Abstract
Objective
This article considers how the social psychology of intergroup processes helps to explain the presence and persistence of health disparities between members of socially advantaged and disadvantaged groups.
Method
Social psychological theory and research on intergroup relations, including prejudice, discrimination, stereotyping, stigma, prejudice concerns, social identity threat, and the dynamics of intergroup interactions, is reviewed and applied to understand group disparities in health and health care. Potential directions for future research are considered.
Results
Key features of group relations and dynamics, including social categorization, social hierarchy, and the structural positions of groups along dimensions of perceived warmth and competence, influence how members of high status groups perceive, feel about, and behave toward members of low status groups, how members of low status groups construe and cope with their situation, and how members of high and low status groups interact with each other. These intergroup processes, in turn, contribute to health disparities by leading to differential exposure to and experiences of chronic and acute stress, different health behaviors, and different quality of health care experienced by members of advantaged and disadvantaged groups. Within each of these pathways, social psychological theory and research identifies mediating mechanisms, moderating factors, and individual differences that can affect health.
Conclusions
A social psychological perspective illuminates the intergroup, interpersonal, and intrapersonal processes by which structural circumstances which differ between groups for historical, political, and economic reasons can lead to group differences in health.
Keywords: discrimination and health, health disparities, stigma and health, health care disparities, intergroup relations
Health disparities between members of socially advantaged (or high status) groups and socially disadvantaged (or low status) groups are pervasive, persistent, and prevalent across cultures (see Penner, Albrecht, Orom, Coleman, & Underwood, 2010; Smedley, Stith, & Nelson, 2003 for reviews).1 In this article we consider how social psychological theory and research on intergroup processes and intergroup relations can help to understand these group health disparities and contribute to ameliorating them. After briefly summarizing disparities in health and traditional explanations for them, we offer a brief overview of key features of intergroup structure and dynamics that contribute directly and indirectly to the development and maintenance of group health disparities. We then elaborate on how intergroup processes that emerge from these dynamics work in concert to produce different levels of health among members of advantaged and disadvantaged groups through the mechanisms of stress, behaviors, and health care interactions. We conclude by identifying potential directions for social psychological and health research that can further illuminate the causes of health disparities and guide the development of interventions to effectively reduce them.
Group Health Disparities
People who belong to socially disadvantaged groups, whether defined by social identities such as race, ethnicity, citizen-immigrant status, socioeconomic status, sexual orientation, or weight, for example, have poorer health on average than people who belong to more advantaged social groups (Matthews & Gallo, 2011; Penner, Albrecht et al., 2010). Even at higher levels of socioeconomic status (SES), Black adults report higher levels of health problems than Whites and have a significantly shorter life expectancy (Smedley et al., 2003). Current data from the Centers for Diseases Control and Prevention (see www.cdc.gov) reveal that (a) Blacks have significantly higher rates of colorectal and lung cancer than do Whites; (b) the incidence of prostate cancer is approximately 50% higher among Black men than White men, and their mortality rate is twice as high; (c) the mortality rate for strokes is over 50% higher for Blacks than for Whites; and (d) the rate of stomach cancer among Latinos compared with Whites is 63% higher for men and 150% higher for women. These health disparities are not limited to the U.S., but are a pervasive problem internationally: Health disparities are evident in at least 126 countries, representing 94.4% of the world’s population (see Penner, Albrecht et al., 2010).
Traditional explanations for group health disparities locate the cause in structural and economic factors, such as differential exposure to toxic environments, access to healthy foods, quality of health care and health insurance coverage (see Penner, Albrecht et al., 2010). Notably, however, health disparities remain even after accounting for these differences (Smedley et al., 2003). We offer here a social psychological perspective on group health disparities. Social psychology provides a bridge between structural factors and group and individual health outcomes and is thus a “gateway” science. It extends traditional approaches to understanding health disparities by addressing the synergistic contributions of culture, context, and individual-level factors and by illuminating how processes associated with intergroup dynamics can contribute to group health disparities. It speaks to how structural factors influence the psychological experience of social devaluation based on group membership via mechanisms such as negative stereotypes, stigmatization, prejudice, discrimination, social identity threat and expectations of bias. Experiences of devaluation, in turn, influence health. Following, we briefly review key processes in the social psychology of intergroup relations and illustrate the relevance of these processes to disparities in health and health care.
From Intergroup Structure to Individual Dynamics
The social environment is highly complex, and made increasingly so by rapidly developing information and communication technology. Categorizing people into social groups is one of the most fundamental ways in which people simplify and understand their world. Some dimensions of social categorization are nearly universal (e.g., sex), whereas others are culturally defined (e.g., caste). People automatically categorize others based on race, gender, and age, and these categories immediately, and often automatically, elicit evaluations (prejudices) and beliefs (stereotypes) about members of the group. Associating characteristics with groups permits people to draw rapid inferences about an individual with minimal effort (Dovidio & Gartner, 2010).
