Abstract
Objectives
To determine the age of significant divergence in body mass index (BMI) and waist circumference in adults with and without the metabolic syndrome, and to provide age- and sex-specific childhood values that predict adult metabolic syndrome.
Study design
Part 1 of this study is a retrospective cohort study of 92 men and 59 women (mean age, 51 years) who had metabolic syndrome and 154 randomly selected adults matched for age and sex who did not have the syndrome. Part 2 is a study of predictive accuracy in a validation sample of 743 participants.
Results
The first appearance of differences between adults with and without metabolic syndrome occurred at ages 8 and 13 for BMI and 6 and 13 for waist circumference in boys and girls, respectively. Odds ratios (ORs) for the metabolic syndrome at 30 years and older ranged from 1.4 to 1.9 across age groups in boys and from 0.8 to 2.8 across age groups in girls if BMI exceeded criterion values in childhood. The corresponding ORs for waist circumference ranged from 2.5 to 31.4 in boys and 1.7 to 2.5 in girls. These ORs increased with the number of examinations.
Conclusions
Children with BMI and waist circumference values exceeding the established criterion values are at increased risk for the adult metabolic syndrome.
The availability of long-term serial data from the Fels Longitudinal Study presents opportunities to directly link obesity, centralized fat pattern, and the metabolic syndrome in adulthood to body mass index (BMI) and waist circumference measured decades earlier in the same individuals as children and to establish criterion values for BMI and waist circumference that predict obesity, centralized fat patterns, and the metabolic syndrome later in life. Recently, we derived age- and sex-specific childhood blood pressures that predict hypertension and the metabolic syndrome in adulthood using a random-effects model in a discovery sample and validated these criterion values in a larger sample using logistic regression.1 In the present study, we apply a similar approach to ascertaining age- and sex-specific values in childhood for BMI and waist circumference that predict the metabolic syndrome later in life.
The National Cholesterol Education Program’s (NCEP) Adult Treatment Panel (ATP) III guidelines define the metabolic syndrome in adults as a cluster of 3, 4, or 5 risk factors that exceed criterion values: waist circumference >102 cm for men and >88 cm for women, systolic blood pressure ≥130 mm Hg and/or diastolic blood pressure ≥85 mm Hg, fasting plasma triglycerides ≥150 mg/dL, fasting plasma high-density lipoprotein (HDL) cholesterol <40 mg/dL for men and <50 mg/dL for women, and fasting plasma glucose ≥110 mg/dL.2 In 2003, the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus recommended lowering the criterion for impaired fasting plasma glucose to 100 mg/dL.3
Currently, there is no agreement on the definition of the metabolic syndrome in children or adolescents. In recent reports, investigators have used arbitrary thresholds for levels of fasting plasma triglycerides, fasting plasma HDL cholesterol, and fasting plasma glucose, coupled with age- and sex-specific ≥90th percentiles for waist circumference and blood pressure from the National Health and Nutrition Examination Survey (NHANES) III to assess the prevalence of the metabolic syndrome in children and adolescents.4–6 In this study, we take a different approach to ascertaining the onset of the metabolic syndrome in children by linking the adult metabolic syndrome directly to childhood risk factors measured in the same individuals decades earlier. This direct linkage permits us to establish criterion values for risk factors in childhood that predict the metabolic syndrome later in life. Equally important is the fact that measured values for these risk factors that fall below the childhood criterion values may be used to predict metabolic health in adulthood.
In the present study, we analyzed serial data for BMI and waist circumference from the Fels Longitudinal Study in the same subjects over many decades. We identified the earliest age of divergence of values for BMI and waist circumference in childhood among adults with the metabolic syndrome and age- and sex-matched adults without the metabolic syndrome. We also established age- and sex-specific criterion values of childhood BMI and waist circumference for predicting the metabolic syndrome later in life in a discovery sample of 305 subjects in the Fels Longitudinal Study and validated the predictive accuracy of these childhood criterion values in a sample of 743 subjects in the Fels Longitudinal Study.
METHODS
Study Sample
The 743 study participants (360 men and 383 women) were drawn from the Fels Longitudinal Study; they were 20 years and older at the time of analysis and had been followed since birth.7 Childhood measurements include weight, height, waist circumference, annual hand-wrist bone age, and blood pressure. These parameters were measured at birth; at 1, 3, 6, 9, and 12 months; every 6 months to age 18 years; and every 2 years thereafter. When these participants reached age 8 years, additional measurements were added to the examination, including levels of fasting plasma lipids and lipoproteins, fasting plasma glucose, and fasting plasma insulin. Approximately 8% of the Fels study participants have been lost to follow-up, but their anthropometric, metabolic and cardiovascular data at last visit do not differ from those of the 92% remaining in the study.
The present study comprises 2 parts. Part 1 is a retrospective cohort study in a discovery sample of 151 subjects (92 men and 59 women; mean age, 51 years) from the Fels Longitudinal Study population. These subjects met the ATP III criteria for the metabolic syndrome. They were matched by age and sex to 154 randomly selected men and women within the Fels study population who did not meet the ATP III criteria. Each of these 305 subjects had been examined an average of 37 times and had no missing values for the 5 risk factors for the metabolic syndrome during their years of participation in the Fels study. Data from these 305 subjects were used to identify the age in childhood when BMI and waist circumference diverge between adults with and without the metabolic syndrome and to establish age- and sex-specific criterion values for these parameters in childhood that predict the metabolic syndrome later in life.
In Part 2 of the study, we validated the accuracy of the age- and sex-specific criterion values for BMI and waist circumference in childhood that we established in Part 1 to predict obesity, waist circumference exceeding ATP III criteria, and the metabolic syndrome later in life. The 743 subjects in Part 2 included the 305 subjects in Part 1. The total of 743 subjects comprised 144 men and 138 women with at least 3 risk factor measurements that exceeded the ATP III threshold values for the metabolic syndrome and 216 men and 245 women with at least 3 risk factor measurements that did not exceed those thresholds. We reviewed the childhood BMI and waist circumference data of the 743 subjects in the validation sample to determine whether their BMI and waist circumference exceeded the age- and sex-specific criterion values that we established in Part 1 at any time during their childhood.
