Abstract
Tuberculosis globally results in almost 2 million human deaths annually, with 1 in 4 deaths from tuberculosis being human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)-related. Primarily a pathogen of the respiratory system, aerobic Mycobacterium tuberculosis complex (MTBC) infects the lungs via the inhalation of infected aerosol droplets generated by people with pulmonary disease through coughing. This review focuses on M. tuberculosis transmission, epidemiology, detection methods and technologies.
Keywords: Mycobacterium infection and tuberculosis
Introduction
Mycobacterium tuberculosis was first discovered in 1882 by Robert Koch and is one of almost 200 mycobacterial species which have been detected by molecular techniques.1 The genus Actinobacteria (given its own family, the Mycobacteriaceae) includes pathogens known to cause serious diseases in mammals, including tuberculosis (MTBC) and leprosy (M. leprae).1 Mycobacteria are grouped neither as Gram-positive nor Gram-negative bacteria, and have a relatively high average G+C content of 61 to 71 mol% for all species, except M. leprae (57 mol%).2,3 The genome size varies from species to species ranging from 4 to 7 million base pairs (bp).2,3 90% of the genome represents coding regions that potentially encode > 6,000 proteins.2,3 MTBC consists of M. tuberculosis, M. bovis, M. bovis BCG (bacillus Calmette-Guérin), M. africanum M. caprae, M. microti, M. canettii and M. pinnipedii, all of which share genetic homology, with no significant variation between sequences (~0.01 to 0.03%), although differences in phenotypes are present.4 Some species such as M. smegmatis and M. tuberculosis are able to grow in a limited oxygen environment. Cells in the genus have a typical rod, or slightly curved-shape, with dimensions of 0.2 to 0.6 μm by 1 to 10 μm.1
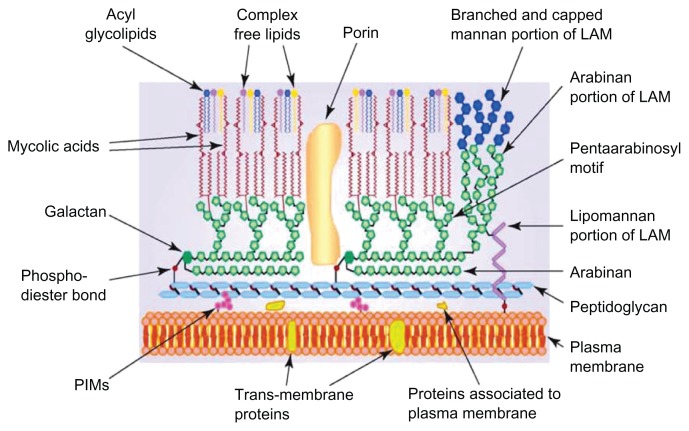
Mycobacterium tuberculosis has a waxy mycolic acid lipid complex coating on its cell surface, making the cells impervious to Gram staining (Fig. 1). Thus, a common staining procedure used is Ziehl-Neelsen (ZN) staining.1 The outer compartment of the cell wall contains lipid-linked polysaccharides consisting of lipoarabinomannan (LAM), lipomannan, phthiocerol dimycocerosate, trehasole, and phosphatidylinositol mannoside, with sulfolipid only being present in M. tuberculosis (Fig. 1).5,6 The outer compartment of the cell wall is soluble and has a role in interacting with the host immune system. The insoluble inner compartment of the cell wall consists of peptidoglycan (PG), arabinogalactan (AG), and mycolic acid (MA). Mycobacteria have some unique qualities that are divergent from members of the Gram-positive group, such as the presence of mycolic acids in the cell wall.5,7
Figure 1.
Schematic representation of Mycobacterium, showing the main components of the outer and inner layer of the cell wall.
Notes: The presence of mycolic acid in the complex of covalent-linked MA-AG-PG is a unique character for identification of the genus Mycobacterium and plays an important role as a permeability barrier. Reproduced with permission from Elsevier.76
Abbreviation: LAM, lipoarabinomannan.
Transmission
MTBC and M. leprae replication occurs in the tissues of warm-blooded human hosts. This air-borne pathogen is transmitted from an active pulmonary tuberculosis patient by coughing.7,8 Droplet nuclei, approximately 1 to 5 μm in size “meander” in the air and are transmitted to susceptible individuals by inhalation. Mycobacteria are incapable of replicating in or on inanimate objects. The risk of infection is dependent to the load of the bacillus that has been inhaled, level of infectiousness, person-to-person contact perimeter and the immune competency of potential hosts. Due to the size of the droplets inhaled into the lungs, the infection penetrates the defense systems of the bronchi and enters the terminal alveoli. Invading bacteria are then engulfed by alveolar macrophage and dendritic cells.7–9 The cell-mediated immune response alleviates the multiplication of M. tuberculosis and halts infection. Tuberculosis can also infect other vital organs of the human body such as the kidneys, spine and brain. Infected individuals with strong immune systems are generally able to combat the infection within 2 to 8 weeks post-infection, when the active cell-mediated immune response stops further multiplication of M. tuberculosis. With latent tuberculosis, the tubercle (infected macrophage or granuloma) bacilli are not completely eradicated from immune system, appearing asymptomatic for a longer period of time.7–9 Although tuberculosis is curable, available treatment regimens merely slow the infection rate rather than eliminating the infection from the population. However, the use of first-line drugs to treat M. tuberculosis does have an effect within 6 months in susceptible patients. For the unsusceptible patient, second-line drug treatments are introduced that are used to treat the multidrug-resistant tuberculosis (MDR-TB).8 Latently infected individuals are non-infectious, and the infection can be detected by tuberculin skin tests (TST) and interferon gamma release assays (IGRA).8 While latent tuberculosis has a low potential to cause recurrent infection (approximately 10%), it has been reported that reactivation of latent tuberculosis (active tuberculosis) may occur after years of post-infection. The risk of reactivation is greater in HIV-infected patients (15%).8 Intracellular replication is initiated before responses of the immune system occurs in the lymph nodes and other extra pulmonary sites, and thus avoids eradication by the host-immune system.8,9
Natural division and growth of Mycobacterium species differs based on slowly-growing to rapidly-growing characteristics. Slowly-growing Mycobacterium (SGM) require more than 7 days for visible growth, as opposed to rapidly-growing Mycobacterium (RGM) which requires < 7 days when grown on Löwenstein-Jensen (L~J) medium. However, the RGM may require > 1 week if grown from clinical specimens.10,11 In healthy adults, tuberculosis progression is generally slow. Tuberculosis infection shows several significant clinical manifestations in pulmonary and extra-pulmonary sites.12 Prolonged coughing, severe weigh-lost, night sweats, low-grade fever, dyspnoea and chest pain are clinical symptoms indicated from pulmonary infections. The extra-pulmonary manifestations of M. tuberculosis infection include meningitis, pleuritis, pericarditis, synovitis, cervical lymphadenitis and infections of the skin, joints, bones and internal organs.8,13 In HIV-infected tuberculosis patients, both types of clinical manifestation are significant due to the rapid progression of infection.
