Abstract
Objectives:
Initial review of patients undergoing screening mammography imaged with a combination of digital breast tomosynthesis (DBT) plus full field digital mammography (FFDM) compared with FFDM alone.
Materials and Methods:
From June 2011 to December 2011, all patients presenting for routine screening mammography were offered a combination DBT plus FFDM exam. Under institutional review board approval, we reviewed 524 patients who opted for combination DBT plus FFDM and selected a sample group of 524 FFDM screening exams from the same time period for a comparative analysis. The χ2 (Chi-square) test was used to compare recall rates, breast density, personal history of breast cancer, and family history of breast cancer between the two groups.
Results:
Recall rate for FFDM, 11.45%, was significantly higher (P < 0001) than in the combination DBT plus FFDM group (4.20%). The biopsy rate in the FFDM group was 2.29% (12/524), with a cancer detection rate of 0.38% (2/524, or 3.8 per 1000) and positive predictive value (PPV) of 16.7% (2/12). The biopsy rate for the DBT plus FFDM group was 1.14% (n = 6/524), with a cancer detection rate 0.57% (n = 3/524, or 5.7 per 1000) and PPV of 50.0% (n = 3/6). Personal history of breast cancer in the FFDM group was significantly lower (P < 0.0001) than in the combination DBT plus FFDM group; 2.5% and 5.7%, respectively. A significant difference in family history of breast cancer (P < 0.0001) was found, with a higher rate in the combination DBT plus FFDM group (36.0% vs. 53.8%). There was a significant difference between the combination DBT plus FFDM group and FFDM alone group, when comparing breast density (P < 0.0147, 61.64% vs. 54.20% dense breasts, respectively) with a higher rate of dense breasts in the DBT plus FFDM group. In follow-up, one cancer was detected within one year of normal screening mammogram in the combination DBT plus FFDM group.
Conclusion:
Our initial experience found the recall rate in the combination DBT plus FFDM group was significantly lower than in the FFDM alone group, despite the fact that the combination DBT plus FFDM group had additional risk factors.
Keywords: Breast imaging, digital breast tomosynthesis, screening mammography
INTRODUCTION

Mammography is the Gold Standard for breast cancer detection and diagnosis, as it has been shown to reduce breast cancer mortality at a rate of 15%-35%.[1] Despite its wide use mammography has limitations. Screening mammography can miss up to 20%-30% of breast cancers.[1,2] Additionally, mammography recall rates average at about 11% with predominantly false positive call-backs.[3,4] One particular shortcoming with the current mammography technology is tissue overlap, which is created by overlap of normal breast structures in a two-dimensional (2D) mammographic projection. Digital breast tomosynthesis (DBT) is a new imaging modality, which can address the limitation of tissue overlap. The only unit to date that has Food and Drug Administration (FDA) approval is a DBT unit that uses a flat panel detector and tube rotation that makes one sweep over the compressed breast. This motion produces a series of projections at different angles creating a three-dimensional (3D) image of the breast that can be reconstructed into a series of slices.[5] The unit can be used for standard full field digital mammography (FFDM) imaging, or combination DBT plus FFDM imaging. Studies to date have evaluated the technology with promising findings.[6,7,8,9,10,11,12,13,14,15,16] In particular, it has been reported that with the addition of DBT, recall rates and false positives can be reduced. Recently, Skaane et al.,[6] published a prospective study of 12, 631 subjects, which found a higher cancer detection rate of 8 per 1,000 in comparison to 6 per 1,000 when mammography alone was used. The study by Skaane et al., detected a substantial number of additional cancers with the use of mammography plus DBT versus mammography alone. However, there was no observed improvement in the detection of ductal carcinoma in situ. As DBT is still in the early phases of implementation, research is ongoing to determine the role this technology will have in the clinical setting: Routine screening mammography or diagnostic evaluation.
As stated previously, FDA approval of one DBT unit came in February of 2011, at which time our facility began using the technology clinically. We report our preliminary experience with patients undergoing screening mammography imaged with combination DBT plus FFDM compared with FFDM alone.