Measurement Protocols
Anthropometric measurements were obtained according to procedures outlined in the Anthropometric Standardization Reference Manual.8 Waist circumference was measured at the suprailiac crest, which is comparable to the method used in the NHANES. Weight was measured to 0.1 kg using a SECA scale, and height was measured to 0.1 cm using a Holtain stadiometer. Waist circumferences were measured twice, and the average values were used for statistical analyses.
We obtained birth weights from hospital records and assessed bone age from hand-wrist radiographs taken at each annual visit.9 We used relative bone age (bone age minus chronological age) to assess the state of biological maturity. A positive relative bone age indicates accelerated maturity, which may hasten the appearance of risk factors in childhood for the metabolic syndrome later in life. All procedures were approved by the Institutional Review Board of Wright State University, and all participants provided written consent to join the Fels Longitudinal Study.
Statistical Analysis
Part 1: Discovery Sample Analysis
We used a random-effects model10 to analyze the complete set of serial data simultaneously. This model is expressed as
yijk = μ + αi + βj + γik + δijxijk + εijk,
where yijk is the dependent variable (ie, serial childhood BMI or waist circumference), i denotes the group variable (adults with the metabolic syndrome versus adults without the metabolic syndrome), j denotes the subject, k denotes the within-subject factor (age), xijk represents the covariates birth weight and relative bone age, and εijk is an error term. Here γik is the difference between the groups with and without the metabolic syndrome, and k is the age at which the dependent variable differs significantly between groups with and without the metabolic syndrome.
We derived annual age- and sex-specific least squares means and standard errors from the fitted random effects models for BMI and waist circumference, with adjustments for relative bone age and birth weight. We chose as childhood criterion values for BMI and waist circumference the age- and sex-specific means that are associated with the metabolic syndrome in adulthood.
Part 2: Validation Sample Analysis
We divided the childhood BMI and waist circumference data of the 743 subjects into 3 age intervals: 5 to 7 years, 8 to 13 years, and 14 to 18 years. These 3 age intervals were chosen to reflect age-by-BMI and age-by-waist circumference interactions during the prepubertal, pubertal, and postpubertal years, respectively. We used logistic regression to link the first appearance of BMI ≥30 kg/m2, waist circumference exceeding ATP III criteria, and/or the metabolic syndrome at age 30 years and older to 2 childhood predictors: elevated BMI (EBMI) and elevated waist circumference (EWC), defined as a single BMI or waist circumference measurement that exceeds age- and sex-specific criteria established in Part 1 at any examination in 1 of the 3 age intervals. We also ascertained the relationship of recurring EBMI and recurring EWC (expressed as the proportion of examinations within an age interval in childhood at which BMI or waist circumference exceeds criterion values established in Part 1) to the odds of developing the metabolic syndrome later in life. We performed logistic models for the 2 dependent variables, adulthood BMI ≥30 kg/m2 and the metabolic syndrome, with childhood BMI as the independent variable. We analyzed the effects of childhood EBMI on the metabolic syndrome independent of the age at which the metabolic syndrome was first diagnosed. We also examined the effects of recurrent EBMI in childhood on the odds of having the metabolic syndrome in adulthood independently of the age at which the metabolic syndrome was first diagnosed. We repeated the analysis with adulthood obesity as the dependent variable, defined as BMI ≥30 kg/m2.
We performed similar logistic models with childhood waist circumference as the independent variable. As the dependent variables in the logistic regression, we used waist circumferences that exceeded ATP III criteria for the metabolic syndrome in adulthood and the metabolic syndrome in adulthood.
Analyses were performed using the SAS, version 9.0.1 (SAS Institute, Cary, NC).
RESULTS
Part 1
The sample characteristics for the 92 men and 59 women who met the ATP III criteria for the metabolic syndrome and the randomly selected 98 men and 56 women matched for age who did not meet the ATP III criteria are presented in Table I (available at www.jpeds.com). Adults with the metabolic syndrome had significantly higher levels of obesity, waist circumferences, dyslipidemia, hypertension, and glucose intolerance than the age-matched adults without the metabolic syndrome.11 The mean waist circumference of affected men was 11.7 cm above the ATP III–defined threshold of 102 cm, and the mean waist circumference of affected women was 20.1 cm above the ATP III–defined threshold of 88 cm.
Table I.
