and pubs, and fast-food restaurants are strongly correlated with each other. These 2 studies, unlike those that do not examine the totality of food environments, help to disentangle the associations of type of food environment and obesity.
Using multilevel structural equation modeling to examine relationships between neighborhood characteristics and obesity advances the field in the following ways: (1) it models the nesting of people within neighborhoods; (2) it allows for multiple indicators of neighborhood constructs, thereby reducing measurement error; and (3) it provides the opportunity to parse variance attributable to individual effects and to neighborhood effects. Results from these analyses highlight the importance of using analytic tools that account for individual and neighborhood resources. Doing so sets the stage for better understanding of what it is about neighborhoods that either supports or undermines efforts toward optimal weight management.
Although this study extends knowledge about the role of neighborhood features vis-à-vis obesity, like all studies, it has its limitations. First, because the data we analyzed were cross-sectional, we do not know the extent to which neighborhood food sources caused obesity. To address this issue, longitudinal data that capture information about changes within neighborhoods are as important as data regarding changes experienced by people over time. Second, it would be important to know how long the individual had been living in the neighborhood, a variable not included in our data set. Third, our analyses relied on self-report information regarding height and weight, and therefore are subject to individual perceptions. Clinical assessment would increase the objectivity associated with measurement of these characteristics.
Fourth, as research in this area advances, it will be important to consider that environments may matter more for some people than others,44 and addressing the differential effects of neighborhoods will be critical. It is also important to acknowledge that since 2007, when our data regarding fast-food restaurants were collected, many fast-food chains have changed their menus, adding healthier food options. Whether and how this changes the association between presence of fast-food restaurants and obesity remain unclear. Finally, there may be confounding variables that can account for the findings. For example, neighborhoods with supermarkets may be safer and have more recreational resources to reduce the obesity levels.31
Extending knowledge regarding the public health significance that neighborhood food environments have on obesity requires further study. Neighborhood food environments are dynamic entities created by and responding to external economic and social factors as well as to the collective actions of its residents. Harnessing and influencing these changes have the potential to lower the rate of obesity. Partnerships between health researchers, communities, area developers, city planners, and policy experts interested in neighborhoods will be central to decreasing rates of obesity.
Acknowledgments
We thank Jonathan Brill, PhD, Yvonne Shands, and the University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine (UMDNJ-SOM) Research Call Center staff, whose hard work and perseverance yielded the data, as well as the UMDNJ-SOM New Jersey Institute for Successful Aging, whose generous support funded the data collection efforts of the ORANJ BOWL research panel.
Human Participant Protection
This project was approved by the institutional review board of the University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine.
References
- 1.Centers for Disease Control and Prevention. Public health and aging: trends in aging—United States and worldwide. JAMA. 2003;289(11):1371–1373. [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Khavjou OA, Thompson H et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–570. doi: 10.1016/j.amepre.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Mendes E. In US, obesity peaks in middle age. Gallup, August 31, 2010. Available at: http://www.gallup.com/poll/142736/obesity-peaks-middle-age.aspx. Accessed February 4, 2014.
- 5.Sturm R, Ringel JS, Andreyeva T. Increasing obesity rates and disability trends. Health Aff (Millwood) 2004;23(2):199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- 6.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff (Millwood) 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 7.Cohen DA, Finch BK, Bower A, Sastry N. Collective efficacy and obesity: the potential influence of social factors on health. Soc Sci Med. 2006;62(3):769–778. doi: 10.1016/j.socscimed.2005.06.033. [DOI] [PubMed] [Google Scholar]
- 8.Berke EM, Gottlieb L, Vernez Moudon A, Larson EB. Protective association between neighborhood walkability and depression in older men. J Am Geriatr Soc. 2007;55(4):526–533. doi: 10.1111/j.1532-5415.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- 9.Fisher KJ, Li F. A community-based walking trial to improve neighborhood quality of life in older adults: a multilevel analysis. Ann Behav Med. 2004;28(3):186–194. doi: 10.1207/s15324796abm2803_7. [DOI] [PubMed] [Google Scholar]
- 10.Fisher KJ, Li F, Michael Y, Cleveland M. Neighborhood-level influences on physical activity among older adults: a multilevel analysis. J Aging Phys Act. 2004;12(1):45–63. doi: 10.1123/japa.12.1.45. [DOI] [PubMed] [Google Scholar]