This process has direct relevance to health care decision making. Because the prevalence of different diseases and conditions varies across groups, a provider who knows a patient’s social category might diagnose that patient’s problems more quickly and more confidently. One problem with stereotypes, however, is that they are overgeneralizations. Thus, they lead observers to see all members of the group in similar ways (ignoring individuating characteristics) and bias perceptions of individuals in stereotype-consistent ways. As a result, social categorization can also lead to misdiagnosis of health problems when group stereotypes are inappropriately applied to an individual. Although people may try to inhibit the use of stereotypes, they may still apply stereotypes when their cognitive resources are challenged by time pressure or deleted by fatigue (Mcrae, Bodenhausen, Milne & Jetten, 1994).
People not only view groups in distinct ways, but they also value groups differently. All societies are hierarchically organized, with some groups having higher status in society than others (Sidanius & Pratto, 1999). Group hierarchy defines intergroup relations and affects the material and psychological realities of members of different groups. Social psychological processes often reinforce the hierarchical structural relations between groups. According to system justification theory (Jost, Banaji, & Nosek, 2004), for example, people are motivated to justify social systems on which they feel dependent, even when they are disadvantaged by the system, because a just system provides a sense of meaning and control. System justification leads people to endorse group stereotypes that explain or rationalize the status quo as fair. Thus, stereotypes rooted in social categorization processes perpetuate differential treatment of groups and lead to stereotypes that justify that treatment. For example, health care providers or insurers may justify limiting the treatment they recommend for Blacks relative to Whites based on the stereotype that Blacks are not sufficiently motivated or capable of taking care of their health (van Ryn et al., 2011). Decisions to withhold services, in turn, may produce health disparities that support the stereotypic perceptions of the group.
Social psychology further explains how structural differences between social groups influence individuals’ thoughts, feelings, and actions, and interactions between individuals, in ways that reinforce the existing social structure. For example, the Stereotype Content Model explains how the structural positions of groups along two dimensions, perceived competence (associated with group status) and warmth (related to whether a group is seen as an ally or competitor) shapes not only the content of group stereotypes, but also the emotional reactions and behavioral orientations people have toward individual group members (Cuddy, Fiske & Glick, 2008). These emotions and behavioral orientations associated with a group’s perceived status and competitiveness can have a direct effect on health through their impact on social policies, allocation of resources, and quality and type of health care provided. For example, groups that are stereotyped as low in both competence and warmth (e.g., poor Blacks, undocumented immigrants, homeless people) generate disgust and contempt, emotions that motivate both passive harm (e.g., neglect) and active harm (attack). Such emotions and orientations may lead members of these groups to receive inferior health care based on the rationale, for example, that they are faking symptoms to receive drugs (Dovidio & Fiske, in press).
Drawing on these core features of intergroup relations— group categorization, hierarchy, and perceived group competence and warmth—social psychology links structural factors with health and health care disparities in three ways. First, social psychology provides direct evidence of key mediating mechanisms, or pathways, by which environmental pressures linked to a group’s position in the social structure translate into psychological perceptions and experiences, psychophysiological responses, and ultimately into health. Second, it identifies moderating factors, processes that increase the vulnerability of people to social or environmental stressors or buffer people against psychological forces or pathogens that would normally adversely affect health. For instance, perceptions of being discriminated against because of one’s membership in a disadvantaged group can increase one’s sense of vulnerability and feeling of stress because of the need for constant vigilance, or it can buffer against stress by providing an external explanation for one’s failure or disadvantaged status. Third, although social psychology generally focuses on typical or normal responses, it also explicitly considers individual differences that explain why people respond differently to the same contextual, social, or medical conditions. Thus, it can explain the significant variation that occurs within groups.
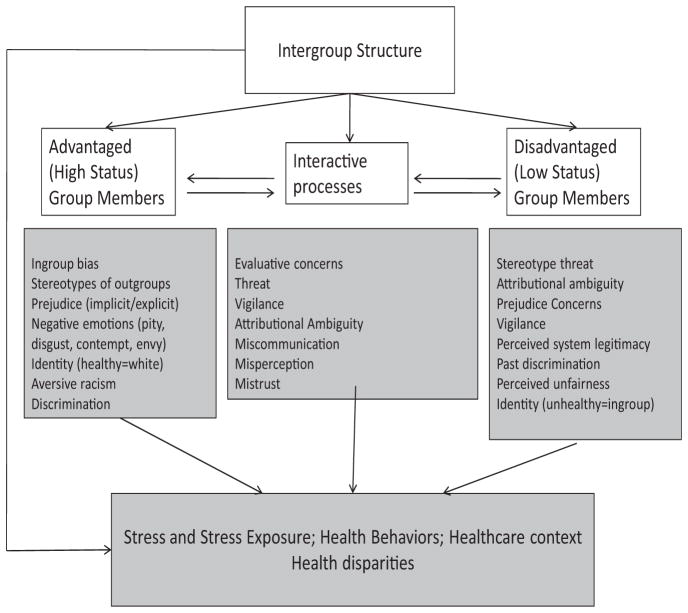
In Figure 1, we present a descriptive model of how structural relationships between groups in society influence social psychological processes relevant to intergroup processes, that in turn, produce group health disparities. This model posits that social and cultural factors determine the status of groups in society and the stereotypes people hold about those groups. Intergroup processes that emerge from these structural dynamics shape how members of high status groups perceive, feel about, and behave toward members of low status or stigmatized groups, how members of low status or stigmatized groups construe and cope with their situation, and how members of high and low status groups interact with each other. These intergroup processes, in turn, affect the extent to which members of high and low status groups are exposed to and experience chronic and acute stress, the health behaviors in which members of these groups engage, and the quality of their health care interactions. As a result of these intergroup processes, group status in society determines not only the material realities of individuals’ lives (e.g., their access to adequate nutrition, safe environments, health care) but also their psychological realities in ways that have important implications for health.
