Abstract
Bile acids are important endocrine signalling molecules, modulating glucose homeostasis through activation of cell surface and nuclear receptors. Bile acid metabolism is altered in type 2 diabetes mellitus; however, whether this is of pathogenic consequence is not fully established. In this study urinary bile acid excretion in individuals with type 2 diabetes and matched healthy volunteers was assessed. Urinary bile acid excretion in type 2 diabetes patients was considered in the context of prevailing glycaemia and the patient body mass index. Urine bile acids were measured by liquid chromatography-tandem mass spectrometry, allowing individual quantification of 15 bile acid species. Urinary bile acid excretion in patients with type 2 diabetes who were normal weight (BMI 18.5–24.9 kg/m2) and overweight (BMI 25–29.9 kg/m2) were elevated compared to healthy normal weight volunteers, both p<0.0001. In obese (BMI≥30 kg/m2) type 2 diabetes patients, urinary bile acid excretion was significantly lower than in the normal and overweight type 2 diabetes groups (both p<0.01). Total bile acid excretion positively correlated with HbA1c in normal (rs = 0.85, p = <0.001) and overweight (rs = 0.61, p = 0.02) but not obese type 2 diabetes patients (rs = −0.08, p = 0.73). The glycaemia-associated increases in urine bile acid excretion in normal weight and overweight type 2 diabetes seen in this study may represent compensatory increases in bile acid signalling to maintain glucose homeostasis. As such alterations appear blunted by obesity; further investigation of weight-dependent effects of bile acid signalling on type 2 diabetes pathogenesis is warranted.
Introduction
Bile acids are important endocrine molecules, initiating signalling by the nuclear farnesoid X receptor (FXR) and G-protein coupled receptor, TGR5 [1]. Bile acid signalling exerts diverse influence over glucose, lipid and energy homeostasis, functions additional to the classical role of bile acids in lipid solubilisation and absorption in the intestine [2].
In the L-cells of the intestinal epithelium, TGR5 activation by bile acids stimulates the release of gut hormones such as glucagon-like peptide-1 (GLP-1) [3], resulting in improved glucose homeostasis [4]. In plasma, bile acid concentrations rise rapidly in response to glucose ingestion, which likely underpins many of the mechanisms by which bile acids play a role in regulation of the body's response to food intake [5]. In pancreatic β-cells TGR5 and FXR activation enhances insulin secretion [6], [7],whilst in the liver, FXR activation may inhibit gluconeogenesis, whilst increasing glycogen synthesis and improving hepatic insulin sensitivity, although a role for FXR in gluconeogenesis remains controversial [1]. Glucose itself stimulates expression of cholesterol 7α-hydroxylase, which catalyses the rate-limiting step in bile acid production [8], [9].
Many diabetes-associated changes in bile acid metabolism have been reported; these include altered synthetic rate (both increased and decreased synthesis reported), pool size and composition of bile acid species [10]–[14]. Lowering of the bile acid pool size using a synthetic FXR agonist reduces energy expenditure and induces obesity and diabetes in mice [15]. Moreover, bile acid sequestrant therapy improves glycaemic control in type 2 diabetes, in addition to its lipid-lowering action [16], [17].
Obesity increases the risk of type 2 diabetes mellitus, and the prevalence of both continues to rise annually [18]. Weight loss, by changes in lifestyle or metabolic surgery, improves glycaemia in type 2 diabetes [19]–[21].The beneficial impact of Roux-en-Y gastric bypass surgery on diabetes control is associated with enhanced β-cell function and improved insulin sensitivity which has been attributed, in part, to an exaggerated post-prandial GLP-1 response [22]–[24]. Fasting plasma bile acids are lower in overweight and severely obese individuals compared to those post-RYGB [25]. Further, obesity blunts post-prandial plasma bile acid response relative to responses in normal weight individuals [26], although obese patients with type 2 diabetes mellitus exhibit greater post-prandial response of plasma bile acid compared to normoglycaemic obese patients [27].
Despite the large body of literature supporting a critical role for bile acids in glucose homeostasis in health and disease, the precise relationship between bile acids and prevailing glycaemia in type 2 diabetes remains ill defined, as does whether this relationship is affected by body weight. Therefore, in this study we investigated the relationship of urinary bile acid excretion with glycated haemoglobin (HbA1c), in a well characterised cohort of people with type 2 diabetes mellitus. Bile acids escaping first pass hepatic clearance reach the circulation and a proportion are subject to glomerular filtration [28]. Whilst up to 97% of the bile acids are recaptured in the proximal renal tubule via the membrane transporter proteins ASBT and OSTα, a small amount ends up in urine. Importantly, urinary bile acid concentration, when expressed as a creatinine ratio, correlates extremely well with fasting plasma values [29]. Therefore, urine provides an excellent, non-invasive matrix in which to investigate glycaemia-associated changes in bile acid concentrations. We hypothesised that in patients with type 2 diabetes there is a compensatory increase of bile acids, possibly mediated by an increase in plasma glucose. Furthermore, we hypothesised that this compensatory increase may be influenced by weight gain.
Methods and Materials
Ethics statement
The study was approved by the King's College Hospital NHS Foundation Trust Research Ethics Committee (reference number 05/Q0703/4). Written informed consent was obtained from all participants in the study.
Samples
Fifty urine samples from patients with type 2 diabetes and 15 from non-diabetic controls were studied. Urine bile acid measurements were performed using early morning first pass urine samples taken for clinical purposes. Sample aliquots were frozen on the same day and stored at −20°C prior to analysis. Electronic patient records were accessed to confirm the people with diabetes were treated by only lifestyle change and/or metformin, had normal albumin:creatinine ratios (men <2.5 mg/mmol, women <3.5 mg/mmol) and had date-matched HbA1c and body mass index (BMI) measurements. All study participants had normal renal function (eGFR>90 mL/min/1.73 m2), normal thyroid function (thyroid stimulating hormone 0.3–5.5 mIU/L) and normal liver function (albumin 35–50 g/L, aspartate aminotransferase <50 IU/L, alkaline phosphatase <130 IU/L, bilirubin <20 µmol/L). Patients using insulin, GLP-1 receptor analogue or dipeptidyl peptidase 4 (DDP4) inhibitor therapies were excluded. The samples were grouped by BMI of the donor, according to World Health Organisation criteria (BMI<24.99 kg/m2 = normal; 25–29.99 kg/m2 = overweight, obese = ≥30 kg/m2) [30]. Statin use across type 2 diabetes subgroups was uniform. Control samples were obtained from 12 non-diabetic volunteers, recruited from the laboratory.
