Abstract
Objectives
The incidence and survival rate of colorectal cancer in Korea are increasing because of improved screening, treatment technologies, and lifestyle changes. In this aging population, increases in economic cost result. This study was conducted to estimate the economic burden of colorectal cancer utilizing claims data from the Health Insurance Review and Assessment Service.
Methods
Economic burdens of colorectal cancer were estimated using prevalence data and patients were defined as those who received ambulatory treatment from medical institutions or who had been hospitalized due to colorectal cancer under the International Classification of Disease 10th revision codes from C18-C21. The economic burdens of colorectal cancer were calculated as direct costs and indirect costs.
Results
The prevalence rate (per 100 000 people) of those who were treated for colorectal cancer during 2010 was 165.48. The economic burdens of colorectal cancer in 2010 were 3 trillion and 100 billion Korean won (KRW), respectively. Direct costs included 1 trillion and 960 billion KRW (62.85%), respectively and indirect costs were 1 trillion and 160 billion (37.15%), respectively.
Conclusions
Colorectal cancer has a large economic burden. Efforts should be made to reduce the economic burden of the disease through primary and secondary prevention.
Keywords: Cost of illness, Economic burden, Colorectal neoplasms, Prevalence
INTRODUCTION
Based on data from 2010, cancer ranks number one as the most fatal disease in Korea [1]; thus, it poses a significant threat to the lives of Koreans. According to the Journal of the Korean Cancer Association, the incidence rate of cancer increased 4.0% in 2010 with 202 053 new cancer diagnoses compared to 194 359 new cancer diagnoses in 2009 [1]. Moreover, the incidence rate among males was 1.04 times higher than that of females [1]. In 2009, 190 000 people were diagnosed with cancer (99 224 males and 93 337 females), and this constituted a 6.7% increase compared to the 180 465 new diagnoses in 2008 [1]. Since 2002, there has been a 98.5% increase in cancer diagnoses in the Korea [1].
Cancer mortality has increased steadily over the last 10 years. The total number of Korean cancer-related deaths has increased 1.3 times from 53 845 people in 1999 to 72 046 people in 2010 [2]. The increase in both the incidence and mortality rate is a global phenomenon. For example, the incidence of cancer in the USA has steadily increased between 1999 and 2008 [3].
Colorectal cancer involves a malignant tumor in the colon (colon cancer) or rectum (rectum cancer). These cancers are designated as colorectal cancer and/or colorectal carcinoma [4]. In the 2012 cancer incidence report by the Korea Ministry of Health and Welfare, the crude incidence rate of colorectal cancer in 2010 was 62.5 in males (per 100 000 people) and 20.8 in females (per 100 000 people). Among all people diagnosed with cancer, 15.2% of males and 10.3% of females had colorectal cancer [1]. In data from 2010, colorectal cancer ranked third among all incident types of cancer. Among men, colorectal cancer ranked second behind stomach cancer, whereas in women, it ranked third following thyroid cancer and breast cancer [5,6]. These values are high relative to other countries. In September 2011, the International Agency for Research on Cancer, an affiliate of the World Health Organization, announced 184 countries as targets to reduce the world's incidence of colorectal cancer in 2008. The incidence of colorectal cancer among Korean men in 2008 was 46.9 per 100 000 people and ranked first among all Asian countries and fourth worldwide. The incidence of colorectal cancer in the Korea followed the incidence rates of Slovakia, Hungary, and the Czech Republic, which were 60.6, 56.4, and 54.4 per 100 000 people, respectively. The incidence among Korean females per 100 000 people was ranked 19th out of the 184 countries and was higher than that of England (25.3), America (25.0), and Japan (22.8) [7].
Patients with cancer require high-level treatment and care. Patients and their families carry the burden of treatment expenses due to the long fight against the disease. Thus, financial loss may prevent ultimate recovery. Cancer incidence and survival rates are both increasing and cancer-related costs for families worldwide are predicted to continue to increase.
For example, it was reported in 2002 that the economic burdens of stomach cancer and liver cancer in the Korea were 2.2 trillion won each Korean won (KRW) each, the highest among all cancers. Lung cancer and colorectal cancer had an economic burden of 1.5 trillion KRW and 1 trillion KRW, respectively. In 2005, the economic burden of liver cancer, stomach cancer, and colorectal cancer was estimated at 2.46 trillion KRW, 2.4 trillion KRW, and 1.38 trillion KRW, respectively. Although the burden of cancer was similar to that of 2002, the expenses substantially increased. Thus, the economic burden of cancer in the Korea is increasing substantially every year [8,9,10].