MATERIALS AND METHODS
Institutional review board approval with a waiver of informed consent was obtained. A retrospective review was conducted on patients presenting for screening mammography at our institution from June 2011 through December 2011. One DBT unit was introduced clinically into our facility in June of 2011. All women presenting for screening mammography at our facility were invited to have a combination DBT plus FFDM exam. Patients were informed of the new technology through advertising within our facility, as well as through mailings that were sent to the patients along with their appointment information. During this initial implementation period (initial 2-week period), our facility charged patients a small fee for the DBT examination. A patient could inform the appointment staff, front desk reception staff, or the technologist that she would like to have a combination DBT plus FFDM exam. During this time period, our facility saw a total of 40,174 screening patients. A total of 524 patients presenting for screening mammography who elected to have a combination DBT plus FFDM exam were selected for inclusion in the study. To be included in this analysis, patients were required to have a complete four view screening examination. A sample set of 524 FFDM only screening exams from the same time period (June-December 2011) was also selected for comparative analysis. The control group was randomly selected with the average age matched to the combination DBT plus FFDM group. These patients were also given the option to have a combination DBT plus FFDM; however, they declined.
Patients opting for a combination DBT plus FFDM exam underwent both FFDM and DBT imaging as per the FDA approved procedure. The patients were examined with a commercially available unit (Selenia Dimensions, Hologic, Bedford, MA, USA). Both breasts were imaged in the craniocaudal (CC) and mediolateral oblique (MLO) positions. Those undergoing mammography with FFDM only were examined on a commercially available FFDM unit (Selenia, Hologic; Dimensions, Hologic; Senographe Essential, GE; Fuji CRm, FUJIFILM, USA). The radiation dose per patient for the combination DBT plus FFDM examination for the average size breast is about twice as much as for a routine FFDM study.[9]
Clinical image interpretation was performed by six board-certified radiologists with a range of 1-35 years of experience in breast imaging. All radiologists underwent the new mammographic modality 8 h Mammography Quality Standard Act mandatory training to interpret tomosynthesis images. Image interpretation of the FFDM exams was performed at a Sectra Picture Archiving and Communication System workstation. DBT exams were interpreted at a dedicated tomosynthesis workstation (SecurView, Hologic Inc.). Radiologists performed all image interpretation independently in the clinical environment. A percentage of patients remain in the facility waiting for results, while our radiologists interpret images. Some patients chose to leave without waiting for results and were then contacted with the results of the mammogram, or called back if additional work-up was needed. For the patients waiting for results, if any additional work-up was needed, it was performed during the same visit. All screening examinations were double read. The reading was performed as per our facility protocol with previous imaging available for comparison. Images were not reinterpreted for the purposes of this study. Patients undergoing additional work-up underwent additional mammographic imaging and/or breast ultrasound.
Statistical analysis
The Chi-square test was used to compare recall rates and personal history between the two groups of patients. Wilcoxon rank sum test was used to compare breast densities. Fisher's exact test was used to compare family history of patients in the two groups. A P value of less than 0.05 was considered to indicate a statistically significant difference.
RESULTS
FFDM only group
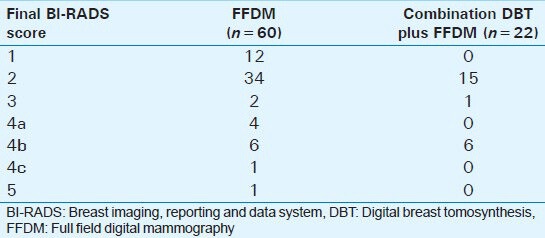
Average patient age in the FFDM group was 59 years (age range: 30-90 years). In this group, 54.30% had heterogeneously dense or extremely dense breasts. Of these 524 patients, 11.45% (n = 60) were recalled for diagnostic work-up. After diagnostic work-up, 14 (23.33%) of the recalls were of masses, 10 (16.67%) microcalcifications, 3 (5%) asymmetries, and 33 (55%) were overlapped tissue. Final Breast Imaging, Reporting and Data System (BI-RADS) score for the recalled cases is shown in [Table 1]. Twelve patients out of the total group of 524 had a vacuum needle core biopsy performed (2.29%); or 12 of the 60 recalled patients (20.0%), resulting in 10 benign findings and two malignant findings (one invasive ductal carcinoma and one ductal carcinoma in situ). The resultant cancer detection rate was 0.38% (2/524, or 3.8 per 1000) and positive predictive value (PPV) of 16.7% (2/12).