Assay methods
HbA1c was measured by boronate affinity chromatography using a Primus Ultra2 HPLC system (Primus Diagnostics, Kansas City, USA). Urine creatinine measurement was performed using a kinetic Jaffé reaction on an Advia 2400 analyser (Siemens Healthcare Diagnostics, Frimley, UK).
Bile acid conjugate hydrolysis
Urinary bile acid profiles exhibit great complexity [31], [32]. Glucuronidated and sulphated species are found at higher concentrations than in plasma, and would not be detected by the mass spectrometry method used, which only measures glycine-, taurine- and unconjugated cholic, chenodeoxycholic, deoxycholic, ursodeoxycholic and lithocholic acid species. Thus, enzymatic digestion using Helix pomatia extract (which contains high sulphatase and glucuronidase activities) was utilised to remove glucuronide and sulphate conjugations using an existing protocol [33]. Briefly, internal standard was added to 10 mL urine and the urine then extracted on Sep-Pak columns, eluted in methanol and dried under nitrogen. Urine residues were then dissolved in 5 mL 0.5 M sodium acetate containing 10 mg/mL of H. pomatia powder and 20 mg/mL of sodium ascorbate (to inhibit cholesterol oxidase activity) for 72 h at 37°C. Freed bile acids were then re-extracted on Sep-Pak columns, eluted and dried. Dried solvolysis and enzyme-treated samples were re-suspended in 250 µL of a 50∶50 (v/v) mix of mobile phases A and B. 10 µL of this solution was injected onto the column (equal to 0.4 mL of the original urine sample).
High performance liquid chromatography tandem mass spectrometry method
Bile acid measurement was carried out using an existing high performance liquid chromatography tandem mass spectrometry (LC-MS/MS) method [26], [34]. The method uses an Acentis fused-core C18 analytical column (150×4.6 mm, particle size 2.7 µm, Sigma-Aldrich) on a Jasco LC2000 series HPLC system attached to an API 3200 triple quadrupole mass spectrometer (Applied Biosystems, Cheshire, UK). Mobile phases comprised (A) methanol or (B) deionised H2O, each containing 5 mM ammonium acetate (w/v) and 0.012% formic acid (v/v). Negative ion mass spectra of the fractionated bile acids were recorded in multiple reaction-monitoring mode. Data were captured using Analyst Software version 1.4.2 (Applied Biosystems) and quantitation carried out by peak area analysis corrected to internal standards (a 2,2,4,4,d4-deoxycholic acid for each of the bile acid chemistries; unconjugated, glycine- and taurine-conjugated). For quantitation, a bile acid calibration curve was prepared using bile acid standards dissolved in charcoal-stripped urine in the concentration range 500–20,000 nmol/L. Urine bile acid concentrations in the study group were normalised to urinary creatinine concentration. Lower limit of quantitation for each bile acid was 0.1 µmol/L, intraassay coefficients of variation for each bile acid were in the range 2.8–12.1% whilst interassay precisions were between 1.6–13.6% [26].
Presentation of bile acid profile: the bilogram
Bile acid data are presented according to biological groupings in a bilogram. The primary bile acids cholic and chenodeoxycholic acids are synthesised in the liver under the control of 7α-hydroxylase. These can be conjugated with either glycine or taurine, giving rise to four primary conjugated species. Bacterial action in the intestine leads to the formation of the secondary bile acids deoxycholic acid, lithocholic acid and ursodeoxycholic acid. Each can be conjugated with glycine or taurine giving rise to six secondary-conjugated bile acids. The bilogram thus shows the primary, primary conjugated, secondary and secondary conjugated bile acids. Total bile acid, total unconjugated, total glycine-conjugated and total taurine-conjugated values are also given in the bilogram.
Statistical analysis
Statistical analysis was performed using Analyse-It® (version 2.21, Leeds, U.K.). Data were tested for normality using a Shapiro-Wilk test and were not normally distributed. Comparison across multiple groups was performed using Kruskal-Wallis ANOVA. Pair-wise comparisons were performed using Mann-Whitney U tests with post-hoc Bonferroni correction. Spearman correlation plots were produced for urinary bile acid excretion with various variables. Data is reported as median and interquartile ranges (IQR).Values of P<0.05 were taken as statistically significant.
Results
The demographics of the sample donors are shown in table 1. The 15 control volunteers were aged 50 (29.3–61) [median (IQR)] years and had a BMI of 23 (20–24) kg/m2. The 50 type 2 diabetes mellitus patients were aged 62 (47–74) years and had a BMI of 30 (27–32) kg/m2 and HbA1c of 8.1 (6.8–9.1)% [65.5 (51.0–76.2) mmol/mol]. BMI, age, HbA1c and urinary creatinine differences did not reach statistical significance between the groups (Table 1). The bilogram shown in Table 2 details urinary bile acid excretion in both groups. The total bile acid excretion was significantly higher in the type 2 diabetes group at 877.4 (406.7–1454.5) nmol/mmol creatinine than in the control group at 124.6 (53.1–172.5) nmol/mmol creatinine (p = <0.0001) (Table 2). Statistically significant differences in urinary bile acid excretion between control and type 2 diabetes mellitus samples were observed in 13 of the 15 individual bile acid species measured (Table 2). In both groups, the glycine-conjugated bile acids were the most abundant species, with the secondary bile acid glycodeoxycholic acid being excreted in the highest amounts (Table 2).
Table 1. Demographics of the study cohort.
| Healthy volunteers | All T2DM data | Normal BMI T2DM | Overweight T2DM | Obese T2DM | P value | |
| Number | 15 | 50 | 14 | 15 | 21 | - |
| Male/female | 8/7 | 30/20 | 10/4 | 8/7 | 12/9 | NS† |
| Age (years) | 50.0 (29.3–61.0) | 61.0 (45.9–75.0) | 53.0 (42.8–66.4) | 65.0 (48.8–75.0) | 61.0 (47.7–77.3) | NS |
| BMI (kg/m2) | 23 (20–24) | 30 (27–32) | 23 (20–25) | 28 (27–30) | 34 (32–40) | - |
| HbA1c % (mmol/mol Hb) | Not measured | 8.1 (6.8–9.1) [65.5 (51.0–76.2)] | 6.6 (5.9–8.7) [48.5 (40.8–71.4)] | 8.2 (7.4–9.5) [66.0 (57.2–80.2)] | 8.2 (7.3–9.0) [66.0 (56.7–75.3)] | NS |
| Urine creatinine (mmol/L) | 8.7 (6.4–16.7 | 7.8 (5.5–12.6) | 10.7 (5.2–17.0) | 7.9 (6.2–12.5) | 7.5 (5.4–9.1) | NS |
Data presented as median and interquartile range. Abbreviations: T2DM, type 2 diabetes mellitus; BMI, body mass index; HbA1c, glycated haemoglobin; NS, not significant. P values were obtained by Kruskal-Wallis ANOVA and Chi-square test (†). P<0.05 was taken as statistically significant.