Sample characteristics of the retrospective cohort discovery sample when the metabolic syndrome was first diagnosed (top part) and of the validation sample at the last examination as of June 30, 2006 (bottom part)
| Men | Women | |||
|---|---|---|---|---|
| Metabolic syndrome | Metabolic syndrome | |||
| Variable | No (n = 98) | Yes (n = 92) | No (n = 56) | Yes (n = 59) |
| Age (years) | 49.2 ± 13.9 | 50.9 ± 15.6 | 48 ± 17.2 | 51.4 ± 15 |
| Body weight (kg) | 82.8 ± 13.2 | 101.1 ± 15.6 | 69.4 ± 14.2 | 88.5 ± 18.7 |
| BMI (kg/m2) | 25.6 ± 3.6 | 31.6 ± 4.8 | 25.3 ± 4.8 | 32.7 ± 6.8 |
| Waist circumference (cm) | 96.9 ± 11.2 | 113.7 ± 11.5 | 89.9 ± 11.4 | 108.1 ± 13.7 |
| HDL cholesterol (mg/dL) | 50.4 ± 12 | 37.7 ± 8.1 | 61.9 ± 11.8 | 44.5 ± 9.4 |
| Plasma triglycerides (mg/dL) | 117.2 ± 53.8 | 237.3 ± 153.3 | 105.3 ± 38.4 | 197 ± 76.1 |
| Systolic blood pressure (mmHg) | 124.3 ± 16.2 | 132.8 ± 14.7 | 115.7 ± 14.9 | 128.1 ± 20.8 |
| Diastolic blood pressure (mmHg) | 76.7 ± 9.5 | 83.2 ± 10.5 | 71.7 ± 7.5 | 78.6 ± 10.3 |
| Plasma glucose (mg/dL) | 92.6 ± 10.6 | 104.8 ± 21.1 | 90.4 ± 8.1 | 107.3 ± 40.6 |
| Metabolic syndrome | Metabolic syndrome | |||
| No (n = 216) | Yes (n = 144) | No (n = 245) | Yes (n = 138) | |
| Age (years) | 41 ± 12.1 | 49.1 ± 12.2 | 39.9 ± 11.7 | 50.3 ± 11.8 |
| Body weight (kg) | 78.8 ± 12.4 | 97.3 ± 15.4 | 64.9 ± 13.4 | 80.9 ± 16.5 |
| BMI (kg/m2) | 24.5 ± 3.4 | 30.1 ± 4.3 | 23.5 ± 4.5 | 29.7 ± 5.7 |
| Waist circumference (cm) | 91.5 ± 10.1 | 109 ± 10.3 | 84.1 ± 11.4 | 101.9 ± 11.4 |
| HDL cholesterol (mg/dL) | 51.4 ± 11.6 | 39.2 ± 8.3 | 60.6 ± 13.1 | 47.6 ± 11 |
| Plasma triglycerides (mg/dL) | 110.8 ± 64.7 | 231.5 ± 148 | 87.8 ± 39 | 201.4 ± 96 |
| Systolic blood pressure (mmHg) | 115.3 ± 11.7 | 133 ± 14.5 | 109.1 ± 15.1 | 126.5 ± 17.7 |
| Diastolic blood pressure (mmHg) | 72.4 ± 8.6 | 83.3 ± 10.1 | 66.5 ± 8.9 | 76.9 ± 11.2 |
| Plasma glucose (mg/dL) | 90.9 ± 14.6 | 103.5 ± 20.8 | 84.3 ± 10.4 | 98.6 ± 21.3 |
Values are reported as mean ± standard deviation.
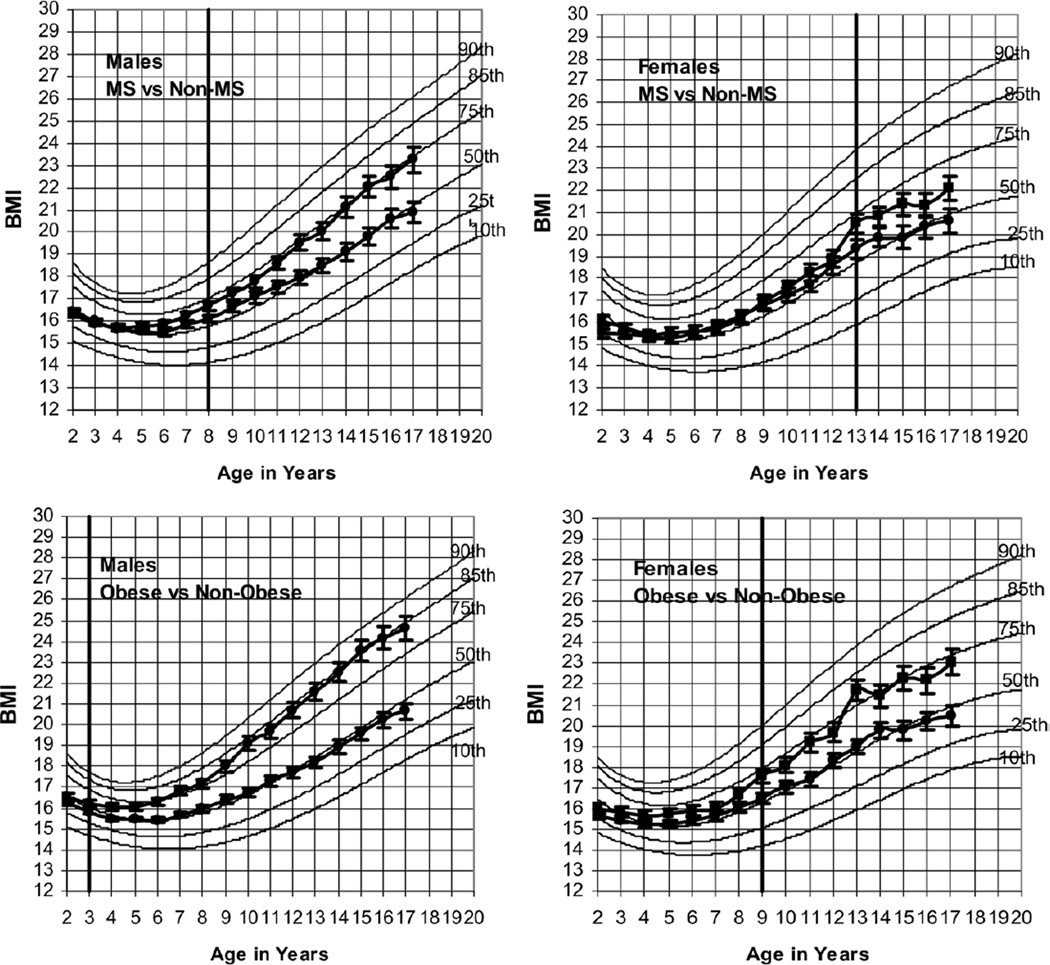
The random effects models indicate that, independent of birth weight and relative bone age, the earliest significant difference in BMI between adults with and without the metabolic syndrome occurred at age 8 in boys and age 13 in girls (P < .1) (Figure 1). We plotted least squares estimated means and standard deviations of BMI in childhood of men and women with and without the metabolic syndrome on Centers for Disease Control and Prevention (CDC) growth charts12 (Figure 1). The vertical lines intersecting the growth curves at age 8 in boys and age 13 in girls indicate the age at which significant divergence first appears between children who later developed the metabolic syndrome and those who did not. Once the curves separated, they remained separate and grew farther apart every year. The differences in BMI between the 2 groups ranged from 0.6 to 2.4 kg/m2 in boys and from 1 to 1.6 kg/m2 in girls.
Figure 1.
