Abstract
Hospitalization among older adults receiving skilled home health services continues to be prevalent. Frontloading of skilled nursing visits, defined as providing 60% of the planned skilled nursing visits within the first two weeks of home health episode, is one way home health agencies have attempted to reduce the need for readmission among this chronically ill population. This was a retrospective observational study using data from five Medicare-owned, national assessment and claim databases from 2009. An independent randomized sample of 4,500 Medicare-reimbursed home health beneficiaries was included in the analyses. Propensity score analysis was used to reduce known confounding among covariates prior to the application of logistic analysis. Although whether skilled nursing visits were frontloaded or not was not a significant predictor of 30-day hospital readmission (p=0.977), additional research is needed to refine frontloading and determine the type of patients who are most likely to benefit from it.
Introduction
Hospitalization among older adults receiving skilled home health services continues to be prevalent. Nationally, 27% of Medicare-reimbursed home health recipients are hospitalized at some point while receiving home health services.1 Hospitalization costs in 2010 for fee-for-service Medicare beneficiaries rose to $116 billion from $113 billion in 2009 and $106 billion in 2005.2 It has been estimated that unplanned, and possibly preventable, hospitalizations costs $12 billion a year and that eliminating just 5.2% of preventable Medicare readmissions could save an estimated $5 billion annually.3
While in its infancy, a growing body of evidence indicates that hospitalization among geriatric skilled home health recipients is most likely to occur within the first two weeks of the home health episode.4-6 Specifically, the Home Health Quality Improvement Organization Support Center found, as reported by Vasquez, that among those hospitalized during the home health episode, 25% of patients are hospitalized within 7 days of admission to home health services6; 50.1% by 14 days5; and 58% by 21 days (cumulative).6 These findings indicate the need to target services immediately following a hospital discharge and in the very beginning of the home health episode in order to reduce preventable readmissions.7
Like many other health care organizations in the United States, home health agencies and advocacy groups throughout the country have focused their efforts on reducing the need for 30-day hospital readmissions among Medicare beneficiaries. Frontloading of skilled nursing visits is one way home health agencies have attempted to reduce the need for readmission among this chronically ill population. Frontloading has been defined as providing 60% of the planned skilled nursing visits within the first 2 weeks of the home health episode.8 Frontloading of skilled nursing visits is thought to allow clinicians to identify issues early-on and intervene before a readmission is needed. Results on the benefits of frontloading are particularly beneficial for those with heart failure decreasing readmission rates from 39.4% to 16%.8 Conversely, the impact of frontloading was not effective for patients with diabetes.8
Despite limited evidence, frontloading for all diagnoses has been encouraged as one of 12 best practices aimed at reducing readmission among skilled home health recipients by the 2007 Home Health Quality Campaign (HHQC) and frontloading was also endorsed by the West Virginia Medical Institute.4,9 The West Virginia Medical Institute is the Quality Improvement Organization, under contract with CMS, was charged with assisting health care providers in improving quality and safety and in developing innovative solutions that assure the quality and necessity of health care services.10 To gain a better understanding of the benefits of frontloading, the purpose of this study was to evaluate the impact frontloading skilled home health nursing visits has on the incidence of 30-day hospital readmission among older adults receiving Medicare-reimbursed skilled home health services over a one-year period.
Frontloading of skilled nursing visits was operationalized by considering the findings of Bowles and colleagues who reported that, on average, skilled home health patients received nine skilled nursing visits during the home health episode.11 Thus, five skilled nursing visits within the first 14 days of the home health episode was considered 60% of the total number of skilled nursing visits. We hypothesized that Medicare-reimbursed skilled home health recipients with frontloaded skilled nursing visits (5 or more skilled nursing visits in the first 14 days of the home health episode) would have a lower incidence of hospital readmission within 30-days of hospital discharge compared to those who received less than five skilled nursing visits within the first 14 days of the home health episode. It was hypothesized that client characteristics, including the hospitalization risk factors identified in the literature, home health agency tax identification status (for-profit vs. not-for-profit), and the intervention of frontloaded skilled home health nursing visits would impact 30-day readmissions to the hospital (Table 1). The covariates employed in this study were derived from a review of the literature as being associated with risk of readmission among skilled home health recipients.7
Table 1.
Data Sources
|
Variable Type
(QHOM Concept) |
Variable | Variable Definition | Variable Source |
|---|---|---|---|
| Independent (Intervention) |
Presence of Front-Loaded Skilled Nursing Visits |
5 or more skilled nursing visits in the first 14 days of the home health episode |
HH Agency Standard Analytic File (HHSAF) |
| Dependent (Outcome) |
30-day Hospital Readmission | The occurrence of a hospital readmission within 30-days of a hospital discharge for CMS-reimbursed patients receiving HH services |
Medicare Provider and Analysis Review File (MedPAR) |
| Covariates (Client) |
Female, White, Hispanic, severity of illness, living alone, guarded rehabilitation prognosis, pressure ulcer, stasis ulcer, dyspnea, urinary incontinence, lacking an informal caregiver, needing assistance with bathing, ambulation, eating or taking medications |
Hospitalization risk factors |
Outcome Assessment Information Set (OASIS) |
| Covariates (Client) |
Diagnosis of DM, Depression, ischemic heart disease, HIV/AIDS, renal failure, HF, COPD; cardiomypathy, dysrythmia, CAD, Alzheimer’s disease, personality/anxiety disorders, osteoporosis, MI; presence of 4 or more diagnoses |
Hospitalization risk factors |
HH Agency Standard Analytic File (HHSAF) |
| Covariate (System) |
Seen by a for-profit home health agency |
Hospitalization risk factor | Provider of Services File |
Theoretical Framework
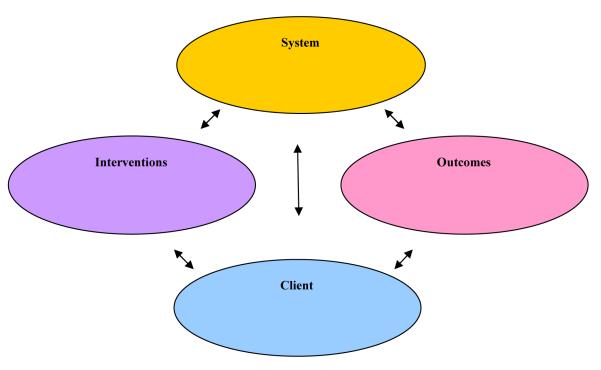
Mitchell and colleagues' Quality Health Outcomes Model (QHOM) guided this study (Figure 1).12 The QHOM is a theoretical framework that relates multiple factors affecting quality of care to desired outcomes and consists of four components: system, client, interventions, and outcomes. Given the heterogeneity of the Medicare-reimbursed skilled home health population, the model suggests that health interventions, specifically frontloaded skilled nursing following a hospitalization, influence and are affected by the client (hospitalization risk factors), to produce positive or negative outcomes (readmission within 30 days of hospital discharge). This study was grounded in the QHOM by conceptualizing and examining the relationships between system components and the impact these factors had on 30-day readmission.