Table 2. Median urinary bile acid excretion in healthy volunteers and type 2 diabetes mellitus.
| Bile acid | Healthy volunteers | All T2DM data | P value healthy vs T2DM |
| Total bile acids | 124.6 (53.1–172.5) | 877.4 (406.7–1454.5) | <0.0001 |
| Total unconjugated | 14.7 (6.9–24.1) | 128.7 (84.1–235.3) | <0.0001 |
| Total glycine-conjugated | 88.3 (43.6–126.1) | 586.5 (281.7–1034.9) | <0.0001 |
| Total taurine-conjugated | 19.8 (4.2–27.1) | 60.2 (17.8–130.3) | 0.0008 |
| Primary | |||
| Cholic acid | 2.4 (1.6–6.9) | 34.0 (12.9–71.4) | <0.0001 |
| Chenodeoxycholic acid | 1.0 (0.4–3.1) | 10.5 (5.6–29.0) | <0.0001 |
| Primary conjugated | |||
| Glycocholic acid | 16.1 (12.6–27.4) | 44.4 (17.2–128.5) | 0.003 |
| Taurocholic acid | 2.2 (1.2–2.9) | 6.0 (2.1–13.4) | 0.01 |
| Glycochenodeoxycholic acid | 11.5 (5.3–21.7) | 100.4 (42.3–148.1) | <0.0001 |
| Taurochenodeoxycholic acid | 3.7 (1.6–7.3) | 7.1 (3.3–17.3) | NS |
| Secondary | |||
| Deoxycholic acid | 6.0 (3.8–8.4) | 42.0 (15.3–91.3) | <0.0001 |
| Ursodeoxycholic acid | 1.8 (1.1–3.5) | 10.1 (4.6–26.1) | <0.0001 |
| Lithocholic acid | 0.6 (0.2–1.8) | 8.6 (4.5–15.8) | <0.0001 |
| Secondary conjugated | |||
| Glycodeoxycholic acid | 25.1 (15.6–39.2) | 187.6 (82.0–433.1) | <0.0001 |
| Taurodeoxycholic acid | 1.9 (0.8–3.6) | 10.5 (2.4–22.9) | 0.0006 |
| Glycoursodeoxycholic acid | 5.3 (2.8–13.4) | 58.9 (22.5–94.7) | <0.0001 |
| Tauroursodeoxycholic acid | 0.9 (0.6–1.3) | 2.1 (0.75–9.0) | NS |
| Glycolithocholic acid | 10.4 (7.0–24.7) | 118.1 (27.1–256.0) | <0.0001 |
| Taurolithocholic acid | 5.3 (1.0–8.5) | 18.0 (3.4–45.8) | 0.006 |
Urinary bile acid excretion expressed as nmol bile acid/mmol creatinine. Data presented as median and inter-quartile range. Mann-Whitney tests were used to compare differences in urinary bile acid excretion between the two groups. NS, not significant. P<0.05 was taken as statistically significant.
When the type 2 diabetes mellitus group was subdivided according to BMI, Kruskal-Wallis ANOVA revealed there to be significant differences in urinary bile acid excretion between the healthy volunteers and normal weight, overweight and obese type 2 diabetes groups. Comparison of the healthy controls to either the normal weight or overweight type 2 diabetes mellitus groups demonstrated significant increases in urinary bile acid excretion in type 2 diabetes for all bile acid species, with the exception of taurochenodeoxycholic acid (controls vs. normal weight or overweight type 2 diabetes) and tauroursodeoxycholic acid (controls vs. overweight type 2 diabetes) (Table 3). In contrast, when urinary bile acid excretion in healthy volunteers and obese type 2 diabetes was compared, significant increase in excretion were seen in only seven out of 15 bile acid species studied (cholic acid, chenodeoxycholic acid and its glycine conjugate, deoxycholic acid and its glycine conjugate, ursodeoxycholic acid and its glycine conjugate and lithocholic acid and its glycine conjugate). Next, urinary bile acid excretion in normal weight type 2 diabetes was compared to that in both the overweight and obese type 2 diabetes groups. There was no difference in excretion between the normal weight and overweight type 2 diabetes groups (Table 3). However, urinary bile acid excretion in the obese type 2 diabetes group was significantly lower for the bile acids glycochenodeoxycholic acid, deoxycholic acid (and its glycine conjugate) and glycine and taurine-conjugated ursodeoxycholic acid, relative to normal weight type 2 diabetes (Table 3). Similar results were seen when the overweight and obese type 2 diabetes mellitus groups were compared, with the exception that cholic acid and its taurine conjugate, as well as glycolithocholic acid, were also significantly lower in the obese (Table 3). Relative proportions of primary and secondary bile acids were not different between control and type 2 diabetes samples (irrespective of patient BMI) (Table 3).
Table 3. Comparison of median urinary bile acid excretion between healthy volunteer and type 2 diabetes mellitus groups classified according to BMI.
