Abstract
Objectives. We examined regional variation in tooth loss in the United States from 1999 to 2010.
Methods. We used 6 waves of the Behavioral Risk Factor Surveillance System and data on county characteristics to describe regional trends in tooth loss and decompose diverging trends into the parts explained by individual and county components.
Results. Appalachia and the Mississippi Delta had higher levels of tooth loss than the rest of the country in 1999. From 1999 to 2010, tooth loss declined in the United States. However, Appalachia did not converge toward the US average, and the Mississippi Delta worsened relative to the United States. Socioeconomic status explained the largest portion of differences between regions in 1999, but a smaller portion of the trends. The Mississippi Delta is aging more quickly than the rest of the country, which explains 17% of the disparity in the time trend.
Conclusions. The disadvantage in tooth loss is persistent in Appalachia and growing in the Mississippi Delta. The increasing disparity is partly explained by changes in the age structure but is also associated with behavioral and environmental factors.
People in Appalachia have worse oral health than other Americans.1–4 West Virginia, the only state entirely located in Appalachia, has the highest rate of people missing 6 or more teeth (65.6%) and the second highest rate of complete tooth loss (37.8%) for people aged 65 years and older.5,6 The Mississippi Delta, another economically disadvantaged region, also has poor oral health. Mississippi, which falls mostly in the Mississippi Delta, follows West Virginia with the second highest rate of people missing 6 or more teeth (58.2%) and the fourth highest rate of complete tooth loss (27.3%) among those aged 65 years and older.5,6 Of the 5 states with the highest rate of people missing 6 or more teeth, 4 fall in the Mississippi Delta or Appalachia.
Numerous studies have examined the causes of poor oral health in Appalachia and the Mississippi Delta. Studies have highlighted the importance of both individual attributes and broader elements that affect Appalachian communities. Individual attributes include socioeconomic status (SES), genetics, oral bacteria, tobacco use, knowledge of health behaviors, and dental insurance.1,2,4,7–9 Broader elements include fluoride in the water supply, cultural importance placed on oral health, presence of coal mining, and number of dentists and dental hygienists per capita.1,2,4,10,11 Less research has been done on oral health in the Mississippi Delta, although this region also has high rates of tooth loss. Studies that have analyzed this region have highlighted the roles of race, private dental insurance, parental oral health, parental health behaviors, and diet.12–15
Oral health in the United States has significantly improved in the past 4 decades. The number of decayed, missing, and filled teeth; prevalence of untreated caries; edentulous rate; and rate of periodontal disease have all declined.16–22 The overall improvement in oral health outcomes in the United States raises the question of whether all areas of the United States are improving equally or whether there are persistent regional disparities in oral health outcomes. Previous reports from the Centers for Disease Control and Prevention have provided raw data on tooth loss in each state,5,6 but data on regional disparities is lacking. Moreover, without microdata it is impossible to discern whether divergent regional trends are attributable to relatively innocuous differences, such as the age structure of the regions, or driven by more concerning disparities, such as poverty and access to oral health care.
To address this gap, we used data from the Behavioral Risk Factor Surveillance System (BRFSS) to examine regional variation in the level and improvement in the rate of tooth loss from 1999 to 2010. Our regions of interest, Appalachia and the Mississippi Delta, are defined as groups of counties. We analyzed the association between tooth loss and individual characteristics, individual behavior, and county factors.
We tested 3 hypotheses: (1) The Mississippi Delta and Appalachia will have had less improvement in oral health than the rest of the country in the past decade, (2) the age profile of the regions will explain a portion of the regional differences, and (3) individual characteristics, individual behavior, and county characteristics will explain a portion of the regional differences.
METHODS
The BRFSS is a telephone survey covering all 50 states, Washington, DC, and the territories. We used the 1999, 2002, 2004, 2006, 2008, and 2010 data sets; in these years, all states asked a question on oral health outcomes. These waves included 1 933 069 respondents.
We excluded respondents who were missing the oral health measure or demographic variables; this affected 81 797 respondents. The county code of a respondent is suppressed if too few respondents live in that county; 252 405 respondents were missing their county code. We could not determine whether these respondents lived in one of our regions of interest, so we excluded them from the analysis.
The BRFSS is representative at the state level, but not at the county level. Both Appalachia and the Mississippi Delta are defined by county. Although some concern exists that the BRFSS may not be representative of these regions,2,23 we showed that it was representative of Appalachia by comparing BRFSS data with the American Community Survey on 7 demographic variables (see Appendix A, available as a supplement to this article at http://www.ajph.org). Krause et al.2 noted that some years of BRFSS data have very few Appalachian respondents because not all states participated in the oral health questions every year. We only used waves of the BRFSS in which all states participated in the question on missing teeth, which dramatically increased the sample of Appalachian respondents to 127 104 over the 6 waves of data.