Figure 1.
From Intergroup Processes to Health Disparities: A Social Psychological Perspective.
From Intergroup Behavior to Health Disparities
In this section we focus on three pathways by which the intergroup structures and dynamics (identified above) may lead to group health disparities: (a) by increasing the extent to which members of disadvantaged groups are exposed to major and minor life stresses, (b) by affecting the health-relevant behaviors that members of disadvantaged groups engage in to cope with their situation, and (c) by shaping the quality and nature of the health care interactions that members of disadvantaged groups experience. Within each of these pathways we highlight critical theories and findings from social psychology that illuminate psychological processes—mediating mechanisms, moderating factors, and individual differences—related to prejudice and stereotyping, perceptions and experiences of stigmatization, and the dynamic interplay of intergroup interactions.
Group Differences in Stress Exposure and Experience
Many models of group health disparities argue for central roles of stress, distress, and stress exposure in accounting for the differences in health experienced by members of disadvantaged and advantaged groups (e.g., Matthews & Gallo, 2011; Williams & Mohammed, 2009). Membership in disadvantaged or stigmatized social groups exposes people to more acute and chronic negative life events, circumstances, social interactions, and affective experiences that have the potential to tax or exceed their adaptive resources and lead to stress that negatively affects their health. Members of disadvantaged groups are exposed to more stress in large part because they are disproportionately likely to be victims of unfair treatment based on their group membership (i.e., discrimination). Discrimination can be institutional (instantiated in policies and programs that unfairly disadvantage some groups relative to others) or interpersonal (Krieger, 2003). Both forms of discrimination emerge from intergroup structure and dynamics.
Beyond direct structural influences on stress, intergroup interactions are also a source of stress. During an intergroup interaction, stress may be experienced by members of both low status and high status groups. Members of low status groups find these encounters stressful because of immediate concerns about potential harm in the environment (e.g., discrimination); members of high status groups may experience stress due to uncertainty associated with limited intergroup experience or concerns about behaving inappropriately (Vorauer, 2006).
Prejudice theories
Research on prejudice and stereotyping, most of which has focused on members of advantaged groups (such as Whites), reveals that members of high status groups often hold negative stereotypes and attitudes about members of lower status outgroups that both justify the latter’s disadvantaged position and promote discrimination against them. Because members of high status groups also typically have more resources and power than members of low status groups, the prejudices and negative stereotypes held by the former can have a direct and detrimental effect on the latter’s health by reducing their access to resources important for health, and by exposing them to more stressful experiences (see Figure 1, left hand panel). Discrimination communicates a lack of regard for an individual’s social identity and social exclusion, thus threatening fundamental social needs for self-esteem and belonging (MacDonald & Leary, 2005). Discrimination also signals that the system is not fair, thus threatening people’s need to believe their social environment is just, predictable and controllable (Jost et al., 2004).
Prejudice and discrimination are not always obvious, however. Although negative attitudes, stereotypes, and emotions are openly expressed against some groups (e.g., against gays and lesbians, people who are obese), increasingly egalitarian social norms in countries such as the U.S. often inhibit the display of overt prejudice toward other groups, such as Blacks and Latinos. In addition, even though explicit bias— beliefs and attitudes people know they hold and can control deliberately and strategically—is declining for many groups, people may still harbor significant implicit biases—automatically activated prejudices and stereotypes that can occur outside of personal awareness and over which people have limited control (Greenwald, Poehlman, Uhlmann, & Banaji, 2009). Implicit biases arise through overlearned associations which may be rooted in personal experiences, widespread media exposure, or cultural representations of different groups. Whereas explicit biases are usually measured via self-report, implicit biases are most commonly measured using response latency techniques, such as the Implicit Association Test (IAT; Greenwald et al., 2009), or with neuro-imaging or psychophysiological techniques.
