Abstract
Objectives. We examined associations of household socioeconomic status (SES) and food security with children’s oral health outcomes.
Methods. We analyzed 2007 and 2008 US National Health and Nutrition Examination Survey data for children aged 5 to 17 years (n = 2206) to examine the relationship between food security and untreated dental caries and to assess whether food security mediates the SES–caries relationship.
Results. About 20.1% of children had untreated caries. Most households had full food security (62%); 13% had marginal, 17% had low, and 8% had very low food security. Higher SES was associated with significantly lower caries prevalence (prevalence ratio [PR] = 0.77; 95% confidence interval = 0.63, 0.94; P = .01). Children from households with low or very low food security had significantly higher caries prevalence (PR = 2.00 and PR = 1.70, respectively) than did children living in fully food-secure households. Caries prevalence did not differ among children from fully and marginally food-secure households (P = .17). Food insecurity did not appear to mediate the SES–caries relationship.
Conclusions. Interventions and policies to ensure food security may help address the US pediatric caries epidemic.
Tooth decay (dental caries) is the most prevalent disease worldwide and the most common pediatric disease in the United States.1,2 From 1999 to 2004, the prevalence of untreated tooth decay was 24.5% for children aged 6 to 11 years and 19.6% for adolescents aged 12 to 19 years.3 Untreated tooth decay can lead to difficulties eating and sleeping, pain, the need for invasive restorative treatment, emergency department visits and inpatient hospitalizations, poor quality of life, systemic health problems, and, in rare cases, death.4–7 To date, most public health efforts aimed at addressing the pediatric caries epidemic have focused on tooth-level interventions (e.g., topical fluorides, dental sealants). Although disparities in oral health are considered a measure of social injustice,8 comparatively less research has been conducted on the social determinants of pediatric oral health.9
Low socioeconomic status (SES), one of the strongest determinants of caries in children,10–12 is associated with food insecurity,10–17 defined as inadequate access to food resulting in food shortages, disrupted eating patterns, and hunger.18 Food insecurity, in turn, is associated with oral health–related behaviors, including increased fermentable carbohydrate intake,19,20 a risk factor for dental caries.21,22 The American Dietetic Association recognizes the link between nutrition and oral health,23 and numerous studies have drawn associations between dietary factors and disparities in dental caries.24 Collectively, these studies suggest that food insecurity is related to caries and is a potential mechanism linking SES and caries, but these relationships have not yet been evaluated empirically. We used nationally representative data from the United States to test 3 hypotheses: (1) food insecurity is positively associated with untreated dental caries, (2) food insecurity mediates the SES–caries relationship, and (3) food insecurity mediates the SES–caries relationship differentially for children from higher- versus lower-SES households.
METHODS
We conducted a cross-sectional analysis of US National Health and Nutrition Examination Survey (NHANES) data from 2007 and 2008. NHANES collects interview and physical examination data from about 5000 nationally representative children and adults each year.25 The 2007 to 2008 NHANES data set includes clinical caries data collected from participants aged 5 years and older. Trained and calibrated oral health examiners screened each child. No dental history or radiographs were taken. The survey collected aggregate data on whether the child had any untreated caries (no or yes). As part of the NHANES oral health protocol, stains, white spots, pitted enamel, and erosion were not classified as untreated caries. The child’s primary caregiver or legal guardian completed a questionnaire that produced demographic, food insecurity, and other self-reported data. Our analyses focused on children aged 5 to 17 years (n = 2206).
Conceptual Model and Variables
A preliminary conceptual model is presented in Figure 1.10–23 The outcome measure was any untreated dental caries (no or yes). Untreated dental caries is a binary variable in the 2007 to 2008 NHANES data set, which precluded an analysis of caries as a continuous variable. We chose untreated caries because it measures disease prevalence at the same time as our predictor variable and mediator were measured. Adopting alternative prevalence measures (e.g., untreated caries + fillings or restorations) would introduce temporality problems. The predictor variable was SES, operationalized as the ratio of household income to poverty, a measure used in previous analyses involving SES.26 Larger income-to-poverty ratios indicated higher SES.