Many studies have investigated the economic burden of cancers in the Korea. However, rapid increases in the incidence of disease and relative survival rates have caused changes in the burden of disease. This is particularly apparent in cancers such as colorectal cancer that have demonstrated rapidly increasing incidence rates. Thus, this study used nationally representative data to investigate the increasing economic burden of colorectal cancer.
METHODS
To estimate the economic burden of colorectal cancer, a prevalence-based approach was employed that targeted existing and newly diagnosed patients [11]. Data from the 2010 cross-sectional study was used to include existing and newly diagnosed colorectal cancer patients to measure the expenses related to colorectal cancer medical treatment in the Korea.
Colorectal cancer was defined according to the International Classification of Disease 10th revision (ICD-10) codes from C18-C21 [12]. Data on salary demands, health insurance reviews, and assessment services were used to calculate the economic expenses for complete medical treatment of both inpatients and outpatients based on reported medical treatments and the prevalence of colorectal cancer patients.
The target participants of this study were patients who had visited clinics primarily for the treatment of colorectal cancer and who had been hospitalized or had claimed health insurance benefits. To improve the accuracy of the selection process, patients with more than three hospital visits were considered prevalent cases [13,14].
To estimate economic burden, expenses were broadly classified as direct expenses or indirect expenses. Direct expenses were considered costs that were incurred during treatment and included direct medical and non-medical care costs. Direct medical care costs were paid by the insurer of inpatients and outpatients. Moreover, the medical expenses incurred during medical treatment were classified as paid by patients (out of pocket), meal costs, upper ward differences, specialized treatments, non-covered care costs, and prescribed pharmaceutical costs (Supplemental Table 1).
For direct non-medical care costs, the cost of transportation for the patient and guardian were included, such as costs incurred when visiting care facilities or during hospitalization.
To estimate loss of productivity, indirect costs were classified as the cost of premature death and loss of productivity as time consumed during outpatient visits to hospital or total time hospitalized.
To measure the direct care costs, we requested the 2010 data from the Health Insurance Review and Assessment Service (HIRA). Colorectal cancer disease codes were used to search for outpatients or inpatients who received colorectal cancer treatments. Moreover, data on non-insured costs compiled by the HIRA were also used [15]. The non-insured costs paid by colorectal patients were identified to be 25% for hospitalized patients and 14.2% for outpatients. All the direct care costs in this study were calculated using this information [15].
Pharmaceutical costs were calculated for patients who had claimed benefits for treatment of colorectal cancer which is main diagnoses, using the 2010 HIRA data. Medications for unrelated diseases such as hypertension were excluded using the ICD-10 codes and drug classification numbers to isolate medications related to colorectal cancer only (Supplemental Table 2).
Direct non-medical care costs were calculated as the sum of transportation expenses incurred when the patient and guardian visited the clinic. Based on 2008 Korea Health Panel, the average one-way cost of transportation among cancer inpatients and their guardians was 12 719.9 KRW. For outpatients and their guardians, the average one-way cost of transportation cost was 4687.3 KRW in 2008 [16]. The 2008 price was converted to the 2010 price index by multiplying by the inflation rate of 113.4.
No determined fixed costs were calculated for the guardians. Costs were applied differently across institutions. According to the Guardian Association, the average cost incurred by guardians was 56 809 KRW (average cost of one day) in 2005, and this cost was multiplied by the number of days guardians cared for their patients in the final calculation [17].
Among outpatients in our study population, those aged 0 to 9 and over 60 years were assumed to be accompanied by a guardian. Therefore, the daily average cost of guardian care in 2005 was applied (56 809 KRW [average cost of one day]), and this number was multiplied by the total number of days at outpatient visits to calculate the total cost. Then, the 2010 inflation rate of 117.1 (price index) was applied for the final calculation. In addition, the estimated time spent visiting the outpatient clinic was calculated by multiplying the number of working hours in the day by one third for the total number of days the patient visited the outpatient clinic.
The 2010 price index was used as the reference year for comparison with that of 2005, and a 115 (price index) adjustment was multiplied by transportation and guardian cost calculations [18].
Indirect cost was defined as medical care costs or the cost of premature death. Thus, indirect cost was estimated according to the loss of productivity calculation based on the human-capital approach [19].
To measure productivity loss for hospitalized patients, the monthly average labor hours, according to the 2007 investigation of labor according to the type of employment, and the monthly average wage by age were applied. Further, 2007 labor statistics data were used to divide the total average monthly wage of laborers by the total labor hours to calculate the average wage per hour [20].
The price index of 117.1 was multiplied to costs calculated for 2010 (reference year). Participants aged 0 to 19 and over 60 were assumed to not participate in actual economic activities; thus, productivity loss was calculated for patients aged 20 to 65. Further, to measure the monthly average cost of productivity loss due to outpatient visits, the total number of days the patient visited the outpatient clinic was multiplied by one-third for the final calculation.