Many people are unaware that they hold negative automatic or implicit racial biases that influence their behavior toward lower status groups. As a result, people may treat members of low status groups, such as ethnic minorities, differently than members of higher status groups or their own group without being aware of doing so. For example, Penner, Dovidio et al. (2010) found that White physicians who were higher in implicit racial bias were perceived by their Black patients as less warm and friendly. The physicians themselves, however, did not recognize the impact of their implicit bias on their behavior.
Stigma theories
Research on stigma, most of which has focused on the perspective of members of low status or disadvantaged groups (such as Blacks), demonstrates that prejudice and discrimination can negatively affect the health of members of disadvantaged groups not only directly but also indirectly, through their appraisals, emotions, and behaviors (see Figure 1, right hand panel). Whether communicated implicitly or explicitly, the perception of being a target of discrimination, or of being stigmatized or devalued, is stressful. As a result of prior experiences (direct or vicarious) of being a target of discrimination, portrayals of their group in the larger culture and the media, and/or socialization by parents, peers, and teachers, members of stigmatized groups are typically aware of the negative stereotypes that are applied to their group within the dominant culture (metastereotypes) and of their risk for being a target of prejudice and discrimination (Crocker, Major, & Steele, 1998). This awareness, once established, exerts a “top down” influence, shaping their perceptions, interpretations, and responses to actual or implied intergroup contexts.
One consequence of this awareness is social identity threat, a psychological state that occurs when a person fears being judged through the lens of a negative group stereotype and/or devalued on the basis of group membership (Steele, Spencer, & Aronson, 2002). Social identity threat is stressful, leading to increased physiological stress responses including increases in blood pressure, skin conductance, and cortisol. Even in the absence of discrimination, situational cues that increase social identity threat can lead people to experience increased stress and associated affective, cognitive, and physiological responses (see Schmader, Johns, & Forbes, 2008, for a review). An obese person, for example, might experience increased stress associated with social identity-threat whenever she is asked her height and weight on a form, or is weighed at the doctor’s office (Burgess, Warren, Phelan, Dovidio, & van Ryn, 2010).
Some people are more sensitive than others to threats to their social identity or to cues that they might be a target of discrimination. Racial minorities who score high on measures of chronic prejudice concerns such as race-based rejection sensitivity (Mendoza-Denton, Downey, Purdie, Davis, & Pietrzak, 2002) or stigma consciousness (Pinel, 1999), compared with those who score low on these measures, are more likely to say they have experienced discrimination in the past, expect to be discriminated against in the future, interpret ambiguous events and interactions as discriminatory, and attend more at a preconscious level to threats to their social identity (e.g., Kaiser, Vick, & Major, 2006).
High chronic prejudice concerns increase vigilance for signs of impending mistreatment and can potentially lead situations to be interpreted as discriminatory even when they are not. Chronic prejudice concerns and associated vigilance may explain why Black patients who perceive more discrimination against them in their lives in general, also are more likely to perceive a specific medical encounter as racially biased (Penner, Dovidio et al., 2010). People who report more instances of past discrimination in their lives also react to recalled instances of discrimination with more anger and rumination and increased blood pressure reactivity (e.g., Guyll, Matthews, & Bromberger, 2001). Worry, rumination, distrust, and uncertainty about anticipated mistreatment can lead to acute increases in blood pressure, reduced heart rate variability, higher cortisol levels, and may ultimately exacerbate physical health problems (Williams & Mohammed, 2009).
Self-reported experiences of chronic and/or acute discrimination are related to poorer mental and physical health (see Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009, for reviews). This relationship is most well-documented for mental health outcomes, such as depression, psychiatric distress, and well-being. However, self-reported experiences of discrimination also are related to poorer physical health outcomes, such as hypertension, diabetes, respiratory problems, self-reported ill health, low birth weight infants, and cardiovascular disease. Although most studies of the discrimination-health link are cross-sectional, several recent prospective studies show that perceived discrimination predicts changes in health over time. Furthermore, this relationship is reliable controlling for potential confounding variables, such as social desirability bias, hostility, and positive and negative affect.
Increased stress associated with being or perceiving oneself to be a target of negative stereotypes, prejudice, and discrimination can negatively affect health through several pathways. Acute episodes of discrimination arouse anger and produce strong cardiac reactions (Guyll et al., 2001; Mendes, Major, McCoy, & Blasco-vich, 2008). Repeated patterns of activation of stress systems in response to acute discrimination can, over time, accumulate to damage the body. In addition to its effects on cardiovascular responses, discrimination affects health through other biological pathways, including repeated activation and ultimately dysregulation of the hypothalamic pituitary adrenal cortical system (McEwen, 2004) and interference with the body’s restorative processes (e.g., by interfering with sleep and relaxation; Beatty et al., 2011).
Although chronic concerns and expectations of unfair treatment can exacerbate stress, it is important to note that they can also prepare an individual for being a target of discrimination. As a result, prejudice expectations may sometimes serve an ironic stress-buffering effect—attenuating stress responses when discrimination is encountered (see Trawalter, Richeson & Shelton, 2009). This stress-buffering function may explain why Black parents sometimes socialize their children to expect to be a target of prejudice (Brodish, Peck, Malanchuk, & Eccles, in press).