Means and standard deviations of BMI in childhood of men and women in the Fels Study with and without the metabolic syndrome (MS) [upper panels] and with or without BMI ≥30 kg/m2 in adulthood [lower panels] plotted on selected BMI percentiles of US CDC growth charts. Data estimated from random effects models with adjustments for birth weight and relative bone age. Vertical lines intersecting the growth curves indicate age at which significant divergence first appears between subjects who will develop the metabolic syndrome [upper panels] or BMI ≥30 kg/m2 [lower panels] in adulthood and those who will not.
BMI values for boys destined to develop the metabolic syndrome (Figure 1) lay along the age-specific 75th percentiles from age 12 to 17. BMI values for girls destined to develop the metabolic syndrome lay approximately along the age-specific 60th percentiles from age 13 to 17 (Figure 1). BMI values for boys not destined to develop the metabolic syndrome lay along the age-specific 50th percentiles from ages 12 to 17, and those for girls not destined to develop the metabolic syndrome lay along the age-specific 50th percentiles from ages 15 to 17 (Figure 1).
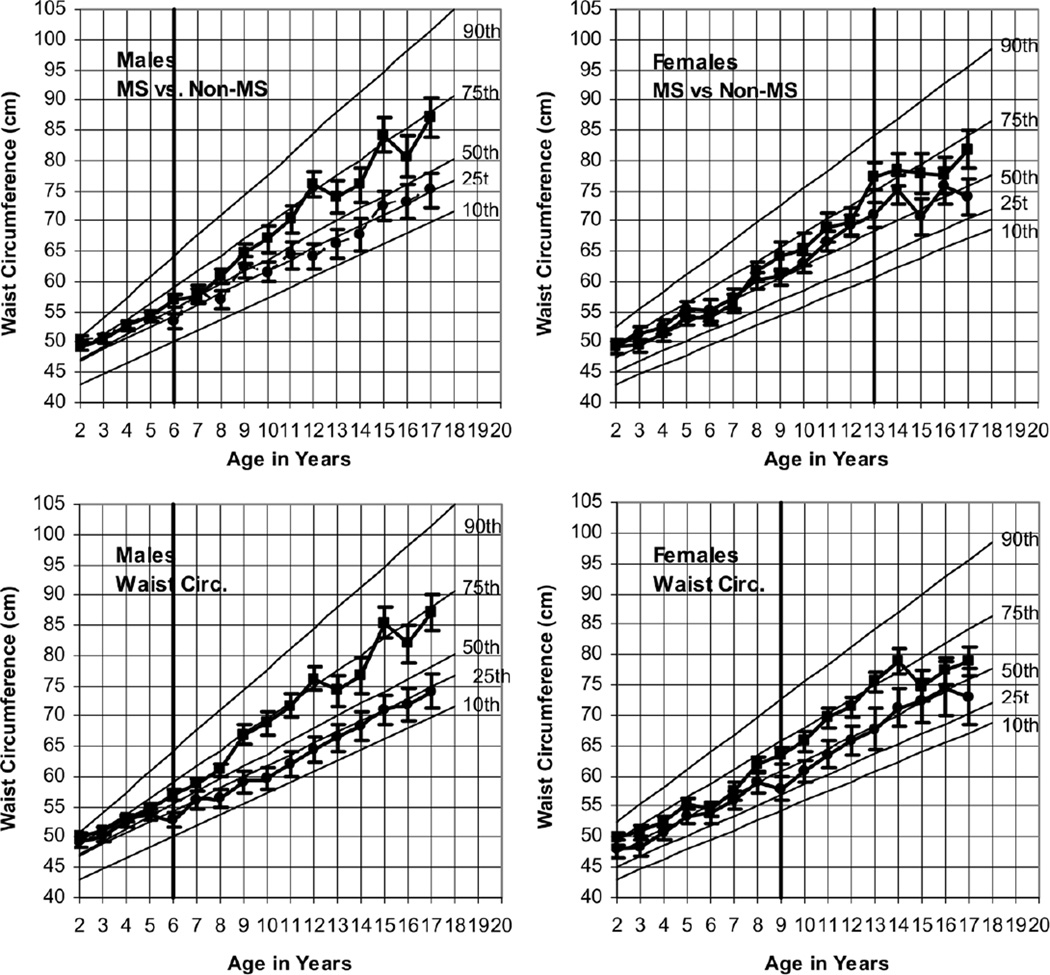
The onset of a significant difference in childhood waist circumference between adults with and without the metabolic syndrome occurred at age 6 in boys and age 13 in girls (P < .1) (Figure 2). Once the curves separated, they remained separate and grew farther apart each year. The differences in waist circumference between the 2 groups ranged from 0.3 to 13 cm in boys and from 5 to 8 cm in girls. Seventeen-year-old boys who later developed the metabolic syndrome had a mean waist circumference of 87 cm, 15 cm below the ATP III threshold of 102 cm. Those who did not develop the metabolic syndrome had a mean waist circumference of 75 cm. The corresponding values for 17-year-old girls were 82 cm—only 6 cm below the ATP III threshold of 88 cm—and 74 cm, respectively. These values indicate the early appearance of sexual dimorphism in mean waist circumference between boys (87 cm) and girls (82 cm) who later developed the metabolic syndrome but not between boys and girls who did not (75 cm for boys and 74 cm for girls). Waist circumference values for boys who later developed the metabolic syndrome approached the age-specific 75th percentiles of the CDC growth charts. The corresponding values for boys who did not develop the metabolic syndrome as adults approached the age-specific 25th percentiles of the CDC growth charts. Comparable plots for girls lay approximately along the age-specific 60th percentiles of the CDC growth charts for those who developed the metabolic syndrome and along the age-specific 50th percentiles for those girls who did not.
Figure 2.
Means and standard deviations of waist circumference in childhood of men and women in the Fels Study with and without the metabolic syndrome (MS), and with or without waist circumference exceeding ATP III criteria in adulthood plotted on selected waist circumference percentiles of NHANES III data. Data estimated from random effects models with adjustments for birth weight and relative bone age. Vertical lines intersecting the growth curves indicate age at which significant divergence first appears between subjects who will develop the metabolic syndrome or waist circumference exceeding ATP III criteria and those who will not.
