Abstract
Our aim is to present a case of a common iliac artery pseudoaneurysm, which complicated an allograft nephrectomy. A 27-year-old woman presented with acute abdominal pain and a palpable pulsatile mass in the right iliac fossa, 1 year after a right pelvic allograft nephrectomy. An iliac pseudoaneurysm was suspected and confirmed on triplex ultrasound and CT angiography. The patient underwent a pseudoaneurysm resection with direct repair of the previous allograft Carrell patch suture dehiscence. The intervention and recovery were uneventful and after a follow-up of 6 months, the patient remains asymptomatic with no clinical or imaging recurrence of the pseudoaneurysm.Vascular complications following allograft nephrectomy are rare but may present significant morbidity and mortality. Endovascular exclusion is currently the preferred option for the management of pseudoaneurysms following allograft nephrectomy; however, open surgical approach remains an alternative for selected patients.
Background
Allograft nephrectomy is not routinely performed in all late allograft failures as it has been associated with significant morbidity (4.3–84.4%) and mortality (1.2–38%). Although patients requiring renal replacement therapy who undergo allograft resection have improved survival in comparison to those with a non-functional graft, this procedure carries a bad prognosis if subsequent retransplantation is to be performed.1–5
Vascular complications following allograft nephrectomy are rare but may be associated to significant morbidity and mortality.1–3
Our aim is to report a case of a common iliac artery pseudoaneurysm following allograft nephrectomy and to perform a literature review on this issue.
Case presentation
We present the case of a 27-year-old woman with a medical history notorious for hypertension and chronic renal failure with renal replacement therapy for 8 years, who had received a right pelvic allograft 4 years before presentation.
This allograft had been complicated by chronic rejection, and would require nephrectomy 3 years after implantation because of sepsis, with a urinary tract and cardiac septic focus.
Our patient presented with a sudden onset of right iliac fossa pain with 24 h of duration, which irradiated to the ipsilateral lumbar region. The patient had several episodes of nausea and vomiting over this period.
A painful and pulsatile mass, approximately 4 cm in diameter, was palpable in the right iliac fossa. The patient was non-feverish, haemodynamically stable and all lower limb pulses were palpable. The remaining physical examination was otherwise unremarkable.
Investigations
Haematological and biochemical laboratory values were normal, apart from elevated creatinine and urea, coincident with the usual values presented by the patient and sustained by her renal disease.
Blood bacterial and fungal cultures were performed, but no microorganism would be isolated after incubation.
Abdominal ultrasound excluded nephrolithiasis, gallbladder lithiasis, ectopic pregnancy, rupture of ovarian cyst or imaging signs suggestive of appendicitis.
Triplex ultrasound identified a pseudoaneurysm of the right common iliac artery, measuring 3.8×3.2 cm (figure 1).
Figure 1.
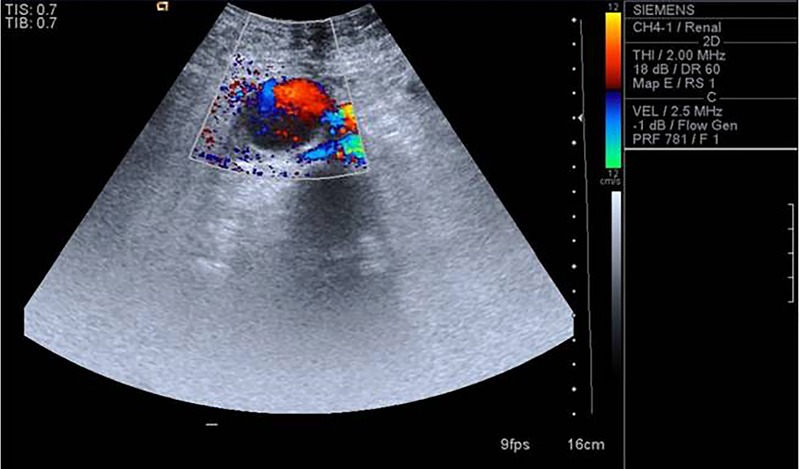
Triplex ultrasound showing a pseudoaneurysm of the right common iliac artery, measuring 3.8×3.2 cm.
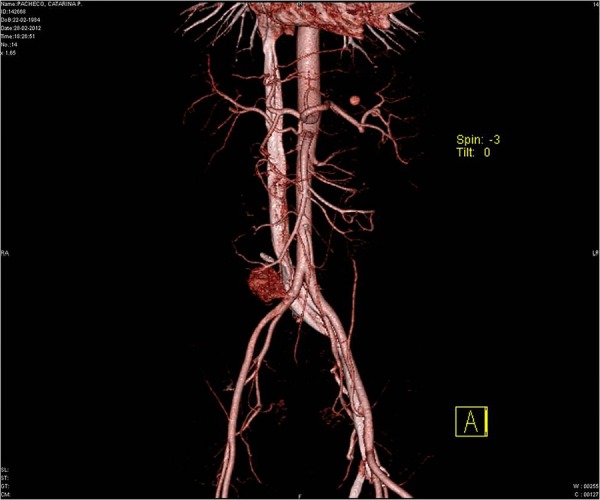
CT angiography confirmed the right common iliac artery pseudoaneurysm, measuring 4×3.9×3.7 cm (figures 2–4).