In summary, experiences and perceptions of discrimination create stress that has a detrimental effect on health and can exacerbate existing physical health problems. However, these direct effects are not the only way in which discrimination affects health disparities. These perceptions and experiences may also influence health indirectly by affecting health behaviors. Next, we explore how intergroup processes influence behaviors that can undermine health.
Group Differences in Health Behavior
Intergroup structure and dynamics can also lead to group health disparities through group differences in health-relevant behaviors. Targets of prejudice are not passive victims of the negative stereotypes, attitudes, and discriminatory behaviors of members of higher status groups. Rather, they are active agents who seek to make sense of and cope with their predicament. Coping refers to strategies that people use to regulate emotions, maintain a positive identity, and pursue self-relevant goals. Experiencing identity threat and perceiving discrimination triggers coping responses among members of disadvantaged groups, some of which may themselves have short term and/or long term negative effects on health (see Major & Townsend, 2010; Trawalter et al., 2009, for reviews).
The coping strategies that people adopt depend on their appraisals of resources relative to demands (Blascovich & Mendes, 2010). When challenged (resources perceived to exceed or meet demands), people are more likely to engage in positive engagement forms of coping, such as trying to solve the problem that is causing stress. Or, they might try to fight or dominate the situation. When threatened (resources perceived as insufficient to meet demands), people feel defeated and powerless. Over time constant threat can turn into disengagement, which may even be worse than threat because no attempt at coping or persevering with a problem will be made.
One coping strategy used by members of disadvantaged or stigmatized groups is compensation. Compensation involves attempting to overcome the effects of negative stereotypes or stigma, for example by trying especially hard or exerting extra effort to make up for a presumed deficit. Ethnic minorities who expect to be targets of prejudice, either chronically or acutely, for instance, exert more effort in interactions with Whites (e.g., by self-disclosing more or by being more engaged while interacting; Richeson & Shelton, 2007). Although these coping efforts may be successful in fostering a smoother interaction, they can also be costly, leaving an individual cognitively depleted and feeling in-authentic (Richeson & Shelton, 2007).
Members of disadvantaged groups also attempt to cope with social identity threat, prejudice, and discrimination by trying to suppress activated negative group stereotypes (Schmader et al., 2008). This coping strategy also can be costly, temporarily depleting cognitive resources, and undermining performance on subsequent tasks that require executive control, such as performance on intellectually demanding tasks. It can also spill over to reduce self-control in unrelated domains. Self-control is essential for many health-related behaviors, such as resisting unhealthy but tasty foods, quitting smoking, or exercising. Thus, efforts to cope with anticipated or experienced prejudice may leave members of stigmatized groups feeling bad, behaviorally exhausted, and out of control, and may make them susceptible to engaging in behaviors that are bad for their health.
Members of disadvantaged groups may also cope with negative cognitions and emotions generated by identity threat and concerns about discrimination by using escape or avoidance coping strategies that are bad for their health. People who report experiencing more discrimination also report more cigarette smoking, alcohol use, eating comfort foods, substance abuse, and less treatment seeking and medical compliance (Pascoe & Smart Richman, 2009). Gibbons et al. (2010) found that Black adolescents who perceived more discrimination reported increased substance abuse 5 years later. They also found that imagining discrimination led Black adolescents to report greater willingness to try drugs. Anger may mediate these effects; discrimination increases anger, which potentiates risky behavior.
Ironically, unhealthy behaviors may be both a response to stress and a way of coping with stress. For example, a study of 2,780 adults, including 874 Blacks (Jackson et al., 2010), found that greater exposure to stressful environments, combined with engaging in unhealthy behaviors like smoking, excessive alcohol use, overeating, and drug use, predicted greater depression among Whites. Among Blacks, however, greater exposure to stressful environments predicted depression only among those who did not engage in these unhealthy behaviors. For Blacks, these unhealthy behaviors may serve as protective coping mechanisms for mental health outcomes but lead to poorer physical health outcomes, thus contributing to health disparities.
Research on intergroup processes suggests another potential contributor to health disparities. When groups compete over a self-defining behavior, higher resource (advantaged) groups are better able to claim esteemed behaviors as ingroup-defining, whereas lower status (disadvantaged) groups maintain a positive social identity by emphasizing alternative, and sometimes oppositional, characteristics or behaviors (a strategy termed “social creativity” by Tajfel & Turner, 1979). Engaging in behaviors that are linked to one’s social identity can have negative or positive health consequences, depending on which behaviors are ingroup-identified. For example, Oyserman, Fryberg, and Yoder (2007) found that racial/ethnic minorities view health promotion behaviors as defining White-middle-class individuals and unhealthy behaviors (such as smoking and eating fast foods) as ingroup-defining. Furthermore, among racial/ethnic minorities and low SES participants, making race/ethnicity and low SES salient increased health fatalism and reduced access to health knowledge. This research suggests that cultural tailoring of health promotion programs must be undertaken with care when unhealthy behaviors are identified with a cultural ingroup (e.g., Hawkins, Kreuter, Resnicow, Fishbein & Dijkstra, 2008).