FIGURE 1—
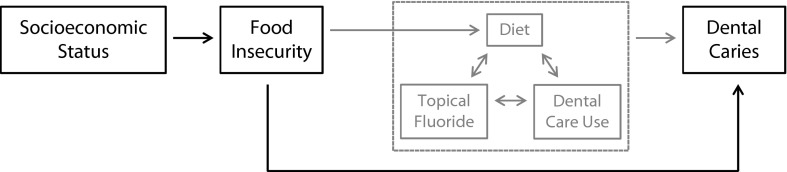
Preliminary conceptual model of relationship between socioeconomic status, food insecurity, and dental caries: National Health and Nutrition Examination Survey, United States, 2007–2008.
Note. Gray boxes and arrows indicate portions of model not tested.
The potential mediator was household-level food security (full, marginal, low, or very low food security), measured with the US Department of Agriculture 18-item Household Food Security Survey.27 We classified respondents with no affirmative responses to any survey items as living in households with full food security. We classified those with 1 to 2 affirmative responses as having marginal, 3 to 7 affirmative responses as having low, and 8 or more affirmative responses as having very low food security.28
Statistical Analyses
We used log-linear regression models to examine the SES–caries (model 1) and food insecurity–caries (model 2) relationships and to estimate prevalence ratios (PRs).29,30 In model 3, we used standard mediation methods to examine the relationship between SES and caries after including food insecurity in model 1.31 We ran similar mediation models stratified on SES (split at the median SES) to identify a potential interaction between SES and food insecurity and age-adjusted models to adjust for age as a potential model confounder. Because findings from the SES-stratified and age-adjusted models were consistent with results from the initial regression models, we only reported the latter findings. We used jackknife methods to estimate standard errors29 and accounted for the complex survey design with Stata version 12.1 (StataCorp LP, College Station, TX).
RESULTS
The mean household size was 4.7 (SD = 1.4; Table 1). Thirty-eight percent of children were Hispanic, 31% were White, and 26% were Black. Forty-three percent were privately insured, 26% were enrolled in Medicaid, 17% had other health insurance, and 14% were uninsured. Forty-three percent of children were in excellent health, 50% in very good or good health, 6% in fair health, and 1% in poor health. About 20.1% of children had untreated caries. The mean household income–to–poverty ratio was 2.1 (SD = 1.5). Most children lived in households with full food security (62%); 13% lived in households with marginal, 17% with low, and 8% with very low food security.
TABLE 1—
Household and Child Characteristics of Children Aged 5–17 Years: National Health and Nutrition Examination Survey, United States, 2007–2008
| Characteristic | No. (%) or Mean ±SD |
| Head of household education level | |
| < grade 9 | 242 (11) |
| Grade 9–11 | 416 (19) |
| High school or GED | 523 (24) |
| Some college | 589 (27) |
| ≥ college | 361 (16) |
| Missing | 75 (3) |
| Persons in household | 4.7 ±1.4 |
| Child race/ethnicity | |
| Mexican American | 563 (25) |
| Other Hispanic | 278 (13) |
| Non-Hispanic White | 689 (31) |
| Non-Hispanic Black | 575 (26) |
| Other/multiracial | 101 (5) |
| Child health insurance | |
| Private | 952 (43) |
| Medicaid only | 575 (26) |
| Other | 374 (17) |
| None | 297 (14) |
| Missing | 8 (< 1) |
| Child health condition | |
| Excellent | 959 (43) |
| Very good | 574 (26) |
| Good | 528 (24) |
| Fair | 125 (6) |
| Poor | 20 (1) |
Note. GED = general equivalency diploma. Sample size was n = 2206.
We detected a significant SES–caries relationship (Table 2). Higher SES was associated with lower untreated caries prevalence (PR = 0.77; 95% confidence interval CI = 0.63, 0.94; P = .01). Children from low or very low food security households had significantly higher untreated caries prevalence (PR = 2.00 and PR = 1.70, respectively) than children with full food security. We observed no difference in untreated caries between children from fully and marginally food-secure households (P = .17). Results from models 1 and 3 indicated that food insecurity did not partially or fully mediate SES and untreated caries. These findings were similar in the SES-stratified and age-adjusted models (data not shown).