Measuring Oral Health Outcomes
Tooth loss reflects overall oral health and has a large impact on quality of life. Significant tooth loss is often caused by other oral health problems, including periodontal disease or extensive caries.3 Losing a significant number of teeth is associated with eating fewer healthy foods and increased risk of stroke, even among those who are not missing all their teeth.24–26 Complete tooth loss, another important measure of oral health, is not ideal for our analyses. Although the disparity in edentulism on the basis of age and SES has decreased over time, the disparity in the number of missing teeth (measured by a dental examination) has increased (B. Wu et al., unpublished data, December 2013). Focusing on edentulism may obscure other oral health disparities.
BRFSS respondents reported whether they are missing no teeth, missing 1 to 5 teeth, missing more than 5 but not all teeth, or missing all teeth. We collapsed this measure into a dichotomous variable indicating whether the respondent was missing 6 or more teeth, a method of identifying significant tooth loss used in previous studies.2,5,6,23,27
Individual Characteristics
The BRFSS contains information on age, race, ethnicity, income, educational attainment, and smoking behavior. For our analysis, we created indicator variables showing (1) whether respondents smoked 100 or more cigarettes in their life, (2) each racial category, and (3) each level of education: elementary, some high school, high school graduate, some college, and college graduate. We included age, age squared, and age cubed to account for nonlinearity in the relationship between missing teeth and age.
The BRFSS reports household income in brackets. We used the Current Population Survey to estimate average family income in each bracket in each year. We then used the Consumer Price Index to convert each income estimate into 1999 dollars. The Bureau of Labor Statistics calculates the Consumer Price Index, the standard method of adjusting for inflation, by tracking changes in the price of consumer goods and services.28 Many respondents declined to answer the question on income (147 835 respondents) or responded that they did not know (120 627 respondents). If a respondent declined to respond or did not know, we replaced their income with the average for the year. We created 2 indicator variables that showed whether the respondent declined to respond or did not know.
Measuring Fluoride Levels in Water
We estimated the fluoride in each respondent’s drinking water with the My Water’s Fluoride system from the Centers for Disease Control and Prevention. My Water’s Fluoride contains fluoride levels in public water systems in some states in the United States. The data are from different years depending on when the state provided the information. The data for each water system contain the primary county of the water system, whether the system adds fluoride, the level of fluoridation achieved, and the number of people served. For systems that do not add fluoride, the Centers for Disease Control and Prevention collects the natural level of fluoride in water. We calculated the population-weighted average level of natural and adjusted fluoride for each county.
Some counties were missing measures of natural or adjusted fluoride. If a county’s water systems use only natural fluoride or only adjusted fluoride, the county will only have 1 measure of fluoride. Additionally, some states do not participate in the My Water’s Fluoride program. If a respondent lived in a county that did not include level of natural or adjusted fluoride, we replaced these missing values with the average (population-weighted) levels in the respondent’s census division (9 subregions of the United States). Of the respondents, 741 572 had missing natural or adjusted fluoride values. We then included an indicator variable showing whether the respondent’s level of fluoride was replaced with the division average. If there was a systematic difference between those whose fluoride was missing and those with a valid measure, this indicator variable’s coefficient would be different from zero.29,30
Guam, Puerto Rico, and the Virgin Islands do not have data in the My Water’s Fluoride system and are not part of any census division; thus, we had no estimate for the fluoride in their water. We therefore did not include respondents from these locations in the analyses.
The 1990 Census indicated each respondent’s main water source. We obtained the percentage of people in each county who were on well water. In areas with low natural fluoride, well water will have much lower levels of fluoride than fluoridated water systems. We included the percentage of the county on well water and the interactions between this variable and the level of natural and adjusted fluoride.
Measuring County-Level Access to Dental Care
The Census Bureau’s County Business Patterns give the number of firms by industry in each county in each year. To estimate each respondent’s access to dental care, we used the number of dental offices in the respondent’s county in the year they were observed. We controlled for population size and land area of the respondent’s county to observe the association between number of dental offices and significant tooth loss, holding population and land area constant. We estimated each county’s population with the closest decennial census.
Data Analysis
We used the following regression framework. In Equation 1, y indicates whether the respondent has lost 6 or more teeth. βa and βm are the additional amount of tooth loss in Appalachia and the Mississippi Delta in the base year (1999). The year variable is a linear year time trend, with βy indicating the average change in the rate of significant tooth loss in the nation each year. The interactions between each region dummy and the year trend demonstrate whether these regions are experiencing a different trend in improvement in oral health.
The second equation adds the county (Zi) and individual (Xi) variables. The difference between βa and βA (and βm and βM) is the amount of the difference in the rate of significant tooth loss in the base year that can be explained by county and individual variables. The difference between βa,y and βA,Y is the amount of the difference in the trend that can be explained by the county and individual variables.