The RGM are grouped as non-tuberculous mycobacteria (NTM) and are opportunistic pathogens that can grow within 7 days in specific growth media.14,15 To date, more than 130 species of RGM have been found.14 Infections due to the RGM are an emerging health problem in the United States.15 The most common RGM to cause human diseases are M. abscessus, M. chelonae, M. fortuitum, and M. massiliense and these have been linked with health care-associated pseudo-outbreaks.14,15 Chronic pulmonary disease and skin/soft-tissue infections are the 2 most common disorders due to these organisms.15 Clinical outcomes in the treatment of M. abscessus infections are generally disappointing.15 Less common human pathogenic RGM species include M. phocacium, M. mucogenicum and M. smegmatis group (known as sensu stricto).14,15 The clinical and microbiologic features of 115 cases involving RGM isolated at the University of Texas from 2000–2005 were examined using 16S ribosomal RNA gene sequencing analysis.14 At least 15 RGM species were included: M. abscessus (43 strains [37.4%]), M. fortuitum complex (33 strains [28.7%]), and M. mucogenicum (28 strains [24.3%]) were the most common, accounting for 90.4%.14 Most M. abscessus (32/43) were isolated from respiratory sources, whereas most M. mucogenicum (24/28) were from blood cultures.14 Antimicrobial susceptibility tests showed that M. abscessus was the most resistant species; M. mucogenicum was most susceptible.14 From blood and catheter sources, 46 strains (40.0%) were isolated; 44 represented bacteremia or catheter-related infections.14 These infections typically manifested as a high fever (mean temperature, 38.9°C), with a high number of RGM colonies cultured.14 All infections resolved with catheter removal and antibiotic therapy.14 Six strains (M. abscessus and M. fortuitum only) were from skin, soft tissue, and wound infections.14 There were 59 strains from respiratory sources, and 28 of these represented definitive to probable infections.14 Prior lung injuries and co-isolation of other pathogenic organisms were common.14 Overall, 78 RGM strains (67.8%) caused true to probable infections without direct deaths.14
The majority of RGM have been found to be sensitive to amikacin, gatifloxacin, moxifloxacin, ciprofloxacin and norfloxacin.16 Although the majority of health care-associated pseudo-outbreak diseases are treatable using antibiotics, the emergence of multidrug-resistant M. abscessus strains worsen the pseudo-outbreak infection scenario, due to the most-virulent and chemotherapy-resistant strains.16,17 Existing diagnostic methods for MDR-TB are slower and take longer to perform in comparison to diagnostics for MTBC common infections. Second-line drug treatment for MDR-TB is relatively expensive due to the long treatment regime required to ensure effectiveness and prevent recurring infections.16,17
Epidemiology
Although all members of MTBC cause infection in humans, M. bovis, M. bovis BCG, M. Microti and M. pinnipedii commonly infect the warm-blooded animal as their primary host. It is likely that transmission occurs from animal to human.18–20 Primarily, animal to human TB transmission cases have been observed in people who have worked or resided in a particular environment.20–23 Unlike M. tuberculosis, non-tuberculous mycobacteria (NTM) are found in the environment, particularly moist habitats such as lakes, rivers and damp-soil. M. avium complex (MAC), M. genavense, M. kansasii, M. xenopi, M. simiae, M. gordonae and some RGM have been recovered from tap water.14,24,25 Some NTM play important roles in nosocomial disease and pseudo-outbreaks and have been isolated from skin, upper respiratory tract, intestinal tract and genital tract of non-symptomatic individuals.26
Mycobacterium bovis is a slow-growing (16 to 20 hour generation time) aerobic bacterium and is the causative agent of tuberculosis in cattle (known as bovine TB). Mycobacterium bovis can also jump the species barrier and cause tuberculosis in humans. The European badger (Meles meles) has been identified as a wildlife reservoir of bovine tuberculosis and a source of transmission to cattle in Britain and Ireland.27 Both behavioral ecology and statistical ecological modeling have indicated the long-term persistence of the disease in some badger communities, and this is postulated to account for the high incidence of bovine tuberculosis in cattle across large tracts of England and Wales.27 Since few of the badgers collected in road traffic accidents between 1972 and 1990 had tuberculosis in counties such as Cheshire, where the disease had until shortly before that been rife in the cattle population, the role of badgers as reservoirs in spreading disease in similar counties outside the south-west of England has to be questioned.27
Mycobacterium africanum and M. canetti tuberculosis infection is mainly reported in tropical Africa.28,29M. africanum can be subdivided into type I (M. bovis-like) and II (M. tuberculosis-like) based on chromosomal deletion distribution and geographic origin.29,30 Infected patients exhibit similar pulmonary clinical features when infected with both strains. However, patients infected with M. africanum type II are more likely to present with major lung complications. 31 Although the main reservoir of M. canetti is unknown, patients show M. tuberculosis-related pulmonary clinical features as well as lymphadenitis in tuberculosis-infected children.
Global Infection Trends
From 2009 to 2012, the majority of tuberculosis cases were reported from less-developed areas, with the highest death rates being recorded in the poorest regions of Africa, India, China and Southeast Asia (approximately 20 to 40 rate per 100,000 population).13,32 The higher prevalence of MTBC in developing countries is known to involve several factors such as poverty and limited access to healthcare systems, close-contact with infected tuberculosis patients, poor nutrition, and reactivation of latent tuberculosis among HIV-infected individuals.1,12,33,34 The World Health Organization (WHO) Millennium Development Goal (MDG) target to halt and reverse the TB epidemic by 2015 has already been achieved.35 New cases of TB have been falling for several years and fell at a rate of 2.2% between 2010 and 2011.35 The TB mortality rate has decreased 41% since 1990 and the world is on track to achieve the global target of a 50% reduction by 2015.35 Mortality and incidence rates are also falling in all of WHO’s 6 regions and in most of the 22 high-burden countries that account for over 80% of the world’s TB cases. At the country level, Cambodia demonstrates what can be achieved in a low-income and high-burden country: new data show a 45% decrease in TB prevalence since 2002.35 However, the global burden of TB remains enormous. In 2011, there were an estimated 8.7 million new cases of TB (13% co-infected with HIV) and 1.4 million people died from TB, including almost 1 million deaths among HIV-negative individuals and 430 000 among people who were HIV-positive.35 Global progress also conceals regional variations; the African and European regions are not on track to halve 1990 levels of mortality by 2015.35 Between 1995 and 2011, 51 million people were successfully treated for TB in countries that had adopted the WHO strategy, saving 20 million lives.35 Progress in responding to multidrug-resistant TB (MDR-TB) remains slow. While the number of cases of MDR-TB notified in the 27 high MDR-TB burden countries is increasing and reached almost 60 000 worldwide in 2011, this is 1 in 5 (19%) of the notified TB patients estimated to have MDR-TB.35 There has been further progress in implementing collaborative TB/HIV activities (first recommended by WHO in 2004). These saved an estimated 1.3 million lives between 2005 and the end of 2011.35
Overall, the reported number global mortality rates from tuberculosis decreased in 2011 among 22 high TB burden countries.35 However, the actual number of deaths from HIV-related tuberculosis cases may still be significantly higher than previously recorded, due to poor diagnosis and the fact that death may not be recorded as being due to tuberculosis. The highest number of HIV-related tuberculosis cases peaked in Africa during the 1980s and increased steadily up to 2004, when extensive treatment and monitoring slowed the epidemic.36 The rise of MDR-TB cases has become a major concern for the WHO. There were an estimated 630,000 cases of MDR-TB among the world’s 12 million prevalent cases reported in 2011 (Table 1).35 This surveillance data is crucial to effectively monitoring the control and spread of global TB.