TABLE 2—
Log-Linear Regression Model of the Relationship Between Food Security and Untreated Dental Caries in Children and Food Security as a Mediator of Socioeconomic Status and Untreated Dental Caries: National Health and Nutrition Examination Survey, United States, 2007–2008
| Variable | Untreated Dental Caries, PR (95% CI) | P |
| Model 1: socioeconomic statusa | 0.77 (0.63, 0.94) | .01 |
| Model 2 | ||
| Full food security (Ref) | 1.00 | |
| Marginal food security | 1.42 (0.85, 2.38) | .17 |
| Low food security | 2.00 (1.09, 3.65) | .03 |
| Very low food security | 1.70 (1.00, 2.90) | .049 |
| Model 3 | ||
| Socioeconomic statusa | 0.79 (0.64, 0.97) | .03 |
| Full food security (Ref) | 1.00 | |
| Marginal food security | 1.07 (0.66, 1.75) | .77 |
| Low food security | 1.42 (0.85, 2.38) | .17 |
| Very low food security | 1.12 (0.60, 2.12) | .7 |
Note. CI = confidence interval; PR = prevalence ratio.
aOperationalized as the ratio of household income to poverty.
DISCUSSION
Ours was the first published study, to our knowledge, that examined the relationship between food insecurity and untreated dental caries in children. Our analyses of nationally representative data from the United States for children aged 5 to 17 years revealed a significant relationship between food insecurity and untreated dental caries. Children living in households with low and very low food security had a greater prevalence of untreated caries than children from fully food-secure households. In addition, food insecurity did not appear to mediate the SES–caries relationship, a finding that was consistent for children from higher- and lower-SES households.
Our main finding was that food insecurity was significantly associated with dental caries. This finding is consistent with published studies demonstrating negative health outcomes associated with food insecurity.32–37 We believe there are 4 potential explanations. First, food insecurity may force caregivers and children to make food-purchasing decisions that optimize for quantity rather than quality.38–41 For example, sugar-sweetened beverages (e.g., Tang, Hawaiian Punch, Kool-Aid) are inexpensive and easily accessible. But these unhealthy drinks contain high-fructose corn syrup or some combination of sugar, sucrose, and fructose, which are risk factors for dental caries.22 Second, food-insecure households may live in food deserts, or neighborhoods where purchasing options are limited to convenience stores, corner markets, and fast-food restaurants.42 These places limit purchasing options to processed foods, snacks, and sugar-sweetened beverages and can deprive children of fresh vegetables and fruits, complex carbohydrates, nonprocessed proteins, and dairy products. Third, children living in food-insecure households may take responsibility for managing food resources,43 for example, by eating smaller amounts more frequently to make food last longer. Constant exposure to carbohydrates can lead to increased caries risk. Fourth, food insecurity may be a proxy for other markers of social inequality and deprivation, including low social capital and biological stress,44,45 both of which are associated with caries in children.46,47
Future work should examine possible mechanisms linking food insecurity and dental caries. The knowledge generated from such studies could be used to develop mechanism-specific interventions aimed at improving the oral health of children living in food-insecure households.
Our secondary findings were that food insecurity did not mediate the SES–caries relationship and that this relationship did not differ among children from lower- and higher-SES households. Although several publications suggest links between SES, food insecurity, and child health outcomes,48–50 our findings suggest that other social factors associated with SES (e.g., food environment)51 and behaviors (e.g., exposure to fluoride, visits to the dentist, specific types of nutrients and food intake)52 may be more plausible mediators. That food insecurity failed to mediate SES–caries differentially for lower- and higher-SES households was surprising but points to the complexity of these relationships. Our preliminary conceptual model suggested that behavioral factors might mediate the food insecurity–caries relationship while simultaneously moderating other relevant behavioral factors (Figure 1). It was not possible to test all the pathways from our model. Future studies could use this model as a guide to shed additional light on how household SES, food insecurity, and other social determinants of health influence behaviors relevant in children’s oral health.
The main study strength was the use of nationally representative data to test hypotheses with clinical and policy significance. Our study was a first step in developing nutrition-focused interventions aimed at improving oral health outcomes for children living in socioeconomically vulnerable households. The policy significance was that US food programs such as the Supplemental Nutrition Assistance Program and the Special Supplemental Nutrition Program for Women, Infants, and Children could strengthen implementation of evidence-based education and outreach that help households make better food choices.53–57 These programs could subsidize the purchase of fresh vegetables, fruits, meats, and dairy58 and implement wireless terminals at farmers’ markets,59,60 which would improve households’ access to healthier foods. Another policy solution is limiting purchases funded by these programs of unhealthy items (e.g., sugar-sweetened beverages) linked to adverse health outcomes and chronic conditions (e.g., dental caries, obesity, diabetes).58,61,62 However, ethical considerations associated with restrictive approaches need to be weighed in relation to the health benefits.63 The relevance of these issues to children’s oral health is open to further scientific inquiry through observational and experimental study designs.