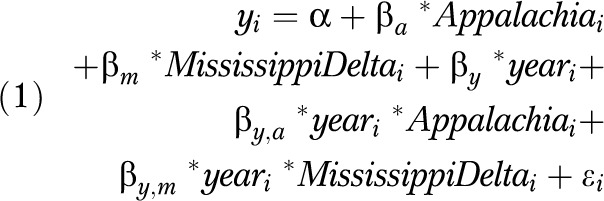 |
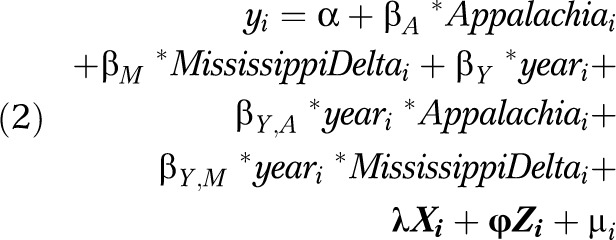 |
The regressions used the final BRFSS weight as complex sampling weights. Each respondent had variables measured at the individual level and at the county level. Thus, the error terms in Equation 2 were correlated within county, and a typical regression would have underestimated the standard errors of the estimates of the coefficients.31 To address this correlation, we clustered the error terms by county (the syntax in Stata version 12 for robust clustered standard errors is as follows: reg dependent independent [weight], robust cluster[cluster variable]).32–34
To determine how much each explanatory variable contributed to regional differences, we used a method of decomposition developed by Gelbach.35 First, we looked at the difference in each explanatory variable between regions and time trends, and then we looked at the association between the explanatory variable and tooth loss conditional on all other explanatory variables. The product of these 2 is the part of the difference in oral health outcomes that is attributable to that explanatory variable. The results of this decomposition, unlike those of other techniques, do not depend on the order in which the variables are added into the equation.
RESULTS
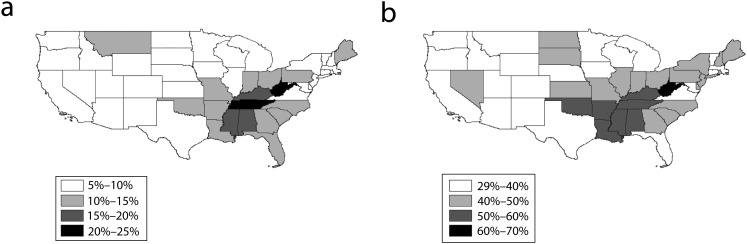
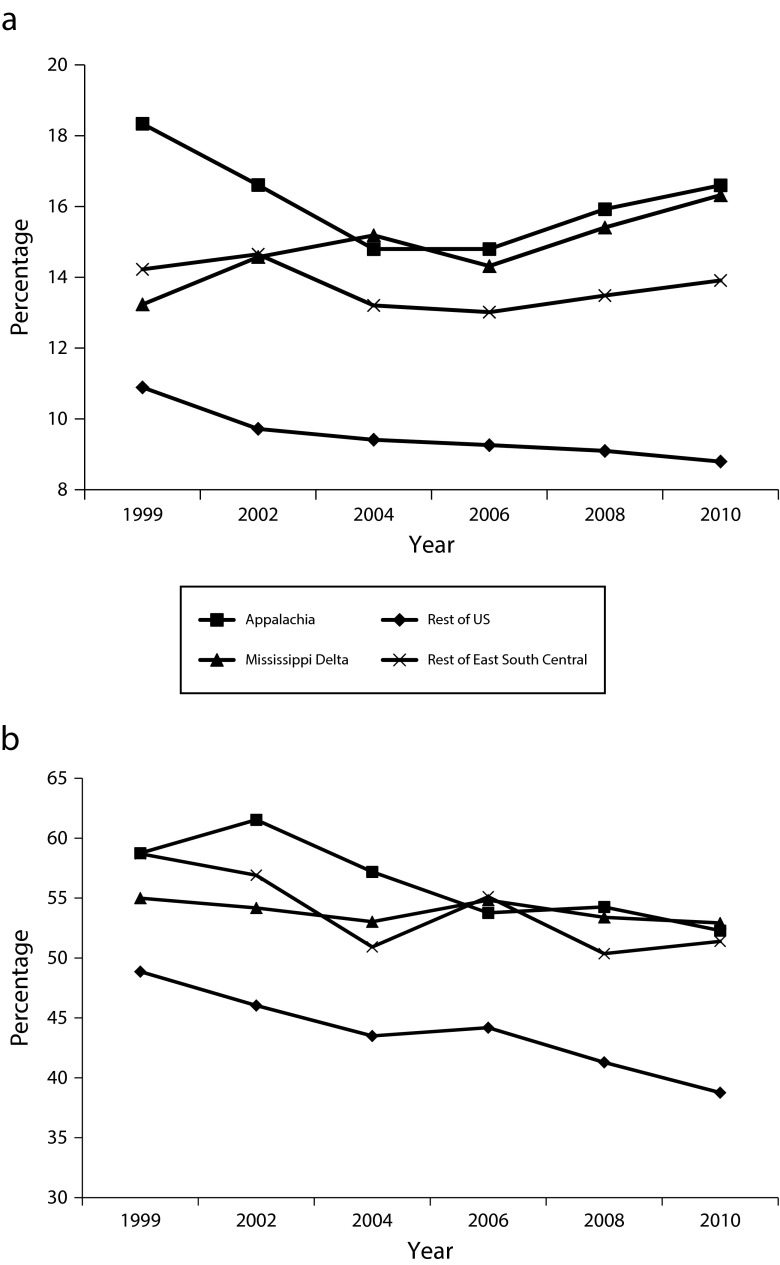
Figure 1 illustrates that even after decades of improvements in oral health, certain regions of the country still have high rates of tooth loss. The time trends in Figure 2 suggest an even more striking pattern: improvements in the rate of tooth loss from 1999 to 2010 appear to be faster in areas that already had better oral health.