Figure 1.
Quality Health Outcomes Model
Methods
Study Design
This was a retrospective observational study using data from five Medicare-owned, national assessment and claim databases from 2009. Propensity score analysis was used to reduce known confounding among covariates. This study was approved using the expedited review procedure by the University’s Institutional Review Board, Office of Regulatory Affairs.
Data Sets
The 2009 assessment and claims data sets were obtained from CMS, through the Research Data Assistance Center (ResDAC). Data originated from a five-percent sample of the Outcome Assessment Information Set (OASIS), the home health assessment required for CMS beneficiaries, then cross-referenced to the home health and hospital claims, eligibility and provider files. The data sets were comprised of the following: OASIS-B113; Home Health Standard Analytic File (HHSAF)14; Medicare Provider and Analysis Review File (MedPAR) (short stay/long stay/skilled nursing facility)15; Denominator/Eligibility File16; Provider of Services File (POS).17 The data sets contained the covariates, independent and dependent variables, related to skilled Medicare home health beneficiaries and home health agencies essential to address the study aims. Table 1 contains the specific variables supplied by each data set.
Sample
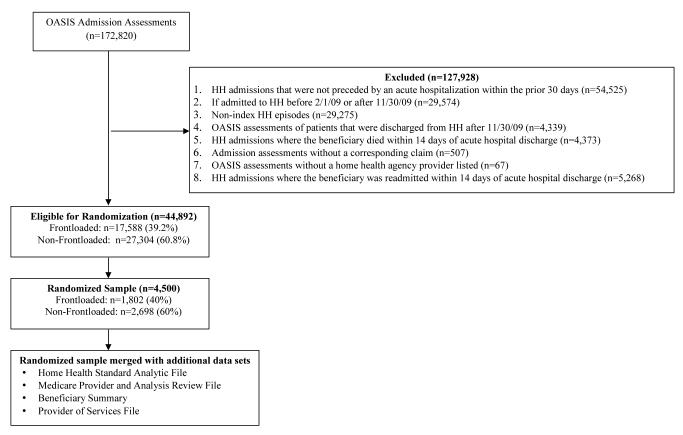
Beneficiaries were eligible for the study if they were admitted to home health within 30 days of a hospital discharge. After applying the first seven of eight exclusions, 50,160 beneficiaries remained. Of these beneficiaries, 15.4% (n=7,740) experienced a 30-day hospital readmission. However, beneficiaries who were readmitted to the hospital within the first 14 days of home health (n=5,268) were excluded from the analysis because frontloading was not possible. After removing those readmitted within the first 14 days, 44,892 eligible home health beneficiaries remained in the data set. Overall there were eight exclusion criteria applied to the data sets (Figure 2).The remaining home health beneficiaries were divided into two groups, those who received 5 or more skilled nursing visits within the first 14 days (frontloaded) and those who received less than 5 (not frontloaded).
Figure 2.
Consort Diagram: Sample of Medicare Beneficiaries Receiving Skilled Home Health
Managed-Medicare beneficiaries were excluded from the data set as home health claims data are not available for this population. The OASIS data set was the anchor data set to prepare the data files since having received home health during 2009 was required. Figure 2 depicts the preparation of the final analytic data file.
Power Analysis
Because the use of all eligible subjects in the analytic data file would lead to an overpowered study, a random sample of all eligible subjects was selected for this analysis. An adequately powered study is designed to detect both statistically and clinically meaningful differences in outcome between groups. The estimated sample size was based on a logistic regression model of rehospitalization on frontloading. Accordingly, a logistic regression of a binary response variable (Y=rehospitalization within 30 days of hospital discharge) on a binary independent variable (X=frontloading dichotomized) with a sample size of 4,468 subjects (of which 50% are assumed to be frontloaded, and 50% are assumed to not be frontloaded) achieves 80% power at a 0.01 significance level to detect a change in the probability of being hospitalized within 30 days of hospital discharge from the baseline value of 0.27 (27% hospitalized among subjects who were frontloaded) to 0.357 (~36% among subjects who were not frontloaded). This change corresponds to an odds ratio of 1.5. An adjustment was made assuming that a multiple regression of the independent variable of interest, frontloading, on the other independent variables in the logistic regression will obtain an R-Squared of 0.80 yielding a necessary sample size of 4,468 beneficiaries. Simple random selection of 4,500 eligible beneficiaries was accomplished using SAS™ version 9.3.