Limitations
The analyses were cross-sectional, and all findings were associations, which do not imply causation. Food security was measured once, making it difficult to assess whether it was transient or persistent.64 Our outcome measure, untreated dental caries, was a measure of disease prevalence at a single time. Some children who recently received dental restorations could have been misclassified as not having caries, but this likely would not have affected many children because of the relatively low proportion of children who get their teeth restored.65 These limitations could be addressed through longitudinal study designs.
Our outcome was dichotomous and measured at the tooth level, which did not provide data on caries severity. In addition, the data did not specify whether caries affected primary or permanent teeth. These are limitations of 2007 and 2008 NHANES data and could be addressed with prospective studies that adopt detailed dental caries measurement protocols or secondary data that include tooth surface–specific caries measures.
SES and food insecurity were self-reported measures. We measured food security with a validated instrument, but future work could validate household-level income to ensure measure accuracy. Our models did not include other potential mediators and moderators from our conceptual model (e.g., diet, fluoride, dental visits). Additional studies are needed to fully test and refine our preliminary conceptual model.
Conclusions
Public health efforts to address food insecurity alone within vulnerable populations are unlikely to solve children’s oral health disparities. Identifying potential mediators of food insecurity and caries (e.g., fast foods, sugar-sweetened beverages, micronutrients) may allow us to develop specific nutrition-focused social and behavioral interventions for vulnerable populations. Future approaches will involve improving the food environment, quality, and choice for low-income communities; educating socioeconomically vulnerable households on healthy meal and snack preparation; and helping individuals to reduce their frequency of carbohydrate intake. Such interventions can be strengthened by reinforcing preventive oral health behaviors (e.g., fluoride use, dental visits) and are likely to reduce the prevalence of other nutrition-mediated systemic conditions such as obesity, diabetes, and cardiovascular diseases.
Acknowledgments
This study was supported by the National Institute of Dental and Craniofacial Research (grants K08DE020856, L60MD003921, T90DE021884, and U54DE019346.) and the William T. Grant Foundation Scholars Program.
Human Participant Protection
This study was exempted from protocol approval by the University of Washington institutional review board because the data were publicly available.
References
- 1.Marcenes W, Kassebaum NJ, Bernabé E et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92(7):592–597. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute of Dental and Craniofacial Research. Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Health; 2000. [Google Scholar]
- 3.Dye BA, Tan S, Smith Vet al. Trends in oral health status: United States, 1988–1994 and 1999–2004 Vital Health Stat 11 2007248)1–92. [PubMed] [Google Scholar]
- 4.Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the dmft: the human and economic cost of early childhood caries. J Am Dent Assoc. 2009;140(6):650–657. doi: 10.14219/jada.archive.2009.0250. [DOI] [PubMed] [Google Scholar]
- 5.Lee HH, Lewis CW, Saltzman B, Starks H. Visiting the emergency department for dental problems: trends in utilization, 2001 to 2008. Am J Public Health. 2012;102(11):e77–e83. doi: 10.2105/AJPH.2012.300965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chi DL, Masterson EE. A serial cross-sectional study of pediatric inpatient hospitalizations for non-traumatic dental conditions. J Dent Res. 2013;92(8):682–688. doi: 10.1177/0022034513490733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hollister MC, Weintraub JA. The association of oral status with systemic health, quality of life, and economic productivity. J Dent Educ. 1993;57(12):901–912. [PubMed] [Google Scholar]
- 8.Treadwell HM, Northridge ME. Oral health is the measure of a just society. J Health Care Poor Underserved. 2007;18(1):12–20. doi: 10.1353/hpu.2007.0021. [DOI] [PubMed] [Google Scholar]
- 9.Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23(2):201–206. doi: 10.1177/0022034511402079. [DOI] [PubMed] [Google Scholar]