In the case of premature death, cause-of-death statistics from the National Statistical Office were used to calculate the colorectal cancer mortality. Moreover, the premature cost of death was measured for those who worked until the age of 65, and a 5% rate was used to calculate productivity loss due to premature death.
SAS version 9.1 (SAS Inc., Cary, NC, USA) was used for statistical analyses.
RESULTS
Prevalence of Treatment for Colorectal Cancer
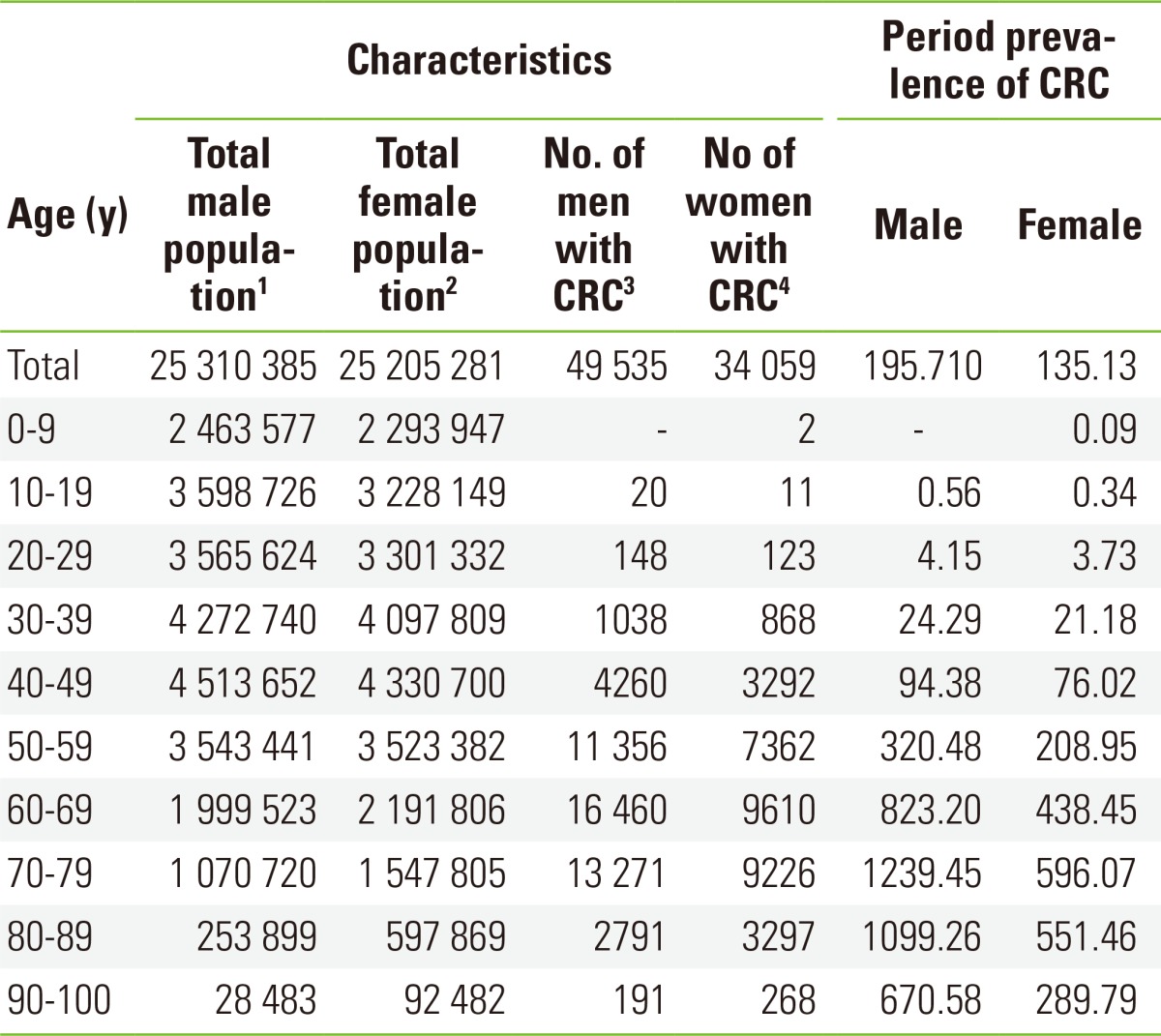
The prevalence of treatment (per 100 000 people) among males and females diagnosed with cancer in 2010 were 195.71 and 135.1, respectively. Treatment was more likely in adults than that in children and increased with adult age. Men and women between 70 to 79 years old had the highest prevalence of treatment (Table 1).
Table 1.