Variables
All variables employed in this study and their sources are listed in Table 1. The unweighted and weighted means, standard deviations, percentages and categories for all study variables are listed in Table 2. Statistics are shown for beneficiaries in both groups (frontloaded [FL] and not frontloaded [Not FL]).
Table 2.
Means and Standard Deviations of Study Variables Pre and Post-Matching
|
PRE-MATCHED
(UNWEIGHTED) |
AFTER MATCHING (WEIGHTED) | |||||
|---|---|---|---|---|---|---|
| Frontloaded (FL) n=1,802 (40%) Not Frontloaded (Not FL) n=2,698 (60%) |
FL | Not FL |
Total
(n=4,500) |
FL | Not FL |
Total
(n=4,500) |
| Variable | Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) |
| Age | 76.09 (11.21) | 76.22 (11.01) | 76.17 (11.09) | 76.09 (11.21) | 75.87 (11.11) | 75.96 (11.15) |
| Number of Diagnoses | 5.79 (1.68) | 5.62 (1.63) | 5.69 (1.65) | 5.79 (1.68) | 5.77 (1.65) | 5.78 (1.67) |
| Severity of Illness | 2.58 (0.67) | 2.49 (0.63) | 2.52 (0.65) | 2.58 (0.67) | 2.59 (0.67) | 2.59 (0.67) |
| Number of High Risk Diagnoses | 1.41 (1.15) | 1.19 (1.12) | 1.28 (1.14) | 1.41 (1.15) | 1.42 (1.23) | 1.42 (1.20) |
| Variable | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) |
| Confusion | ||||||
| Never | 1,059 (23.53) | 1,630 (36.22) | 2,689 (59.76) | 1,059 (23.53) | 1,616 (35.92) | 2,675 (59.45) |
| In new or complex situations only | 594 (13.20) | 812 (18.04) | 1,406 (31.24) | 594 (13.20) | 857 (19.05) | 1,451 (32.25) |
| On awakening or at night only | 22 (0.49) | 27 (0.60) | 49 (1.09) | 22 (0.49) | 25 (0.56) | 47 (1.05) |
| During the day and evening, not constantly | 108 (2.40) | 204 (4.53) | 312 (6.93) | 108 (0.24) | 181 (4.02) | 289 (6.42) |
| Constantly | 19 (0.42) | 25 (0.56) | 44 (.98) | 19 (0.42) | 19 (0.41) | 38 (0.83) |
| Cognitive Function | ||||||
| Alert/oriented, able to focus and shift attention,
comprehends and recalls task directions independently |
1,227 (27.27) | 1,836 (40.80) | 3,063 (68.07) | 1,227 (27.27) | 1,841 (40.91) | 3,068 (68.18) |
| Requires prompting (cueing, repetition, reminders) only
under stressful or unfamiliar conditions |
413 (9.18) | 610 (13.56) | 1,023 (22.73) | 413 (9.18) | 619 (13.76) | 1,032 (22.94) |
| Requires assistance and some direction in specific
situations or consistently requires low stimulus environment due to distractibility |
132 (2.93) | 192 (4.27) | 324 (7.20) | 132 (2.93) | 192 (4.26) | 324 (7.19) |
| Requires considerable assistance in routine situations. Is
not alert and oriented or is unable to shift attention and recall directions more than half the time |
27 (0.60) | 51 (1.13) | 78 (1.73) | 27 (0.60) | 38 (0.84) | 65 (1.44) |
| Totally dependent due to disturbances such as constant
disorientation, coma, persistent vegetative state, or delirium |
3 (0.07) | 9 (0.20) | 12 (0.27) | 3 (0.07) | 8 (0.19) | 11 (0.25) |
| Bathing Ability | ||||||
| Able to bathe self in shower or tub independently | 102 (2.27) | 141 (3.13) | 543 (5.40) | 102 (2.27) | 132 (2.92) | 234 (5.19) |
| With the use of devices, is able to bathe self in shower or
tub independently |
227 (5.04) | 354 (7.87) | 581 (12.81) | 227 (5.04) | 353 (7.84) | 580 (12.88) |
| Able to bathe in shower or tub with the assistance of
another person:(a) for intermittent supervision or encouragement or reminders, OR (b) to get in and out of the shower/tub, OR (c) for washing difficult to reach areas |
479 (10.64) | 8.05 (17.89) | 1,284 (28.53) | 479 (10.64) | 773 (17.18) | 1,252 (27.83) |
| Participates in bathing self in shower or tub, but required
presence of another person throughout in the bath for assistance or supervision |
512 (11.38) | 741 (16.47) | 1,253 (27.84) | 512 (11.38) | 736 (16.35) | 1,248 (27.73) |
| Unable to use the shower or tub and is bathed in bed or
bedside chair |
422 (9.38) | 591 (13.13) | 1,013 (22.51) | 422 (9.38) | 638 (14.19) | 1,060 (23.57) |
| Unable to effectively participate in bathing and is totally
bathed by another person |
60 (1.33) | 66 (1.47) | 126 (2.80) | 60 (1.33) | 66 (1.47) | 126 (2.80) |
| Ambulation Ability | ||||||
| Able to independently walk on even and uneven surfaces
and climb stairs with or without railings (needs no human assistance or assistive device) |
187 (4.16) | 201 (4.47) | 388 (8.62) | 187 (4.16) | 265 (5.89) | 452 (10.05) |
| Requires use of a device to walk alone or Requires
human supervision or assistance to negotiate stairs or steps or uneven surfaces |
1,013 (22.51) | 1,503 (33.40) | 2,516 (55.91) | 1,013 (22.51) | 1,524 (33.88) | 2,537 (56.39) |