Figures 2.

CT angiography showing a right common iliac artery pseudoaneurysm, measuring 4×3.9×3.7 cm.
Figures 3.

CT angiography showing a right common iliac artery pseudoaneurysm, measuring 4×3.9×3.7 cm.
Figures 4.
CT angiography showing a right common iliac artery pseudoaneurysm, measuring 4×3.9×3.7 cm.
Differential diagnosis
In a young woman presenting with right fossa iliac pain and pulsatile mass we could think of a uterine artery pseudoaneurysm or arteriovenous malformation. However, these complications are usually related to uterine surgery or trauma, vaginal delivery or caesarean section and the patient had never been submitted to such procedures and there was no history of pregnancies.6
Given the history of endocarditis by the time of transplant nephrectomy, we could also think of an iliac mycotic aneurysm.7
Takayasu's disease is an immune arteritis causing inflammation of the aorta and its major branches, which usually occurs in young women in the second or third decade of life, and can cause aneurysms of the aorta or its branches, including the iliac arteries, but it commonly affects patients from East Asia.7
Treatment
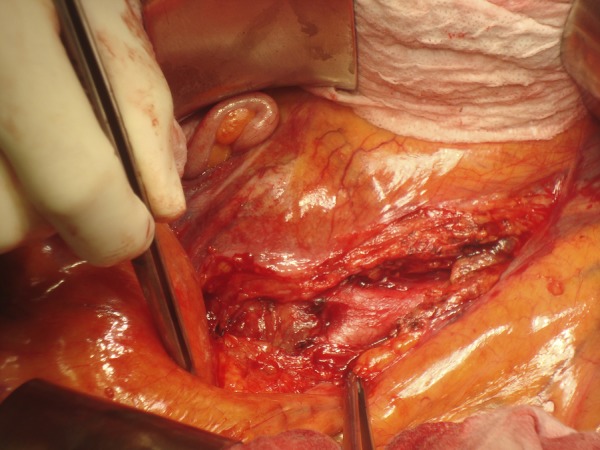
The patient underwent a resection of the pseudoaneurysm through a transperitoneal approach, with intraoperative confirmation of an anastomotic disruption of the Carrell's patch. The Carrell's patch was partially resected and the remaining defect was directly repaired (figures 5–8). The patient was started on vancomycin, while awaiting results from the blood and pseudoaneurysm biopsy tissue cultures.
Figure 5.
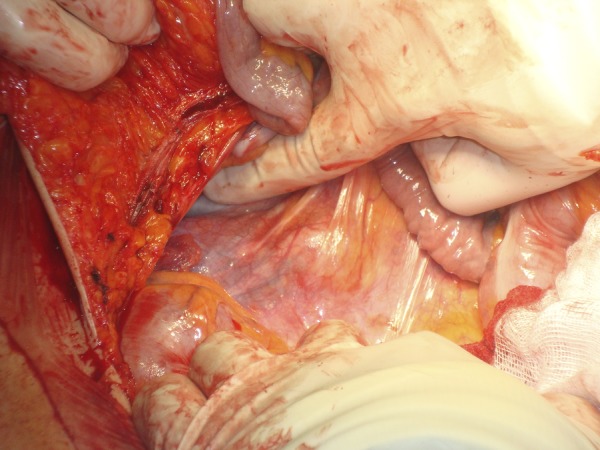
Pseudoaneurysm visualisation before opening the retroperitoneum.
Figure 6.
Aortic bifurcation and relation with the pseudoaneurysm.
Figure 7.
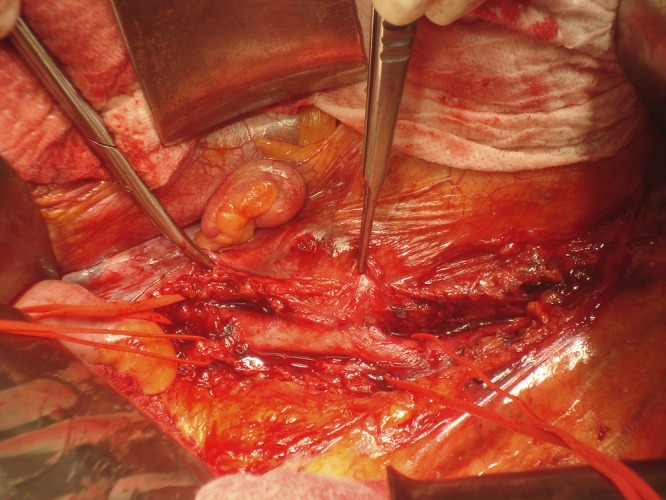
Control of the right iliac arteries and relation of the common iliac artery with the pseudoaneurysm.