Treated prevalence of CRC in 2010
Economic Burden
The total economic burden of colorectal cancer in 2010 was 3.1 trillion KRW. The direct cost was 1.97 trillion KRW (62.85%), and the indirect cost was 1.16 trillion KRW (37.15%). The ratio of direct-to-indirect cost was 1.69:1, indicating that the direct cost was about 1.7 times higher than the indirect cost. The direct medical care cost was 774.6 million KRW, and the direct non-medical care cost was 1.19 trillion KRW. For indirect costs, productivity loss was 132.3 million KRW and the cost of premature death was 1.27 trillion KRW (Table 2).
Table 2.
Economic burden of colorectal cancer in Korea, 2010
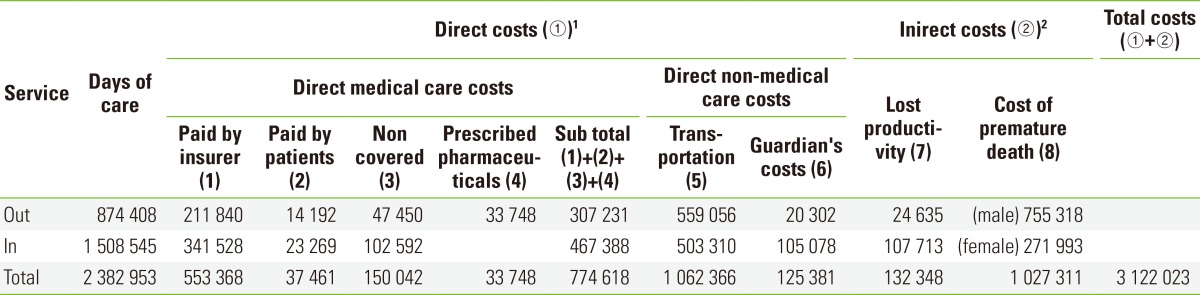
Unit: 1 000 000 Korean won.
1Direct costs=(1)+(2)+(3)+(4)+(5)+(6).
2Indirect costs=(7)+(8).
For outpatients who visited clinics in 2010, the direct medical care cost for colorectal cancer was 307.2 million KRW. This cost was further divided as 211.8 million KRW (69.0%), 47.5 million KRW (15.4%), 33.7 million KRW (11.0%), and 14.2 million KRW (5.0%) for the cost of health insurance, non-insured fees, pharmaceutical cost, and out-of-pocket fees, respectively.
In addition, the direct medical care cost for inpatients in 2010 was 467.4 million KRW. Of this total cost, 341.5 million KRW (73.1%), 102.6 million KRW (21.9%), and 23.3 million KRW (5.0%) was estimated as the cost of insurance, non-insured fees, and out-of-pocket fees, respectively.
A total of 1.183 trillion KRW in economic expenses was spent by women compared to 1.94 trillion KRW by men. The direct medical care costs for men and women were 394.4 and 380.2 billion KRW, respectively; thus, the cost for men was 1.04 times higher than that of women. Moreover, among those aged 20 to 69, women and men spent 238.9 and 281.5 billion KRW, respectively, indicating that men spent 1.18 times more than did women. According to the gender-specific results, the direct medical care cost (women, 99.8 billion KRW vs. men, 129.9 billion KRW) and the average cost per person (women, 35 million KRW vs. men, 39 million) were highest in men (Table 3). The direct medical care cost of outpatients was around 300 billion KRW, whereas the direct medical care cost for hospitalized patients was approximately 470 billion KRW.
Table 3.
Medical/non-medical care expenses by gender
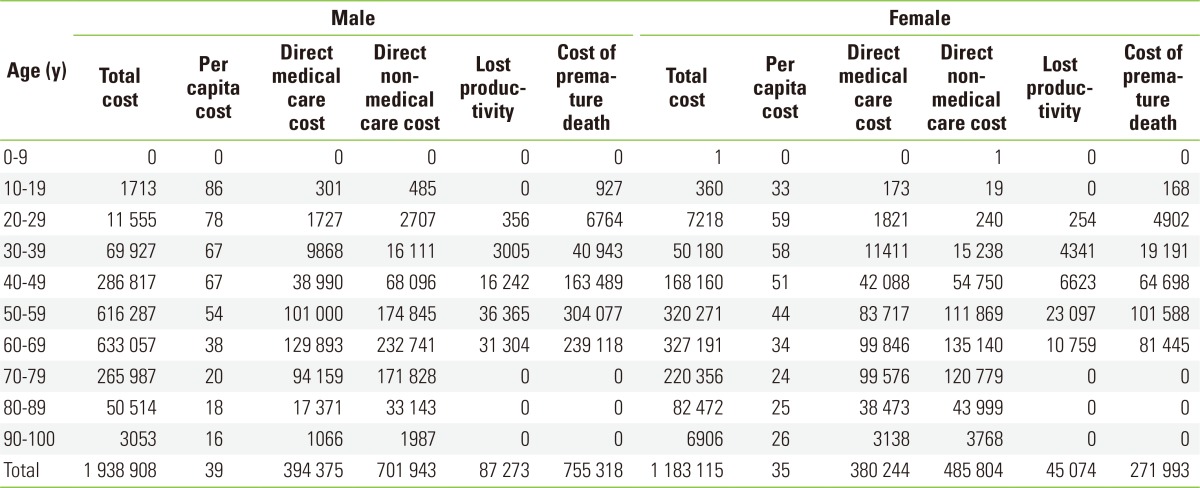
Unit: 1 000 000 Korean won.