- 11.Glass TA, Rasmussen MD, Schwartz BS. Neighborhoods and obesity in older adults: The Baltimore Memory Study. Am J Prev Med. 2006;31(6):455–463. doi: 10.1016/j.amepre.2006.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grafova IB, Freedman VA, Kumar R, Rogowski J. Neighborhoods and obesity in later life. Am J Public Health. 2008;98(11):2065–2071. doi: 10.2105/AJPH.2007.127712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King T, Kavanagh AM, Jolley D, Turrell G, Crawford D. Weight and place: a multilevel cross-sectional survey of area-level social disadvantage and overweight/obesity in Australia. Int J Obes (Lond) 2006;30(2):281–287. doi: 10.1038/sj.ijo.0803176. [DOI] [PubMed] [Google Scholar]
- 14.Li F, Harmer P, Fisher KJ, McAuley E. Tai chi: improving functional balance and predicting subsequent falls in older persons. Medicine. 2004;36(12):2046–2052. doi: 10.1249/01.mss.0000147590.54632.e7. [DOI] [PubMed] [Google Scholar]
- 15.Chou SY, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23(3):565–587. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19(2):137–143. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 17.Mehta N, Chang V. Weight status and restaurant availability: a multilevel analysis. Am J Prev Med. 2008;34(2):127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J Urban Health. 2010;87(5):771–781. doi: 10.1007/s11524-010-9460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–495. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopez RP. Neighborhood risk factors for obesity. Obesity (Silver Spring) 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- 22.Stafford M, Cummins S, Ellaway A, Sacker A, Wiggins RD, Macintyre S. Pathways to obesity: identifying local, modifiable determinants of physical activity and diet. Soc Sci Med. 2007;65(9):1882–1897. doi: 10.1016/j.socscimed.2007.05.042. [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 24.Rundle A, Neckerman KM, Freeman L et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect. 2009;117(3):442–447. doi: 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanibuchi T, Kondo K, Nakaya T et al. Neighborhood food environment and body mass index among Japanese older adults: results from the Aichi Gerontological Evaluation Study (AGES) Int J Health Geogr. 2011;10:43. doi: 10.1186/1476-072X-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morland K, Diez Roux A, Wing S. Supermarkets, other food stores, and obesity: the Atherosclerosis Risk in Communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Blumberg SJ, Luke JV. Coverage bias in traditional telephone surveys of low-income and young adults. Public Opin Q. 2007;71(5):734–749. [Google Scholar]
- 29.Morland K, Wing S, Diez-Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 30.Heck RH, Thomas SL. An Introduction to Multilevel Modeling Techniques. New York, NY: Routledge; 2009. [Google Scholar]
- 31.Mehta PD, Neale MC. People are variables too: multilevel structural equations modeling. Psychol Methods. 2005;10(3):259–284. doi: 10.1037/1082-989X.10.3.259. [DOI] [PubMed] [Google Scholar]
- 32.Muthen LK, Muthen BO. Mplus User’s Guide. 6th ed. Los Angeles, CA: Muthen & Muthen; 2009. [Google Scholar]
- 33.Curran PJ. Have multilevel models been structural equation models all along? Multivariate Behav Res. 2003;38(4):529–569. doi: 10.1207/s15327906mbr3804_5. [DOI] [PubMed] [Google Scholar]
- 34.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods. 2010;15(3):209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- 35.Rovine MJ, Molenaar PCM. A structural modeling approach to the random coefficients model. Multivariate Behav Res. 2000;35(1):51–88. doi: 10.1207/S15327906MBR3501_3. [DOI] [PubMed] [Google Scholar]
- 36.Beets MW, Foley JT. Association of father involvement and neighborhood quality with kindergartners’ physical activity: a multilevel structural equation model. Am J Health Promot. 2008;22(3):195–203. doi: 10.4278/ajhp.22.3.195. [DOI] [PubMed] [Google Scholar]
- 37.Kuntsche E, Kuendig H, Gmel G. Alcohol outlet density, perceived availability and adolescent alcohol use: a multilevel structural equation model. J Epidemiol Community Health. 2008;62(9):811–816. doi: 10.1136/jech.2007.065367. [DOI] [PubMed] [Google Scholar]
- 38.Newsom JT. A multilevel structural equation model for dyadic data. Struct Equ Modeling. 2002;9(3):431–447. [Google Scholar]
- 39.Walsh BM, Matthews RA, Tuller MD, Parks KM, McDonald DP. A multilevel model of the effects of equal opportunity climate on job satisfaction in the military. J Occup Health Psychol. 2010;15(2):191–207. doi: 10.1037/a0018756. [DOI] [PubMed] [Google Scholar]
- 40.Muthen BO. Multilevel factor analysis of class and student achievement components. J Educ Meas. 1991;28(4):338–354. [Google Scholar]
- 41.Pruchno RA, Wilson-Genderson M, Cartwright FP. The texture of neighborhoods and disability among older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67(1):89–98. doi: 10.1093/geronb/gbr131. [DOI] [PubMed] [Google Scholar]
- 42.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson MI. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. 2006;16(1):275–280. [PubMed] [Google Scholar]
- 43.Wang MC, Kim S, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health. 2007;61(6):491–498. doi: 10.1136/jech.2006.051680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility disability and the urban built environment. Am J Epidemiol. 2008;168(5):506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]