- 10.Vargas CM, Crall JJ, Schneider DA. Sociodemographic distribution of pediatric dental caries: NHANES III, 1988–1994. J Am Dent Assoc. 1998;129(9):1229–1238. doi: 10.14219/jada.archive.1998.0420. [DOI] [PubMed] [Google Scholar]
- 11.Dye BA, Arevalo O, Vargas CM. Trends in paediatric dental caries by poverty status in the United States, 1988–1994 and 1999–2004. Int J Paediatr Dent. 2010;20(2):132–143. doi: 10.1111/j.1365-263X.2009.01029.x. [DOI] [PubMed] [Google Scholar]
- 12.Tellez M, Sohn W, Burt BA, Ismail AI. Assessment of the relationship between neighborhood characteristics and dental caries severity among low-income African-Americans: a multilevel approach. J Public Health Dent. 2006;66(1):30–36. doi: 10.1111/j.1752-7325.2006.tb02548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casey PH, Szeto K, Lensing S, Bogle M, Weber J. Children in food-insufficient, low-income families: prevalence, health, and nutrition status. Arch Pediatr Adolesc Med. 2001;155(4):508–514. doi: 10.1001/archpedi.155.4.508. [DOI] [PubMed] [Google Scholar]
- 14.Carter MA, Dubois L, Tremblay MS, Taljaard M. Local social environmental factors are associated with household food insecurity in a longitudinal study of children. BMC Public Health. 2012;12:1038. doi: 10.1186/1471-2458-12-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gundersen CG, Garasky SB. Financial management skills are associated with food insecurity in a sample of households with children in the United States. J Nutr. 2012;142(10):1865–1870. doi: 10.3945/jn.112.162214. [DOI] [PubMed] [Google Scholar]
- 16.Martin-Fernandez J, Grillo F, Parizot I, Caillavet F, Chauvin P. Prevalence and socioeconomic and geographical inequalities of household food insecurity in the Paris region, France, 2010. BMC Public Health. 2013;13:486. doi: 10.1186/1471-2458-13-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook JT, Frank DA. Food security, poverty, and human development in the United States. Ann N Y Acad Sci. 2008;1136:193–209. doi: 10.1196/annals.1425.001. Epub 2007 Oct 22. [DOI] [PubMed] [Google Scholar]
- 18. US Dept of Agriculture. Economic Research Center. Definitions of food security. Available at: http://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx. Accessed May 23, 2013.
- 19.Mello JA, Gans KM, Risica PM, Kirtania U, Strolla LO, Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low-income, ethnically diverse participants in a nutrition intervention study. J Am Diet Assoc. 2010;110(12):1906–1911. doi: 10.1016/j.jada.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharkey JR, Nalty C, Johnson CM, Dean WR. Children’s very low food security is associated with increased dietary intakes in energy, fat, and added sugar among Mexican-origin children (6–11 y) in Texas border colonias. BMC Pediatr. 2012;12:16. doi: 10.1186/1471-2431-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall TA, Levy SM, Broffitt B et al. Dental caries and beverage consumption in young children. Pediatrics. 2003;112(3 pt 1):e184–e191. doi: 10.1542/peds.112.3.e184. [DOI] [PubMed] [Google Scholar]
- 22.Touger-Decker R, van Loveren C. Sugars and dental caries. Am J Clin Nutr. 2003;78(4):881S–892S. doi: 10.1093/ajcn/78.4.881S. [DOI] [PubMed] [Google Scholar]
- 23.Touger-Decker R, Mobley CC American Dietetic Association. Position of the American Dietetic Association: oral health and nutrition. J Am Diet Assoc. 2007;107(8):1418–1428. doi: 10.1016/j.jada.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Mobley C, Marshall TA, Milgrom P, Coldwell SE. The contribution of dietary factors to dental caries and disparities in caries. Academic Pediatrics. 2009;9(6):410–414. doi: 10.1016/j.acap.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention. About the National Health and Nutrition Examination Survey. Available at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed August 16, 2013.
- 26.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Hyattsville, MD: National Center for Health Statistics; 2010. Obesity and socioeconomic status in adults: United States, 2005–2008. NCHS data brief 50. [Google Scholar]
- 27.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Alexandria, VA: US Dept of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 28. National Health and Nutrition Examination Survey 2007–2008 data documentation, codebook, and frequencies: food security. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/FSQ_E.htm. Accessed August 13, 2013.