For pharmaceutical costs, the total treatment cost for medical prescriptions was 33.7 billion KRW (excluding the cost of treatment from the direct medical treatment cost data). Per day, an average of 3859.7 KRW was spent on pharmaceuticals at the clinic.
Transportation fees for outpatients, a direct non-medical care cost for outpatients, were estimated to be 559.1 billion KRW. Furthermore, the direct non-medical care cost of hospitalization was 500.3 billion KRW for transportation fees. The guardian cost for both outpatients and inpatients was 125.4 billion KRW.
The indirect cost was calculated as the loss of income due to either premature death or loss of productivity from outpatient visits or hospitalization. The total costs of productivity loss and premature death were 132.3 billion KRW and 1.23 trillion KRW, respectively.
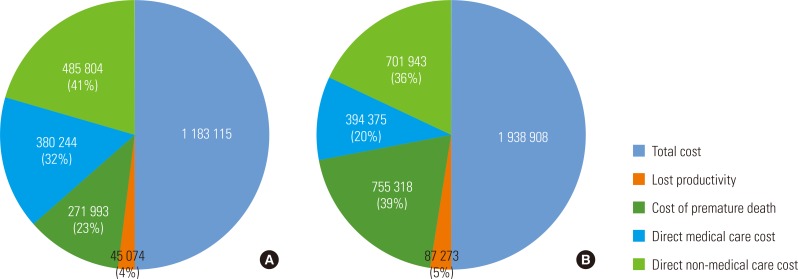
For indirect costs, the loss to labor among outpatients was 24.6 billion KRW, and men incurred 2.05 times more of a loss than women did (men, 16.6 billion KRW vs. women, 8.1 billion KRW). The loss to labor among inpatients was 107.7 billion KRW, and men incurred 1.91 times more of a loss than women did (men, 70.7 billion KRW vs. women, 37.0 billion KRW). The loss of opportunity due to premature death was 755.3 billion KRW for men and 272.0 billion KRW for women; men incurred 2.78 times more of a loss than women did (Figure 1).
Figure 1.
The proportion of medical/non-medical expenses by gender (unit: 1 000 000 Korean won). (A) Female and (B) male.
The total direct and indirect economic burden of colorectal cancer was calculated to be 3.1 trillion KRW.
DISCUSSION
In this study, the HIRA health insurance claims data were used to estimate the economic burden and prevalence of treatment in the Korea. According to the National Statistical Office, approximately 83 594 patients of the total Korean population (n=50 515 666) were treated for colorectal cancer in 2010; thus, the treatment prevalence for colorectal cancer was 165.48 (per 100 000 people). Among the total female population in the Korea (n=25 205 281), approximately 34 059 females were diagnosed with colorectal cancer at a prevalence of 135.13 (per 100 000 people). Among the total Korean male population (n=25 310 385), 49 535 were diagnosed with colorectal cancer with a prevalence rate of 195.71 (per 100 000 people). Therefore, a 1.45 times higher prevalence rate was found in men than that of women.
In a study from 2009, the total number of patients with colorectal cancer was 81 769 with a 164.7 prevalence per 100 000 people, and the age-standardized prevalence rate was 122.0 per 100 000 people. The prevalence of treatment in this study was 165.48, which is similar to the prevalence in 2009, which were based on the National Cancer Registration data [21]. Our study used data from insurance claims reported by the HIRA for inpatients and outpatients treated for colorectal cancer in 2010. As a result, the calculated prevalence rates were similar for the two datasets.
The economic burden of colorectal cancer was 3.1 trillion KRW. The direct cost was 1.97 trillion KRW (62.85%), and the indirect cost was 1.16 trillion KRW. The direct-to-indirect cost ratio was approximately 1.7. Furthermore, when looking at age- and gender-specific distributions, the total cost increased with age. The economic burden of colorectal cancer was 1.94 and 1.12 trillion KRW for men and women, respectively. The direct medical care cost of men and women were 394.4 billion KRW and 380.2 billion KRW, respectively, which are approximately equal. However, loss to labor was 842.6 billion KRW for men and 317.1 billion KRW for women, indicating that men experienced a 2.7 times greater loss than did women. Men and women aged 60 to 69 years incurred the most costs for direct medical care (women, 99.8 billion KRW; men, 129.9 billion KRW).