FIGURE 1—
Map showing the percentage of significant tooth loss in 2010 for those aged (a) younger than 65 years and (b) 65 years and older: Behavioral Risk Factor Surveillance System, United States, 2010.
Note. Results use complex sampling weight provided by the Behavioral Risk Factor Surveillance System.
FIGURE 2—
Rate of significant tooth loss by region among those aged (a) younger than 65 years and (b) 65 years and older: Behavioral Risk Factor Surveillance System, United States, 1999–2010.
Note. Appalachia is based on the definition from the Appalachian Regional Commission. Mississippi Delta is based on the definition from the Delta Regional Authority. East South Central is based on the US Census Bureau definition (Kentucky, Tennessee, Mississippi, and Alabama). Results use complex sampling weight provided by the Behavioral Risk Factor Surveillance System.
Table 1 illustrates the results of the ordinary least squares regressions of Equations 1 and 2. The table shows that for those younger than 65 years and those aged 65 years and older, the base rate of significant tooth loss was higher in Appalachia and the Mississippi Delta than in the rest of the country. For those younger than 65 years, the rate of significant tooth loss in 1999 was 6.2 percentage points higher in Appalachia and 2.9 percentage points higher in the Mississippi Delta. For those aged 65 years and older, the difference was 13.4 percentage points for Appalachia and 5.9 percentage points for the Mississippi Delta. All differences were statistically significant at the .01 or .001 level.
TABLE 1—
Regression Results of Significant Tooth Loss for Those Younger Than 65 Years and Those Aged 65 Years and Older: Behavioral Risk Factor Surveillance System, United States, 1999–2010
| Missing ≥ 6 Teeth, Aged < 65 Years (n = 1 127 140) |
Missing ≥ 6 Teeth, Aged ≥ 65 Years (n = 405 532) |
|||
| Variable | Equation 1,a b (SE) | Equation 2,b b (SE) | Equation 1,a b (SE) | Equation 2,b b (SE) |
| Rest of the United States | ||||
| Average in base year | 0.105** (0.0025) | 0.109** (0.0015) | 0.489** (0.0066) | 0.475** (0.0050) |
| Year trend | −0.002** (0.0002) | −0.002** (0.0002) | −0.009** (0.0006) | −0.007** (0.0005) |
| Mississippi Delta | ||||
| Additional tooth loss in base year relative to rest of the United States | 0.029* (0.0098) | 0.007 (0.0073) | 0.059* (0.0210) | 0.014 (0.0167) |
| Additional tooth loss in year trend relative to rest of the United States | 0.004** (0.0009) | 0.003** (0.0007) | 0.007** (0.0019) | 0.005* (0.0018) |
| Appalachia | ||||
| Additional tooth loss in base year relative to rest of the United States | 0.062** (0.0086) | 0.039** (0.0061) | 0.134** (0.0139) | 0.091** (0.0152) |
| Additional tooth loss in year trend relative to rest of the United States | 0.001 (0.0007) | −0.0003 (0.0006) | −0.0004 (0.0014) | −0.001 (0.0017) |
| R2 | 0.005 | 0.168 | 0.010 | 0.136 |
Note. Standard errors were robust, and observations were clustered at the county level. All results used complex sampling weights provided by the Behavioral Risk Factor Surveillance System.
Equation 1 data show the results of regressing the indicator variable for missing ≥ 6 teeth on indicator variables for being in Appalachia or the Mississippi Delta, a year trend, and an interaction between each region and the year trend. The base regressions show that for both age groups, Appalachia and the Mississippi Delta have significantly higher rates of significant tooth loss than the rest of the country in the base year. The year trend for the nation shows a decrease in the percentage with significant tooth loss, but this trend is much slower in the Mississippi Delta.