Table 1.
Estimated burden of disease caused by TB, 2011. Numbers in thousands.a
| Population | Mortalityb | Prevalence | Incidence | HIV-positive incident TB cases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||
| Bestc | Low | High | Best | Low | High | Best | Low | High | Best | Low | High | ||
| Afghanistan | 32358 | 13 | 5.3 | 23 | 110 | 55 | 190 | 61 | 51 | 73 | 0.3 | 0.2 | 0.4 |
| Bangladesh | 150494 | 68 | 29 | 120 | 620 | 300 | 1100 | 340 | 280 | 400 | 0.6 | 0.3 | 1 |
| Brazil | 196655 | 5.6 | 4.6 | 6.8 | 91 | 36 | 170 | 83 | 69 | 97 | 16 | 13 | 19 |
| Cambodia | 14305 | 9.1 | 4.2 | 16 | 120 | 99 | 140 | 61 | 52 | 70 | 3.1 | 2.6 | 3.6 |
| China | 1347565 | 47 | 45 | 49 | 1400 | 1200 | 1600 | 1000 | 890 | 1100 | 13 | 8.6 | 17 |
| DR_Congo | 67758 | 36 | 16 | 65 | 350 | 180 | 570 | 220 | 190 | 250 | 34 | 27 | 41 |
| Ethiopia | 84734 | 15 | 11 | 20 | 200 | 160 | 240 | 220 | 160 | 280 | 38 | 28 | 49 |
| Indiad | 1241492 | 300 | 190 | 430 | 3100 | 2100 | 4300 | 2200 | 2000 | 2500 | 94 | 72 | 120 |
| Indonesia | 242326 | 65 | 29 | 120 | 680 | 310 | 1200 | 450 | 380 | 540 | 15 | 11 | 20 |
| Kenya | 41610 | 9.2 | 4.7 | 15 | 120 | 63 | 200 | 120 | 110 | 120 | 47 | 45 | 49 |
| Mozambique | 23930 | 11 | 4 | 22 | 120 | 56 | 200 | 130 | 91 | 180 | 83 | 58 | 110 |
| Myanmar | 48337 | 23 | 11 | 40 | 240 | 190 | 310 | 180 | 160 | 210 | 18 | 15 | 22 |
| Nigeria | 162471 | 27 | 6.1 | 64 | 280 | 71 | 620 | 190 | 90 | 330 | 50 | 23 | 86 |
| Pakistan | 176745 | 59 | 26 | 110 | 620 | 280 | 1100 | 410 | 340 | 490 | 1.5 | 1 | 2.1 |
| Philippines | 94852 | 28 | 25 | 31 | 460 | 400 | 520 | 260 | 210 | 310 | 1.1 | 0.6 | 1.6 |
| Russian Federation | 142836 | 22 | 22 | 23 | 180 | 72 | 330 | 140 | 120 | 160 | 9.3 | 7.4 | 11 |
| South Africa | 50460 | 25 | 11 | 44 | 390 | 200 | 630 | 500 | 410 | 600 | 330 | 270 | 390 |
| Thailand | 69519 | 9.8 | 4.2 | 18 | 110 | 51 | 200 | 86 | 71 | 100 | 13 | 10 | 15 |
| Uganda | 34509 | 5 | 2.1 | 9 | 63 | 33 | 100 | 67 | 54 | 81 | 35 | 28 | 42 |
| UR_Tanzania | 46218 | 6.4 | 3.3 | 11 | 82 | 43 | 130 | 78 | 73 | 83 | 30 | 28 | 32 |
| Vietnam | 88792 | 30 | 12 | 55 | 290 | 130 | 500 | 180 | 140 | 220 | 14 | 11 | 18 |
| Zimbabwe | 12754 | 6 | 2.4 | 11 | 70 | 37 | 110 | 77 | 59 | 96 | 46 | 36 | 58 |
| High-burden Countriese | 4370719 | 820 | 680 | 980 | 9700 | 8300 | 11000 | 7100 | 6800 | 7500 | 890 | 810 | 970 |
| AFR | 857382 | 220 | 180 | 270 | 2500 | 2100 | 3000 | 2300 | 2100 | 2400 | 870 | 800 | 950 |
| AMR | 943019 | 21 | 18 | 24 | 330 | 250 | 420 | 260 | 240 | 280 | 37 | 34 | 40 |
| EMR | 608628 | 99 | 61 | 150 | 1000 | 660 | 1500 | 660 | 590 | 740 | 8.7 | 7.6 | 9.9 |
| EUR | 899500 | 45 | 44 | 46 | 500 | 370 | 650 | 380 | 350 | 400 | 23 | 20 | 25 |
| SEAR | 1830361 | 480 | 350 | 630 | 5000 | 3800 | 6300 | 3500 | 3200 | 3700 | 140 | 120 | 170 |
| WPR | 1808797 | 130 | 100 | 150 | 2500 | 2200 | 2800 | 1700 | 1500 | 1800 | 36 | 31 | 42 |
| Global | 6947687 | 990 | 840 | 1100 | 12000 | 10000 | 13000 | 8700 | 8300 | 9000 | 1100 | 1000 | 1200 |
Notes:
Numbers for mortality, prevalence and incidence shown to two significant figures. Totals (HBCs, regional and global) are computed prior to rounding;
mortality excludes deaths among HIV-positive TB cases. Deaths among HIV-positive TB cases are classified as HIV deaths according to ICD-10;
best, low and high indicate the point estimate and lower and upper bounds of the 95% uncertainty interval;
estimates for India have not yet been officially approved by the Ministry of Health and Family Welfare, Government of India, and should therefore be considered provisional;
AFR: WHO African Region, AMR: WHO Region of the Americas, EMR: WHO Eastern Mediterranean Region, EUR: WHO European Region, SEAR: WHO South-East Asia Region and WPR: WHO Western Pacific Region. Reproduced with permission from World Health Organization (WHO).35
Diagnosis of M. tuberculosis from Clinical Specimens
The most frequent type of sample used to detect the presence of M. tuberculosis is respiratory expectorate or sputum. Samples are taken from potential patients after clinical manifestations are confirmed by chest X-rays, except for the HIV infected and elderly patients that do not show typical pulmonary clinical features.10,11,37 Conventionally, 3 sputum samples collected from persistent coughing patients are processed to ensure a sufficient number of bacilli.37,38 The sample is suspended in sterile saline (0.85%) or bovine albumin (0.2%) and centrifuged (≥3000 × g, 15 minutes) prior to inoculation of the sediment.37,38
Mycobacterium tuberculosis detection from preprocessed samples is performed by acid-fast staining to identify the presence of acid-fast bacillus (AFB), followed by culturing on solid media. Due to the slowly-growing character of M. tuberculosis, at least 4 to 8 weeks are required for visible growth on solid media.37,38 The Centers for Disease Control and Prevention (CDC) recommends that positive results from AFB smears must be reported after 24 hours of receipt of the specimen.12,38 The standard culture media used in many diagnostic laboratories for identification of M. tuberculosis isolated from sputum samples are L~J, Kirchner solid/liquid media, and Middlebrook (7H9, 7H10 and 7H11) formulation agar and broth. Following confirmation of tuberculosis from standard protocols, an AFB microscopy analysis must be performed to ensure the prescribed treatment is successful.38,40
Microscopy Techniques
The most common microscopy technique used for the detection of mycobacteria is light microscopy combined with a ZN stain smear and is rapid and cheaper in comparison to other methods described below. The sensitivity detection of ZN staining microscopy analysis can be as low as 5 × 103 AFBs/mL and detection proficiency may be between 22% to 80% of culture positive respiratory specimen.10,11 Previous studies have shown that using > 5 mL of a sputum sample increased detection sensitivity by 3-fold AFBs/mL, in contrast to processed/concentrated sputum samples (1 × 103:1 × 106 AFB/mL).39 Whilst the specificity of performing smears to detect mycobacteria is quite high, prolongation of decontamination and concentrating processes from sputum samples, as well as shortening culture incubation time, may result in smear-positive, but culture-negative results.