Birth weight was significantly and positively associated with childhood BMI in both boys and girls and was significantly and positively associated with waist circumference in girls only. Among children of the same age, advanced bone age was associated with a significantly higher BMI increase of 1.4 kg/m2 per year in boys and 2.3 kg/m2 per year in girls (P < .05). Advanced bone age also was associated with a significantly higher increase in waist circumference of 2.8 cm per year in boys and 8 cm per year in girls (P < .05).
Part 2
The characteristics of the 144 men and 138 women who met the ATP III criteria for the metabolic syndrome and the 216 men and 245 women in the Fels study sample who did not meet the ATP III criteria are presented in Table I.
Childhood BMI in Relation to Adulthood Obesity
We evaluated the accuracy of childhood BMI in predicting adult BMI ≥30 kg/m2 using a receiver operating characteristic (ROC) curve. The c statistics of the ROC curves ranged between 0.78 and 0.84 in the males and between 0.83 and 0.87 in the females. These c statistics indicate that the criterion values for childhood BMI established in Part 1 accurately predicted those children who developed BMI ≥30 kg/m2 in adulthood and those who did not.
The odds of becoming obese at 30 years and older in 5- to 18-year-old boys who had a mean BMI at any examination that exceeded the age- and sex-specific criterion values that we established in Part 1 were 1.3 to 16.7 times greater than those in boys in the same age range whose BMI never exceeded these criterion values. Comparable ORs for 5- to 18-year-old girls ranged from 2.3 to 10 (Table II).
Table II.
ORs of adulthood BMI ≥30/adulthood waist circumference >102 cm for men and >88 cm for women and metabolic syndrome at age 30 and older (adjusted for adult age) given BMI/waist circumference exceeding criterion values at a single examination in childhood
| Males | Females | |||||
|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||
| OR | Lower | Upper | OR | Lower | Upper | |
| Adulthood BMI ≥30 | ||||||
| 5 to 7 years | ||||||
| EBMI (yes/no) | 1.3 | 0.6 | 2.7 | 2.3 | 1.1 | 5.1 |
| 8 to 13 years | ||||||
| EBMI (yes/no) | 6.4 | 4.2 | 9.6 | 4.9 | 3.3 | 7.3 |
| 14 to 18 years | ||||||
| EBMI (yes/no) | 16.7 | 10.6 | 26.5 | 10 | 6.9 | 14.6 |
| Metabolic syndrome | ||||||
| 5 to 7 years | ||||||
| EBMI (yes/no) | 1.9 | 1.1 | 3.4 | 0.8 | 0.4 | 1.5 |
| 8 to 13 years | ||||||
| EBMI (yes/no) | 1.4 | 1 | 2 | 1.9 | 1.3 | 2.9 |
| 14 to 18 years | ||||||
| EBMI (yes/no) | 1.8 | 1.3 | 2.5 | 2.8 | 1.9 | 4 |
| Adulthood waist circumference (cm) >102 for men and >88 for women | ||||||
| 5 to 7 years | ||||||
| EWC (yes/no) | 8.6 | 2.1 | 35.2 | 0.1 | 0 | 0.8 |
| 8 to 13 years | ||||||
| EWC (yes/no) | 31.4 | 7.7 | 127.9 | 1.7 | 0.5 | 5.7 |
| 14 to 18 years | ||||||
| EWC (yes/no) | 24.1 | 7.9 | 73.1 | 1.3 | 0.7 | 2.6 |
| Metabolic syndrome | ||||||
| 5 to 7 years | ||||||
| EWC (yes/no) | 2.5 | 0.8 | 8 | 2.5 | 0.6 | 10.4 |
| 8 to 13 years | ||||||
| EWC (yes/no) | 31.4 | 7.7 | 127.9 | 1.7 | 0.5 | 5.7 |
| 14 to 18 years | ||||||
| EWC (yes/no) | 9.6 | 3.6 | 25.7 | 1.8 | 0.8 | 4.1 |
Model: Ln odds of adulthood values exceed cutpoint = Intercept + a (yes(1)/no(0) corresponding childhood values exceeds criterion values) + b (age adulthood BMI ≥30 first discovered).
EBMI, elevated BMI at a single examination in childhood that exceeds age- and sex-specific criteria established the first part of the table; EWC, enlarged waist circumference at a single examination in childhood that exceeds age- and sex-specific criteria established in the first part of the table.
ORs in bold face are significant at P < .05.