Equation 2 data show that a large portion of the base and trend differences are explained by the additional explanatory variables included. The control variables are demeaned, so the constants reflect the rate of tooth loss at the mean values for the explanatory variables.
*P < .01; **P < .001.
Moreover, as suggested in Figure 2, the Mississippi Delta is improving more slowly than the rest of the country. In the rest of the United States, without Appalachia and the Mississippi Delta, each year was associated with a 0.16 percentage point decrease in the rate of those younger than 65 years who were missing 6 or more teeth. In the Mississippi Delta, each year was associated with a 0.23 percentage point increase in the rate of those missing 6 or more teeth (this figure was obtained by adding the additional trend in the Mississippi Delta of 0.39 percentage points to the trend in the United States of −0.16 percentage points). For those aged 65 years and older, each year was associated with a 0.91 percentage point decrease in the rest of the United States, but only a 0.17 percentage point annual decrease in the Mississippi Delta. Appalachia did not experience a different time trend from the rest of the United States.
The data from Equation 2 include individual and county variables (Table 1). Including these covariates explains a large portion of both the difference in base year (1999) and in the time trend. Table 2 illustrates how much each group of covariates contributed to the difference in the base year and to the time trend. To help understand Table 2, we focus on the results for the Mississippi Delta for those younger than 65 years. Race/ethnicity explained 47% of the difference between the Mississippi Delta and the rest of the United States in 1999. This means that in 1999, the Mississippi Delta had a higher proportion of African Americans, and African Americans were more likely to be missing 6 or more teeth. However, race/ethnicity accounted for only 1% of the difference in the time trend between the Mississippi Delta and the rest of the United States because the proportion of African Americans in the Mississippi Delta did not change relative to the rest of the United States. By contrast, age explained −17% of the difference between the Mississippi Delta and the United States in 1999 because the Mississippi Delta was younger than the rest of the United States. However, the Mississippi Delta is aging more quickly than rest of the United States, so age explained 17% of the difference in the time trend.
TABLE 2—
Decomposition of Significant Tooth Loss in 1999 and the Difference in the Time Trend: Behavioral Risk Factor Surveillance System, United States, 1999–2010
| Mississippi Delta, Base Year (1999) |
Appalachia, Base Year (1999) |
Mississippi Delta, Time Trend |
||||
| Aged < 65 Years, Difference (% of Total Difference) | Aged ≥ 65 Years, Difference (% of Total Difference) | Aged < 65 Years, Difference (% of Total Difference) | Aged ≥ 65 Years, Difference (% of Total Difference) | Aged < 65 Years, Difference (% of Total Difference) | Aged ≥ 65 Years, Difference (% of Total Difference) | |
| Total difference | 0.029 (100) | 0.059 (100) | 0.062 (100) | 0.134 (100) | 0.004 (100) | 0.007 (100) |
| Unexplained difference | 0.007 (23) | 0.014 (24) | 0.039 (63) | 0.091 (68) | 0.003 (72) | 0.005 (71) |
| Explained difference | 0.023 (77) | 0.045 (76) | 0.023 (37) | 0.043 (32) | 0.001 (28) | 0.002 (29) |
| Individual | ||||||
| Age | –0.005 (–17) | –0.005 (–9) | 0.004 (7) | –0.001 (–1) | 0.001 (17) | 0.0004 (6) |
| Race/ethnicity | 0.014 (47) | 0.022 (38) | 0.004 (6) | 0.002 (2) | 0.0000 (1) | –0.0002 (–3) |
| Income | 0.009 (30) | 0.006 (10) | 0.006 (10) | 0.014 (10) | –0.0002 (–4) | 0.001 (9) |
| Education | 0.005 (18) | 0.028 (48) | 0.004 (7) | 0.031 (23) | 0.0002 (4) | 0.001 (7) |
| Smoking | –0.001 (–3) | –0.006 (–10) | 0.003 (4) | –0.007 (–5) | 0.0002 (6) | 0.0001 (1) |
| County | ||||||
| Fluoride in water | –0.001 (–2) | –0.003 (–4) | 0.002 (3) | 0.004(3) | 0.0001 (2) | 0.0001 (2) |
| Dental offices | 0.003 (11) | 0.021 (36) | 0.003 (4) | 0.017 (12) | 0.0001 (3) | 0.001 (10) |
| Population, land area | –0.002 (–6) | –0.019 (–33) | –0.002 (–3) | –0.016 (–12) | 0.0000 (–1) | –0.0002 (–3) |
Note. This table shows an accounting of the difference between Appalachia, the Mississippi Delta, and the rest of the country. The base year columns decompose the base year differences in both regions, and the time trend columns decompose the difference in the time trend in the Mississippi Delta. The first row shows the total difference between Appalachia, the Mississippi Delta, and the rest of the country. The second row shows the amount of difference that is unexplained after including the explanatory variables. The third row shows the amount that is explained by all the explanatory variables. The subsequent rows show the portion explained by each group of explanatory variables. There was no statistically significant time trend for Appalachia; therefore, there is no decomposition.
