Abstract
Background:
Ayurvedic drugs have been used since ancient times to treat diseases including periodontal diseases. Oral rinses made from ayurvedic medicines are used in periodontal therapy to control bleeding and reduce inflammation. The aim of this clinical study is to verify the efficacy of herbal mouthwash containing Pilu, Bibhitaka, Nagavalli, Gandhapura taila, Ela, Peppermint satva, and Yavani satva on reduction of plaque and gingivitis.
Materials and Methods:
A total of 100 volunteers with clinical signs of mild to moderate gingivitis were selected and assigned to Group A (only scaling done) and Group B (scaling along with the use of herbal mouthwash). After recording the clinical parameters, the patients were instructed to use herbal mouthwash 15 ml for 30 s twice daily after food in Group B and oral hygiene instructions were given to all patients. Plaque and gingivitis assessment were carried out using the plaque index (Silness nd Loe, 1964), Gingival index (Loe And Silness, 1963), Gingival bleeding index (Ainamo and Bay, 1975) at baseline and at 21 days of the herbal mouthwash use. Statistically analysis was carried out using the student's t-test for normally distributed data and Wilcoxson test or Mann-Whitney U-test for skewed data.
Results:
Our results showed that herbal mouthwash was effective in treatment of plaque induced gingivitis in Group B when compared with the Group A.
Conclusion:
Herbal mouthwash is effective in treatment of plaque induced gingivitis and can be effectively used as an adjunct to mechanical therapy with lesser side-effects.
Keywords: Gingivitis, herbal mouthwash, plaque
INTRODUCTION
Periodontal diseases affect the supporting tissues of the teeth. Gingivitis, the mildest form of periodontal disease is generally caused by insufficient oral hygiene.[1] Gingivitis is characterized by inflammation and bleeding of the gums. The main cause of gingivitis is plaque that forms on the surface of teeth and gums. As a main stay to maintain oral hygiene, mechanical plaque control measures are used. Mechanical plaque control techniques are time consuming and require motivation and skill to be performed well; hence, antimicrobial agents have been employed extensively as an adjunct to mechanical cleaning. Several antimicrobial chemical agents such as chlorhexidine, metronidazole etc., have been used. However, these artificial drugs have unpleasant side-effects; so researchers are trying to pay more attention to herbal drugs. Phytotherapy has a long history and has been used world-wide. Plants and plants isolates demonstrates effects that are immune enhancing, anti-inflammatory, anti-cancer etc. (Lee, 2005).[2] Development in alternative medicine research has led to many mouthrinses and tooth-pastes based on plant extracts (Ozakietal., 2006).[2] The aim of this clinical study is to verify the efficacy of herbal mouthwash containing Pilu, Bibhitaka, Nagavalli, Gandhapurataila, Ela, Peppermint satva, Yavani satva on reduction of plaque and gingivitis.
MATERIALS AND METHODS
After obtaining the ethical clearance from the A. M. E's Dental College and Hospital, Raichur, study was conducted. The patients for this study were selected from the Out-patient Department of Periodontics, A. M. E's Dental College and Hospital, Raichur. The present study was a simple randomized, using tossing a coin method, which included a total 100 patients.
Inclusion criteria
Healthy patients 20-45 years.
Minimum of 20 teeth should be present in the dentition, no visible signs of untreated caries.
Patient diagnosed with mild to moderate type of gingivitis.
Patient with bleeding on probing present, clinically.
Patient who had not received any periodontal therapy for the past 6 months.
Patient willing to give the informed consent and willing to comply with the study were selected.
Exclusion criteria
Subjects taking antibiotics or any other drugs within last 3 months.
Pregnant women and lactating mothers.
Medically compromised patients.
Smokers.
Patients who had periodontal pockets in excess of 4 mm.
No partial dentures or clinically unacceptable restorations or bridges.
Patient with orthodontic appliances.
Patient with a known history of allergic to chemical or any herbal products.
Materials used
Materials used were herbal Mouthwash (HiOra[FNx01HiOra Mouthwash Regular- Manufactured by the Himalaya Drug Company Makali, Bangalore 562123 (India).]), each gram of HiOra FNx01 mouthwash containing Pilu (Salvadora persica) - 5.0 mg, Bibhitaka (Terminalia bellerica) - 10 mg, Nagavalli (Piper betel) - 10 mg, Gandhapura taila - 1.2 mg, Ela - 0.2 mg, Peppermint satva - 1.6 mg, Yavanisatva - 0.4 mg. Other materials used were Mouthmirror, Williams periodontal probe, explorer, and ultrasonic scalers.
Group distribution
Patients were randomly assigned to Group A and Group B and an informed consent was obtained from all the patients.
Group A: Patients were treated by scaling alone without the use of herbal mouthwash.