| P value | ||||||||||
| Bile acid | Healthy volunteers | Normal weight T2DM | Overweight T2DM | Obese T2DM | Volunteer vs normal weight T2DM | Volunteer vs overweight T2DM | Volunteer vs obese T2DM | Normal weight T2DM vs overweight T2DM | Normal weight T2DM vs obese T2DM | Overweight T2DM vs obeseT2DM |
| Total bile acids | 124.6 (53.1–172.5) | 1298.6 (969.2–1708.9) | 1163.2 (503.8–2713.6) | 385.9 (190.0–719.3) | <0.0001 | <0.0001 | <0.001 | NS | <0.01 | <0.01 |
| Total unconjugated | 14.7 (6.9–24.1) | 123.1 (130.7 288.3) | 158.7 (102.0–313.7) | 84.6 (47.3–125.2) | <0.0001 | <0.0001 | <0.001 | NS | <0.01 | 0.03 |
| Total glycine-conjugated | 88.3 (43.6–126.1) | 1027.0 (731.4–1268.3) | 788.7 (357.6–1238.8) | 258.9 (113.7–505.6) | <0.0001 | <0.0001 | <0.01 | NS | <0.01 | <0.01 |
| Total taurine-conjugated | 19.8 (4.2–27.1) | 184.7 (51.7–150.4) | 62.7 (40.4–183.2) | 18.2 (9.3–85.2) | <0.0001 | <0.001 | NS | NS | 0.02 | NS |
| Primary | NS | |||||||||
| Cholic acid | 2.4 (1.6–6.9) | 35.7 (18.3–65.0) | 58.7 (35.8–126.6) | 12.9 (6.9–47.8) | <0.0001 | <0.0001 | 0.002 | NS | NS | <0.01 |
| Chenodeoxycholic acid | 1.0 (0.4–3.1) | 10.5 (7.2–29.0) | 16.2 (7.4–30.8) | 7.2 (2.0–25.1) | <0.0001 | <0.0001 | 0.002 | NS | NS | NS |
| Primary conjugated | NS | |||||||||
| Glycocholic acid | 16.1 (12.6–27.4) | 72.9 (24.6–173.8) | 72.0 (28.8–166.3) | 34.6 (12.7–54.4) | 0.007 | 0.002 | NS | NS | NS | NS |
| Taurocholic acid | 2.2 (1.2–2.9) | 12.4 (3.5–19.0) | 10.3 (4.6–25.5) | 5.6 (1.3–7.6) | 0.001 | <0.01 | NS | NS | NS | 0.04 |
| Glycochenodeoxycholic acid | 11.5 (5.3–21.7) | 135.8 (82.1–148.1) | 140.4 (65.2–246.7) | 56.0 (19.6–103.3) | <0.0001 | <0.0001 | 0.002 | NS | 0.01 | 0.03 |
| Taurochenodeoxycholic acid | 3.7 (1.6–7.3) | 10.0 (4.2–37.5) | 8.5 (4.6–33.6) | 4.0 (1.8–8.2) | NS | NS | NS | NS | NS | NS |
| Secondary | ||||||||||
| Deoxycholic acid | 6.0 (3.8–8.4) | 87.0 (51.5–107.6) | 51.1 (34.5–122.5) | 16.3 (12.6–37.5) | 0.0003 | <0.0001 | <0.01 | NS | <0.01 | <0.01 |
| Ursodeoxycholic acid | 1.8 (1.1–3.5) | 20.2 (10.0–31.9) | 9.3 (7.1–19.8) | 6.5 (4.1–32.6) | <0.0001 | <0.0001 | 0.002 | NS | NS | NS |
| Lithocholic acid | 0.6 (0.2–1.8) | 9.7 (5.8–15.6) | 11.1 (6.7–18.6) | 5.0 (0.8–15.8) | <0.0001 | <0.0001 | 0.03 | NS | NS | NS |
| Secondary conjugated | ||||||||||
| Glycodeoxycholic acid | 25.1 (15.6–39.2) | 455.1 (236.2–641.6) | 243.7 (112.9–480.0) | 60.9 (39.5–187.0) | <0.0001 | <0.0001 | 0.002 | NS | <0.01 | NS |
| Taurodeoxycholic acid | 1.9 (0.8–3.6) | 15.1 (6.1–27.2) | 14.1 (6.7–19.7) | 3.7 (0.8–19.5) | <0.0001 | 0.0004 | NS | NS | NS | NS |
| Glycoursodeoxycholic acid | 5.3 (2.8–13.4) | 80.7 (43.6–123.7) | 67.3 (29.1–131.6) | 22.2 (11.8–63.0) | <0.0001 | <0.0001 | 0.005 | NS | <0.01 | 0.02 |
| Tauroursodeoxycholic acid | 0.9 (0.6–1.3) | 6.5 (1.6–16.8) | 4.0 (0.5–8.1) | 1.1 (0.3–2.5) | 0.002 | NS | NS | NS | NS | NS |
| Glycolithocholic acid | 10.4 (7.0–24.7) | 208.6 (58.7–300.1) | 122.3 (108.5–335.0) | 34.6 (22.8–144.8) | 0.001 | <0.0001 | 0.02 | NS | NS | 0.03 |
| Taurolithocholic acid | 5.3 (1.0–8.5) | 26.5 (8.5–51.4) | 21.0 (9.6–61.0) | 4.5 (1.5–40.1) | 0.003 | 0.002 | NS | NS | NS | NS |
Urinary bile acid excretion expressed as nmol bile acid/mmol creatinine. Mann-Whitney test with Bonferroni correction (following prior Kruskal-Wallis ANOVA) was used to compare differences in excretion between 1) healthy volunteers and T2DM subgroups and 2) in the BMI 25–30 and BMI>30 groups relative to normal weight T2DM (BMI<25). Individual P values are indicated. P<0.05 was taken as statistically significant. NS = not significant.
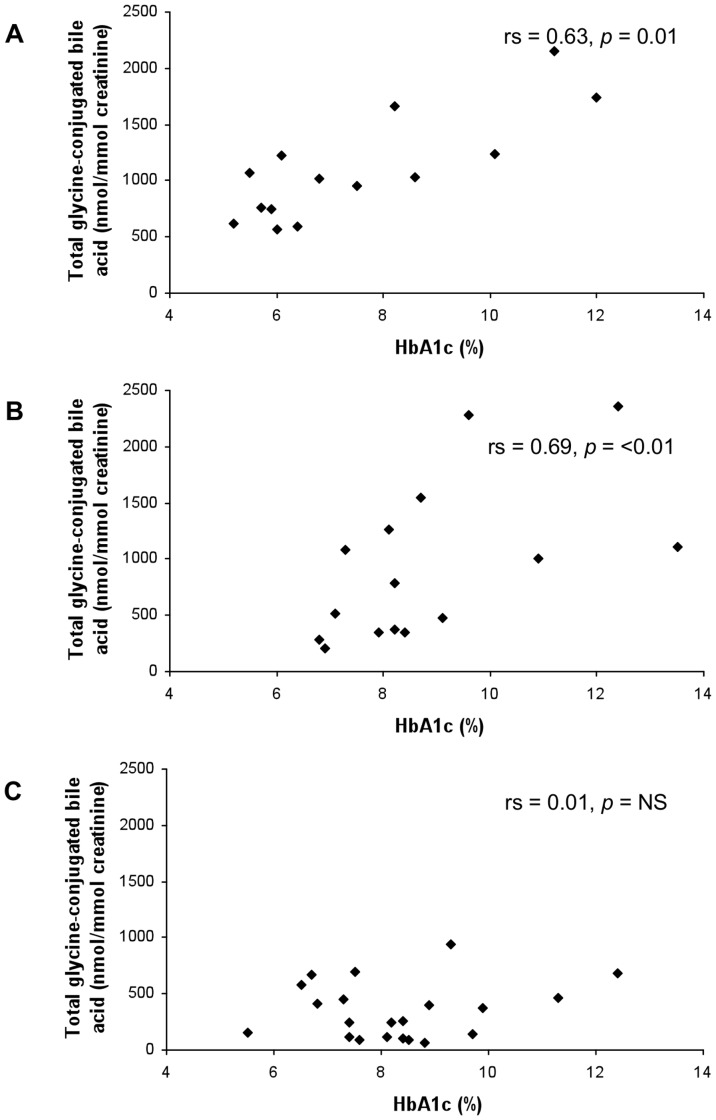
To assess whether the increased urinary bile acid excretion seen in type 2 diabetes mellitus was related to glycaemia, Spearman correlation plots were constructed for HbA1c with urine bile acid data (Table 4). When all type 2 diabetes data were considered, no correlation with HbA1c was observed (Table 4). However, in normal weight type 2 diabetes, total, total unconjugated and total glycine-conjugated urinary bile acid excretion were positively correlated with HbA1c (Table 4, Figure 1, representative graphs for total glycine conjugated bile acid excretion). In contrast, taurine-conjugated urinary bile acid excretion was not associated with glycaemic control (Table 4). The secondary bile acid deoxycholic acid and its glycine conjugate, as well as lithocholic acid demonstrated the most statistically significant correlation with glycaemia.