For both regions and age groups, income, education, and number of dental offices played an important role in the differences between Appalachia, the Mississippi Delta, and the rest of the United States in 1999. Smoking and fluoride in the water explained a small or negative portion of the difference between regions in 1999. However, income, education, and dental offices played a smaller role in the difference in the time trend in the Mississippi Delta. Smoking and fluoride in the water explained a positive portion of the difference in the time trend in the Mississippi Delta.
DISCUSSION
The maps presented in Figure 1 show striking regional differences in oral health. However, it is hard to understand what these maps mean for health disparities. Certain populations in the United States, such as older people, have worse oral health outcomes. If these vulnerable groups are disproportionately represented in Appalachia and the Mississippi Delta, these regions could have high tooth loss solely because of the composition of their populations. Our regression analysis and decomposition allow us to both describe the regional differences over time and assess how much is attributable to the composition of each region’s population and how much is associated with behavioral or environmental characteristics.
Despite the overall improvement in oral health in the United States, the Mississippi Delta and Appalachia are being left behind. The rate of significant tooth loss in the Mississippi Delta is improving at a significantly slower rate than the rest of the country—leading to a rising inequality between the Mississippi Delta region and the country as a whole. Appalachia starts with a much higher rate of tooth loss and is improving at the same rate as the rest of the nation. Thus, although the disparity in Appalachia is not worsening, it is persisting. These findings confirm our first hypothesis: these 2 historically disadvantaged regions continue to experience worse oral health outcomes.
As hypothesized, age plays a striking role in these regional disparities. The different age profiles of these regions do not explain a large portion of these regional differences in 1999 but are extremely important in explaining why the Mississippi Delta is improving more slowly than the rest of the nation. The Mississippi Delta is aging more quickly than the rest of the nation, which suggests that regional differences in oral health will continue to increase because of the changing demographic composition of the Mississippi Delta.36,37
Our results also support our third hypothesis that individual and county characteristics would explain a large portion of the regional differences. Smoking and fluoride variables explained small or negative portions of the regional difference in the base year, but they explained a positive portion of difference in the time trend for the Mississippi Delta. Thus, the increasing oral health disparities between the nation and the Mississippi Delta are associated with differences in behavior and the environment as well as compositional changes.
The vast majority of oral health disparities remain tied to SES. In both regions and in both age groups, the SES variables explained a sizable proportion of the difference in tooth loss in the base year and a smaller portion of the time trend. Having lower SES is strongly associated with poor oral health, and lower SES groups have seen less improvement in their oral health over the past decade.20,38 Because Appalachia and the Mississippi Delta are economically disadvantaged areas, their populations’ oral health suffers relative to the rest of the United States.
Limitations
The BRFSS suppressed respondents’ county codes if too few respondents lived in the county. Both Appalachia and the Mississippi Delta are defined as a group of counties; without the county code, we could not determine whether the respondent lived in one of our regions of interest. These respondents had worse teeth on average: Of those without county codes, 22.8% were missing 6 or more teeth compared with only 15.7% of those with county codes.
The BRFSS relies on self-reported oral health measures. Self-reported measures are commonly used in large epidemiological and surveillance studies, and self-reported number of remaining teeth is approximately consistent with a dental exam; however, we are aware that how well a self-report matches a dental examination depends on demographic characteristics.39,40 The BRFSS is also a cross-sectional survey, so we were not able to track individual respondents over time. Additionally, the BRFSS does not contain any information on key mediators between SES and oral health, such as diet, oral hygiene, and oral health knowledge.
A third limitation of the study is that My Water’s Fluoride does not contain data for all counties. In our analysis, we included an indicator variable that showed whether a respondent’s county’s level of natural or adjusted fluoride was replaced with the division average. If there was a systematic difference between those with estimated levels of fluoride and those with a measure from My Water’s Fluoride, the coefficient on this indicator variable would be different from 0.29,30 For both age groups, the estimate of the coefficient on this indicator variable was not different from 0 (0.0003; P = .8 for those < 65 years and −0.0032; P = .5 for those aged ≥ 65 years). Additionally, we addressed the missing values through listwise deletion and multiple imputation.30 The results were similar to those presented here and are available on request.
Conclusions
Regional oral health disparities in the United States are large and persistent. The Mississippi Delta is aging more quickly than the rest of the nation; because tooth loss accumulates over the life span, this measure is sensitive to changes in the age composition of a region. Different regional age compositions are not concerning in and of themselves, nor are they very malleable by policy; however, this highlights the role of improving oral health over the life course. Preventing deterioration in oral health as people age will incidentally reduce regional disparities, because these regions are aging more quickly than the rest of the nation.