Group B: Patients were treated by scaling along with the usage of herbal mouthwash.
Clinical parameters
Prior to scaling, patient was subjected to assessment of the following clinical parameters.
Plaque index (Silness and Loe, 1964)
Gingival index (Loe and Silness, 1963)
Gingival bleeding index (Ainamo and Bay, 1975).
After recording the clinical parameters in selected patients, a thorough scaling was carried out using ultrasonic scalers in Group A and Group B. The recording of clinical parameters was carried out by main investigator and treatment was carried out by co-investigator. The clinical parameters were assessed on day ‘0’ and 21st day.
Usage of mouthwash
After recording of clinical parameters by the main investigator, patients in Group B were instructed to use herbal mouthwash 15 ml for 30 s twice daily after food that is after breakfast and dinner in order to reduce the bias following brushing in both groups and more over the mouthwashes serve as a popular and simple delivery method that eliminates the bacteria and rinse the food debris from the mouth thereby preventing plaque formation. Oral hygiene instructions were given to all patients.
Statistical analysis
The data were examined for normality by Kolmogorov and Smirnov test. Wherever, the datawere not normally distributed, non-parametric test was used. Data expressed as mean ± standard deviation (SD); comparison of before and after, Group A and Group B were analyzed using the student's t-test for normally distributed data and Wilcoxson test or Mann-Whitney U-test for skewed data. A two tailed P value less than 0.05 was considered as significant. Data analysis was carried out using the SPSS version 16.0.
To examine intra-examiner measurement error, the second measurements were compared to the first ones and Dahlberg's formula was used to calculate the error of estimation. The equation for Dahlberg's formula is
Where D is the difference between two measurements of a pair and n is the number of samples. Table 1 gives the intra - examiner error.
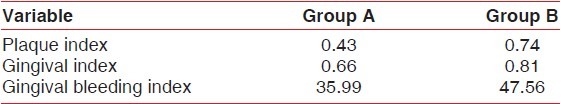
Table 1.
Intra-examiner measurement error
RESULTS
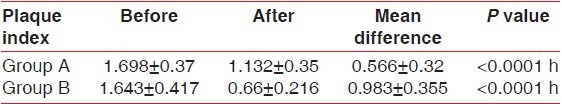
The results showed that there was a significant reduction in plaque scores, gingival index scores, and gingival bleeding index scores both in the Group A and the Group B following scaling as represented in Table 2 (plaque index scores), Graph 1, Table 3 (Gingival index scores), Graph 2, Table 4 (Gingival bleeding index scores), Graph 3. However, a greater reduction in Plaque index scores, gingival index scores, and Gingival bleeding scores were seen in Group B compared with the Group A as mentioned in Table 5, Graph 1–3 and Figures 1–4.
Table 2.
Intra group comparison of plaque index scores before and after treatment
Graph 1.
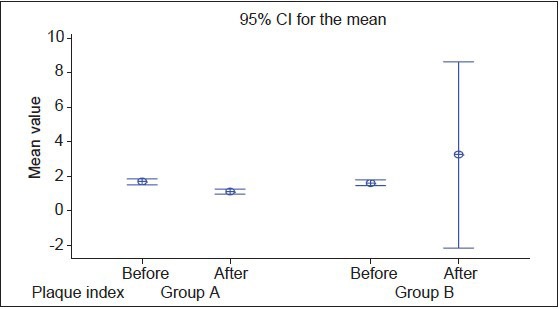
Interval plot of before and after for plaque index in Group A and Group B
Table 3.
Intra group comparison of gingival index scores before and after treatment
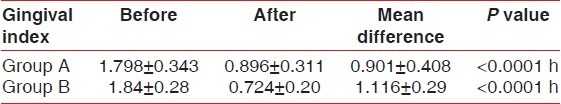
Graph 2.
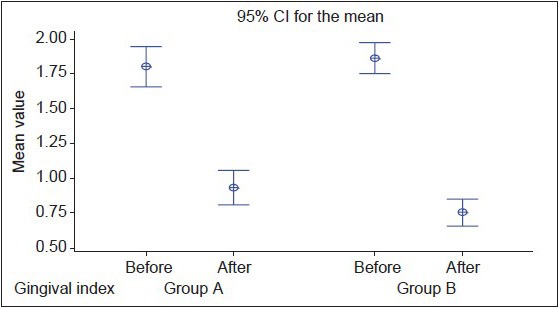
Interval plot of before, after of gingival index for Group A and Group B
Table 4.
Intra group comparison of gingival bleeding index scores before and after treatment
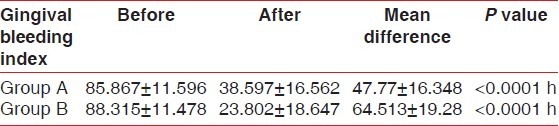
Graph 3.