Table 4. Correlation of urinary bile acid excretion with glycaemic control in type 2 diabetes mellitus.
| All T2DM data | Normal weight T2DM | Overweight T2DM | Obese T2DM | |||||
| rs | P | rs | P | rs | P | rs | P | |
| Total bile acids | 0.19 | 0.18 | 0.85 | <0.001 | 0.61 | 0.02 | −0.08 | NS |
| Total unconjugated | 0.24 | 0.09 | 0.83 | <0.001 | 0.62 | 0.01 | −0.05 | NS |
| Total glycine-conjugated | 0.18 | 0.21 | 0.69 | <0.01 | 0.63 | 0.01 | 0.01 | NS |
| Total taurine conjugated | 0.03 | 0.82 | −0.12 | NS | 0.44 | NS | −0.14 | NS |
| Primary | ||||||||
| Cholic acid | 0.08 | 0.57 | 0.13 | NS | 0.56 | 0.03 | −0.16 | NS |
| Chenodeoxycholic acid | 0.11 | 0.43 | 0.27 | NS | 0.59 | 0.02 | −0.25 | NS |
| Primary conjugated | ||||||||
| Glycocholic acid | 0.09 | 0.53 | −0.14 | NS | 0.47 | NS | 0.06 | NS |
| Taurocholic acid | 0.08 | 0.60 | −0.24 | NS | 0.63 | 0.01 | −0.07 | NS |
| Glycochenodeoxycholic acid | 0.13 | 0.37 | 0.05 | NS | 0.50 | NS | 0.17 | NS |
| Taurochenodeoxycholic acid | 0.03 | 0.83 | −0.06 | NS | 0.57 | 0.03 | −0.26 | NS |
| Secondary | ||||||||
| Deoxycholic acid | 0.14 | 0.33 | 0.82 | <0.001 | 0.41 | NS | −0.38 | NS |
| Ursodeoxycholic acid | 0.05 | 0.71 | 0.03 | NS | 0.40 | NS | −0.01 | NS |
| Lithocholic acid | 0.25 | 0.08 | 0.56 | 0.04 | 0.75 | <0.01 | −0.17 | NS |
| Secondary conjugated | ||||||||
| Glycodeoxycholic acid | 0.17 | 0.2433 | 0.81 | <0.001 | 0.70 | <0.01 | −0.18 | NS |
| Taurodeoxycholic acid | 0.04 | 0.7839 | 0.11 | NS | 0.24 | NS | −0.08 | NS |
| Glycoursodeoxycholic acid | 0.13 | 0.38 | 0.30 | NS | 0.28 | NS | 0.15 | NS |
| Tauroursodeoxycholic acid | −0.09 | 0.55 | −0.44 | NS | 0.20 | NS | 0.09 | NS |
| Glycocholic acid | 0.09 | 0.53 | −0.14 | NS | 0.47 | NS | 0.06 | NS |
| Taurolithocholic acid | 0.07 | 0.61 | 0.28 | NS | 0.35 | NS | −0.31 | NS |
Spearman correlation plots were constructed for urinary bile acid excretion and HbA1c, the preferred marker of glycaemic control. Correlation (rs) and P values are indicated. P<0.05 was taken as statistically significant. NS = not significant.
Figure 1. HbA1c plotted against total glycine-conjugated bile acid urinary excretion for normal weight (A), overweight (B) and obese (C) type 2 diabetes mellitus groups.
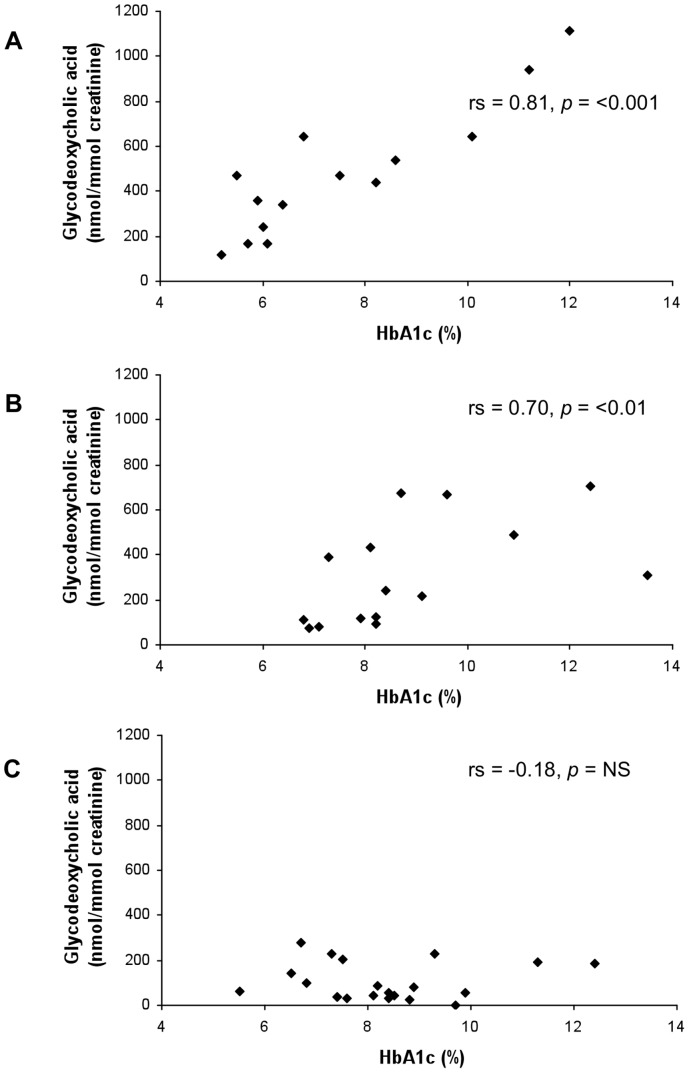
In the overweight type 2 diabetes group, total, total unconjugated and total glycine-conjugated urinary bile acid excretion showed positive correlation with HbA1c; however, the correlation was not as strong as for normal weight type 2 diabetes mellitus (Table 4). In this group, significant correlations between the primary bile acids cholic acid and chenodeoxycholic acid, and the secondary bile acids glycodeoxycholic acid, lithocholic acid and glycolithocholic acid with glycaemic control were seen (Table 4, Figure 2).