The vast majority of the explained regional difference is associated with SES. Smoking and the level of fluoride in the water play roles in the regional differences in the time trends. If SES and these proximate factors in the Mississippi Delta continue to worsen relative to the rest of the nation, the difference in oral health will grow. Unlike the changes in age composition, this is not a natural divergence resulting from differentially aging populations but rather a heath disparity that reflects differences in SES and proximate causes of oral health. This disparity suggests that policy should adopt a multipronged approach that improves access to dental care, increases exposure to fluoridated water, and reduces oral health–related risk behaviors.
Acknowledgments
B. Wu is funded by the National Institutes of Health/National Institute of Dental and Craniofacial Research (grant 1R01DE019110).
Human Participant Protection
The analysis used publicly available data that is not identifiable, so Duke University’s institutional review board indicated it did not need approval or exemption.
References
- 1.Polk DE, Weyant RJ, Crout RJ et al. Study protocol of the Center for Oral Health Research in Appalachia (COHRA) etiology study. BMC Oral Health. 2008;8:18. doi: 10.1186/1472-6831-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krause DD, May WL, Lane NM, Cossman JS, Konrad TR. An Analysis of Oral Health Disparities and Access to Services in the Appalachian Region. Washington, DC: Appalachian Regional Commission; 2011. [Google Scholar]
- 3.McNeil DW, Crout R, Marazita ML. Appalachian Health and Well-Being. Lexington, KY: University Press of Kentucky; 2012. [Google Scholar]
- 4.Hendryx M, Ducatman AM, Zullig KJ, Ahern MM, Crout R. Adult tooth loss for residents of US coal mining and Appalachian counties. Community Dent Oral Epidemiol. 2012;40(6):488–497. doi: 10.1111/j.1600-0528.2012.00691.x. [DOI] [PubMed] [Google Scholar]
- 5.National Oral Health Surveillance System. Lost 6 or more teeth: Adults aged 65+ who have lost six or more teeth due to tooth decay or gum disease. Oral Health Resources. 2010. Available at: http://apps.nccd.cdc.gov/nohss/ListV.asp?qkey=7&DataSet=2. Accessed April 1, 2013.
- 6.National Oral Health Surveillance System. Complete tooth loss: Adults aged 65+ who have lost all of their natural teeth due to tooth decay or gum disease. Oral Health Resources. 2010. Available at: http://apps.nccd.cdc.gov/nohaa/ListV.asp?qkey=8&DataSet=2. Accessed April 1, 2013.
- 7.Chu YH, Tatakis DN, Wee AG. Smokeless tobacco use and periodontal health in a rural male population. J Periodontol. 2010;81(6):848–854. doi: 10.1902/jop.2010.090310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wendell S, Wang X, Brown M et al. Taste genes associated with dental caries. J Dent Res. 2010;89(11):1198–1202. doi: 10.1177/0022034510381502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olson JC, Cuff CF, Lukomski S et al. Use of 16S ribosomal RNA gene analyses to characterize the bacterial signature associated with poor oral health in West Virginia. BMC Oral Health. 2011;11:7. doi: 10.1186/1472-6831-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin CA, McNeil DW, Crout RJ et al. Oral health disparities in Appalachia: orthodontic treatment need and demand. J Am Dent Assoc. 2008;139(5):598–604. doi: 10.14219/jada.archive.2008.0221. [DOI] [PubMed] [Google Scholar]
- 11.Susi L, Mascarenhas AK. Using a geographical information system to map the distribution of dentists in Ohio. J Am Dent Assoc. 2002;133(5):636–642. doi: 10.14219/jada.archive.2002.0239. [DOI] [PubMed] [Google Scholar]
- 12.Southward LH, Robertson A, Edelstein BL et al. Oral health of young children in Mississippi Delta child care centers: a second look at early childhood caries risk assessment. J Public Health Dent. 2008;68(4):188–195. doi: 10.1111/j.1752-7325.2007.00061.x. [DOI] [PubMed] [Google Scholar]
- 13.Southward LH, Robertson A, Wells-Parker E et al. Oral health status of Mississippi Delta 3- to 5-year-olds in child care: an exploratory study of dental health status and risk factors for dental disease and treatment needs. J Public Health Dent. 2006;66(2):131–137. doi: 10.1111/j.1752-7325.2006.tb02568.x. [DOI] [PubMed] [Google Scholar]
- 14.Nunn ME, Braunstein NS, Krall Kaye EA, Dietrich T, Garcia RI, Henshaw MM. Healthy eating index is a predictor of early childhood caries. J Dent Res. 2009;88(4):361–366. doi: 10.1177/0022034509334043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Champagne CM, Bogle ML, McGee BB et al. Dietary intake in the lower Mississippi Delta region: results from the Foods of Our Delta Study. J Am Diet Assoc. 2004;104(2):199–207. doi: 10.1016/j.jada.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Wu B, Furter R, Plassman BL, Liang J. Racial and ethnic variation in number of teeth missing among adults aged 50 and above in the US. Paper presented at: 64th Annual Scientific Meeting of the Gerontological Society of America; November 18–22, 2011; Boston, MA. [Google Scholar]