In summary, coping is a complex process that may result in behaviors that reduce stress in the short term but that ironically can accumulate to produce worse health over time. We next turn to interactions between disadvantaged and advantaged group members, specifically in the context of a doctor–patient interaction, as a third pathway to health disparities.
Group Differences in Health Care: Doctor–Patient Interactions
Intergroup processes can create and maintain health disparities by affecting the nature and quality of the health care that members of advantaged and disadvantaged groups receive in interactions with health care providers. Health care interactions can be viewed as a microcosm of the intergroup dynamics discussed above. They are shaped by the perceivers’ (i.e., typically White physicians’) conscious and unconscious attitudes, beliefs, and behaviors, the targets’ (i.e., disadvantaged group members’) expectations and apprehensions, and by the dynamic interplay between the two as they communicate, perceive, and reciprocally influence each other. In intergroup interactions, the reciprocal responses of members of different groups can both reflect and reinforce existing social biases, thereby making intergroup interactions stressful (Vorauer, 2006). Participants in mixed-race interactions, for example, typically refer to the crossed-race nature of the exchange to interpret and explain the other person’s actions, which can potentially reinforce bias (Richeson & Shelton, 2007). Because interpersonal interactions between members of different groups occur across a “category divide,” disagreements may be assessed as being less open to a solution than in within-group interactions. Furthermore, once a difference of opinion is seen to reflect group differences, it may be especially difficult to resolve. When these intergroup dynamics occur in the context of provider-patient interactions, the expectations, apprehensions, and biases of members of both high status and low status groups can affect the quality of the health care interaction, and ultimately contribute to disparities in the quality of health care. Following, we review social psychological research on disparities in health care interactions, most of which has focused on White physicians interacting with Black patients.
Physician attitudes, expectations, and biases
Even though people in helping professions such as health care typically see themselves as socially conscious and fair, research suggests that they can hold biases that influence their responses to members of lower status groups within the medical context (see Penner, Al-brecht et al., 2010; Smedley et al., 2003). Sometimes physicians and nurses express their prejudice explicitly and engage in treatment bias openly, such as with patients who belong to groups for which the norms against bias are weak. For instance, physicians explicitly express more negative attitudes toward obese than average-weight patients, and report that they would spend less time treating obese patients (Hebl & Xu, 2001). For groups in which there are strong social norms against bias, such as Blacks, health care providers are less likely to express explicit prejudice and stereotypes. Nonetheless, they still have high levels of implicit biases toward these groups (Dovidio & Fiske, in press). These biases can systematically affect their medical decision-making. Green et al. (2007) found that White physicians responding to a vignette about an emergency room patient with symptoms of serious heart problems were less likely to recommend appropriate medical treatment (prescribing thrombolytic drugs) to Black than White patients the higher they were in implicit racial bias. Because implicit negative attitudes are automatically activated and often operate unconsciously, however, medical providers may be unaware that they hold negative racial biases that influence their behavior toward patients who belong to minority groups.
According to Aversive Racism Theory (Dovidio & Gaertner, 2004), people who believe they are not prejudiced but who harbor implicit biases tend to express their bias in subtle, rationalizable ways (attributing their actions to nonracial factors), but avoid acting in openly bigoted ways that violate normative standards. Consistent with this perspective, in the context of health care, racial disparities in treatment are more likely to occur for “high-discretion” procedures, such as recommending a test or making a referral for a procedure or drug in which the provider has multiple interpretations and alternatives to consider than for “low-discretion” procedures, such as emergency surgery, in which appropriate action is clearer (see Smedley et al., 2003). In addition, compared with Whites, ethnic/racial minority patients are under-treated for pain, which is difficult to empirically verify and quantify (van Ryn et al., 2011). However, when presented with relatively straightforward medical vignettes and minimal other demands on their cognitive resources, medical students do not show racial biases in medical decision-making overall and no systematic influence of implicit bias (Haider et al., 2011).
Patient attitudes, expectations, and biases
Patients who are members of lower status, or stigmatized groups, particularly if they are high in prejudice concerns, may be wary and suspicious of mistreatment by health care providers who are members of higher status groups, leading them to be distrustful of medical advice (see Penner, Albrecht et al., 2010, for a review). Patient participation, trust, and satisfaction are important determinants of patients’ medical adherence and commitment to continued treatment. Thus, the perceptions of members of disadvantaged groups have significant health-related implications.