| Able to walk only with the supervision or Assistance of
another person at all times |
499 (11.09) | 835 (18.56) | 1,334 (29.64) | 499 (11.09) | 794 (17.64) | 1,293 (28.72) |
| Chairfast, unable to ambulate but is able to Wheel self
independently |
47 (1.04) | 76 (1.69) | 123 (2.73) | 47 (1.04) | 55 (1.23) | 102 (2.27) |
| Chairfast, unable to ambulate and is unable to wheel self | 45 (1.00) | 71 (1.58) | 116 (2.58) | 45 (1.00) | 53 (1.17) | 98 (2.17) |
| Bedfast, unable to ambulate or be up in a chair | 11 (0.24) | 12 (0.27) | 23 (0.51) | 11 (0.24) | 7 (0.16) | 18 (0.40) |
| Presence of Dyspnea | ||||||
| Never, patient is not short of breath | 470 (10.44) | 863 (19.18) | 1,333 (29.62) | 470 (10.44) | 695 (15.43) | 1,165 (25.88) |
| When walking more than 20 feet, climbing stairs | 485 (10.78) | 823 (18.29) | 1,308 (29.07) | 485 (10.78) | 840 (18.68) | 1,325 (29.45) |
| With moderate exertion (e.g., while dressing, using
commode or bedpan, walking distances less than 20 feet) |
541 (12.02) | 667 (14.82) | 1,208 (26.84) | 541 (12.02) | 728 (16.18) | 1,269 (28.20) |
| With minimal exertion (e.g., while eating, talking, ADLs)
or with agitation |
261 (5.80) | 281 (6.24) | 542 (12.04) | 261 (5.80) | 332 (7.39) | 593 (13.19) |
| At rest (during day or night) | 45 (1.00) | 64 (1.42) | 109 (2.42) | 45 (1.00) | 103 (2.28) | 148 (3.28) |
| Presence of Anxiety | ||||||
| None of the time | 1,017 (22.60) | 1,643 (36.51) | 2,660 (59.11) | 1,017 (22.60) | 1,568 (34.85) | 2,585 (57.45) |
| Less often than daily | 448 (9.96) | 605 (13.44) | 1,053 (23.40) | 448 (9.96) | 623 (13.84) | 1,071 (23.80) |
| Daily, but not constantly | 316 (7.02) | 411 (9.13) | 727 (16.16) | 316 (7.02) | 462 (10.26) | 778 (17.29) |
| All of the time | 21 (0.47) | 39 (0.87) | 60 (1.33) | 21 (0.47) | 45 (1.00) | 66 (1.46) |
| All of the time | 21 (0.47) | 39 (0.87) | 60 (1.33) | 21 (0.47) | 45 (1.00) | 66 (1.46) |
| Transfer Ability | ||||||
| Able to independently transfer | 370 (8.22) | 446 (9.91) | 816 (18.13) | 370 (8.22) | 505 (11.23) | 875 (19.45) |
| Transfers with minimal human assistance or with use of
an assistive device |
1,152 (25.60) | 1,834 (40.76) | 2,986 (66.36) | 1,152 (25.60) | 1,835 (40.77) | 2,987 (66.37) |
| Unable to transfer self but is able to bear weight and
pivot during the transfer |
218 (4.84) | 333 (7.40) | 551 (12.21) | 218 (4.84) | 289 (6.43) | 507 (11.27) |
| Unable to transfer self and is unable to bear weight or
pivot when transferred by another person |
38 (0.84) | 59 (1.31) | 97 (2.16) | 38 (0.84) | 50 (1.12) | 88 (1.97) |
| Bedfast, unable to transfer but is able to turn and position
self in bed |
11 (0.24) | 10 (0.22) | 21 (0.47) | 11 (0.24) | 6 (0.14) | 17 (0.38) |
| Bedfast, unable to transfer and is unable to turn and
position self |
13 (0.29) | 16 (0.36) | 29 (0.64) | 13 (0.29) | 12 (0.26) | 25 (0.55) |
| Feeding Ability | ||||||
| Able to independently feed self | 1,068 (23.73) | 1,700 (37.78) | 2,768 (61.51) | 1,068 (23.73) | 1,606 (35.70) | 2,674 (59.43) |
| Able to feed self independently but requires: (a). meal
set-up; OR (b) intermittent assistance or supervision from another person; OR (c) a liquid, pureed or ground meat diet |
671 (14.91) | 920 (20.44) | 1,591 (35.36) | 671 (14.91) | 1,012 (22.49) | 1,683 (37.40) |
| Unable to feed self and must be assisted or supervised
throughout the meal/snack |
45 (1.00) | 59 (1.31) | 104 (2.31) | 45 (1.00) | 57 (1.27) | 102 (2.27) |
| Able to take in nutrients orally and receives supplemental
nutrients through a nasogastric tube or gastrostomy |
7 (0.16) | 3 (0.07) | 10 (0.22) | 7 (0.16) | 5 (0.11) | 12 (0.27) |
| Unable to take in nutrients orally and is fed nutrients
through a nasogastric tube or gastrostomy |
8 (0.18) | 14 (0.31) | 11 (0.49) | 8 (0.18) | 16 (0.35) | 24 (0.53) |
| Unable to take in nutrients orally or by tube feeding | 2 (0.04) | 3 (0.07) | 5 (0.11) | 3 (0.07) | 2 (0.04) | 5 (0.10) |
| Living Alone | 487 (10.82) | 687 (15.27) | 1,174 (26.09) | 487 (10.82) | 743 (16.51) | 1,230 (27.33) |
| Urinary Incontinence | 740 (16.44) | 1,068 (23.73) | 1,808 (40.18) | 740 (16.44) | 1,091 (24.24) | 1,831 (40.69) |
| Depressed Mood | 352 (4.82) | 461 (10.24) | 813 (18.07) | 352 (7.82) | 502 (11.16) | 854 (18.98) |
| Memory Deficits | 201 (4.47) | 337 (7.49) | 538 (11.96) | 201 (4.47) | 296 (6.58) | 497 (11.05) |
| Female | 1,084 (24.09) | 1,729 (38.42) | 2,813 (62.51) | 1,084 (24.09) | 1,624 (36.08) | 2,708 (60.17) |