- 17.Wu B, Liang J, Plassman BL, Remle C, Luo X. Edentulism trends among middle-aged and older adults in the United States: comparison of five racial/ethnic groups. Community Dent Oral Epidemiol. 2012;40(2):145–153. doi: 10.1111/j.1600-0528.2011.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dye BA, Tan S, Smith V et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;(248):1–92. [PubMed] [Google Scholar]
- 19.Brown LJ, Wall TP, Lazar V. Trends in total caries experience: permanent and primary teeth. J Am Dent Assoc. 2000;131(2):223–231. doi: 10.14219/jada.archive.2000.0151. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. Health, United States. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Edentulism (lack of natural teeth) pp. 39–61. [Google Scholar]
- 21.National Center for Health Statistics. Health, United States. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Untreated dental caries; pp. 266–267. [Google Scholar]
- 22.Brunelle JA, Carlos JP. Recent trends in dental caries in US children and the effect of water fluoridation. J Dent Res. 1990;69(spec no):723–727. doi: 10.1177/00220345900690S141. discussion 820–723. [DOI] [PubMed] [Google Scholar]
- 23.Krause DD, May W, Cossman J. Overcoming data challenges examining oral health disparities in Appalachia. Online J Public Health Inform. 2012;4(3) doi: 10.5210/ojphi.v4i3.4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hung HC, Willett W, Ascherio A, Rosner BA, Rimm E, Joshipura KJ. Tooth loss and dietary intake. J Am Dent Assoc. 2003;134(9):1185–1192. doi: 10.14219/jada.archive.2003.0353. [DOI] [PubMed] [Google Scholar]
- 25.Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. 2003;34(1):47–52. doi: 10.1161/01.str.0000052974.79428.0c. [DOI] [PubMed] [Google Scholar]
- 26.Brennan DS, Singh KA, Liu P, Spencer A. Fruit and vegetable consumption among older adults by tooth loss and socio-economic status. Aust Dent J. 2010;55(2):143–149. doi: 10.1111/j.1834-7819.2010.01217.x. [DOI] [PubMed] [Google Scholar]
- 27.Mouden LD, Balamurugan A. Oral Health in Arkansas. Little Rock, AR: Arkansas Department of Health; 2009. [Google Scholar]
- 28. Bureau of Labor Statistics. Consumer Price Index. Available at: http://stats.bls.gov/cpi/home.htm. Accessed May 15, 2013.
- 29.Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 2 ed. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- 30.Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3 ed. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- 31.Moulton BR. An illustration of a pitfall in estimating the effects of aggregate variables on micro units. Rev Econ Stat. 1990;72(2):334–338. [Google Scholar]
- 32.Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. J Financ Quant Anal. 1989;24(3):333–355. [Google Scholar]
- 33.Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1993;3(13):19–23. [Google Scholar]
- 34.Stata User’s Guide Release 12. College Station, TX: Stata Corp LP; 2011. pp. 291–296. [Google Scholar]
- 35. Gelbach JB. When do covariates matter? And which ones, and how much? Social Science Research Network. 2009. Available at: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1425737. Accessed May 18, 2012.
- 36.Shaffer SD. Perceptions and attitudes of Mississippi Delta residents. In: Cosby AG, Brackin MW, Mason TD, McCulloch ER, editors. A Social and Economic Portrait of the Mississippi Delta. Mississippi State, MS: Social Science Research Center, Mississippi Agricultural and Forestry Experiment Station; 1992. pp. 64–89. [Google Scholar]
- 37.Neaves TT, Feierabend N, Butts CC, Weiskopf WL. A portrait of the Delta: enduring hope and enduring despair. J Health Hum Serv Adm. 2008;31(1):10–29. [PubMed] [Google Scholar]
- 38.Dye BA, Li X, Beltran-Aguilar ED. Selected oral health indicators in the United States, 2005–2008. NCHS Data Brief. 2012;(96):1–8. [PubMed] [Google Scholar]
- 39.Pitiphat W, Garcia RI, Douglass CW, Joshipura KJ. Validation of self-reported oral health measures. J Public Health Dent. 2002;62(2):122–128. doi: 10.1111/j.1752-7325.2002.tb03432.x. [DOI] [PubMed] [Google Scholar]
- 40.Gilbert GH, Duncan RP, Kulley AM. Validity of self-reported tooth counts during a telephone screening interview. J Public Health Dent. 1997;57(3):176–180. doi: 10.1111/j.1752-7325.1997.tb02970.x. [DOI] [PubMed] [Google Scholar]