Fluorescent microscopy with fluorochrome stains, such as single auramine O or the combination of auramine-rhodamine B, is quicker to perform and more sensitive.38 The auramine O fluorescence is enhanced on binding to DNA or RNA as opposed to the carbol fuchsin dye that stains the cell membrane in ZN staining. Despite being more sensitive and taking less time to perform, fluorescent microscopy uses mercury vapor as the light source and so may pose a health risk to the lab operative.40.41 Furthermore, there is a requirement for a dark room, equipment and reagents are more expensive. As a result small laboratories may be cost-compromised. Despite quick results, microscopy analysis using either ZN or fluorochrome staining dyes may potentially give false-positive results due to cross contamination from many sources, such as the presence of Gram-positive-like Nocardia sp.42 False-positive results may also be due to the handling process, suitability of stain used for NTM, the transfer of AFB from slides to slides through immersion oil and misinterpretation of results by untrained lab personnel.43 In addition, light and fluorescent microscopy is not adequately sensitive for the detection of MDR-TB and cannot differentiate between MTBC and NTM.44,45
A peptide nucleic acids (PNAs) fluorescent technique is another alternative in microscopy, which can be used to distinguish between M. tuberculosis and NTM directly in respiratory specimens.38,46 This technique uses a peptide-like structure to replace the sugar phosphate backbone and binds at specific sequences such as 16S rRNA. Due to the hydrophobicity of PNA, it can enter the mycobacterial cell wall and bind to intracellular nucleic acid sequences and is visualized using fluorescent microscopy.46
Culture Techniques
Conventional methods for tuberculosis detection using AFB microscopic staining are insensitive due to the misinterpretation with other genus of AFB group (Gordonia, Norcadia, Rhodococcus and Tsukamurella). Sub-culturing concentrated respiratory specimens, together with clinical indicators, remains the most reliable method of mycobacterial identification. Culture on solid or broth media (selective and non-selective) remains the gold standard method for detection of the phenotypic Mycobacterium.47,48 The option of using solid or liquid media depends on the routine practices and preferences of the laboratory; however, both must be optimized to ensure the rapid detection and reduction of risks for cross contamination. The common media used to culture mycobacterial species is L~J or Kirchner and various Middlebrook formulations (7H9, 7H10 and 7H11).38,49 Egg-based L-J media is most commonly used to recover M. tuberculosis and can poorly recover other species without modifications such as additional of glycerol (M. ulcerans) or substitution of glycerol with pyruvate (M. bovis). Visible colonies may be observed within 18 to 24 days.49,50 Visible growth on an agar-based media (Middlebrook formulation) may be observed in 10 to 12 days. Early growth of microscopic colonies can be observed at 10× and 100× magnifications due to media transparency after 11 days (7H11). Agar-based media can be used for drug susceptibility testing in comparison to egg-based media as this is due to the inhibition of contaminant growth. Like L~J media, substitution and addition of certain chemical compounds facilitates the recovery of mycobacterial species.48–50 Addition of 0.1% enzymatic hydrolysate of casein Middlebrook 7H11 improves the recovery of isonazid-resistant M. tuberculosis. The addition of antimicrobial agents enables the elimination of contaminating organisms and plays a role of selective media. However, the use of selective media should be in conjunction with either egg-or mediabased media.48–50
Immunodiagnostic Tests for Tuberculosis
The immuno-based tests are performed following clinical diagnosis. The classic serologic test for tuberculosis is tuberculin-serological-testing. However, this method is incapable of distinguishing active tuberculosis disease from past-sensitization of BCG, it has unknown predictive values and it allows cross-reaction with NTM.51,52 In clinical application, serological tests have not been used widely due to the insensitivity and low antigen specificity. 2 systems of whole-blood IGRA determination kits, T-SPOT.TB and QuantiFERON Gold In-Tube (QFNG-IT) are also available to use with the TST.51–53 Both systems use the principles of response of T-cell IFN-γ to M. tuberculosis specific antigens (ESAT-6, CFP-10 and TB 7.7) for >16 to 24 hour incubation periods. The T-SPOT.TB assay is based on an enzyme-linked immunospot assay methodology that requires approximately 250,000 peripheral blood mononuclear cells per test well. In contrast, the QFNG-IT is performed by employing whole blood to the M. tuberculosis antigen pre-coated tube which is simpler, quicker and reproducible.53 Studies have shown that several variables affect the diagnosis of pulmonary tuberculosis including age, country of origin, symptoms, AFB positivity and duration of exposure of patient to infection.51–54 Detection sensitivity is higher with IGRA testing kits (QFNGIT and T-SPOT.TB) in comparison with TST.55,56 Although several comparison studies of IGRA for M. tuberculosis have been carried out, their clinical application is still limited, especially among at-risk populations and children.55–57
Nucleic Acid Amplification (NAA) Assays
The limitations of AFB microscopy analysis and the length of time required for culture methods have led to the development of NAA assays.58–60 Polymerase chain reaction (PCR) provides a rapid and specific diagnostic technique for the simultaneous detection and identification of MTBC or NTM species from clinical samples.59–61 However, NAA assays are relatively expensive, requiring a fully equipped laboratory and trained personnel. Several commercially-available kits based on classical PCR or isothermal amplification qualitative assays have been developed. These include Amplified Mycobacterium tuberculosis direct test (AMTD), the AMPLICOR Mycobacterium tuberculosis Test (AMPLICOR M. tuberculosis), the COBAS AMPLICOR M. tuberculosis test and the COBAS TaqMan M. tuberculosis test.62,63