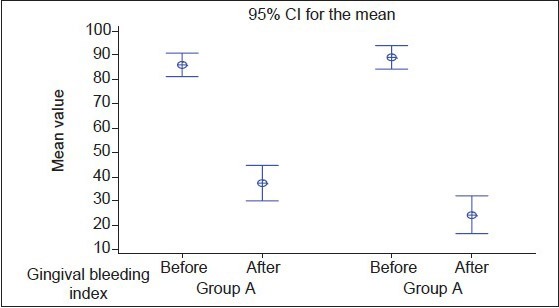
Interval plot of before, after for gingival bleeding index in Group A and Group B
Table 5.
Inter group comparison of plaque index, gingival index, and gingival bleeding index
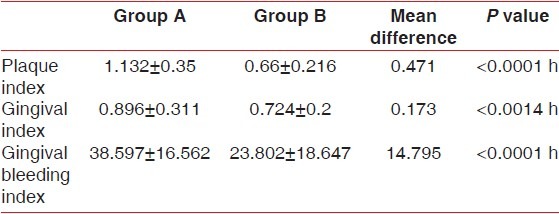
Figure 1.

Pre‑operative photo at ‘0’ day of Group B
Figure 4.

Post‑operative photo at 21st day of Group A
Figure 2.

Post-operative photo at 21st of Group B
Figure 3.

Pre‑operative photo at ‘0’ day of Group A
DISCUSSION
The chemical plaque control is generally considered to be an adjunct to mechanical oral hygiene practices: Agents being most commonly delivered in toothpaste or mouthrinse vehicles.[3] The evaluation of antiplaque agents or formulations typically uses a step-by-step series of clinical study protocols, often supported by laboratory tests, finally culminating in the home-use study(Addy 1995 and Addy and Moran 1997).[3,4] The classic experiments of Loe et al., (1965)[5] demonstrated that accumulation of microbial plaque results in the development of gingivitis and its removal and control results in resolution of the lesions in humans, thereby plaque proving as the microbial etiology of the disease as mentioned by Page (1986).[6] Research centers and World Health Organization prepare lots of programs to make use of plant extracts.[7] Finding plants that have antimicrobial effects and using them as mouthwash have advantages, such as a decreased side-effects and also they are more economical.[7] Ayurvedic drugs have been used since ancient times to treat diseases including periodontal diseases. Oral rinses made from ayurvedic medicines are used in periodontal therapy to control bleeding and reduce inflammation.[8] Dee et al., (1999) evaluated 35 different Indian spices traditionally used.[7] Evidence shows that the herbs such as Bibhitaka (T. bellerica) one of the ingredients of highly praised Ayurvedic compound triphala, used both, internally as well as externally has many of the properties such as astringent, laxative, used in treatment of skin diseases, respiratory diseases etc.,[9] Nagavalli (P. betle) shows the antioxidant, anti-inflammatory, antiplatelet, antimicrobial etc.,[10] Pilu (S. persica) shows antioxidant activity,[11] peppermint that contain menthol activates cold-sensitive TRPM8 (family of Trasient receptor potential ion channels, M stands for melastatin) receptors in the skin and mucosal tissues, and is the primary source of the cooling sensation that follows the topical application of peppermint oil also used as a flavoring agent in tooth pastes, ice creams, confectionaries, chewing gums etc.,[12] Ela is an effective gargle in bad odor of the oral cavity and dental ailments. The paste is also beneficial in the skin diseases, chronic ulcers, and pruritus. Ela oil is used with great benefit in toothache due to infections,[13] Gandhapura taila has analgesic, anti-inflammatory effect used in treatment of joint pains. Here, a first attempt has been made to use these herbal plants in the form of herbal mouthwash. This study was carried out to see the efficacy of herbal plant mouthwash containing Pilu (S. persica), Bibhitaka (T. bellerica), Nagavalli, Gandhapura taila, Ela (Cardamomum), Peppermint satva, and Yavani satva in treatment of gingivitis as an adjunct to scaling. Earlier studies shows evidence of usage of herbal mouthwashes such as Turmeric,[14] neem,[15] and triphala,[8] compared to chlorhexidine showed a significant reduction in plaque indices scores, gingival indices scores, and gingival bleeding index scores as in the present study with a value of plaque index (PI) <0.0001, gingival index (GI) <0.0014 and gingival bleeding index (GBI) <0.0001. The effectiveness of herbal mouthrinse likely was due to the ingredients such as Bibhitiki, Pilu, Gandhapura tailum, which has antimicrobial, anti-inflammatory property. Moreover, the ingredients Ela, Nagavelli it has an added effect on reducing the oral malodor. Though chlorhexidine was developed in 1950, which is still considered one of the most effective antiplaque agents in dentistry. However, long-term usage is limited by its disagreeable taste and propensity to stain the teeth brown.[16] Therefore, a new formulation with similar or superior efficacy and possible with less side-effects and long effect need to be investigated. This herbal mouthwash showed no adverse effects and no staining of teeth with the usage of mouthwash. Limitations of the study were it was dependent on the patient compliance and the study was of short duration.