Figure 2. HbA1c plotted against glycodeoxycholic acid urinary excretion for (A) normal weight, (B) overweight and (C) obese type 2 diabetes mellitus groups.
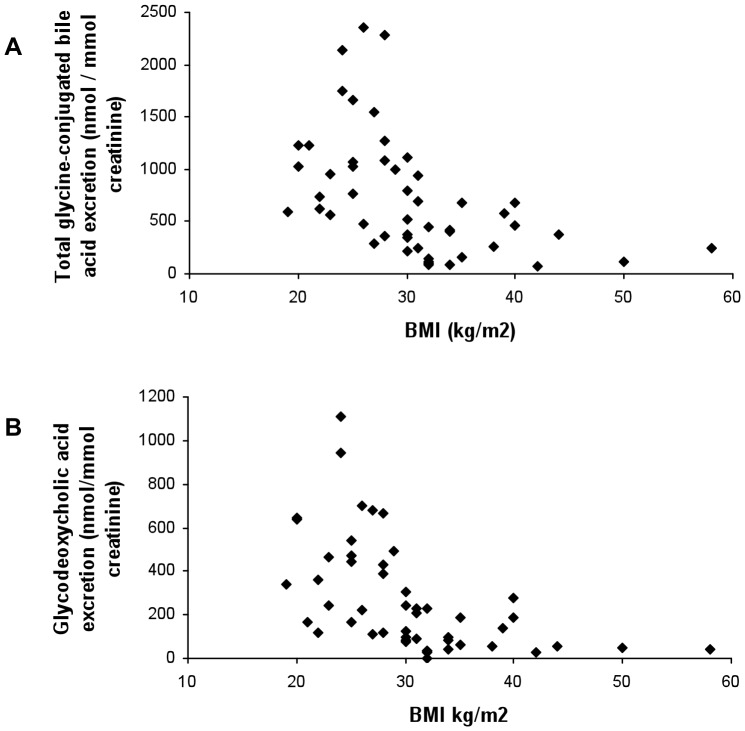
Strikingly, correlation of urinary bile acid excretion (both total and individual species) with glycaemic control was lost altogether in patients classified as obese (Table 4, Figures 1 and 2). As a demonstration of the differences in correlation of glycaemic control with urinary bile acid excretion between the different BMI subgroups, graphs for total glycine-conjugated bile acid (Figure 1) and glycodeoxycholic acid (Figure 2) excretion are shown. When BMI was plotted against urinary bile acid excretion, there was a marked negative correlation of urinary bile acid excretion with BMI≥30 kg/m2 (Figure 3). Indeed, urinary bile acid excretion was almost undetectable in morbidly obese individuals (Figure 3).
Figure 3. Graph plotting BMI of patient against total glycine-conjugated (A) and glycodeoxycholic acid (B) urinary bile acid excretion.
Discussion
In this study we demonstrate that urinary bile acid excretion is increased in type 2 diabetes mellitus compared to healthy controls, and that this increase is most evident in normal weight and overweight type 2 diabetic patients. Moreover, despite the study groups being relatively small, we clearly show that urinary bile acids are related to glycaemia, reflected by HbA1c, in normal weight and overweight, but not obese type 2 diabetic patients. Finally, we show that in type 2 diabetes, urinary bile acid excretion is suppressed at higher BMI.
Gross rearrangements of bile acid metabolism in type 2 diabetes are well established, with altered synthetic rate [10], [11], pool size [12], [13] and individual species composition [10], [14]. Given the emerging evidence that bile acids are important regulators of glucose homeostasis [2], such alterations may reflect altered bile acid signalling in type 2 diabetes mellitus pathogenesis in humans. In support, a recent study demonstrated insulin resistance in healthy subjects is associated with increased 12-hydroxylated bile acid species including cholic and deoxycholic acid [35], Nonetheless in type 2 diabetes the relationship between bile acids and prevailing glycaemic control remains poorly defined, as does its dependence of BMI. In the present study, urine samples were used to study whether bile acid turnover is related to HbA1c as a marker of glycaemic control. As urinary bile acid excretion expressed as a creatinine ratio correlates tightly with fasting plasma bile acid concentration [29], its measurement on early morning first pass urine samples represents an excellent non-invasive test for this purpose. Moreover, urinary bile acid excretion has been shown to increase in both human and animal studies of diabetes mellitus, providing support for the validity of the findings of glycaemia-associated changes in urinary bile acid excretion in type 2 diabetes in this study [14], [36]. Plasma bile acid measurement, on the other hand, was not performed owing to large intra-individual biological variation over a 24 hour period (23% to 91%) [37]. Such variation largely reflects increased post-prandial bile acid concentrations [5].
The increased bile acid excretion in people with type 2 diabetes mellitus is compatible either with an impact of diabetes on bile acid turnover, or with the increase in bile acid production being a compensatory response to the diabetic milieu to maintain glucose homeostasis. Post-prandial release of the incretin GLP-1 is impaired in type 2 diabetes mellitus [38], and HbA1c inversely correlates with maximal GLP-1 release [39]; suggesting that poorer glycaemic control is associated with a greater defect in incretin function. In normal physiology, bile acid activation of TGR5 stimulates GLP-1 release [3], [4], and plasma glycochenodeoxycholic acid and glycodeoxycholic acid concentrations correlate with GLP-1 after a mixed meal test [40]. Moreover, concomitant intra-jejunal infusion of both taurocholic acid and glucose was shown to increase both GLP-1 and C-peptide:glucose ratio relative to glucose infusion alone in healthy volunteers [41]. Therefore, the increased bile acid turnover in type 2 diabetes seen in this study may suggest the existence of a positive feedback mechanism to increase GLP-1 response. Glucose stimulates bile acid production by increasing CYP7A1 expression [8], [9] which may provide a mechanism for the increased bile acid excretion in poorly controlled type 2 diabetes mellitus, and the correlation we have found between bile acid excretion and HbA1c. Increasing GLP-1 release by bile acid -mediated mechanisms would be expected to be beneficial in type 2 diabetes mellitus. In support, bile acid sequestrants structurally mimic bile acids and improve glycaemic control by a TGR5-dependent mechanism [42], [43].