| Hispanic | 102 (2.27) | 116 (2.58) | 218 (4.84) | 102 (2.27) | 142 (3.16) | 244 (5.43) |
| White | 1,488 (33.07) | 2,207 (49.04) | 3,695 (82.11) | 1,488 (33.07) | 2,230 (49.57) | 3,718 (82.64) |
| Serviced by a For-Profit Home Health Agency | 920 (20.44) | 1,290 (28.67) | 2,210 (49.11) | 920 (20.44) | 1,330 (29.57) | 2,250 (50.01) |
| Presence of a Primary Caregiver | 1,577 (35.04) | 2,343 (52.07) | 3,920 (87.11) | 1,577 (35.04) | 2,340 (52.01) | 3,917 (87.05) |
| Guarded Rehabilitation Prognosis | 435 (9.67) | 562 (12.49) | 997 (22.16) | 435 (9.67) | 610 (13.55) | 1,045 (23.22) |
| Requires Assistance with ADLs | ||||||
| Yes | 1,032 (22.93) | 1,559 (34.64) | 2,591 (57.58) | 1,032 (22.93) | 1,539 (34.21) | 2,571 (57.14) |
| No | 505 (11.02) | 727 (16.16) | 1,232 (27.38) | 505 (11.22) | 749 (16.64) | 1,254 (27.86) |
| Unknown | 265 (5.89) | 412 (9.16) | 677 (15.04) | 265 (5.89) | 410 (9.11) | 675 (14.99) |
| Requires Assistance with IADLs | ||||||
| Yes | 1,434 (31.87) | 21.55 (47.89) | 3,589 (79.76) | 1,434 (31.87) | 2,136 (47.47) | 3,570 (79.34) |
| No | 103 (2.29) | 1,434 (31.87) | 2,155 (47.89) | 103 (2.29) | 152 (3.38) | 255 (5.67) |
| Unknown | 265 (5.89) | 412 (9.16) | 677 (15.04) | 265 (5.89) | 410 (9.11) | 675 (14.99) |
| Presence of a Pressure Ulcer | ||||||
| Yes | 110 (2.44) | 98 (2.18) | 208 (4.62) | 110 (2.44) | 154 (3.42) | 264 (5.87) |
| No | 1,446 (32.13) | 2,172 (48.27) | 3,618 (80.40) | 1,446 (32.13) | 2,154 (47.87) | 3,600 (80.00) |
| Unknown | 246 (5.47) | 428 (9.51) | 674 (14.98) | 246 (5.47) | 390 (8.67) | 636 (14.13) |
| Presence of a Stasis Ulcer | ||||||
| Yes | 16 (0.36) | 11 (0.24) | 27 (0.60) | 16 (0.36) | 5 (0.10) | 21 (0.46) |
| No | 1,540 (34.22) | 2,259 (50.20) | 3,799 (84.42) | 1,540 (34.22) | 2,303 (51.19) | 3,843 (85.41) |
| Unknown | 246 (5.47) | 428 (9.51) | 674 (14.98) | 246 (5.47) | 390 (8.67) | 636 (14.13) |
| Requires Assistance with Oral Medications | ||||||
| Yes | 759 (16.87) | 1,013 (22.51) | 1,772 (39.38) | 759 (16.87) | 1,097 (24.38) | 1,856 (41.25) |
| No | 687 (15.27) | 1,172 (26.04) | 1,859 (41.31) | 687 (15.27) | 1,050 (23.34) | 1,737 (38.60) |
| Unknown | 356 (7.91) | 513 (11.40) | 869 (19.31) | 356 (7.91) | 551 (12.23) | 907 (20.15) |
Dependent Variable
The MedPAR file provided the dependent variable, the occurrence of 30-day hospital readmission measured as a hospitalization (yes/no) within 30 days of the initial hospital discharge.
Independent Variable
Frontloading of skilled nursing visits was operationalized as having five skilled nursing visits within the first 14 days of the home health episode as this was considered 60% of the total number of skilled nursing visits. Frontloading of skilled nursing visits was the dichotomous, independent variable and was defined as receiving 5 or more skilled nursing visits within the first 14 days of the home health episode.
Covariates (Matching Variables)
The OASIS, HHSAF or Provider of Services Summary contained the covariates included when deriving the propensity score. Several of the variables derived from the OASIS have a category of "unknown". This is not missing data, but is an option on the OASIS assessment where the clinician was unable to accurately determine the appropriate answer at the time the tool was completed and is therefore considered an acceptable response (Table 2).13
Statistical Analysis
Propensity Score Analysis
In this type of study, random assignment to study group is not possible. Therefore, propensity score analysis18 and matching methods19 were conducted to control for differences between beneficiaries in the frontloaded and not frontloaded groups.20
Propensity score analysis is the conditional probability of receiving treatment, given the distribution of observed covariates.19 It is a rigorous analytic method that controls for observed confounders that might influence group assignment18 by reducing the confounding covariates into a single variable, the propensity score. The propensity scores were created using the covariates found in Table 2. Beneficiaries in each group were matched on these scores using the full-matching technique.21 During propensity score analysis, frontloaded (treated) beneficiaries received a weight of 1 and non-frontloaded (control) beneficiaries received a weight proportional to the number of treated individuals in the matched set divided by the number of control beneficiaries in the set.21, 22 These weights were then used in the logistic regression model in the statistical analyses.