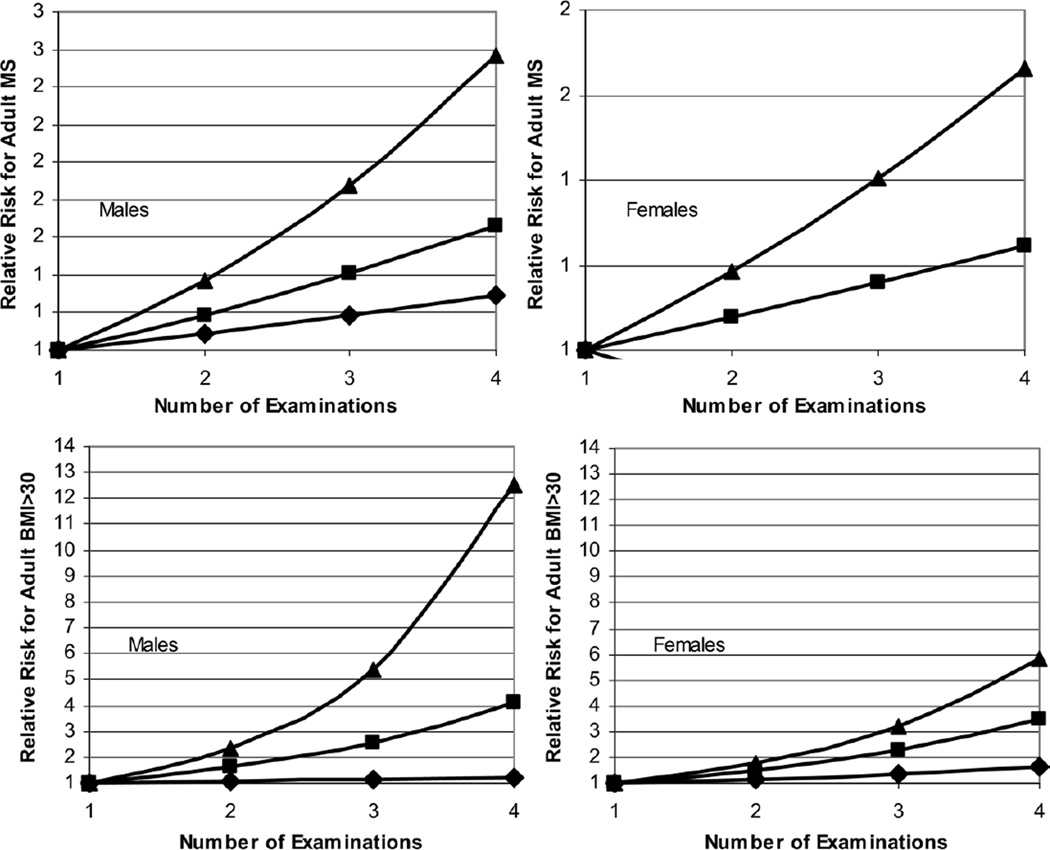
Boys and girls age 8 to 18 with BMI values exceeding the criterion values derived in Part 1 (Figure 1) on more than 1 examination in childhood had significantly higher ORs (1.6 to 29 for boys; 1.5 to 10.5 for girls) of developing BMI ≥30 kg/m2 as adults compared with boys and girls of similar age whose BMI values exceeded the criterion values at only a single examination in childhood (P < .05) (Figure 3).
Figure 3.
Relative risk of obesity (upper panels) and metabolic syndrome (lower panels) in adulthood by number of examinations in childhood at which BMI exceeded criterion values relative to a single examination at which BMI exceeded criterion values.  , 5–8 years;
, 5–8 years;  , 8–13 years;
, 8–13 years;  , 13–18 years.
, 13–18 years.
Childhood BMI in Relation to Adult Metabolic Syndrome
Table II shows the results of a logistic model that uses childhood BMI values to predict the metabolic syndrome in adulthood. ORs ranged from 1.4 to 1.9 in boys and 0.8 to 2.8 in girls. A ROC curve was used to assess the accuracy of the predictions. The c statistics ranged from 0.75 to 0.79 for males and from 0.81 to 0.85 for females, indicating that the criterion values for childhood BMI established in Part 1 accurately predicted which subjects did and did not develop the metabolic syndrome. The ORs of developing the metabolic syndrome were significantly greater in boys with a mean BMI that exceeded age- and sex-specific criterion values on any examination between age 5 and 18 years and girls with a mean BMI that exceeded these criterion values on any examination between age 8 and 18 years compared with boys and girls in the same age ranges whose BMI never exceeded these criterion values (P < .05) (Figure 1).
Boys age 8 to 18 years and girls age 13 to 18 years with recorded BMIs on more than 1 examination exceeding the criterion values had a significantly greater risk of developing the metabolic syndrome (P < .05) than boys and girls of the same age whose BMI values exceeded criterion values at only 1 examination (Figure 3).
Childhood Waist Circumference in Relation to Adulthood Waist Circumference
The accuracy of using childhood waist circumference values exceeding the criterion values established in Part 1 to predict waist circumferences >102 cm in men and >88 cm in women was evaluated using a ROC curve. The c statistics ranged from 0.64 to 0.84 for males and from 0.77 to 0.85 for females, indicating that the criterion values for childhood waist circumference that we established in Part 1 predicted those children who developed waist circumferences that met ATP III criteria in adulthood and those who did not.
The ORs of developing a waist circumference >102 cm at age 30 years and older for 5- to 18-year-old boys with a mean waist circumference at any examination that exceeded the age- and sex-specific criterion values established in Part 1 (Figure 2) were 8.6 to 24.1 times greater (significant at P < .05) than those of boys in the same age range whose waist circumference never exceeded these criterion values (Table II). Comparable ORs for 8-to 18-year-old girls ranged from 1.3 to 1.5.
Boys age 8 to 18 and girls age 13 to 18 with waist circumferences exceeding criterion values on more than 1 examination during childhood had a significantly greater risk of developing waist circumferences exceeding ATP III criteria as adults compared with boys and girls of the same age whose waist circumference values exceeded the criterion values at only 1 examination (P < .05) (Figure 4). The ORs of waist circumference in adulthood meeting ATP III criteria ranged from 1.5 to 18.2 in boys and from 1.4 to 4.1 in girls and varied directly with the number of examinations at which waist circumference exceeded childhood the criterion values established in Part 1.
Figure 4.
Relative risk of centralized fat distribution (upper panels) and metabolic syndrome (lower panels) in adulthood by number of examinations in childhood at which waist circumference exceeded criterion values relative to a single examination at which waist circumference exceeded criterion values.  , 5–8 years;
, 5–8 years;  , 8–13 years;
, 8–13 years;  , 13–18 years.
, 13–18 years.
Childhood Waist Circumference in Relation to Adult Metabolic Syndrome
Table II shows the results of a logistic model using childhood waist circumferences to predict the metabolic syndrome in adulthood. The accuracy of the prediction was evaluated using a ROC curve. The c statistics ranged from 0.74 to 0.78 for males and from 0.75 to 0.78 for females and indicate the ability of the criterion values for childhood waist circumference established in Part 1 to predict which children did and did not develop metabolic syndrome. The OR of developing metabolic syndrome as adults was significantly greater in boys with a mean waist circumference at any examination at age 8 to 18 years that exceeded age- and sex- specific criterion values compared with boys in the same age range whose waist circumference never exceeded those criterion values (P < .05) (Table II). Childhood BMI at any age interval did not contribute significantly to the incidence of adult metabolic syndrome in men or women after childhood waist circumference was included in the models (Table III). Independent of childhood waist circumference, childhood BMI in boys at any age interval did not significantly determine whether waist circumference exceeded ATP III criteria in adulthood (Table III); however, girls’ BMI values did influence their waist circumferences in adulthood independent of their childhood values for waist circumference (Table III).