In our study, the relationship between bile acid excretion and glycaemia appears lost in obese type 2 diabetic patients, as urinary bile acid excretion is suppressed in this group. Obesity is a state of low grade chronic inflammation, inducing insulin resistance in target tissues [44], [45]. Cytokines are known to reduce bile acid synthesis by direct inhibition of CYP7A1 expression [46]. Thus, low urinary bile acid excretion in obese type 2 diabetic patients may reflect cytokine suppression, which in turn may have damaging effects on glucose homeostasis. In support of this, post-prandial plasma bile acid response is blunted in the obese [26], and several bile acid metabolites are associated with insulin sensitivity [47]. Chemically reducing bile acid pool size in animal models induces both diabetes mellitus and obesity [15], supporting the hypothesis that the suppressed urinary bile acid output seen in the obese in this study is of pathological significance.
One of the limitations of the study is the small cohort. The small numbers were the consequence of the strict selection criteria applied to try to avoid any influence of confounding factors on bile acid metabolism. Despite this, study numbers were sufficient to demonstrate the profound glycaemia-related changes in bile acid metabolism in normal weight and overweight type 2 diabetes.
The data in this study argue that at least for the obese type 2 diabetes patients, restoration of bile acid metabolism may be beneficial. Weight loss is associated with improvements in bile acid metabolism [25], [48]. Bariatric surgery provides the most significant and durable weight loss, but remission of type 2 diabetes mellitus precedes significant weight loss. This may be associated with enhanced β-cell function, hepatic insulin sensitivity, and nutrient rerouting, which many studies have causally related to the improved post-prandial GLP-1 responses [22]–[24]. Fasting bile acids are dramatically increased post-RYGB relative to obese controls [25], [48], and may thus contribute to type 2 diabetes remission perhaps via GLP-1. Weight loss by dietary means alone has also been shown to improve post-prandial GLP-1 response in the obese although bile acids were not measured [49].
In summary, the data in this study show that bile acids are increased in type 2 diabetes mellitus as a function of glycaemia in individuals with a BMI below 30 kg/m2. This is consistent with glucose stimulating bile acid production to maintain glucose homeostasis, possibly by increased GLP-1 response and altering FXR mediated signalling. Understanding how these compensatory mechanisms are lost in obese individuals with type 2 diabetes may provide an avenue for the development of new therapeutic strategies.
Funding Statement
The authors have no support or funding to report.
References
- 1. Prawitt J, Caron S, Staels B (2011) Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diab Rep 11: 160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lefebvre P, Cariou B, Lien F, Kuipers F, Staels B (2009) Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev 89: 147–191. [DOI] [PubMed] [Google Scholar]
- 3. Katsuma S, Hirasawa A, Tsujimoto G (2005) Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun 329: 386–390. [DOI] [PubMed] [Google Scholar]
- 4. Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, et al. (2009) TGR5-Mediated Bile Acid Sensing Controls Glucose Homeostasis. Cell Metabolism 10: 167–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhao X, Peter A, Fritsche J, Elcnerova M, Fritsche A, et al. (2009) Changes of the plasma metabolome during an oral glucose tolerance test: is there more than glucose to look at? Am J Physiol Endocrinol Metab 296: E384–E393. [DOI] [PubMed] [Google Scholar]
- 6. Kumar DP, Rajagopal S, Mahavadi S, Mirshahi F, Grider JR, et al. (2012) Activation of transmembrane bile acid receptor TGR5 stimulates insulin secretion in pancreatic β cells. Biochem Biophys Res Commun 427: 600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Popescu IR, Helleboid-Chapman A, Lucas A, Vandewalle B, Dumont J, et al. (2010) The nuclear receptor FXR is expressed in pancreatic beta-cells and protects human islets from lipotoxicity. FEBS Lett 584: 2845–2851. [DOI] [PubMed] [Google Scholar]
- 8. Li T, Chanda D, Zhang Y, Choi HS, Chiang JY (2010) Glucose stimulates cholesterol 7alpha-hydroxylase gene transcription in human hepatocytes. J Lipid Res 51: 832–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li T, Francl JM, Boehme S, Ochoa A, Zhang Y, et al. (2012) Glucose and insulin induction of bile acid synthesis: mechanisms and implication in diabetes and obesity. J Biol Chem 287: 1861–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brufau G, Stellaard F, Prado K, Bloks VW, Jonkers E, et al. (2010) Improved glycemic control with colesevelam treatment in patients with type 2 diabetes is not directly associated with changes in bile acid metabolism. Hepatology 52: 1455–1464. [DOI] [PubMed] [Google Scholar]
- 11. Suhre K, Meisinger C, Döring A, Altmaier E, Belcredi P, et al. (2010) Metabolic footprint of diabetes: a multiplatform metabolomics study in an epidemiological setting. PLoS One 5: e13953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bennion LJ, Grundy SM (1977) Effects of diabetes mellitus on cholesterol metabolism in man. N Engl J Med 296: 1365–1371. [DOI] [PubMed] [Google Scholar]
- 13. Li LO, Hu YF, Wang L, Mitchell M, Berger A, et al. (2010) Early hepatic insulin resistance in mice: a metabolomics analysis. Mol Endocrinol 24: 657–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Andersen E, Karlaganis G, Sjovall J (1988) Altered bile acid profiles in duodenal bile and urine in diabetic subjects. Eur J Clin Invest 18: 166–172. [DOI] [PubMed] [Google Scholar]
- 15. Watanabe M, Horai Y, Houten SM, Morimoto K, Sugizaki T, et al. (2011) Lowering bile acid pool size with a synthetic farnesoid X receptor (FXR) agonist induces obesity and diabetes through reduced energy expenditure. J Biol Chem 286: 26913–26920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Staels B, Fonseca VA (2009) Bile acids and metabolic regulation: mechanisms and clinical responses to bile acid sequestration. Diabetes Care 32: S237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Handelsman Y (2011) Role of bile acid sequestrants in the treatment of type 2 diabetes. Diabetes Care 34: S244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Leibson CL, Williamson DF, Melton LJ 3rd, Palumbo PJ, Smith SA, et al. (2001) Temporal trends in BMI among adults with diabetes. Diabetes Care 24: 1584–1589. [DOI] [PubMed] [Google Scholar]