In 2002 the estimated socioeconomic burden due to cancer in the Korea was 11.3 trillion KRW. In 2005, the cost increased by 1.25 times to 14.1 trillion KRW [10,21]. In 2002 and 2005, colorectal cancer's economic burden was 1 trillion KRW and 1.4 trillion KRW, respectively. The economic burden of colorectal cancer in this study was estimated at 3.1 trillion KRW. Thus, a 2.23-fold increase in socioeconomic burden due to colorectal cancer was noted in 2005 [10]. In this study, the direct medical care cost was 774.6 billion KRW (24.81% of the total cost), the direct non-medical care cost was 1.10 trillion KRW (38.04% of the total cost), and the indirect cost was 1.16 trillion KRW (37.14% of the total cost). In the previous study from 2005, the direct and indirect costs were 79.6% and 20.4%, respectively. Thus, in 2005, the direct cost was 3.9 times more than indirect cost. However, in the present study, the direct cost (1.97 trillion KRW) was 1.7 times greater than the indirect cost (1.16 trillion KRW). The different methods used in this study, including the transportation fees, costs related to guardian care, and the increased price index, likely contributed to this difference. For example, data on the use of complementary and alternative medicine for were included in the 2005 study on direct medical care costs. However, when calculating indirect cost, the loss of productivity among cancer patients was calculated according to the rate of economic activity. Thus, the rate of indirect cost was compared to direct cost.
To investigate the socioeconomic burden of colorectal patients, this study utilized the 2010 data from HIRA to calculate the prevalence of cancer. Moreover, health insurance claims data were used to estimate costs. The Korea has a single, national insurance system; therefore, the national prevalence of colorectal could be estimated [22]. This method has the added advantage of maintaining internal consistency. Although we used health insurance claims data, the prevalence rates reported here were similar to data from cancer registries. The direct cost of 1.9624 trillion KRW reported here corresponded to approximately 4.09% of the 2010 medical care costs in the Korea (total medical costs in the public sector in 2010=48.293577 trillion KRW) [23]. In addition, the health insurance guarantee rate for colorectal cancer was 68.9%, which was lower than lung cancer at 74.6% and lower than liver cancer at 70.9%. However, in the non-insured cost per patient for colorectal cancer ranked first among all main cancers at 25.0% [15]. According to data from the National Health Insurance Corporation in 2010, deductibles for the treatment of target diseases decreased from 10% to 5%, and the health insurance guarantee rate for these diseases improved from 71.4% compared to the rate of the previous year 67.8%. The guarantee rate does not include non-covered costs, thus is insufficient at estimating total costs.
Colorectal cancer was one of the cancers that demonstrated an increase in socioeconomic cost. When examining the changes to medical care costs from 2001 to 2009 for the main types cancers, prostate cancer increased 9.9-fold (9.4 to 93.2 billion KRW), breast cancer increased 5.0-fold (63.6 to 316.2 billion KRW), and colorectal cancer increased 4.5-fold (101 to 453 billion KRW). Thus, colorectal cancer showed the most drastic increase with a difference of 357.1 billion KRW, with stomach cancer ranking second. Therefore, colorectal cancer consumes a substantial amount of economic burden and available finances [15]. To lessen the socioeconomic burden of colorectal cancer, early treatment and early examinations along with altering lifestyle behaviors should be emphasized [8,24]. Moreover, the national estimated rate of cancer examinations was 36.0% in 2008, 22.9% among medical payment recipients, and 8.8% among patients with registered health insurance, which indicates a tendency to increase each year. However, for each type of cancer, breast cancer had the highest participation rate in 2008 at 43.5% followed by liver cancer (42.5%), stomach cancer (37.3%), and colorectal cancer (30.7%). When considering the socioeconomic burden of colorectal cancer, increasing the examination rate of colorectal cancer may decrease the economic burden of colorectal cancer [25]. Moreover, the rapidly aging population, with increased life expectancy, increases the relative survival rate of cancer. Thus, increased prevention and training about the risk factors for colorectal cancer as well as changes to health care policy are needed [26].