CONCLUSION
Within the limits of this clinical study, it may be concluded that the ingredients in the herbal oral rinse were effective in controlling plaque and gingivitis. Furthermore, it may serve as a natural antimicrobial mouthrinse alternative for patients who wish to avoid alcohol, artificial preservatives and artificial flavors and colors. Further, clinical and invitro studies are required to clarify and broaden our understanding of the role of this herbal mouthwash in periodontal disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kumar P, Ansari SH, Ali J. Herbal remedies for the treatment of periodontal disease: A patent review. Recent Pat Drug Deliv Formul. 2009;3:221–8. doi: 10.2174/187221109789105603. [DOI] [PubMed] [Google Scholar]
- 2.Rao NJ, Subhas KR, Kumar KS. Role of Phytotherapy in gingivitis; a review. J Pharmacol. 2012;8:1–5. [Google Scholar]
- 3.Yates R, Shearer BH, Huntington E, Addy M. A method to compare four mouthrinses: Time to gingivitis level as the primary outcome variable. J Clin Periodontol. 2002;29:519–23. doi: 10.1034/j.1600-051x.2002.290608.x. [DOI] [PubMed] [Google Scholar]
- 4.Addy M, Moran JM. Evaluation of oral hygiene products: Science is true; don't be misled by the facts. Periodontol 2000. 1997;15:40–51. doi: 10.1111/j.1600-0757.1997.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 5.Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177–87. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 6.Page RC. Gingivitis. J Clin Periodontol. 1986;13:345–59. doi: 10.1111/j.1600-051x.1986.tb01471.x. [DOI] [PubMed] [Google Scholar]
- 7.Dalirsani Z, Aghazedeh M, Adibpour M, Amirchaghamaghi M, Pakfetrat A, Mosannen P, et al. In vitro comparison of the antimicrobial activity often herbal extracts against streptococcus mutans with chlorhexidine. J Appl Sci. 2011;11:878–82. [Google Scholar]
- 8.Anupama D, Anil M, Surangama D. A clinical trial to evaluate the effect of triphala as a mouthwash in comparison with chlorhexidine in chronic generalized periodontitis patient. Indian J Dent Adv. 2010;2:243–7. [Google Scholar]
- 9.Dr. Ripudaman Signh. herb-bibhitaka-terminalia belerica. [Last accessed on 2012 Jun 19]. Available from: http://www.google.com .
- 10.Nagori K, Singh MK, Alexander A, Kumar T, Dewangan D, Badwaik H, Tripathi D. K. L. Piperbetle L: A review on its ethnobotany, phytochemistry, pharmacological profile and profiling by new hyphenated technique DART-MS (direct analysis in real time mass spectrometry) J Pharm Res. 2011;4:2991–7. [Google Scholar]
- 11.Tiwari S, Sarkar B, Dubey G, Jain A. Comparative evaluation of in vitro free radical scavenging activity of different extract of Salvadora persical. Asian J Pharm Life Sci. 2011;1:133–6. [Google Scholar]
- 12.Peppermint from Wikipedia, the free encyclopedia. [Last accessed on 2012 Sep 22]. Available from: http://www.google.com .
- 13.ELA (Elettaria Cardamomum) Herbal cure India world premerier health information site. [Last accessed on 2012 Jun 19]. Available from: http://www.google.com .
- 14.Waghmare PF, Chaudhari AU, Karhadkar VM, Jamkhande AS. Comparative evaluation of turmeric and chlorhexidine gluconate mouthwash in prevention of plaque formation and gingivitis: A clinical and microbiological study. J Contemp Dent Pract. 2011;12:221–4. doi: 10.5005/jp-journals-10024-1038. [DOI] [PubMed] [Google Scholar]
- 15.Chatterjee A, Saluja M, Singh N, Kandwal A. To evaluate the antigingivitis and antipalque effect of an Azadirachtaindica (neem) mouth rinse on plaque induced gingivitis: Adouble-blind, randomized, controlled trial. J Indian Soc Periodontol. 2011;15:398–401. doi: 10.4103/0972-124X.92578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fardal O, Turnbull RS. A review of the literature on use of chlorhexidine in dentistry. J Am Dent Assoc. 1986;112:863–9. doi: 10.14219/jada.archive.1986.0118. [DOI] [PubMed] [Google Scholar]