AMTD is the only commercial NAA assay kit approved by Food and Drug Administration (FDA) for smear-positive and smear-negative respiratory specimens due to the higher sensitivity and specificity compared to other NAA assays.37,59,61–63 The AMTB or Gen-Probe assay uses the transcriptional mediated amplification (TMA) and hybridization protection methods to amplify an RNA target gene (16S rRNA) at constant temperature (42°C), in <4 hours.59,63 There are 2 types of AMTD assays, Gen-Probe AMTD and AMTD2. The Gen-Probe AMTD assay detects MTBC rRNA in a single tube, contrary to AMTD2, which enables detection of all organisms within MTBC.61 Following clinical manifestations, smear-positive and smear negative respiratory samples are cultured for tuberculosis infection confirmation and requires up to 8 weeks to obtain culture conversion prior to results validation.64 Therefore, detection using the NAA assay enables early confirmation, especially for culture-negative samples. NAA testing for specimens collected from patients treated with anti-tuberculosis drugs within 12 months is excluded to avoid false-positive results. BD ProbeTec also uses isothermal amplification.65,66 The amplification method used is strand displacement amplification, which amplifies a specific transposable element of M. tuberculosis (IS6110).65–67 The line-probe assay involves amplification followed by reverse hybridization of amplicons to immobilized and membrane-bound probes.68 The commercial first line probe assay provides detection for rifampin-resistant M. tuberculosis from culture and NTM including M. kansasii, M. xenopi, M. avium, M. chelonae, M. scrofulaceum, M. gordonae and M. intracellulare.68 However, a second line-probe assay (GenoType MTBDRplus) was developed to detect the mutation of rpoB and inhA mutation (rifampin and isoniazid resistance) in MTBC, enabling the detection of NTM isolated directly from clinical specimens.69
The simultaneous detection of multiple genetic sequences of M. tuberculosis and mutation in drug resistance can be performed using oligonucleotide microarray technology.70,71 A DNA microarray for simultaneous detection of various drug resistant tuberculosis targeting different genetic markers (katG, inhA, rpoB, rpsL and gyrA) is actively being developed. 40,60 The use of microarray technology may lead to the development of a new biomarker for detection of MDR-and XDR-TB. The urgent need for qualified tuberculosis biomarkers enables the prediction of reactivation and cure and also indicates vaccine-induced protection.73–75
The Xpert MTB/RIF is a rapid molecular test that can diagnose TB and rifampicin resistance within 100 minutes directly from sputum samples.35 Between its endorsement by WHO in December 2010 and the end of June 2012, 1.1 million tests had been purchased by 67 low-and middle-income countries; South Africa (37% of purchased tests) is the leading adopter.35 A 41% price reduction (from US$ 16.86 to US$ 9.98) in August 2012 should accelerate uptake.35 An on-demand patient detection system such as the GeneX-pert system by Cepheid is one of the current detection assays that detects the rifampin-resistance. This single-tube molecular beacon-based real-time PCR assay targets a mutation in the rifampin resistance-determining region (RRDR) of the rpoB gene.72 Although this assay has been approved by the WHO, it is unable to detect isoniazid resistance.72
Discussion
Improved and affordable molecular-based detection technologies for MTBC, including highly sensitive, rapid and less-laborious techniques are needed especially in high-risk populations with poorly-resourced laboratories. There are critical funding gaps for TB care and control.35 Between 2013 and 2015, up to US$ 8 billion per year is needed in low-and middle-income countries, with an annual funding gap of up to US$ 3 billion.35 International donor funding is especially critical to sustain recent gains and make further progress in 35 low-income countries (25 in Africa), where donors provide more than 60% of current funding.35
The modern concept of drug discovery utilizes the integrated knowledge of genomics, proteomics, molecular biology and systems biology to identify more specific targets. The development of new drugs and new vaccines is also progressing. New or re-purposed TB drugs and novel TB regimens to treat drug-sensitive or drug resistant TB are advancing in clinical trials and regulatory review.35 11 vaccines to prevent TB are moving through developmental stages.35 However, to be significantly successful, these potential vaccine(s) must be made affordable and available to developing countries.
Whole-genome sequencing of bacteria has recently emerged as a cost-effective and convenient approach for addressing many microbiological questions.77 In developed countries, the application of next-generation sequencing may soon be sufficiently fast, accurate and cheap to be used in routine clinical microbiology practice, where it could replace many complex current techniques with a single, more efficient workflow.77 During the past 20 years, microbial detection methods that are genetically based, such as real-time PCR and peptide nucleic acid fluorescent hybridization, coexisted with traditional microbiological methods and were typically based on the identification of individual genetic targets.78 For these methods to be successful, a potential cause of infection must be suspected. More recently, multiplex PCR and multiplex RT-PCR were used to enable more broad-range testing based on panels of suspected pathogens.78 PCR-electrospray ionization mass spectrometry (PCR-ESI/MS) has emerged as a technology that is capable of identifying nearly all known human pathogens either from microbial isolates or directly from clinical specimens.78 Assay primers are strategically designed to target one or more of the broad pathogen categories: bacterial, mycobacterial, fungal, or viral.78 With broad-range amplification followed by detection of mixed amplicons, the method can identify genetic evidence of known and unknown pathogens.78 This unique approach supports a higher form of inquiry, asking the following question: What is the genetic evidence of known or unknown pathogens in the patient sample?78 This approach has advantages over traditional assays that commonly target the presence or absence of one or more pathogens with known genetic composition.78 However, the widespread application of these relatively new techniques in clinical laboratories will require significant retraining and method validation, and without significant financial aid will remain in more wealthy countries.
Acknowledgements
Acknowledge any contributions not in the nature of authorship here. RDS is coordinator of the FP7-PEOPLE-2012-IAPP grant ClouDx-i.
Footnotes
Author Contributions
Wrote the first draft of the manuscript: BAT, JSGD, CJL. Contributed to the writing of the manuscript: RDS, WJS. Agree with manuscript results and conclusions: BAT, RDS, CJL, JSGD, WJS. Jointly developed the structure and arguments for the paper: RDS, WJS. All authors reviewed and approved of the final manuscript.
Funding
BAT was funded through a SLAB-KPT scholarship from the Ministry of Higher Education Malaysia and Universiti Tun Hussein Onn Malaysia.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication the authors have provided signed confirmation of their compliance with ethical and legal obligations including but not limited to compliance with ICMJE authorship and competing interests guidelines, that the article is neither under consideration for publication nor published elsewhere, of their compliance with legal and ethical guidelines concerning human and animal research participants (if applicable), and that permission has been obtained for reproduction of any copyrighted material. This article was subject to blind, independent, expert peer review. The reviewers reported no competing interests. Provenance: the authors were invited to submit this paper.