Matching methods balance the distribution of observed covariates in the comparison groups (frontloaded vs. not frontloaded) imitating what would have occurred in a randomized control trial.19 This controls for the observed confounders between the groups. Therefore, within the sample of frontloaded and non-frontloaded beneficiaries with similar propensity scores, both groups will have similar distributions of the observed covariates included in the propensity score (Table 1).21
Data Analysis
Following the propensity score analysis, propensity score weighted bivariate logistic regression models were used to regress 30-day hospital readmission on each individual variable using the SAS Proc Logistic procedure. Other than the primary predictor of interest, dichotomized frontloading, only covariates demonstrating significance at the p≤0.05 level in the bivariate analyses were included in the final multivariate analyses.23 Table 2 provides a comprehensive list of the independent variables considered in the simple logistic regression models. Correlation coefficients were generated to assess multicollinearity, and variables demonstrating collinearity were chosen for inclusion on the basis of clinical importance. Using Bonferroni's correction, statistical significance in the final multivariate analyses was set at p≤0.01. Odds ratios are provided for intervention and covariates in addition to their 99% confidence intervals.
Results
An independent randomized sample of 4,500 Medicare-reimbursed home health beneficiaries was included in the analyses. Beneficiaries were predominately female (60.17%), white (82.64%), and not frontloaded (60%) (Table 2). Overall, 207 (4.6%) readmissions occurred between 15 and 30 days of home health admission with more occurring in the not frontloaded group (n= 124; 2.75%) compared to the frontloaded group (n=83; 1.84%). However, this was not statistically significant (p=0.972) (Table 3). The final regression model included variables significant at the 0.05 level in the bivariate model as predictors and their proportional weights as generated by the propensity score analysis.
Table 3.
Participant Hospitalization between days 15-30 (n=4,500)
| N | %of Sample |
|
|---|---|---|
| Total Hospitalizations | 207 | 4.59% |
| Hospitalizations among the frontloaded group | 83 | 1.84% |
| Hospitalizations among the non-frontloaded group | 124 | 2.75% |
Bivariate logistic regression modeling of frontloading on 30-day readmission showed 12 variables to be significant at the 0.05 level (Table 4). However, five variables were removed due to collinearity. Frontloading of skilled nursing visits was not significant (p=0.972) but was included in the multivariate model as it was the predictor of interest. Multivariate modeling (Table 5) indicated that depressed patients compared to those not depressed, increased the odds of a 30-day readmission by 94% (odds ratio [OR]=1.94; 99% confidence interval [CI]=1.27-2.98; p<.001). The odds of a 30-day readmission were increased by 51% among home health beneficiaries with a guarded rehabilitation prognosis (OR=1.51; 99% CI=1.01-2.28; p=0.009). In addition, with each unit increase in the number of high-risk diagnoses, the odds of a 30-day readmission increased by 17% (OR=1.17; 99% CI=1.01-1.37; p=0.008). Finally, with every unit increase in bathing dependence the odds of a 30-day readmission decreased by 17% (OR=1.17; 99% CI=1.01-1.37; p=0.008). Similar to the bivariate model, frontloading was not a significant predictor of 30-day hospital readmission (p=0.977).
Table 4.
Bivariate Logistic Regression Analysis of Frontloading on Hospitalization
| Parameter | Parameter Estimate | SE | P value | Odds Ratio | 95% Hazard Ratio CI | |
|---|---|---|---|---|---|---|
| Frontloaded | 0.01 | 0.145 | 0.972 | 1.01 | 0.76 | 1.34 |
| Age | −0.01 | 0.006 | 0.076 | 0.989 | 0.97 | 1.00 |
| Number of Diagnoses | 0.07 | 0.043 | 0.099 | 1.07 | 0.99 | 1.17 |
| Severity of Illness | −0.05 | 0.107 | 0.673 | 0.96 | 0.77 | 1.18 |
| High Risk Diagnosis Frequency | 0.26 | 0.055 | <.001* | 1.30 | 1.17 | 1.45 |
| Confusion | 0.16 | 0.074 | 0.031! | 1.17 | 1.02 | 1.35 |
| Cognitive Function | 0.11 | 0.095 | 0.261 | 1.11 | 0.92 | 1.34 |
| Difficulty Bathing | −0.14 | 0.058 | 0.014* | 0.87 | 0.77 | 0.97 |
| Difficulty Ambulating | 0.02 | 0.088 | 0.796 | 1.02 | 0.86 | 1.22 |
| Dyspnea | 0.27 | 0.063 | <.001* | 1.31 | 1.16 | 1.48 |
| Anxiety | 0.27 | 0.081 | 0.001* | 1.32 | 1.12 | 1.54 |
| Difficulty Transferring | 0.02 | 0.099 | 0.838 | 1.02 | 0.84 | 1.24 |
| Difficulty Feeding | 0.02 | 0.113 | 0.867 | 1.02 | 0.82 | 1.27 |
| Living Alone | 0.19 | 0.154 | 0.211 | 1.21 | 0.90 | 1.64 |
| Urinary Incontinence | 0.12 | 0.144 | 0.417 | 1.12 | 0.85 | 1.49 |
| Depressed Mood | 0.84 | 0.152 | <.001* | 2.3 | 1.72 | 3.11 |
| Memory Deficit | 0.04 | 0.224 | 0.845 | 1.05 | 0.67 | 1.62 |
| Female | −0.30 | 0.143 | 0.034* | 0.74 | 0.56 | 0.98 |
| Hispanic | −0.16 | 0.330 | 0.726 | 0.89 | 0.47 | 1.70 |
| White | 0.22 | 0.201 | 0.281 | 1.24 | 0.84 | 1.84 |
| For-Profit Agency | −0.10 | 0.143 | 0.501 | 0.91 | 0.69 | 1.20 |
| Presence of a Primary Caregiver | −0.05 | 0.208 | 0.797 | 0.95 | 0.63 | 1.43 |
| Guarded Rehabilitation Prognosis | 0.62 | 0.150 | <.001* | 1.86 | 1.39 | 2.50 |
| Requiring Assistance with ADLs (0 vs. 2) | 0.27 | 0.105 | 0.010! | 1.36 | 0.89 | 2.08 |
