Abstract
Central odontogenic fibroma World Health Organization (WHO)-type (OFWT) is a rare lesion that has differential diagnosis with other radiolucent periapical lesions. It has a slow growth and is usually an asymptomatic lesion found in routine examinations. We report a case of a central OFWT occurring in the maxilla, for which the first symptom was teeth mobility, simulating a periodontal condition. A 54-year-old woman, with superior premolar mobility, was referred to our clinic. An oral examination showed teeth vitality and advanced periodontal disease. Radiography showed a unilocular radiolucent area between the left superior lateral incisor and first left molar, with bone reabsorption. The granulomatous tissue was removed and microscopic examination revealed cellular connective tissue with multiple islands of odontogenic epithelium, covered by stratified squamous epithelium, confirming the OFWT diagnosis. The central OFWT is a non-aggressive lesion, with rare recidivism. Biopsy is an important procedure for correct diagnosis and treatment, as some radiolucent lesions can lead to misdiagnosis.
Keywords: Endodontic/diagnosis lesions, intraosseous fibroma, odontogenic fibroma, radiolucent lesions
INTRODUCTION
Central odontogenic fibroma WHO-type is a rare lesion that corresponds to 0.1% of the jaw tumors.[1] It is a benign neoplasm, probably derived from the odontogenic mesenchymal tissue.[2,3,4] Histologically, the odontogenic fibroma is characterized by fibroblastic neoplasia, with a variable amount of odontogenic epithelium that may contain dentin or cementum-like material.[3,5,6] It can occur in the gingiva (peripheral) or intraosseous (central) and most of time can resemble a periodontal or endodontic lesion.[5,7]
It usually appears like an asymptomatic, slow-growing lesion, which can cause cortical expansion with no predilection for the mandible or maxilla.[1,2,3] Radiographic images show a radiolucent lesion, sometimes with a mixed radiodensity and well-defined borders, either uni- or multilocular. There are reports in literature on root reabsorption and displacement.[1,2] The aim of this study is to report a case where a careful diagnosis process was decisive for correct treatment.
CASE REPORT
A 54-year-old Caucasian woman was referred to the clinic of Periodontology at the School of Dentistry of the University of Sγo Paulo, complaining of mobility of tooth 25. Oral examination showed the overlying mucosa and gingiva to be with normal color and texture, with no swelling, accentuated mobility of tooth 25, and no other symptoms or history of pain. Percussion and palpation tests showed normal response. There was generalized advanced periodontal disease compromising the other teeth.
The radiographic examination showed the presence of a unilocular radiolucent area between the left superior lateral incisor and the first left molar [Figure 1]. Computed tomography (CT) showed bone wall reabsorption between the right first premolar and first molar, compromising of the maxillary sinus floor.
Figure 1.
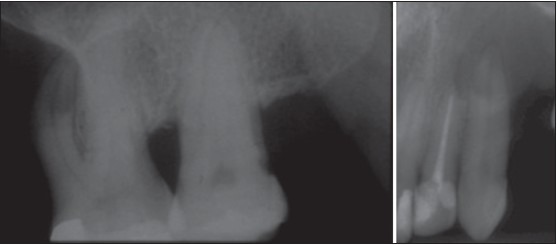
Radiography showing a radiolucent area with bone resorption between teeth 22 and 26
An incisional biopsy was performed; removing all the granulomatous tissue present in the area and tooth 25 was removed, as it was decayed [Figure 2]. The specimen was sent for histopathological analysis [Figure 3]. The microscopic examination revealed a cellular connective tissue with multiple islands and strands of odontogenic epithelium covered by stratified squamous epithelium [Figure 4a]. Immunohistochemical reactions for AE1/AE3 showed positive staining for an odontogenic epithelium, confirming the central odontogenic fibroma WHO-type diagnosis [Figure 4b].
Figure 2.
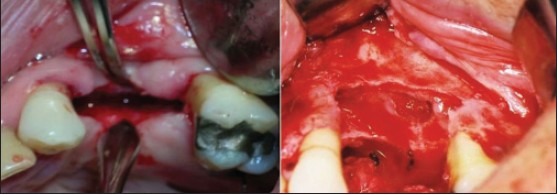
Lesion surgical enucleation and extraction of tooth 26
Figure 3.
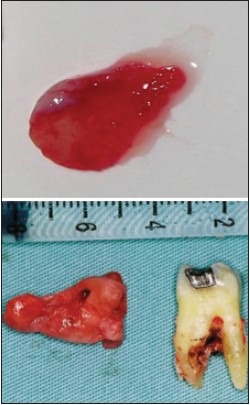
Specimen for histopathological analysis tooth 26
Figure 4.