References
- 1.Pfyffer GE, Palicova F. Mycobacterium: General Characteristics, Laboratory Detection, and Staining Procedures. In: Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry M, Warnock DW, editors. Manual of Clinical Microbiology. 10th ed. Vol. 1. Washington: ASM Press; 2011. pp. 472–502. [Google Scholar]
- 2.Cole ST, Brosch R, Parkhill J, et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature. 1998;393(6685):537–44. doi: 10.1038/31159. [DOI] [PubMed] [Google Scholar]
- 3.Zakham F, Belayachi L, Ussery D, et al. Mycobacterial species as case-study of comparative genome analysis. Cell Mol Biol. 2011;57(Suppl):OL1462–9. [PubMed] [Google Scholar]
- 4.Homolka S, Post E, Oberhauser B, et al. High genetic diversity among Mycobacterium tuberculosis complex strains from Sierra Leone. BMC Microbiol. 2008;8(1):103. doi: 10.1186/1471-2180-8-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hett EC, Rubin EJ. Bacterial growth and cell division: a mycobacterial perspective. Microbiol Mol Biol Rev. 2008;72(1):126–56. doi: 10.1128/MMBR.00028-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Draper P. The outer parts of the mycobacterial envelope as permeability barriers. Front Biosci. 1998;3:D1253–61. doi: 10.2741/a360. [DOI] [PubMed] [Google Scholar]
- 7.Brennan PJ. Structure, function and biogenesis of the cell wall of Mycobacterium tuberculosis. Tuberculosis (Edinb) 2003;83(1–3):91–7. doi: 10.1016/s1472-9792(02)00089-6. [DOI] [PubMed] [Google Scholar]
- 8.Ahmad S. Pathogenesis, immunology and diagnosis of latent Mycobacterium tuberculosis infection. Clin Dev Immunol. 2011;2011:814943. doi: 10.1155/2011/814943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obregon-Henao A, Duque-Correa MA, Rojas M. Stable extracellular RNA fragments of Mycobacterium tuberculosis induce early apoptosis in human monocytes via a caspase-8 dependent mechanism. PloS ONE. 2012;7(1):e29970. doi: 10.1371/journal.pone.0029970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown-Elliott BA, Wallace RJJ. Mycobacterium: Clinical and laboratory characteristics of rapidly growing mycobacteria. In: Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry M, Warnock DW, editors. Manual of Clinical Microbiology. 10th ed. Vol. 1. Washington: ASM Press; 2011. pp. 525–38. [Google Scholar]
- 11.Richter E, Brown-Elliott BA, Wallace RJJ. Mycobacterium: Laboratory Characteristics of Slowly Growing Mycobacteria. In: Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry M, Warnock DW, editors. Manual of Clinical Microbiology. 10th ed. Vol. 1. Washington: ASM Press; 2011. pp. 503–24. [Google Scholar]
- 12.Knechel NA. Tuberculosis: Pathophysiology, clinical features, and diagnosis. Crit Care Nurse. 2009;29(2):34–43. doi: 10.4037/ccn2009968. [DOI] [PubMed] [Google Scholar]
- 13.Fitzgerald DW, Sterling TR, Haas DW. Mycobacterium tuberculosis. In: Mandel GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. 7th ed. Philidelphia: Churchill Livingstone Elsevier; 2010. pp. 3129–63. [Google Scholar]
- 14.Han XY, De I, Jacobson KL. Rapidly growing mycobacteria: Clinical and microbiologic studies of 115 cases. Am J Clin Pathol. 2007;128(4):612–21. doi: 10.1309/1KB2GKYT1BUEYLB5. [DOI] [PubMed] [Google Scholar]
- 15.Chan ED, Bai X, Kartalija M, Orme IM, Ordway DJ. Host immune response to rapidly growing mycobacteria, an emerging cause of chronic lung disease. Am J Respir Cell Mol Biol. 2010;43(4):387–93. doi: 10.1165/rcmb.2009-0276TR. [DOI] [PubMed] [Google Scholar]
- 16.Gayathri R, Therese K, Deepa P, Mangai S, Madhavan H. Antibiotic susceptibility pattern of rapidly growing mycobacteria. J Postgrad Med. 2010;56(2):76–8. doi: 10.4103/0022-3859.65278. [DOI] [PubMed] [Google Scholar]
- 17.Leao SC, Tortoli E, Vianna-Niero C, et al. Characterization of mycobacteria from a major Brazilian outbreak suggests that revision of the taxanomic status of members of Mycobacterium chelonae-M. abscessus group is needed. J Clin Microbiol. 2009;47(9):2691–8. doi: 10.1128/JCM.00808-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de la Rua-Domenech R. Human Mycobacterium bovis infection in the United Kingdom: Incidence, risks, control measures and review of the zoonotic aspects of bovine tuberculosis. Tuberculosis (Edinb) 2006;86(2):77–109. doi: 10.1016/j.tube.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Leung A, Tran V, Wu Z, et al. Novel genome polymorphisms in BCG vaccine strains and impact on efficacy. BMC Genomics. 2008;9:413. doi: 10.1186/1471-2164-9-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kiers A, Klarenbeek A, Mendelts B, van Soolingen D, Koëter G. Transmission of Mycobacterium pinnipedii to humans in a zoo with marine mammals. Int J Tuberc Lung Dis. 2008;12(12):1469–73. [PubMed] [Google Scholar]
- 21.Romero B, Aranaz A, Bezos J, et al. Drug susceptibility of Spanish Mycobacterium tuberculosis complex isolates from animals. Tuberculosis (Edinb) 2007;87(6):565–71. doi: 10.1016/j.tube.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Cisneros LF, Valdivia AG, Waldrup K, et al. Surveillance for Mycobacterium bovis transmission from domestic cattle to wild ruminants in a Mexican wildlife-livestock interface area. Am J Vet Res. 2012;73(10):1617–25. doi: 10.2460/ajvr.73.10.1617. [DOI] [PubMed] [Google Scholar]
- 23.Cvetnic Z, Katalinic-Jankovic V, Sostaric B, et al. Mycobacterium caprae in cattle and humans in Croatia. Int J Tuberc Lung Dis. 2007;11(6):652–8. [PubMed] [Google Scholar]
- 24.Esteban J, Martín-de-Hijas NZ, Fernandez AI, Fernandez-Roblas R, Gadea I. Epidemiology of infections due to nonpigmented rapidly growing mycobacteria diagnosed in an urban area. Eur J Clin Microbiol Infect Dis. 2008;27(10):951–7. doi: 10.1007/s10096-008-0521-7. [DOI] [PubMed] [Google Scholar]
- 25.Stout JE, Gadkowski LB, Rath S, Alspaugh JA, Miller MB, Cox GM. Pedicure-associated rapidly growing mycobacterial infection: an endemic disease. Clin Infect Dis. 2011;53(8):787–92. doi: 10.1093/cid/cir539. [DOI] [PubMed] [Google Scholar]