| Requiring Assistance with ADLs (1 vs. 2) | −0.23 | 0.010 | 0.020! | 0.823 | 0.55 | 1.24 |
| Requiring Assistance with IADLs (0 vs. 2) | 0.47 | 0.163 | 0.004! | 1.95 | 1.11 | 3.44 |
| Requiring Assistance with IADLs (1 vs. 2) | −0.27 | 0.111 | 0.015! | 0.93 | 0.63 | 1.38 |
| Presence of a Pressure Ulcer (0 vs. 2) | 0.02 | 0.127 | 0.891 | 1.15 | 0.76 | 1.76 |
| Presence of a Pressure Ulcer (1 vs. 2) | 0.11 | 0.200 | 0.591 | 1.26 | 0.64 | 2.48 |
| Presence of a Stasis Ulcer (0 vs. 2) | −0.03 | 0.323 | 0.918 | 1.16 | 0.76 | 1.77 |
| Presence of a Stasis Ulcer (1 vs. 2) | 0.21 | 0.628 | 0.734 | 1.48 | 0.23 | 9.67 |
| Requiring Assistance with Oral Medications (0 vs. 2) | −0.20 | 0.103 | 0.0512 | 0.70 | 0.48 | 1.02 |
| Requiring Assistance with Oral Medications (1 vs. 2) | 0.04 | 0.096 | 0.654 | 0.89 | 0.62 | 1.27 |
significant at the 0.05 level, included in the final model
not included in final model due to multiplicity
SE: Standard Error
CI: Confidence Interval
Table 5.
Multivariate Logistic Regression Analysis of Frontloading on Hospitalization
| Parameter | Parameter Estimate |
SE | P value |
Odds Ratio | 99% Hazard Ratio CI |
|
|---|---|---|---|---|---|---|
| Frontloaded | 0.01 | 0.147 | 0.977 | 1.01 | 0.68 | 1.47 |
| High Risk Diagnosis Frequency | 0.16 | 0.060 | 0.008* | 1.17 | 1.01 | 1.37 |
| Difficulty Bathing | −0.16 | 0.060 | 0.008* | 0.85 | 0.73 | 0.99 |
| Dyspnea | 0.14 | 0.070 | 0.052 | 1.15 | 0.96 | 1.37 |
| Anxiety | 0.08 | 0.090 | 0.380 | 1.08 | 0.86 | 1.37 |
| Depressed Mood | 0.66 | 0.166 | <.001* | 1.94 | 1.27 | 2.98 |
| Female | −0.33 | 0.146 | 0.024 | 0.72 | 0.50 | 1.05 |
| Guarded Rehab Prognosis | 0.41 | 0.159 | 0.009* | 1.51 | 1.01 | 2.28 |
significant at the 0.01 level
SE: Standard Error
CI: Confidence Interval
Discussion
While more 30-day readmissions occurred among the group not frontloaded, the hypothesis that frontloading skilled home health nursing visits would impact 30-day readmissions was not supported by the results of this study. Prior to excluding beneficiaries who were readmitted within the first 14 days of home health, it was found that 15.4% (n=7,740) of Medicare-reimbursed home health beneficiaries experienced a 30-day hospital readmission. Prior research has shown that among the home health beneficiaries readmitted, approximately 50% of them are readmitted within the first 14 days of admission to home health.4-6 Similarly, our findings indicate that of those readmitted, 68% (n=5,268) were readmitted within the first 14 days of home health but were excluded from this analysis as frontloading (five or more skilled nursing visits within 14 days), defined a priori, was not possible. This left only 32% (n=2,472) of the 30-days readmissions, those readmitted between 15 to 30 days, eligible for analysis.
These findings suggest that it may be critically important to provide intense and targeted home health services to Medicare-reimbursed beneficiaries within the first 14 days of skilled home health. As this study and prior research has shown, stretching out the services over the first 30 days of skilled home health is often too late and readmission has already occurred. However, intense and targeted interventions within the first 14 days of skilled home health remain a gap in knowledge and therefore must be designed and tested to determine their impact on reducing 30-day readmission. Equally important, is the need to admit Medicare beneficiaries at high risk for readmission, to home health soon after hospital discharge. At present, Medicare's Conditions of Participation mandate that beneficiaries are evaluated for skilled home health services within 48 hours of referral, within 48 hours of the patient's return home, or on the physician-ordered start of care date.24 Future research must evaluate home health agency compliance with this Condition of Participation in evaluating patients with 48 hours of hospital discharge and its relationship to readmission.
Prior research suggests that frontloading reduced the need for readmission among skilled home health patients.8, 25 However, samples for both studies were not randomly selected, lacked methodological rigor and considered frontloading of skilled nursing visits only. Frontloading remains one of 12 best practices endorsed by the West Virginia Medical Institute aimed at reducing readmission among skilled home health recipients.4, 9 However, additional research is essential to refine the practice of frontloading, perhaps to place greater emphasis on the first 7 days of home health admission as 14 days is clearly too late to meet the needs of this unique and vulnerable population. The refinement of frontloading could also include additional home health disciplines such as physical and occupational therapy. Admission to home health within 24 hours of hospital discharge, especially among those at high risk for readmission, might also be an important component of refining how frontloading is operationalized. As a part of the refinement of frontloading, we must determine the types of patients who are most likely to benefit from it. Finally, in order to build upon our knowledge we must closely examine the Medicare beneficiaries who are readmitted within the first 14 days of home health. It will be essential to determine this group's unique characteristics and to identify the unmet needs that may underlie their 30-day readmission.