Table 1.
Final BI-RADS score of recalled cases per modality
Combination DBT plus FFDM group
Average patient age for the DBT plus FFDM group was 59 years (age range: 36-92 years). In this group, 61.64% had heterogeneously dense or extremely dense breasts. Of these 524 patients, 4.20% (n = 22) were recalled for diagnostic work-up. After diagnostic work-up, 11 (50.0%) of the recalls were of masses, 1 (4.6%) mass with calcium, 5 (22.7%) microcalcifications, 1 (4.6%) asymmetry, and 4 (18.2%) were overlapped tissue. Final BI-RADS score for the recalled cases is shown in [Table 1]. Six ultimately had a vacuum needle core biopsy performed revealing three benign findings and three malignancies; two ductal carcinoma in situ and one invasive ductal carcinoma [Figure 1]. The biopsy rate for this group was 1.14% (n = 6/524), with a cancer detection rate 0.57% (n = 3/524, or 5.7 per 1000) and PPV of 50.0% (n = 3/6).
Figure 1.
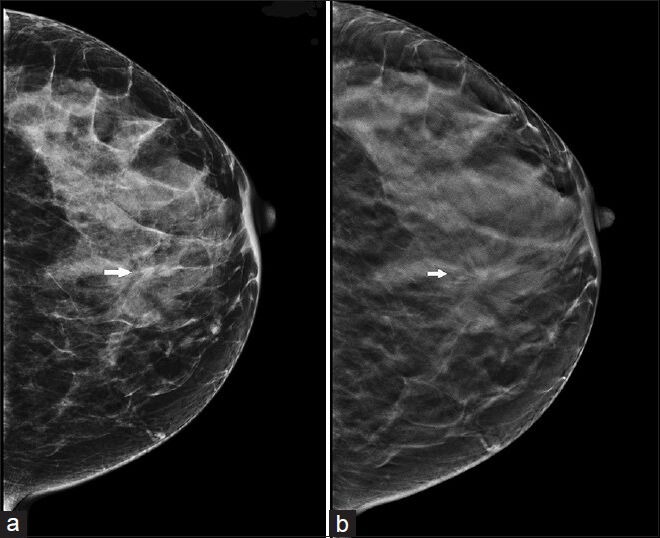
42-year-old asymptomatic woman presents for routine screening with combination digital breast tomosynthesis plus full field digital mammography (a) Full field digital mammography craniocaudal view demonstrates a possible area of architectural distortion (arrow). (b) Digital breast tomosynthesis slice demonstrates the area of architectural distortion more definitively (arrow). Biopsy result was invasive ductal carcinoma.
Recall rates
Six radiologists read the FFDM and the combination DBT plus FFDM exams during the time period of this review. [Figure 2] shows the total exams interpreted per modality by each reader. [Figure 3] shows the recall rates per radiologist for FFDM and the recall rates per radiologist for combination DBT plus FFDM. Of the 524 cases, the recall rate for FFDM, 11.45%, was significantly higher (P < 0.0001) when compared with DBT plus FFDM (4.20%).
Figure 2.
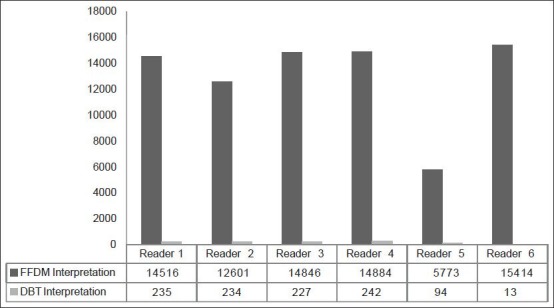
Total examinations interpreted per reader.
Figure 3.