- 29.Schechtman E. Odds ratio, relative risk, absolute risk reduction, and the number needed to treat—which of these should we use? Value Health. 2002;5(5):431–436. doi: 10.1046/J.1524-4733.2002.55150.x. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health. 2008;53(3):165–167. doi: 10.1007/s00038-008-7068-3. [DOI] [PubMed] [Google Scholar]
- 31.MacKinnon DP. Introduction to Statistical Mediation Analysis. New York, NY: Taylor and Francis Group; 2008. [Google Scholar]
- 32.Olson CM. Nutrition and health outcomes associated with food insecurity and hunger. J Nutr. 1999;129(2S suppl):521S–524S. doi: 10.1093/jn/129.2.521S. [DOI] [PubMed] [Google Scholar]
- 33.Cook JT, Frank DA, Berkowitz C et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–1438. doi: 10.1093/jn/134.6.##. [DOI] [PubMed] [Google Scholar]
- 34.Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr. 2005;135(12):2831–2839. doi: 10.1093/jn/135.12.2831. [DOI] [PubMed] [Google Scholar]
- 35.Belsky DW, Moffitt TE, Arseneault L, Melchior M, Caspi A. Context and sequelae of food insecurity in children’s development. Am J Epidemiol. 2010;172(7):809–818. doi: 10.1093/aje/kwq201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med. 2010;164(8):754–762. doi: 10.1001/archpediatrics.2010.117. [DOI] [PubMed] [Google Scholar]
- 37.Rose D, Bodor JN. Household food insecurity and overweight status in young school children: results from the Early Childhood Longitudinal Study. Pediatrics. 2006;117(2):464–473. doi: 10.1542/peds.2005-0582. [DOI] [PubMed] [Google Scholar]
- 38.Bauer KW, Widome R, Himes JH et al. High food insecurity and its correlates among families living on a rural American Indian Reservation. Am J Public Health. 2012;102(7):1346–1352. doi: 10.2105/AJPH.2011.300522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosas LG, Harley K, Fernals LC et al. Dietary associations of household food insecurity among children of Mexican descent: results of a binational study. J Am Diet Assoc. 2009;109(12):2001–2009. doi: 10.1016/j.jada.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating where there is not enough to eat: eating behaviors and perceptions of food among food-insecure youths. Am J Public Health. 2009;99(5):822–828. doi: 10.2105/AJPH.2008.139758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kendall A, Olson CM, Frongillo EA., Jr Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc. 1996;96(10):1019–1024. doi: 10.1016/S0002-8223(96)00271-4. [DOI] [PubMed] [Google Scholar]
- 42.Jiao J, Moudon AV, Hurvitz PM, Drewnowski A. How to identify food deserts: measuring physical and economic access to supermarkets in King County, Washington. Am J Public Health. 2012;102(10):e32–e39. doi: 10.2105/AJPH.2012.300675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fram MS, Frongillo EA, Jones SJ et al. Children are aware of food insecurity and take responsibility for managing food resources. J Nutr. 2011;141(6):1114–1119. doi: 10.3945/jn.110.135988. [DOI] [PubMed] [Google Scholar]
- 44.Dean WR, Sharkey JR. Food insecurity, social capital and perceived personal disparity in a predominantly rural region of Texas: an individual-level analysis. Soc Sci Med. 2011;72(9):1454–1462. doi: 10.1016/j.socscimed.2011.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laraia BA. Food insecurity and chronic disease. Adv Nutr. 2013;4(2):203–212. doi: 10.3945/an.112.003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pattussi MP, Hardy R, Sheiham A. The potential impact of neighborhood empowerment on dental caries among adolescents. Community Dent Oral Epidemiol. 2006;34(5):344–350. doi: 10.1111/j.1600-0528.2006.00283.x. [DOI] [PubMed] [Google Scholar]
- 47.Boyce WT, Den Besten PK, Stamperdahl J et al. Social inequalities in childhood dental caries: the convergent roles of stress, bacteria and disadvantage. Soc Sci Med. 2010;71(9):1644–1652. doi: 10.1016/j.socscimed.2010.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramsey R, Giskes K, Turrell G, Gallegos D. Food insecurity among Australian children: potential determinants, health and developmental consequences. J Child Health Care. 2011;15(4):401–416. doi: 10.1177/1367493511423854. [DOI] [PubMed] [Google Scholar]