The limitations of this study relate mostly to the design as it was a secondary data analysis. The analysis included only one year of data previously collected in 2009. Also, only traditional, fee-for-service Medicare beneficiaries were included because managed-Medicare beneficiary claims are not available. However, despite the limitations, national Medicare-owned data sets represent the largest and most robust source of information available to address the study’s hypothesis.
Conclusion
Reducing 30-day readmission among Medicare-reimbursed skilled home health beneficiaries remains a national priority and is still an elusive goal. While frontloading was not found to be significantly associated with a reduction in 30-day readmission among Medicare-reimbursed home health beneficiaries in this study, additional research is needed to refine frontloading, determine the type of patients who are most likely to benefit from it and further evaluate these findings. In moving the science forward, it will be critical to examine the Medicare beneficiaries who are readmitted within the first 14 days of home health to determine this group's unique characteristics and to identify their unmet needs that may underlie their 30-day readmission.
Acknowledgements
The authors would like to acknowledge and thank The University of Maryland Online Dissemination and Implementation Institute funded by the University of Maryland and the John A. Hartford Foundation.
Funding:
This project was supported by the National Institute for Nursing Research, Individualized Care for At-Risk Older Adults (T32-NR009356) and the Sigma Theta Tau International/National Gerontological Nursing Association Research Grant
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Medicare and Medicaid Services Home health compare. 2012 Available at: www.medicare.gov/homehealthcompare. Cited October 12, 2013.
- 2.Medicare Payment Advisory Commission Report to the congress: Medicare payment policy. 2012 Available at: www.medpac.gov/documents/Mar12_EntireReport.pdf. Cited September 27, 2013.
- 3.Medicare Payment Advisory Commission (MedPAC) Report to the congress: Promoting greater efficiency in Medicare. 2007 Available at: www.medpac.gov/documents/jun07_entirereport.pdf. Cited September 27, 2013.
- 4.Home Health Quality Campaign Home Health Quality Improvement National Campaign. 2010 Available at: www.homehealthquality.org. Cited August 12, 2013.
- 5.Rosati RJ, Huang L. Development and testing of an analytic model to identify home healthcare patients at risk for a hospitalization within the first 60 days of care. Home Health Care Services Quarterly. 2007;26(4):21–36. doi: 10.1300/J027v26n04_03. (2007) [DOI] [PubMed] [Google Scholar]
- 6.Vasquez MS. Preventing rehospitalization through effective home health nursing care. Home Healthcare Nurse. 2008;26(2):75–81. doi: 10.1097/01.NHH.0000311023.03399.ed. [DOI] [PubMed] [Google Scholar]
- 7.O'Connor M. Hospitalization among Medicare-reimbursed skilled home health recipients. Home Health Care Management and Practice. 2012;24(1):25–35. doi: 10.1177/1084822311419498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rogers J, Perlic M, Madigan EA. The effect of frontloading visits on patient outcomes. Home Healthcare Nurse. 2007;25(2):103–109. doi: 10.1097/00004045-200702000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Esslinger E, Kevech M, Anderson D, et al. Home health quality improvement national campaign: The journal and potential impact on clinical practice. Home Healthcare Nurse. 2008;26(7):398–40. doi: 10.1097/01.NHH.0000326317.94218.5a. [DOI] [PubMed] [Google Scholar]
- 10.West Virginia Medical Institute About us. 2013 Available at: www.wvmi.org. Cited August 12, 2013.
- 11.Bowles KH, Holland DE, Horowtiz DA. A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management. Journal of Telemedicine and Telecare. 2009;15(7):344–350. doi: 10.1258/jtt.2009.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. Image: Journal of Nursing Scholarship. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services OASIS background. 2010a Available at www.cms.gov/OASIS/02_Background.asp#TopOfPage. Cited July 27, 2013.
- 14.Centers for Medicare and Medicaid Services Home Health PPS. 2010b Available at: www.cms.gov/HomeHealthPPS/01_overview.asp. Cited July 27, 2013.
- 15.Centers for Medicare and Medicaid Services MedPAR limited data set. 2010c Available at: xwww.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/MEDPARLDSHospitalNational.html. Cited August 20, 2013.
- 16.Centers for Medicare and Medicaid Services Denominator file. 2010d Available at http://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/IdentifiableDataFiles/DenominatorFile.html. Cited August 8, 2013.
- 17.Centers for Medicare and Medicaid Services Provider of Services file. 2010e Available at: www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/NonIdentifiableDataFiles/ProviderofServicesFile.html. Cited August 20, 2013.
- 18.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 19.Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical Science. 2010;25(1):1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubin DB. Using propensity scores to help design observational studies: Application to the tobacco litigation. Health Services & Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- 21.Stuart EA, Green KM. Using full matching to estimate causal effects in nonexperiemental studies: Examining the relationship between adolescent marijuana use and adult outcomes. Developmental Psychology. 2008;44(2):395–406. doi: 10.1037/0012-1649.44.2.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychological Methods. 2010;15(3):234–249. doi: 10.1037/a0019623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleinbaum DG, Kupper LL, Nizam A, et al. Duxbury Press; California: 2008. Applied regression analysis and other multivariate methods. [Google Scholar]
- 24.Centers for Medicare and Medicaid Services Appendix B of the state operations manual. 2013 Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_b_hha.pdf. Cited October 11, 2013.
- 25.Markley J, Sabharwal K, Wang Z, et al. A community-wide quality improvement project on patient care transitions reduces 30-day hospital readmissions from home health agencies. Home Healthcare Nurse. 2012;30(3):E1–E11. doi: 10.1097/NHH.0b013e318246d540. [DOI] [PubMed] [Google Scholar]