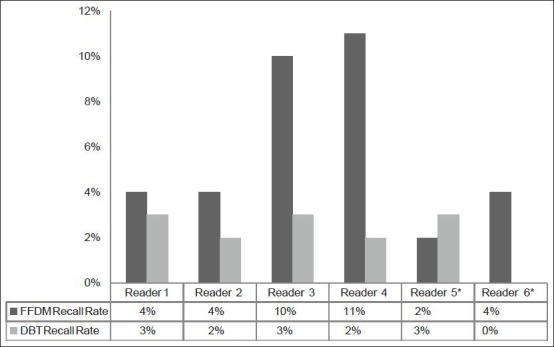
Comparison of recall rates per reader for full field digital mammography and digital breast tomosynthesis during the study period. *Reader 5 had 1 year of experience with mammography and digital breast tomosynthesis (DBT) at the time of this review. Reader 6 had the least amount of experience with DBT.
Additional risk factors
Reported personal history of breast cancer in the FFDM group (n = 13) was significantly lower (P < 0.0001) than in the combination DBT plus FFDM group (n = 30); 2.5% and 5.7%, respectively. There was a significant difference in family history of breast cancer (P <.0001) amongst the groups, with a higher rate in the combination DBT plus FFDM group (36.0% (n = 189) versus 53.8% (n = 282) in the FFDM alone group. There was a significant difference between the FFDM alone and combination DBT plus FFDM groups when comparing heterogeneously dense or extremely dense breast density, with higher breast density in the DBT plus FFDM group (P < O.0147, 54.20% vs. 61.64%, respectively).
Imaging follow-up
Patients were evaluated after 1 year to determine cancer status. A total of 122 of the 524 (23%) patients in the FFDM cohort did not have 1-year follow-up imaging. Of those with 1-year follow-up, 400 had normal/benign findings and two had a cancer diagnosis at subsequent screening (one ductal carcinoma in situ and one invasive mammary carcinoma). Neither of the later cancer diagnoses were interval cancers (within one year of last screening). In the combination DBT plus FFDM group, 77 (15%) patients did not have 1-year imaging follow-up. A total of 443 had normal/benign findings and four had a cancer diagnosis; three invasive ductal carcinomas and one invasive lobular carcinoma. One of the four subsequent cancers was an interval cancer, diagnosed 7 months after the routine screening appointment thus between yearly screening examinations.
DISCUSSION
In the research setting, DBT has been shown to have the ability to reduce recall rates. Early research by Poplack et al.,[7] in 2007 found that approximately half of the findings in the study would not have been recalled when FFDM was supplemented with DBT. Poplack et al., added that when adjusting for confounding conditions, the recall reduction was 40%. Gur et al.,[8] in 2009 published similar findings on the use of combination DBT and FFDM, finding a 30% reduction in recall rate for non-cancer cases that would have led to a recall had FFDM been used alone. Most recently, Rafferty et al.,[9] in 2013 published findings on two-reader studies related to using combination FFDM and DBT compared with FFDM alone. The study found that FFDM and DBT combined improved diagnostic accuracy compared with FFDM alone. A large increase in sensitivity was found for invasive cancers compared with in situ cancers. For non-cancer cases, all readers had a decrease in recall rate, ranging from 6% to 67%.
Our study findings in clinical practice are in agreement with the published research. In our clinical environment, we found the recall rate for FFDM was significantly higher when compared with the recall rate for combination DBT plus FFDM. Readers 1 and 2 had a smaller but significant decrease in recall rate from 4% to 3% (25% reduction) and 4% to 2% (50% reduction), respectively. There was a more significant decrease for Reader 3 and Reader 4; from 10% to 3% (70% reduction) and 11% to 2% (82% reduction), respectively. These two readers had the most dramatic change in recall rate and had these two readers not been included, the overall recall rate decrease may not have been as extreme; however, due to the small sample size further statistical analysis was not performed. Two readers (5 and 6) had an increase in recall by 50% or a decrease by 100% as Reader 5 increased from 2% to 3% and Reader 6 decreased from 4% to 0%, but it should be noted that these readers had the least amount of DBT experience. We feel it is important to report our findings on all readers, as in clinical practice radiologists will have varying levels of mammography experience. While at this time no one can be certain how reader experience with tomosynthesis will change over time, it is clear that there is a learning curve associated with interpreting DBT examinations and there is expected variability among radiologists during the initial clinical implementation.