- 49.Hadley C, Stevenson EG, Tadesse Y, Belachew T. Rapidly rising food prices and the experience of food insecurity in urban Ethiopia: impacts on health and well-being. Soc Sci Med. 2012;75(12):2412–2419. doi: 10.1016/j.socscimed.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 50.da Fonseca MA. The effects of poverty on children’s development and oral health. Pediatr Dent. 2012;34(1):32–38. [PubMed] [Google Scholar]
- 51.Gordon C, Purciel-Hill M, Ghai NR, Kaufman L, Graham R, Van Wye G. Measuring food deserts in New York City’s low-income neighborhoods. Health Place. 2011;17(2):696–700. doi: 10.1016/j.healthplace.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 52.Brennan DS, Spencer AJ, Roberts-Thomson KF. Dental self-care and visiting behaviour in relation to social inequality in caries experience. Community Dent Health. 2011;28(3):216–221. [PubMed] [Google Scholar]
- 53.Leung CW, Hoffnagle EE, Lindsay AC et al. A qualitative study of diverse experts’ views about barriers and strategies to improve the diets and health of Supplemental Nutrition Assistance Program (SNAP) beneficiaries. J Acad Nutr Diet. 2013;113(1):70–76. doi: 10.1016/j.jand.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ghirardelli A, Linares A, Fong A. Usage and recall of the Food Stamp Office Resource Kit (FSORK) by food stamp applicants in 4 California counties. J Nutr Educ Behav. 2011;43(4) supple 2:S86–S95. doi: 10.1016/j.jneb.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 55.Landers PS. The Food Stamp Program: history, nutrition education, and impact. J Am Diet Assoc. 2007;107(11):1945–1951. doi: 10.1016/j.jada.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 56.Bensley RJ, Anderson JV, Brusk JJ, Mercer N, Rivas J. Impact of internet vs traditional Special Supplemental Nutrition Program for Women, Infants, and Children nutrition education on fruit and vegetable intake. J Am Diet Assoc. 2011;111(5):749–755. doi: 10.1016/j.jada.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 57.Gerstein DE, Martin AC, Crocker N, Reed H, Elfant M, Crawford P. Using learner-centered education to improve fruit and vegetable intake in California WIC participants. J Nutr Educ Behav. 2010;42(4):216–224. doi: 10.1016/j.jneb.2009.03.125. [DOI] [PubMed] [Google Scholar]
- 58.Basu S, Seligman H, Bhattacharva J. Nutritional policy changes in the Supplemental Nutrition Assistance Program: a microsimulation and cost-effectiveness analysis. Med Decis Making. 2013;33(7):937–948. doi: 10.1177/0272989X13493971. [DOI] [PubMed] [Google Scholar]
- 59.Bertmann FM, Ohri-Vachaspati P, Buman MP, Wharton CM. Implementation of wireless terminals at farmers’ markets: impact on SNAP redemption and overall sales. Am J Public Health. 2012;102(7):e53–e55. doi: 10.2105/AJPH.2012.300727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Buttenheim AM, Havassy J, Fang M, Glyn J, Karpyn AE. Increasing supplemental nutrition assistance program/electronic benefits transfer sales at farmers’ markets with vendor-operated wireless point-of-sale terminals. J Acad Nutr Diet. 2012;112(5):636–641. doi: 10.1016/j.jand.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 61.Andreyeva T, Luedicke J, Henderson KE, Tripp AS. Grocery store beverage choice by participants in federal food assistance and nutrition programs. Am J Prev Med. 2012;43(4):411–418. doi: 10.1016/j.amepre.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 62.Andreyeva T, Luedicke J, Tripp AS, Henderson KE. Effects of reduced juice allowances in food packages for the Women, Infants, and Children program. Pediatrics. 2013;131(5):919–927. doi: 10.1542/peds.2012-3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. US Dept of Agriculture, Food and Nutrition Service. Implications of restricting the use of food stamp benefits. Available at: http://www.fns.usda.gov/ora/menu/Published/SNAP/FILES/ProgramOperations/FSPFoodRestrictions.pdf. Accessed August 20, 2013.
- 64.Ryu JH, Bartfeld JS. Household food insecurity during childhood and subsequent health status: the early childhood longitudinal study—kindergarten cohort. Am J Public Health. 2012;102(11):e50–e55. doi: 10.2105/AJPH.2012.300971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chi DL, Momany ET, Neff J et al. Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Med Care. 2011;49(2):180–192. doi: 10.1097/MLR.0b013e3181f81c16. [DOI] [PMC free article] [PubMed] [Google Scholar]