- 26.Lim JM, Kim JH, Yang HJ. Management of infections with rapidly growing mycobacteria after unexpected complications of skin and subcutaneous surgical procedures. Arch Plast Surg. 2012;39(1):18–24. doi: 10.5999/aps.2012.39.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Atkins PJ, Robinson PA. Bovine tuberculosis and badgers in Britain: relevance of the past. Epidemiol Infect. 2013;25:1–8. doi: 10.1017/S095026881200297X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miltgen J, Morillon M, Koeck JL, et al. Two cases of pulmonary tuberculosis caused by Mycobacterium tuberculosis subsp canetti. Emerg Infect Dis. 2002;8(11):1350–2. doi: 10.3201/eid0811.020017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Jong BC, Antonio M, Gagneux S. Mycobacterium africanum—Review of an important cause of human tuberculosis in West Africa. PLoS Negl Trop Dis. 2010;4(9):e744. doi: 10.1371/journal.pntd.0000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mostowy S, Onipede A, Gagneux S, et al. Genomic analysis distinguishes Mycobacterium africanum. J Clin Microbiol. 2004;42(8):3594–9. doi: 10.1128/JCM.42.8.3594-3599.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Jong BC, Hill PC, Aiken A, et al. Clinical presentation and outcome of tuberculosis patients infected by M. africanum versus M. tuberculosis. Int J Tuberc Lung Dis. 2007;11(4):450–6. [PubMed] [Google Scholar]
- 32.Small P. Why India should become a global leader in high-quality, affordable TB diagnostics. Indian J Med Res. 2012;135(5):685–9. [PMC free article] [PubMed] [Google Scholar]
- 33.Balakrishnan S, Vijayan S, Nair S, et al. High diabetes prevalence among tuberculosis cases in Kerala, India. PLoS One. 2012;7(10):e46502. doi: 10.1371/journal.pone.0046502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.El Khechine A, Henry M, Raoult D, Drancourt M. Detection of Mycobacterium tuberculosis complex organisms in the stools of patients with pulmonary tuberculosis. Microbiology. 2009;155(7):2384–9. doi: 10.1099/mic.0.026484-0. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization (WHO) Global Tuberculosis Report. Geneva: WHO Press; 2012. [Google Scholar]
- 36.World Health Organization (WHO) Global Tuberculosis Control: A short update to the 2009 report. Geneva: WHO Press; 2009. [Google Scholar]
- 37.Perkins MD, Cunningham J. Facing the crisis: improving the diagnosis of tuberculosis in the HIV era. J Infect Dis. 2007;196(Suppl 1):S15–27. doi: 10.1086/518656. [DOI] [PubMed] [Google Scholar]
- 38.Watterson SA, Drobniewski FA. Modern laboratory diagnosis of mycobacterial infections. J Clin Pathol. 2000;53(10):727–32. doi: 10.1136/jcp.53.10.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Steingart KR, Ng V, Henry M, et al. Sputum processing methods to improve the sensitivity of smear microscopy for tuberculosis: A systematic review. Lancet Infect Dis. 2006;6(10):664–74. doi: 10.1016/S1473-3099(06)70602-8. [DOI] [PubMed] [Google Scholar]
- 40.Wilson ML. Recent advances in the laboratory detection of Mycobacterium tuberculosis complex and drug resistance. Clin Infect Dis. 2011;52(11):1350–5. doi: 10.1093/cid/cir146. [DOI] [PubMed] [Google Scholar]
- 41.Steingart KR, Henry M, Ng V, et al. Fluorescence versus conventional sputum smear microscopy for tuberculosis: a systematic review. Lancet Infect Dis. 2006;6(9):570–81. doi: 10.1016/S1473-3099(06)70578-3. [DOI] [PubMed] [Google Scholar]
- 42.Saubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. J Clin Microbiol. 2003;41(10):4497–501. doi: 10.1128/JCM.41.10.4497-4501.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tu HZ, Chen CS, Huang TS, et al. Use of a disposable water filter for prevention of false-positive results due to non-tuberculosis mycobacteria in a clinical laboratory performing routine acid-fast staining for tuberculosis. Appl Environ Microbiol. 2007;73(19):6296–8. doi: 10.1128/AEM.00325-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caviedes L, Lee TS, Gilman RH, et al. Rapid, efficient detection and drug susceptibility testing of Mycobacterium tuberculosis in sputum by microscopic observation of broth cultures. The Tuberculosis Working Group in Peru. J Clin Microbiol. 2000;38(3):1203–8. doi: 10.1128/jcm.38.3.1203-1208.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Minion J, Leung E, Menzies D, Pai M. Microscopic-observation drug susceptibility and thin layer agar assays for the detection of drug resistant tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(10):688–98. doi: 10.1016/S1473-3099(10)70165-1. [DOI] [PubMed] [Google Scholar]
- 46.St Amand AL, Frank DN, De Groote MA, Basaraba RJ, Orme IM, Pace NR. Use of specific rRNA oligonucleotide probes for microscopic detection of Mycobacterium tuberculosis in culture and tissue specimens. J Clin Microbiol. 2005;43(10):5369–71. doi: 10.1128/JCM.43.10.5369-5371.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Su W, Feng J, Chiu Y, Huang S, Lee Y. Role of 2-month sputum smears in predicting culture conversion in pulmonary tuberculosis. Eur Respir J. 2011;37(2):376–83. doi: 10.1183/09031936.00007410. [DOI] [PubMed] [Google Scholar]
- 48.Senkoro M, Mfinanga SG, Mørkve O. Smear microscopy and culture conversion rates among smear positive pulmonary tuberculosis patients by HIV status in Dar es Salaam, Tanzania. BMC Infect Dis. 2010;10:210. doi: 10.1186/1471-2334-10-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abe C, Hosojima S, Fukasawa Y, et al. Comparison of MB-Check, BACTEC, and egg-based media for recovery of Mycobacteria. J Clin Microbiol. 1992;30(4):878–81. doi: 10.1128/jcm.30.4.878-881.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bhattacharya S, Roy R, Chowdhury NR, Dasgupta A, Dastidar SG. Comparison of novel bilayered medium with the conventional media for cultivation of Mycobacterium tuberculosis. Indian J Med Res. 2009;130(5):561–6. [PubMed] [Google Scholar]
- 51.Arend SM, Thijsen SF, Leyten EM, et al. Comparison of two interferon-gamma and tuberculin skin test for tracing tuberculosi contacts. Am J Respir Crit Care Med. 2007;175(6):618–27. doi: 10.1164/rccm.200608-1099OC. [DOI] [PubMed] [Google Scholar]
- 52.Mazurek GH, Jereb J, Lobue P, Iademarco MF, Metchock B, Vernon A. Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005;54(RR-15):49–55. [PubMed] [Google Scholar]
- 53.Connell T, Ritz N, Paxton G, Buttery J, Curtis N, Ranganathan S. A three-way comparison of tuberculin skin testing, QuantiFERON-TB Gold and T-SPOT.TB in children. PLoS One. 2008;3(7):e2624. doi: 10.1371/journal.pone.0002624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee JY, Choi HJ, Park I, Hong S, Oh Y, Lim C. Comparison of two commercial interferon-gamma assays for diagnosing Mycobacterium tuberculosis infection. Eur Respir J. 2006;28(1):24–30. doi: 10.1183/09031936.06.00016906. [DOI] [PubMed] [Google Scholar]