We found that more than half the recalls in the FFDM group were for overlapped tissue, compared with only 18% in the combination DBT plus FFDM group. This is to be expected as one of the benefits of DBT is the technology's ability to reconstruct the breast into slices, helping to remove the issue of overlapped tissue. This report describes our initial implementation of DBT plus FFDM into clinical practice; we expect the number of recalls due to overlapped tissue to decrease over time. The decrease in recall rate with the use of combination DBT plus FFDM was an important finding, as in our small study the combination DBT plus FFDM group also had additional risk factors such as higher breast density and personal and family history of breast cancer in comparison to the FFDM group. We did have one cancer found in follow-up in the combination DBT plus FFDM cohort. This was an interval cancer as it was diagnosed between annual screening rounds. There were no interval cancers detected in the FFDM group.
Research is still ongoing to determine the best use for DBT; for screening or diagnostic purposes. Several studies to date have evaluated DBT in the diagnostic setting, in particular comparing DBT to the standard mammographic diagnostic views.[11,12,13] Hakim et al.,[11] reported that DBT may be an alternative to current additional mammographic imaging for most, though they do report not for cases of calcifications. Such findings as from Hakim et al., demonstrate one approach for implementing DBT into clinical practice.
Limitations
Our preliminary study did have some limitations. The study cohort was small, due to several factors. The small fee our facility initially charged may have held back patients from opting to have the DBT exam. After we stopped charging the fee, we did see an increase in the number of patients choosing to have the exam. An additional potential reason for the small number of patients opting for DBT is the increased radiation dose associated with the exam. Patients were made aware of the increased dose with DBT and this could have been a factor. We believe that the small cohort in this study may also have been related to limited equipment availability as only one DBT unit was in service at the time.
The combination DBT plus FFDM group included patients having additional risk factors such as personal or family history of breast cancer, prior atypia on biopsy, and dense breast tissue, although the technology was offered to all patients. We believe these patients may have preselected themselves to have their mammography exam with the new technology. The patients that have additional risk factors for breast cancer are often more eager to participate in additional screening that could be helpful in earlier breast cancer detection. We found this to be true for our subset of patients during the study period. Despite this biased population, our study did show decreased recall rates in this group with DBT. Additionally, the cases were imaged during the early stages of clinical implementation of this technology at our facility, when the true benefit offered by the technology may not have yet been optimized. However, even with this limitation and the varying levels of experience among the radiologists, the overall recall rate did drop with DBT, as well as for each reader.
CONCLUSION
The addition of DBT can provide important benefits including reduction in recall rate. In our initial experience in the screening setting, we found the recall rate in the combination DBT plus FFDM group, despite having additional risk factors, such as higher breast tissue density and personal and family history of breast cancer, was significantly lower than in the FFDM group. The technology is still new and in the early stages of adoption into clinical practice. We are excited by the possibilities of this new technology and we will continue to collect our data, as we move forward with its implementation in our practice.