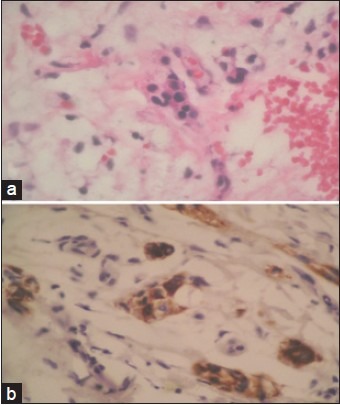
(a) Histological features of the biopsy specimen showing cellular connective tissue and presence of multiple islands and strands of odontogenic epithelium (Hematoxylin-eosin stain; original magnification ×400). (b) Immunohistochemical reaction for AE1/AE3 — positive staining for odontogenic epithelium (original magnification ×400)
The lesion was surgically removed along with other teeth extractions, as the bone support was lost. The patient showed no signs of recidivism after the six-month follow up.
DISCUSSION
The central odontogenic fibroma WHO-type is a rare lesion that often resembles an endodontic lesion or odontogenic tumor. It is usually diagnosed in the second or third decade of life, with a small preference for women (2:1).[1] Most times it is an asymptomatic lesion, and the most frequent sign is swelling and sometimes teeth dislocation.[2,3] Symptoms like pain and paresthesia are uncommon.[3]
The radiographic features may generate doubts, as many lesions have similar characteristics, such as, traumatic bone cyst, ameloblastoma, odontogenic cysts, central giant cell granuloma, and endodontic lesions.[1,2] Most reported cases show a unilocular presentation, and the multilocular aspect may be related to an advanced lesion and more aggressive behavior.[2]
Histologically it has a more complex aspect, with a fibrous connective tissue and enlaced collagen fibers. Presence of calcifications, dentin or cementum can differentiate it from a simple-type odontogenic fibroma.[6] Odontogenic fibroma and similar fibrous lesions of the jaw must also be included in the differential diagnosis. The presence of multiple islands and strands of odontogenic epithelium are also important findings for the diagnosis.[1,3,4,6]
The most recent WHO classification suggested that this variety should be named as the, ‘odontogenic fibroma complex type’ or ‘fibroblastic odontogenic fibroma’.[1] Much confusion existed in the past about the real nature of this entity.
The treatment of choice is surgical excision.[4,6] The lesion is usually easily removed, showing little adherence to the bone. Recidivism is not expected and conservative surgical intervention with enucleation and curettage is often successful.[1] Depending on the extent of the lesion, the bone regenerative procedure may be considered.[3] In our case, there was no need of a bone regenerative procedure and the patient showed good reparation, without a bone defect.
Radiolucent lesions on the periapical region of a non-endodontic origin may lead to wrong initial diagnosis.[3] It is important to include pulp vitality tests and periodontal examinations in the clinical examination.
This case report showed an asymptomatic lesion, which had led to dental dislocation and mobility, and had already compromised the maxillary sinus floor. The patient showed poor oral hygiene and generalized periodontitis, which corroborated with the initial diagnosis of periodontal disease. The clinical characteristics of the presented case could have led to misdiagnosis if biopsy had not been performed. Analysis of the specimen removed at the time of tooth 25 extraction was of great importance for a correct diagnosis. Fortunately, the lesion could be easily removed and no bone defects could be seen after, despite the size and extension of the lesion.
Careful examination of the clinical and radiographic findings as also an incisional biopsy, are important for the correct diagnosis and treatment of radiolucent lesions of the maxillomandibular complex.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Daniels JS. Central odontogenic fibroma of mandible: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:295–300. doi: 10.1016/S1079210404000848. [DOI] [PubMed] [Google Scholar]
- 2.Kaffe I, Buchner A. Radiologic features of central odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994;78:811–8. doi: 10.1016/0030-4220(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 3.Covani U, Crespi R, Perrini N, Barone A. Central odontogenic fibroma: A case report. Med Oral Patol Oral Cir Bucal. 2005;10(Suppl 2):E154–7. [PubMed] [Google Scholar]
- 4.Cicconetti A, Bartoli A, Tallarico M, Maggiani F, Santaniello S. Central odontogenic fibroma interesting the maxillary sinus. A case report and literature survey. Minerva Stomatol. 2006;55:229–39. [PubMed] [Google Scholar]
- 5.Martelli-Júnior H, Mesquita RA, De Paula AM, Pêgo SP, Souza LN. Peripheral odontogenic fibroma (WHO type) of the newborn: A case report. Int J Paediatr Dent. 2006;16:376–9. doi: 10.1111/j.1365-263X.2006.00738.x. [DOI] [PubMed] [Google Scholar]
- 6.Bodner L. Central odontogenic fibroma: A case report. Int J Oral Maxillofac Surg. 1993;22:166–7. doi: 10.1016/s0901-5027(05)80244-9. [DOI] [PubMed] [Google Scholar]
- 7.Garcia BG, Johann AC, da Silveira-Júnior JB, Aguiar MC, Mesquita RA. Retrospective analysis of peripheral odontogenic fibroma (WHO-type) in Brazilians. Minerva Stomatol. 2007;56:115–9. [PubMed] [Google Scholar]