- 55.Tavast E, Salo E, Seppala I, Tuuminen T. IGRA tests perform similarly to TST but cause no adverse reactions: pediatric experience in Finland. BMC Res Notes. 2009;2:9. doi: 10.1186/1756-0500-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zellweger JP, Zellweger A, Ansermet S, de Senerclens B, Wrighton-Smith P. Contact tracing using a new T-cell-based test: better correlation with tuberculosis exposure than tuberculin skin test. Int J Tuberc Lung Dis. 2005;9(11):1242–7. [PubMed] [Google Scholar]
- 57.Menzies D, Pai M, Comstock G. Meta-analysis: new tests for the diagnosis of latent tuberculosis infection: areas of uncertainty and recommendations for research. Ann Intern Med. 2007;146(5):340–54. doi: 10.7326/0003-4819-146-5-200703060-00006. [DOI] [PubMed] [Google Scholar]
- 58.Pai M, Kalantri S, Dheda K. New tools and emerging technologies for the diagnosis of tuberculosis: Part II. Active tuberculosis and drug resistance. Expert Rev Mol Diagn. 2006;6(3):423–32. doi: 10.1586/14737159.6.3.423. [DOI] [PubMed] [Google Scholar]
- 59.Soini H, Musser JM. Molecular diagnosis of mycobacteria. Clin Chem. 2001;47(5):809–14. [PubMed] [Google Scholar]
- 60.Forbes BA. Molecular detection and characterization of Mycobacterium tuberculosis. In: Persing DH, Tenover FC, Tang YJ, Nolte FS, Hayden RT, Belkum AV, editors. Molecular microbiology: Diagnostic Principles and Practice. 2nd ed. Washington: ASM Press; 2011. pp. 415–36. [Google Scholar]
- 61.Woods GL. Molecular Techniques in mycobacterial detection. Arch Pathol Lab Med. 2001;125(1):122–6. doi: 10.5858/2001-125-0122-MTIMD. [DOI] [PubMed] [Google Scholar]
- 62.Peter-Getzlaff S, Luthy J, Boddinghaus B, Bottger EC, Springer B. Development and evaluation of a molecular assay for detection of nontuberculous mycobacteria by use of the cobas amplicor platform. J Clin Microbiol. 2008;46(12):4023–8. doi: 10.1128/JCM.01101-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peter-Getzlaff S, Luthy J, Voit A, Bloemberg GV, Bottger EC. Detection and identification of Mycobacterium spp. in clinical specimens by combining the Roche Cobas Amplicor Mycobacterium tuberculosis assay with Mycobacterium genus detection and nucleic acid sequencing. J Clin Microbiol. 2010;48(11):3943–8. doi: 10.1128/JCM.00851-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vijdea R, Stegger M, Sosnovskaja A, Andersen AB, Thomsen VØ, Bang D. Multidrug-resistant tuberculosis: Rapid detection of resistance to rifampin and high or low levels of isoniazid in clinical specimens and isolates. Eur J Clin Microbiol Infect Dis. 2008;27(11):1079–86. doi: 10.1007/s10096-008-0548-9. [DOI] [PubMed] [Google Scholar]
- 65.Rusch-Gerdes S, Richter E. Clinical evaluation of the semi-automated BDProbeTec ET System for the detection of Mycobacterium tuberculosis in respiratory and nonrespiratory specimens. Diagn Microbiol Infect Dis. 2004;48(4):265–70. doi: 10.1016/j.diagmicrobio.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 66.Barrett A, Magee JG, Freeman R. An evaluation of the BD ProbeTec ET system for the direct detection of Mycobacterium tuberculosis in respiratory samples. J Med Microbiol. 2002;51(10):895–8. doi: 10.1099/0022-1317-51-10-895. [DOI] [PubMed] [Google Scholar]
- 67.Fang Z, Doig C, Kenna DT, et al. IS6110-mediated deletions of wild-type chromosomes of Mycobacterium tuberculosis. J Bacteriol. 1999;181(3):1014–20. doi: 10.1128/jb.181.3.1014-1020.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Morgan M, Kalantri S, Flores L, Pai M. A commercial line probe assay for the rapid detection of rifampicin resistance in Mycobacterium tuberculosis: A systematic review and meta-analysis. BMC Infect Dis. 2005;5:62. doi: 10.1186/1471-2334-5-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dubois Cauwelaert N, Ramarokoto H, Ravololonandriana P, Richard V, Rasolofo V. DNA extracted from stained sputum smears can be used in the MTBDRplus assay. J Clin Microbiol. 2011;49(10):3600–3. doi: 10.1128/JCM.00745-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Diaz R, Siddiqi N, Rubin EJ. Detecting genetic variability among different Mycobacterium tuberculosis strains using DNA microarrays technology. Tuberculosis (Edinb) 2006;86(3–4):314–8. doi: 10.1016/j.tube.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 71.Wallis RS, Pai M, Menzies D, et al. Biomarkers and diagnostics for tuberculosis: progress, needs and translation into practice. Lancet. 2010;375(9729):1920–37. doi: 10.1016/S0140-6736(10)60359-5. [DOI] [PubMed] [Google Scholar]
- 72.Al-Ateah SM, Al-Dowaidi MM, El-Khizzi NA. Evaluation of direct detection of Mycobacterium tuberculosis complex in respiratory and nonrespiratory clinical specimens using the Cepheid Gene Xpert® system. Saudi Med J. 2012;33(10):1100–5. [PubMed] [Google Scholar]
- 73.Tortoli E, Mariottini A, Mazzarelli G. Evaluation of INNO-LiPA MYCOBACTERIA v2: Improved reverse hybridization multiple DNA probe assay for mycobacterial identification. J Clin Microbiol. 2003;41(9):4418–20. doi: 10.1128/JCM.41.9.4418-4420.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lebrun L, Weill FX, Lafendi L, et al. Use of the INNO-LiPA-MYCOBACTERIA Assay (Version 2) for identification of Mycobacterium avium-Mycobacterium intracellulare-Mycobacterium scrofulaceum complex isolates. J Clin Microbiol. 2005;43(6):2567–74. doi: 10.1128/JCM.43.6.2567-2574.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Helb D, Jones M, Story E, et al. Rapid detection of Mycobacterium tuberculosis and rifampin resistance by use of on-demand, near-patient technology. J Clin Microbiol. 2010;48(1):229–37. doi: 10.1128/JCM.01463-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Medjahed H, Gaillard J, Reyrat J. Mycobacterium abscessus: a new player in the mycobacterial field. Trends Microbiol. 2010;18(3):117–23. doi: 10.1016/j.tim.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 77.Didelot X, Bowden R, Wilson DJ, Peto TE, Crook DW. Transforming clinical microbiology with bacterial genome sequencing. Nat Rev Genet. 2012;13(9):601–12. doi: 10.1038/nrg3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wolk DM, Kaleta EJ, Wysocki VH. PCR-electrospray ionization mass spectrometry: the potential to change infectious disease diagnostics in clinical and public health laboratories. J Mol Diagn. 2012;14(4):295–304. doi: 10.1016/j.jmoldx.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]