Blacks, for example, are significantly more likely than Whites to believe that their race negatively affects their health care and are less trusting of their physicians than are Whites. The majority of Black patients (57%) report that White physicians display bias toward them in their health care interactions either “often” or “very often” (Malat & Hamilton, 2006). These perceptions of bias, irrespective of their accuracy, negatively affect the health care of the individuals who hold them. Black patients are less likely to schedule appointments with their physicians and are more likely to postpone or delay their appointments with a White physician than a Black physician. Among minority women, those who have less trust in the health care system or their provider are less likely to pursue recommended tests and use recommended preventive services (see Dovidio & Fiske, in press for a review). Overall, Black patients who perceive greater discrimination against them in their lives are more likely to perceive racial bias in a specific medical encounter, and the perception of bias predicts less medical adherence and ultimately poorer health. Furthermore, because social identity threat is likely to be aroused in racially discordant medical interactions, minority patients may be especially reluctant to ask questions that could reveal a failure to understand instructions (Burgess et al., 2010).
The medical encounter
Medical encounters between health care professionals (who tend to belong to higher status groups) and patients are, on average, less effective and less satisfying when the patient is a member of a disadvantaged group. Social psychological research illuminates why. Compared with interactions between members of the same group, medical encounters between members of different groups are more likely to be characterized by vigilance, threat, attributional ambiguity, miscommunication, and mis-perception (center panel of Figure 1; see also Blascovich & Mendes, 2010).
In intergroup interactions, members of both advantaged and disadvantaged groups, but especially the latter, are often vigilant for cues of bias or potential threat (Richeson & Shelton, 2007; Vorauer, 2006). Vigilance, in turn, produces a prevention focus that directs cognitive resources toward potentially threatening information, tuning attention, perception, judgment, and memory toward possible threats, such as the potential for being treated unfairly (Oyserman, Uskul, Yoder, Nesse, & Williams, 2007). Anticipating being negatively stereotyped or mistreated by members of another group, either chronically or due to specific cues in the situation, leads to negative emotions and cognitions, depleted cognitive resources, and physiological stress responses. Women high in chronic prejudice concerns (who perceived more sexism), for example, showed signs of greater stress (had greater increases in the hormone cortisol) while interacting with a male partner than did women lower in chronic prejudice concerns when cues in the situation signaled that being a target of sexism was likely or possible (Townsend, Major, Gangi, & Mendes, 2011). Expecting prejudice can also create additional stressors by arousing hostility in interactions that cause others to behave in ways that lead those expectations to come true.
Although everyone can be uncertain at times about why they are being treated a given way, intergroup interactions are characterized by attributional ambiguity, that is, uncertainty as to whether group membership is an explanation for outcomes or treatment(Crocker et al., 1998). This can further heighten the stressfulness of medical encounters between members of different groups. Contemporary prejudice is often subtle, indirect, and/or disguised. Attributional ambiguity can be experienced not only with respect to negative treatment but also with regard to positive treatment or outcomes. Indeed, highly prejudiced Whites sometimes exert more effort and display more superficially positive behavior than less prejudiced Whites during interracial interactions, possibly to avoid appearing prejudiced (Mendes & Koslov, 2011). As a result, although being a recipient of positive treatment or accepting feedback from others typically increases feelings of self-esteem and positive affect, positive treatment from Whites to Blacks sometimes does not engender these same beneficial responses. Lower self-esteem, more negative emotions, poorer performance, and cardiovascular responses associated with threat have all been observed among Blacks after they receive positive interpersonal feedback from Whites, possibly because Blacks are uncertain whether the feedback is genuine (Major & Sawyer, 2009). Consequently, in interactions with health care providers who are members of advantaged groups, members of disadvantaged groups may wonder to what extent prejudice or group membership explains their treatment, either negative or positive.
Miscommunication also characterizes intergroup interactions. Effective communication depends on accurately and sensitively decoding the thoughts, intentions, and feelings of others (Epley & Waytz, 2010). People are generally more accurate at detecting the emotions and intentions of ingroup members than outgroup members (Ambady & Weisbuch, 2010). Moreover, people are systematically biased in their interpretations of the emotions expressed by members of other groups. Whereas racial/ethnic majority and minority group members recognize the cues of anxiety among members of their own group, because nonverbal expressions of anxiety overlap with those of dislike, they tend to interpret these expressions as dislike when displayed by members of another group. Also, cultural differences in nonverbal displays and their interpretations (Ambady & Weisbuch, 2010) and difficulty in understanding non-native accents (Gluszek & Dovidio, 2010) can make medical interactions between members of different groups difficult.