This study has important limitations. First, the human-capital method was used to estimate productivity loss, which uses the differences in wages according to the financial market [27]. The friction-cost method estimates the employer's expenses rather than the patient's expenses. Therefore, the human-capital method can identify a greater difference in cost than the friction-cost method can, and this can lead to an overestimation of productivity loss. Second, costs related to medical care for specific diseases and the exact classification of colorectal cancer patients is needed. In this study, patients were classified as having colorectal cancer if they were hospitalized or visited the outpatient clinic three times for colorectal cancer treatment. Thus, we may not have included all patients with colorectal cancer because not all patients visit the outpatient clinic or become hospitalized. This may have led to an underestimation of economic burden. Nonetheless, we estimated transportation fees, guardian costs, and time lost for guardians and patients, which may have led to an overestimation. Third, costs related to cancer treatment and comorbidities were not included, and medications not related to colorectal cancer were excluded. These exclusion criteria improved the accuracy of our measures; however, treatment costs from accompanying diseases may have also been included. Fourth, the cost of complementary and alternative medicine must be considered in future studies. Last, loss related to psychological pain endured by patients and family members and other self-sterilization tools and medicine required after colorectal cancer treatment/surgery could not be estimated.
This study utilized insurance claims data for colorectal cancer according to the 2010 data by the HIRA to estimate the economic burden of the disease. The prevalence of treatment among patients diagnosed with colorectal cancer (per 100 000 people) was 195.71 for men and 135.1 for women; men had an approximately 1.45 times higher prevalence than that of women. The economic burden of colorectal cancer was 3.122 trillion KRW, representing a 2.23-fold increase compared to the 2005 socioeconomic burden of 1.4 trillion KRW. In a review of the 2005 economic cost of cancer from previous research (Table 2), the number of colorectal cancer patients increased nearly 2-fold from 2010 to 2005 (97.3%), which may be due to an increase in the economic burden of the disease. Furthermore, the prevalence with patient age, with men and women age 60 to 69 consuming most of the direct medical care costs (females, 99.8 billion KRW; males, 129.9 billion KRW).
To reduce the economic burden of colorectal cancer, primary and secondary prevention must be promoted [28,29]. Participation rates in colorectal cancer examinations must be increased along with the development of healthy behaviors [30] to lessen the economic burden of colorectal cancer. Future studies should address these areas.
ACKNOWLEDGMENTS
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Korea (grant no. 1020310).
Footnotes
The authors have no conflicts of interest with the material presented in this paper.
Supplementary Material
Description of the sources of data used in this study
Colorectal cancer is considered to have few comorbidities in patients who are taking certain pharmaceuticals for diabetes, hypertension, hyperlipidemia, and depression
References
- 1.Ministry of Health and Welfare. Annual report of cancer statistics in Korea in 2010. Seoul: Ministry of Health and Welfare; 2012. pp. 10–21. (Korean) [Google Scholar]
- 2.Statistics Korea. Causes of death statistics in 2012: incidence and mortality of cancer. [cited 2014 Mar 7]. Available from: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=2770(Korean)
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 4.Azrak MF, Yang VW. Colorectal neoplasms. In: Sitaraman SV, Friedman LS, editors. Essentials of gastroenterology. Oxford: Wiley-Blackwell; 2012. pp. 132–146. [Google Scholar]
- 5.Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012;44(1):11–24. doi: 10.4143/crt.2012.44.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health and Welfare. Cancer facts and figures. Seoul: Ministry of Health and Welfare; 2010. pp. 13–16. (Korean) [Google Scholar]
- 7.International Agency for Research on Cancer. Colorectal cancer incidence: mortality and prevalence worldwide in 2008 summary. [cited 2014 Mar 7]. Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
- 8.Lee BI, Hong SP, Kim SE, Kim SH, Kim HS, Hong SN, et al. Korean guidelines for colorectal cancer screening and polyp detection. Clin Endosc. 2012;45(1):25–43. doi: 10.5946/ce.2012.45.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SG, Hahm MI, Choi KS, Seung NY, Shin HR, Park EC. The economic burden of cancer in Korea in 2002. Eur J Cancer Care (Engl) 2008;17(2):136–144. doi: 10.1111/j.1365-2354.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim J, Hahm MI, Park EC, Park JH, Park JH, Kim SE, et al. Economic burden of cancer in South Korea for the year 2005. J Prev Med Public Health. 2009;42(3):190–198. doi: 10.3961/jpmph.2009.42.3.190. (Korean) [DOI] [PubMed] [Google Scholar]
- 11.Segel JE. Cost-of-illness studies: a primer. 2006. [cited 2014 Mar 7]. Available from: http://www.rti.org/pubs/coi_primer.pdf.
- 12.World Health Organization. ICD-10 International Statistical Classification of Diseases and related health problems: 10th revision. 2010. [cited 2014 Mar 7]. Available from: http://apps.who.int/classifications/icd10/browse/2010/en.