Figure 8.
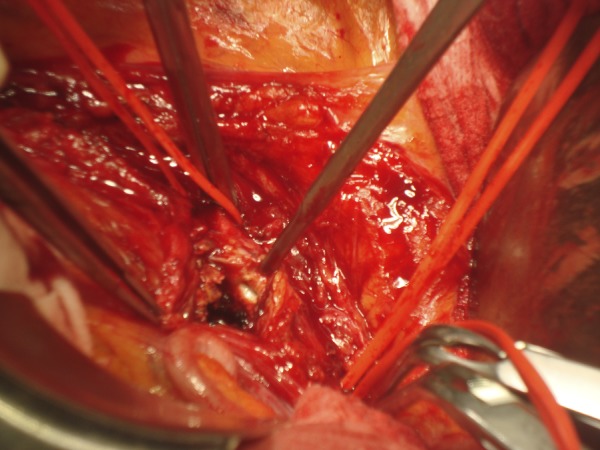
Resection of the pseudoaneurysm and visualisation of the anastomosis between the common iliac artery and the Carrell patch.
Outcome and follow-up
No complications were registered in the early postoperative period. Blood and pseudoaneurysm biopsy tissue cultures did not show any bacterial or fungal growth. After 6 months of follow-up, the patient was well, and lower limb perfusion was unchanged. No clinical recurrence was identified, which was confirmed on triplex ultrasound. No other vascular complications were detected.
Discussion
Transplant nephrectomy is indicated for early graft failure (up to 1 year following renal graft implantation), acute rejection refractory to medical therapy, symptomatic chronic rejection or when major allograft-related complications arise, such as allograft arterial or venous thrombosis, septic pyonephrosis, allograft or pseudoaneurysm rupture, uncontrollable bleeding after allograft biopsy, development of a malignant tumour, persistent haematuria, recurrent urinary tract infections with graft failure, primary disease-recurrence, organ donor lymphoma or polyomavirus nephropathy.1–3 8–10
The most common complication of allograft nephrectomy is infection, followed by bleeding. Other less frequent complications include urinary fistulae, iatrogenic bowel injury, obturator nerve or lateral cutaneous nerve injury and pseudoaneurysm of the iliac artery where the previous allograft was implanted.1 3 9 11 Allograft nephrectomy for late failure is associated with an increased complication rate and depends greatly upon surgical technique.1 11 12 To reduce the risk of iatrogenic complications, juxta-hilar allograft artery ligation has been recommended, leaving the Carrell's patch in place.2 Although the extracapsular approach has been associated with less intraoperative blood loss and lower complication rates, solely early graft failures may be resected in such a manner due to the progressive installation of an extensive pericapsular adhesion process, leaving the intracapsular approach the preferred method for late graft failure.1 3 11 However, according to a retrospective analysis performed by Mazzucchi et al,12 when compared with the extracapsular technique, the intracapsular technique was associated with less blood loss and transfusional support regardless of the timing of the surgical procedure. Other factors such as urgent allograft nephrectomy, allograft implantation near the iliac vessels, coagulopathy and local or systemic infectious processes may increase the risk of allograft nephrectomy-related complications.9
Vascular complications following allograft nephrectomy are uncommon, having been reported in 0.9–14% of cases, but are associated with poor outcomes.1 2 13 The most important risk factor for the development of such complications is local infection or sepsis by the time of the procedure, independent of the preferred surgical technique, which may lead to anastomotic disruption of the Carrell's patch with consequent pseudoaneurysm formation or rupture.1 2 14 Iliac artery pseudoaneurysm is usually clinically silent, unless adjacent structure compression produces pain. However, it may present as a pulsatile mass, fever, anaemia or rupture.14
Endovascular exclusion is currently the preferred option for the management of iliac artery pseudoaneurysm, because it is a safe and effective method, associated with less intraoperative bleeding, lower incidence of postoperative complications and a lower mortality rate, when compared to open surgery.11 3 15 Durability of endovascular repair of iliac pseudoaneurysms is still a concern however, as long-term outcomes have not been reported. Nevertheless, there are some studies comparing endovascular and open surgical repair of isolated iliac aneurysms that show a similar patency rate between the two procedures.13 16 Alternatively, conventional surgical approach with pseudoaneurysm resection can be performed and even iliac artery ligation and subsequent extra-anatomical revascularisation may be required when there is vascular injury. In these cases, an anatomic revascularisation should be avoided due to the high risk of infection and subsequent anastomotic disruption and bleeding. A two-staged approach has been advocated with initial iliac artery ligation followed by extra-anatomical revascularisation, due to the risk of infection.1 2 13 16
Our option for open surgical intervention instead of an endovascular procedure was due to the history of sepsis with identification of a urinary tract and endocarditis septic focus by the time of transplant nephrectomy, so we wanted to avoid covered stent implantation due to high suspicion of an infected pseudoaneurysm.