Table III.
Results of logistic model in predicting adulthood waist circumference (cm) >102 for men and >88 for women
| Males | Females | |||||
|---|---|---|---|---|---|---|
| Parameter | Estimate | Error | P | Estimate | Error | P |
| Waist circumference | ||||||
| 5 to 7 years | ||||||
| Intercept | 2.26 | 4.55 | .6194 | −17.96 | 5.18 | .0005 |
| A | 1.08 | 0.36 | .0027 | −0.96 | 0.43 | .0265 |
| B | −0.32 | 0.31 | .2939 | 0.83 | 0.28 | .0033 |
| C | 0.07 | 0.02 | .0006 | 0.13 | 0.03 | <.0001 |
| 8 to 12 years | ||||||
| Intercept | −3.21 | 2.42 | .1848 | −12.46 | 2.7 | <.0001 |
| A | 1.22 | 0.31 | <.0001 | 0.2 | 0.26 | .4422 |
| B | −0.07 | 0.12 | .5763 | 0.39 | 0.12 | .0014 |
| C | 0.13 | 0.03 | .0002 | 0.17 | 0.05 | .0008 |
| 13 to 18 years | ||||||
| Intercept | −4.96 | 2.34 | .0339 | −11.69 | 2.49 | <.0001 |
| A | 1.59 | 0.28 | <.0001 | 0.15 | 0.16 | .3681 |
| B | 0 | 0.09 | .9975 | 0.32 | 0.07 | <.0001 |
| C | 0.15 | 0.05 | .0023 | 0.16 | 0.04 | .0002 |
| Metabolic syndrome | ||||||
| 5 to 7 years | ||||||
| Intercept | −0.84 | 4.03 | .835 | −0.81 | 4.1 | .8436 |
| A | 0.46 | 0.3 | .126 | 0.46 | 0.36 | .2008 |
| B | −0.13 | 0.27 | .6411 | −0.2 | 0.24 | .4067 |
| C | 0.06 | 0.02 | .0006 | 0.08 | 0.02 | .0003 |
| 8 to 12 years | ||||||
| Intercept | 2.24 | 2.61 | .3913 | −9.89 | 2.56 | .0001 |
| A | 1.72 | 0.36 | <.0001 | 0.26 | 0.31 | .4067 |
| B | −0.42 | 0.14 | .0037 | 0.12 | 0.11 | .2763 |
| C | 0.15 | 0.04 | <.0001 | 0.18 | 0.05 | <.0001 |
| 13 to 18 years | ||||||
| Intercept | −6.68 | 2.07 | .0013 | −11.14 | 2.24 | <.0001 |
| A | 1.13 | 0.25 | <.0001 | 0.3 | 0.2 | .1344 |
| B | −0.05 | 0.08 | .5483 | 0.11 | 0.06 | .0861 |
| C | 0.22 | 0.04 | <.0001 | 0.23 | 0.05 | <.0001 |
Logistic model: Ln odds of adulthood waist circumference exceeds standard criteria = Intercept + a (yes(1)/no(0) childhood waist circumference exceeds criterion values) + b (childhood BMI) + c (age adulthood waist circumference exceeds standard criteria first discovered).
Boys age 8 to 18 years and girls age 13 to 18 years with recorded waist circumferences exceeding criterion values on more than 1 examination had significantly higher ORs of developing the metabolic syndrome as adults (P < .05) than boys and girls of the same age whose waist circumference values exceeded criterion values on only 1 examination (Figure 4).
DISCUSSION
Obesity tracks from childhood into adulthood; however, because of the paucity of serial data on individuals over several decades, little is known about the accuracy of BMI and waist circumference measurements in childhood for predicting BMI ≥30 kg/m2, waist circumference meeting ATP III criteria, and/or the metabolic syndrome in adulthood. In this study, we determined that the onset of pathological values for BMI and waist circumference begins in childhood in those subjects destined to develop the metabolic syndrome. We also established and validated childhood criterion values for BMI and waist circumference that predict the development of the metabolic syndrome later in life. This report directly links childhood BMI and waist circumference and the metabolic syndrome ascertained in the same subjects decades later.
The set of childhood values for BMI and waist circumference in adults who did not develop the metabolic syndrome can be used by health care professionals to predict with some certitude those children who will not develop the metabolic syndrome as adults. The onset of a difference in BMI (P < .1) between adults with and without the metabolic syndrome occurred at age 8 in boys and 13 in girls. BMI values in childhood for men with the metabolic syndrome approach the 75th percentile for BMI of the CDC growth charts,12 whereas the corresponding BMI values for boys who did not develop the metabolic syndrome as adults tracked along the 50th percentile. Our results imply that the current CDC age- and sex-specific percentile thresholds for overweight (≥95th percentile) and at risk of overweight (between the 85th and 95th percentiles) are overly conservative; our data show that children with BMI >50th percentile are at risk of significant metabolic consequences later in life.