- 13.Benson AB., 3rd Epidemiology, disease progression, and economic burden of colorectal cancer. J Manag Care Pharm. 2007;13(6 Suppl C):S5–S18. doi: 10.18553/jmcp.2007.13.s6-c.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hornbrook MC. On the definition and measurement of the economic burden of cancer. In: Lipscomb J, Gotay CC, Snyder C, editors. Outcomes assessment in cancer. Cambridge: Cambridge University Press; 2005. pp. 480–502. [Google Scholar]
- 15.Park M, Choi Y, Tae Y, Choi J, Back S, Lee H. Health Insurance Patients Payments Survey (2010) Seoul: National Health Insurance Corporation; 2011. p. 15. (Korean) [Google Scholar]
- 16.Jung YH, Seo NG, Go SG, Han EJ. A report on the Korea Health Panel Survey of 2008. Seoul: Korea Institute for Health and Social Affairs 2010; p. 38. (Korean) [Google Scholar]
- 17.The Korea Patient Helper Society. Nursing pay guide. [cited 2014 Mar 7]. Available from: http://www.help114.or.kr/(Korean)
- 18.Statistics Korea. Consumer Price Survey (index) guide. 2010. [cited 2014 Mar 7]. Available from: http://kostat.go.kr/portal/english/surveyOutlines/4/2/index.static(Korean)
- 19.Cartwright WS. Methods for the economic evaluation of health care programmes, second edition. By Michael F. Drummond, Bernie O'Brien, Greg L. Stoddart, George W. Torrance. Oxford: Oxford University Press, 1997. J Ment Health Policy Econ. 1999;2(1):43. [Google Scholar]
- 20.Ministry of Employment and Labor. Survey on the structure of wages by the Ministry of Labor in Korea. 2007. [cited 2014 Mar 7]. Available from: http://www.moel.go.kr/view.jsp?cate=3&sec=1&smenu=2&mode=view&bbs_cd=116&state=A&seq=1167352846789(Korean)
- 21.Kim SG, Hahm MI, ChoiI KS, Seung NY, Shin HR, Park EC. The economic burden of cancer in Korea in 2002. Eur J Cancer Care. 2008;17(2):136–144. doi: 10.1111/j.1365-2354.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- 22.Jo HS. Strategies for improvement of primary care in Korea. J Korean Med Assoc. 2012;55(10):959–968. (Korean) [Google Scholar]
- 23.Ministry of Health and Welfare. Korean national health accounts and total health expenditure. 2010. [cited 2014 Mar 7]. Available from: https://www.index.go.kr(Korean)
- 24.Myong JP, Shin JY, Kim SJ. Factors associated with participation in colorectal cancer screening in Korea: the fourth Korean National Health and Nutrition Examination Survey (KNHANES IV) Int J Colorectal Dis. 2012;27(8):1061–1069. doi: 10.1007/s00384-012-1428-4. [DOI] [PubMed] [Google Scholar]
- 25.Shim JI, Kim Y, Han MA, Lee HY, Choi KS, Jun JK, et al. Results of colorectal cancer screening of the national cancer screening program in Korea, 2008. Cancer Res Treat. 2010;42(4):191–198. doi: 10.4143/crt.2010.42.4.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jung KW, Park S, Won YJ, Kong HJ, Lee JY, Seo HG, et al. Prediction of cancer incidence and mortality in Korea, 2012. Cancer Res Treat. 2012;44(1):25–31. doi: 10.4143/crt.2012.44.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fautrel B, Clarke AE, Guillemin F, Adam V, St-Pierre Y, Panaritis T, et al. Costs of rheumatoid arthritis: new estimates from the human capital method and comparison to the willingness-to-pay method. Med Decis Making. 2007;27(2):138–150. doi: 10.1177/0272989X06297389. [DOI] [PubMed] [Google Scholar]
- 28.Martin-Moreno JM, Anttila A, von Karsa L, Alfonso-Sanchez JL, Gorgojo L. Cancer screening and health system resilience: keys to protecting and bolstering preventive services during a financial crisis. Eur J Cancer. 2012;48(14):2212–2218. doi: 10.1016/j.ejca.2012.02.060. [DOI] [PubMed] [Google Scholar]
- 29.Ferrante JM, McCarthy EP, Gonzalez EC, Lee JH, Chen R, Love-Jackson K, et al. Primary care utilization and colorectal cancer outcomes among Medicare beneficiaries. Arch Intern Med. 2011;171(19):1747–1757. doi: 10.1001/archinternmed.2011.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martinez ME. Primary prevention of colorectal cancer: lifestyle, nutrition, exercise. In: Senn HJ, Morant R, editors. Tumor prevention and genetics III. New York: Springer; 2005. pp. 177–211. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of the sources of data used in this study
Colorectal cancer is considered to have few comorbidities in patients who are taking certain pharmaceuticals for diabetes, hypertension, hyperlipidemia, and depression