The transperitoneal approach was preferred as the retroperitoneal approach had been used for the allograft implant and nephrectomy.
Learning points.
Vascular complications following allograft nephrectomy are rare but may be associated with high morbidity and mortality.
Iliac artery pseudoaneurysm should be suspected in patients presenting with abdominal pain with history of allograft nephrectomy.
Endovascular exclusion is currently the preferred option for the management of iliac artery pseudoaneurysm. However, conventional surgery still remains indicated in selected cases.
Footnotes
Contributors: LB was involved in conception and design, acquisition, analysis and interpretation of data; drafting of the article and final approval given. NO, ED and IC were involved in acquisition, analysis and interpretation of data; critical review of the article and final approval given.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Akoh JA. Transplant nephrectomy. World J Transplant 2011;1:4–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eng MMP, Power RE, Hickey DP, et al. Vascular complications of allograft nephrectomy. Eur J Vasc Endovasc Surg 2006;32:212–16 [DOI] [PubMed] [Google Scholar]
- 3.Secin FP, Rovegno AR, Brunet MR, et al. Cumulative incidence, indications, morbidity and mortality of transplant nephrectomy and the most appropriate time for graft removal: only non-functioning transplants that cause intractable complications should be excised. J Urol 2003;169:1242–6 [DOI] [PubMed] [Google Scholar]
- 4.Schaefer HM, Helderman JH. Allograft nephrectomy after transplant failure: should it be performed in all patients returning to dialysis? J Am Soc Nephrol 2010;21:207–8 [DOI] [PubMed] [Google Scholar]
- 5.Johnston O, Rose C, Landsberg D, et al. Nephrectomy after transplant failure: current practice and outcomes. Am J Transplant 2007;7:1961–7 [DOI] [PubMed] [Google Scholar]
- 6.Sharma N, Ganesh D, Devi L, et al. Prompt diagnosis and treatment of uterine arcuate pseudoaneurysm: a case report and review of the literature. J Clin Diagn Res 2013;7:2303–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abularrage CJ, Arora S. Takayasu's disease, in Cronenwett and Johnston, Rutherford's vascular surgery. 7th edn Elsevier Saunders, 2010:1187–99 [Google Scholar]
- 8.Aparicio TF, López BM, Gómez BF, et al. Renal transplantectomy. Arch Esp Urol 1996;49:1079–91 [PubMed] [Google Scholar]
- 9.Durbán MM, Valor PC, Sebastian JN, et al. Non-functioning renal graft: indications for transplant excision. Arch Esp Urol 1989;42:873–8 [PubMed] [Google Scholar]
- 10.Pérez-Flores I, Sánchez-Fructuoso A, Marcén R, et al. Manejo del injerto renal falido. Nefrectomía versus embolización. Nefrología 2009;29:54–61 [DOI] [PubMed] [Google Scholar]
- 11.Touma NJ, Sener A, Caumartin Y, et al. Extracapsular versus intracapsular allograft nephrectomy: impact on allosensitization and surgical outcomes. Can Urol Assoc J 2011;5:49–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazzucchi E, Nahas WC, Antonopoulos JM, et al. Surgical complications of graft nephrectomy in the modern transplant era. J Urol 2003;170:734–7 [DOI] [PubMed] [Google Scholar]
- 13.Chaer RA, Barbato JE, Lin SC, et al. Isolated iliac artery aneurysms: a contemporary comparison of endovascular and open repair. J Vasc Surg 2008. 47:708–13 [DOI] [PubMed] [Google Scholar]
- 14.Bracale UM, Carbone F, del Guercio L, et al. External iliac artery pseudoaneurysm complicating renal transplantation. Interact Cardiovasc Thorac Surg 2009;8:654–60 [DOI] [PubMed] [Google Scholar]
- 15.Diller R, Holzen J, Senninger N, et al. Interventional stenting for ruptured iliac aneurysm following transplant nephrectomy. Transplant Proc 2006;38:718–20 [DOI] [PubMed] [Google Scholar]
- 16.Pitoulias GA, Donas KP, Schulte S, et al. Isolated iliac artery aneurysms: endovascular versus open elective repair. J Vasc Surg 2007;46:648–54 [DOI] [PubMed] [Google Scholar]