- 19. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, et al. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 20. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, et al. (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, et al. (2009) Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 122: 248–256.e5. [DOI] [PubMed] [Google Scholar]
- 22. Polyzogopoulou EV, Kalfarentzos F, Vagenakis AG, Alexandrides TK (2003) Restoration of euglycemia and normal acute insulin response to glucose in obese subjects with type 2 diabetes following bariatric surgery. Diabetes 52: 1098–1103. [DOI] [PubMed] [Google Scholar]
- 23. Guidone C, Manco M, Valera-Mora E, Iaconelli A, Gniuli D, et al. (2006) Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric surgery. Diabetes 55: 2025–2031. [DOI] [PubMed] [Google Scholar]
- 24. Laferrère B (2011) Diabetes remission after bariatric surgery: is it just the incretins? Int J Obes (Lond) 35: S22–S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Patti ME, Houten SM, Bianco AC, Bernier R, Larsen PR, et al. (2009) Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring) 17: 1671–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Glicksman C, Pournaras DJ, Wright M, Roberts R, Mahon D, et al. (2010) Postprandial plasma bile acid responses in normal weight and obese subjects. Ann Clin Biochem 47: 482–484. [DOI] [PubMed] [Google Scholar]
- 27. Vincent RP, Omar S, Ghozlan S, Taylor DR, Cross G, et al. (2013) Higher circulating bile acid concentrations in obese type 2 diabetics. Ann Clin Biochem 50: 360–364. [DOI] [PubMed] [Google Scholar]
- 28. Dawson PA, Lan T, Rao A (2009) Bile acid transporters. J Lipid Res 50: 2340–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Simko V, Michael S, Kelley RE (1987) Predictive value of random sample urine bile acids corrected by creatinine in liver disease. Hepatology 7: 115–121. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization (2000) Obesity: preventing and managing the global epidemic. Geneva, Switzerland: World Health Organization. [PubMed]
- 31. Takikawa H, Beppu T, Seyama Y (1984) Urinary concentrations of bile acid glucuronides and sulfates in hepatobiliary diseases. Gastroenterol Jpn 19: 104–109. [DOI] [PubMed] [Google Scholar]
- 32. Ikegawa S, Murao N, Motoyama T, Yanagihara T, Niwa T, et al. (1996) Separation and detection of bile acid 3-glucuronides in human urine by liquid chromatography/electrospray ionization-mass spectrometry. Biomed Chromatogr 10: 313–317. [DOI] [PubMed] [Google Scholar]
- 33.Taylor NF (2006) Urinary steroid profiling. In: Wheeler MJ, Hutchinson JSM, editors. Hormone assays in biological fluids. pp. 159–175.
- 34. Tagliacozzi D, Mozzi AF, Casetta B, Bertucci P, Bernardini S, et al. (2003) Quantitative analysis of bile acids in human plasma by liquid chromatography-electrospray tandem mass spectrometry: a simple and rapid one-step method. Clin Chem Lab Med 41: 1633–1641. [DOI] [PubMed] [Google Scholar]
- 35. Haeusler RA, Astiarraga B, Camastra S, Accili D, Ferrannini E (2013) Human Insulin Resistance is Associated with Increased Plasma Levels of 12α-hydroxylated Bile Acids. Diabetes 62: 4184–4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cai S, Huo T, Xu J, Lu X, Zheng S, et al. (2009) Effect of mitiglinide on Streptozotocin-induced experimental type 2 diabetic rats: a urinary metabonomics study based on ultra-performance liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 877: 3619–3624. [DOI] [PubMed] [Google Scholar]
- 37. Steiner C, Othman A, Saely CH, Rein P, Drexel H, et al. (2011) Bile acid metabolites in serum: intraindividual variation and associations with coronary heart disease, metabolic syndrome and diabetes mellitus. PLoS One 6: e25006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nauck M, Stöckmann F, Ebert R, Creutzfeldt W (1986) Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29: 46–52. [DOI] [PubMed] [Google Scholar]
- 39. Mannucci E, Pala L, Monami M, Da Vico L, Bardini G, et al. (2010) Glucagon-like peptide-1 response to meals and post-prandial hyperglycemia in Type 2 diabetic patients. J Endocrinol Invest 33: 147–150. [DOI] [PubMed] [Google Scholar]
- 40. Roberts RE, Glicksman C, Alaghband-Zadeh J, Sherwood RA, Akuji N, et al. (2011) The relationship between postprandial bile acid concentration, GLP-1, PYY and ghrelin. Clin Endocrinol (Oxf) 74: 67–72. [DOI] [PubMed] [Google Scholar]
- 41. Wu T, Bound MJ, Standfield SD, Jones KL, Horowitz M, et al. (2013) Effects of Taurocholic Acid on Glycemic, Glucagon-like Peptide-1, and Insulin Responses to Small Intestinal Glucose Infusion in Healthy Humans. J Clin Endocrinol Metab 98: E718–722. [DOI] [PubMed] [Google Scholar]
- 42. Shang Q, Saumoy M, Holst JJ, Salen G, Xu G (2010) Colesevelam improves insulin resistance in a diet-induced obesity (F-DIO) rat model by increasing the release of GLP-1. Am J Physiol Gastrointest Liver Physiol 298: G419–424. [DOI] [PubMed] [Google Scholar]
- 43. Chen L, McNulty J, Anderson D, Liu Y, Nystrom C, et al. (2010) Cholestyramine reverses hyperglycemia and enhances glucose-stimulated glucagon-like peptide 1 release in zucker diabetic Fatty rats. J Pharmacol Exp Ther 334: 164–170. [DOI] [PubMed] [Google Scholar]
- 44. Arkan MC, Hevener AL, Greten FR, Maeda S, Li ZW, et al. (2005) IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med 11: 191–198. [DOI] [PubMed] [Google Scholar]
- 45. Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, et al. (2005) Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med 11: 183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Li T, Jahan A, Chiang JY (2006) Bile acids and cytokines inhibit the human cholesterol 7 alpha-hydroxylase gene via the JNK/c-jun pathway in human liver cells. Hepatology 43: 1202–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shaham O, Wei R, Wang TJ, Ricciardi C, Lewis GD, et al. (2008) Metabolic profiling of the human response to a glucose challenge reveals distinct axes of insulin sensitivity. Mol Syst Biol 4: 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Simonen M, Dali-Youcef N, Kaminska D, Venesmaa S, Käkelä P, et al. (2012) Conjugated bile acids associate with altered rates of glucose and lipid oxidation after Roux-en-Y gastric bypass. Obes Surg 22: 1473–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Verdich C, Toubro S, Buemann B, Madsen Lysgård J, Holst Juul J, et al. (2001) The role of postprandial releases of insulin and incretin hormones in meal-induced satiety - effect of obesity and weight reduction. Int J Obes Relat Metab Disord 25: 1206–1214. [DOI] [PubMed] [Google Scholar]