ACKNOWLEDGMENTS
The authors would like to thank David Cavanaugh, MA for his statistical assistance.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/9/127838
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, et al. Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–83. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 2.Holland R, Mravunac M, Hendriks JH, Bekker BV. So-called interval cancers of the breast. Pathologic and radiologic analysis of sixty-four cases. Cancer. 1982;49:2527–33. doi: 10.1002/1097-0142(19820615)49:12<2527::aid-cncr2820491220>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 3.Gur D, Sumkin JH, Rockette HE, Ganott M, Hakim C, Hardesty L, et al. Changes in breast cancer detection and mammography recall rates after the introduction of a computer-aided detection system. J Natl Cancer Inst. 2004;96:185–90. doi: 10.1093/jnci/djh067. [DOI] [PubMed] [Google Scholar]
- 4.Lewin JM, D’Orsi CJ, Hendrick RE, Moss LJ, Isaacs PK, Karellas A, et al. Clinical comparison of full-field digital mammography and screen-film mammography for detection of breast cancer. AJR Am J Roentgenol. 2002;179:671–7. doi: 10.2214/ajr.179.3.1790671. [DOI] [PubMed] [Google Scholar]
- 5.Niklason LT, Christian BT, Niklason LE, Kopans DB, Castleberry DE, Opsahl-Ong BH, et al. Digital tomosynthesis in breast imaging. Radiology. 1997;205:399–406. doi: 10.1148/radiology.205.2.9356620. [DOI] [PubMed] [Google Scholar]
- 6.Skaane P, Bandos AI, Gullien R, Eben EB, Ekseth U, Haakenaasen U, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267:47–56. doi: 10.1148/radiol.12121373. [DOI] [PubMed] [Google Scholar]
- 7.Poplack SP, Tosteson TD, Kogel CA, Nagy HM. Digital breast tomosynthesis: Initial experience in 98 women with abnormal digital screening mammography. AJR Am J Roentgenol. 2007;189:616–23. doi: 10.2214/AJR.07.2231. [DOI] [PubMed] [Google Scholar]
- 8.Gur D, Abrams GS, Chough DM, Ganott MA, Hakim CM, Perrin RL, et al. Digital breast tomosynthesis: Observer performance study. AJR Am J Roentgenol. 2009;193:586–91. doi: 10.2214/AJR.08.2031. [DOI] [PubMed] [Google Scholar]
- 9.Rafferty EA, Park JM, Philpotts LE, Poplack SP, Sumkin JH, Halpern EF, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: Results of a multicenter, multireader trial. Radiology. 2013;266:104–13. doi: 10.1148/radiol.12120674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernardi D, Ciatto S, Pellegrini M, Anesi V, Burlon S, Cauli E, et al. Application of breast tomosynthesis in screening: Incremental effect on mammography acquisition and read time. Br J Radiol. 2012;85:e1174–8. doi: 10.1259/bjr/19385909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hakim CM, Chough DM, Ganott MA, Sumkin JH, Zuley ML, Gur D. Digital breast tomosynthesis in the diagnostic environment: A subjective side-by-side review. AJR Am J Roentgenol. 2010;195:W172–6. doi: 10.2214/AJR.09.3244. [DOI] [PubMed] [Google Scholar]
- 12.Noroozian M, Hadjiiski L, Rahnama-Moghadam S, Klein KA, Jeffries DO, Pinsky RW, et al. Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization. Radiology. 2012;262:61–8. doi: 10.1148/radiol.11101763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brandt KR, Craig DA, Hoskins TL, Henrichsen TL, Bendel EC, Brandt SR, et al. Can Digital breast tomosynthesis replace conventional diagnostic mammography views for screening recalls without calcifications? A comparison study in a simulated clinical setting. AJR Am J Roentgenol. 2013;200:291–8. doi: 10.2214/AJR.12.8881. [DOI] [PubMed] [Google Scholar]
- 14.Gennaro G, Toledano A, di Maggio C, Baldan E, Bezzon E, La Grassa M, et al. Digital breast tomosynthesis versus digital mammography: A clinical performance study. Eur Radiol. 2010;20:1545–53. doi: 10.1007/s00330-009-1699-5. [DOI] [PubMed] [Google Scholar]
- 15.Good WF, Abrams GS, Catullo VJ, Chough DM, Ganott MA, Hakim CM, et al. Digital breast tomosynthesis: A pilot observer study. AJR Am J Roentgenol. 2008;190:865–9. doi: 10.2214/AJR.07.2841. [DOI] [PubMed] [Google Scholar]
- 16.Teertstra HJ, Loo CE, van den Bosch MA, van Tinteren H, Rutgers EJ, Muller SH, et al. Breast tomosynthesis in clinical practice: Initial results. Eur Radiol. 2010;20:16–24. doi: 10.1007/s00330-009-1523-2. [DOI] [PubMed] [Google Scholar]