BMI values diverged between adults with BMI <30 kg/m2 and with BMI ≥30 kg/m2 as early as age 3 in boys and age 9 in girls (Figure 1), and a significant difference in childhood waist circumference between adults with and without the metabolic syndrome began at age 6 in boys and age 13 in girls. In boys, having an EWC at a single examination at any age generated significant ORs for the development of a waist circumference >102 cm in adulthood, and having an EWC at a single examination at age 8 to 18 generated significant ORs for developing the metabolic syndrome as adults (Table II). The situation in girls was quite different. Finding an EWC at a single examination at any age in girls did not generate significant ORs for developing either a waist circumference >88 cm or the metabolic syndrome in adulthood. In fact, girls age 5 to 7 years with an EWC appear to be protected from developing a waist circumference >88 cm in adulthood (Table II), although this finding is of borderline statistical significance. These findings may reflect the fact that the NCEP ATP III waist circumference criterion value for a diagnosis of the metabolic syndrome in women is set so low as to be noninformative. In our discovery sample, 71% of all the women had waist circumferences >88 cm, and 100% of the women with 3 of 5 positive risk factors had waist circumferences >88 cm. The mean waist circumference of women in the Fels Longitudinal Study with the metabolic syndrome was 20.1 cm greater than the NCEP ATP III threshold of 88 cm. Therefore, our ability to detect true statistical associations is weakened by the lack of variation in waist circumference in adult women in the Fels Longitudinal Study. In the boys, the ORs for developing a waist circumference >102 cm in adulthood were significant in all age groups, given a single observation of an EWC in childhood. This sex-specific discrepancy may reflect the fact that the NCEP ATP III criterion for a waist circumference diagnostic of the metabolic syndrome is set 14 cm higher in men than in women and thus is more discriminating.
Waist circumferences in childhood for men with the metabolic syndrome approach the 75th percentile of the CDC growth charts. The corresponding values for subjects who did not develop the metabolic syndrome tracked along the 25th percentile.13 The ability of BMI and waist circumference measured as early as age 6 to 8 years in boys and age 9 to 13 years in girls to predict the metabolic syndrome later in life suggests that prevention of the 5 components of the metabolic syndrome should begin as early as the first decade of life.
The prevalence of childhood obesity in the US population nearly tripled between 1963 and 1991.14 The participants in the present study were born between 1950 and 1983. We have observed an increase in BMI values over the past 20 years among annual cohorts in the Fels study (unpublished data). Participants in the Fels study were enrolled at birth and were not selected in regard to factors associated with any clinical condition. Consequently, the relationships revealed by this analysis reflect the natural history of the development of obesity, centripetal fat accumulation, and the onset of the metabolic syndrome. These analyses imply that children at risk for the metabolic syndrome can be identified as early as the first decade of life. Because the subjects who enrolled in the Fels study were drawn from southwestern Ohio, most of the participants are non-Hispanic whites. Therefore, our findings may not apply to other races and ethnicities. However, in view of the prevalence of obesity in African-American and Hispanic children and adolescents that has been documented in national surveys,14 our findings likely do not apply only to non-Hispanic white children.
The results of our current analysis echo those of our earlier report of the predictive power of measurements of systolic blood pressure in childhood1 and demonstrate that central obesity and/or the metabolic syndrome can be predicted by measuring BMI and waist circumference in childhood as early as age 6 years. This predictive power would appear to be of clinical and public health importance. Such predictions indicate the need to intervene in childhood instead of later in life when deleterious clusterings of risk factors have developed and established lifestyles are difficult to alter. Our results show the remarkable predictive power of simple, easily performed anthropometric measurements in childhood. In light of the rapidly increasing prevalence of childhood obesity and of the public health challenges that will surely follow, our results demonstrate the importance of recording serial anthropometric measurements of BMI and waist circumference at each well-child visit. These serial measurements should permit health care workers to identify as early as possible those children headed for stormy metabolic futures.
The present findings are among the important results of our ongoing analyses of the serial data generated by the Fels Longitudinal Study. In our earlier analysis of serial blood pressure measurements in childhood, we showed that systolic blood pressure exceeding the 65th percentile for age and sex in childhood predicts an increased risk of the metabolic syndrome in adulthood.1 We urged health care workers to pay attention to even slightly elevated blood pressure in childhood in view of the public health significance of such childhood measurements. We recognize that no matter how important and simple a measurement may be, it will be a challenge for health care workers to include another physical measurement in the examination of apparently healthy children within a busy practice. However, in view of the public health implications of our findings, it is important to keep sounding the tocsin. Eventually, pediatric practice will have to be refashioned in response to the metabolic and cardiovascular dangers inherent in the twin epidemics of obesity and type 2 diabetes mellitus in childhood and adolescence.
Acknowledgments
Supported by in part by National Institutes of Health grants DK 071485, HL 072838, and HD 12252.
This manuscript was prepared for the Pediatric Metabolic Syndrome Working Group.
Glossary
- ATP
Adult Treatment Panel
- BMI
Body mass index
- CDC
Centers for Disease Control and Prevention
- EBMI
Elevated body mass index
- EWC
Elevated waist circumference
- HDL
High-density lipoprotein
- NCEP
National Cholesterol Education Program
- NHANES
National Health and Nutrition Examination Survey
- OR
Odds ratio
- ROC
Receiver operating characteristics
REFERENCES
- 1.Sun SS, Grave GD, Siervogel RM, Pickoff A, Arslanian S, Daniels S. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel on the Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 3.Kahn R. Follow-up report on the diagnosis of diabetes mellitus. The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 4.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents. Arch Pediatr Adolesc Med. 2003;137:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 5.Cruz ML, Goran MI. The metabolic syndrome in children and adolescents. Curr Diabetes Rep. 2004;4:53–62. doi: 10.1007/s11892-004-0012-x. [DOI] [PubMed] [Google Scholar]
- 6.Weiss R, Dziura J, Burgert T. Obesity and metabolic syndrome in children and adolescents. New Engl J Med. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 7.Roche AF. Growth, Maturation and Body Composition: The Fels Longitudinal Study 1929–1991. Cambridge, UK: Cambridge University Press; 1992. [Google Scholar]
- 8.Lohman T, Martorell R, Roche AF. Anthropometric Standardization Manual. Springfield, IL: Human Kinetics; 1988. [Google Scholar]
- 9.Roche AF, Chumlea WC, Thissen D. Assessing the Skeletal Maturity of the Hand-Wrist: Fels Method. Springfield, IL: Charles C. Thomas; 1988. [DOI] [PubMed] [Google Scholar]
- 10.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 11.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;283:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 12.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;246:1–190. [PubMed] [Google Scholar]
- 13.Fernandez J, Redden D, Pietrobelli A, Allison D. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 14.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents: the National Health and Nutrition Examination Surveys, 1963–1991. Arch Pediatr Adolesc Med. 1995;149:1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]