Observational studies reveal that medical encounters between White physicians and racial/ethnic minority patients are briefer, less patient-centered, and less positive than same-race interactions (see Penner, Albrecht et al., 2010, for a review). White physicians spend significantly less time planning treatment, providing health education, and answering questions with Black than White patients. Nonetheless, despite the evidence of group disparities in health care treatment and interactions, physicians do not fully recognize the bias in this process. Only 55% of White physicians agree that “minority patients generally receive lower quality care than White patients” (AMA/NHMA/NMA Commission to End Health Care Disparities, 2005). One reason, as we suggested earlier, is that physicians may be unaware of the existence and operation of their implicit prejudices and stereotypes. In contrast, as discussed above, patients who are members of disadvantaged groups may be vigilant for cues of bias and may thus recognize the subtle cues of a physician’s implicit bias (Dovidio et al., 2008). When a White physician is higher in implicit racial bias, Black patients feel less respected, like their physician less, and have less confidence in the physician (Cooper, 2011). They are especially dissatisfied if the physician is also low in explicit prejudice (i.e., an aversive racist), presumably because they detect mixed messages that undermine their trust in the physician (Penner, Dovidio et al., 2010). Although physicians in this latter study did not recognize the impact of their implicit bias on their behavior, those higher in explicit prejudice did admit that they made less effort to involve the Black patient in medical decisions.
In summary, social psychological theory and research on intergroup dynamics provide important insights into, and a useful framework for considering, how health disparities between social groups emerge and persist in health care interactions. Vigilance, attributional ambiguity, misunderstanding, miscommunication, and misperceiving intentions of others across the racial divide collectively contribute to strained, awkward, and less satisfying medical encounters between members of different groups.
Future Directions and Unanswered Questions
The causes of health disparities between members of advantaged and disadvantaged groups are complex. A fundamental message of social psychological research is that the expectations, assumptions, interpretations, actions, and reactions of both members of advantaged groups and members of disadvantaged groups contribute to disparities in health and health care. Fully understanding and addressing health disparities will benefit from integrative, multidisciplinary efforts of social and health psychologists. Following, we identify several research directions that we see as ripe for collaborative investigation. Our goal here is to highlight a few research questions and areas that we believe are at the frontier of the nexus of social psychology and health disparities research.
Implicit Versus Explicit Bias
One clear implication of research on explicit and implicit bias is that researchers who study health disparities cannot simply rely on explicit self-report questionnaires to index the extent of racial bias present (Greenwald et al., 2009). Many individuals who report low explicit bias are nonetheless still high in implicit bias. Although individuals who explicitly express high racial bias are likely to be the most discriminatory, it could be argued that individuals with low explicit and high implicit bias are even more problematic for minorities because they do not acknowledge their biases, which they may express subtly and systematically. Moreover, these unacknowledged, implicit biases are particularly likely to translate into discriminatory judgments during stressful, time-pressured, or other high emotional arousal situations, because in these situations their automatic/intuitive judgments will override their more controlled, thoughtful reactions. These are the conditions under which many health care providers frequently operate.
Beyond understanding more fully the joint influences of explicit and implicit bias and stereotyping in medical decision making and encounters, it is important to develop effective strategies to eliminate, or at least limit, the effect of bias in health care. Interventions that seek to educate health care providers about explicit-implicit discrepancies may guide more egalitarian actions. In addition, evidence-based guidelines for treatment may restrict the unintended influence of bias by reducing the degree to which biased thoughts, expectations, and assumptions produce differential treatment. Social psychology tends to focus on social problems more than on interventions to address the problems. Thus, collaborations among social and health psychologists and medical researchers and practitioners can yield practical interventions and new theoretical insights into managing implicit and explicit bias.
Perceived Discrimination and Health
Numerous studies reveal a negative relationship between perceptions of discrimination and mental and physical health outcomes. The mechanisms that explain this relationship, however, are still relatively unknown. Because perceptions of discrimination do not always show a one-to-one correspondence with objective exposure to discrimination (Major & Sawyer, 2009), it is unclear how much the negative relationship between self-reported discrimination and health reflects differences in objective experiences of discrimination or in subjective perceptions of discrimination that are independent of actual exposure, and perhaps associated with chronic prejudice concerns. Disentangling the contributions of person and environment to this relationship clearly is important for designing effective interventions. Also unknown are the relative health risks of being certain versus being unsure of whether one was a victim of discrimination. Blatant discrimination can be more readily understood and processed than discrimination that is more subtle or attributionally ambiguous. Thus, it is possible that incidents of overt bias can be less stressful, and less detrimental to health, than instances of subtle bias which arouse suspicion but not certainty of bias. Evidence consistent with this idea that uncertainty can be stressful was found in a study in which Blacks were asked to write about past experiences with discrimination. The less they expressed certainty that their experiences were actually due to racism (vs. other factors), the weaker antibody response they showed to a viral strain (Stetler, Chen, & Miller, 2006).
Moderators of Health Disparities
Another important avenue for future research is to identify personal, situational, institutional, and cultural factors that moderate reactions to social disadvantage and perceived discrimination. Some individuals are more vulnerable to the stress associated with perceived discrimination than others. People who believe the system is fair, for example, show more negative acute reactions to perceiving discrimination against themselves or their group than do those who believe the system is unfair (Major & Sawyer, 2009). Over the long-term, however, believing the system is unfair may undermine health by enhancing vigilance and chronic prejudice concerns. Institutional factors may moderate health disparities by reinforcing or attenuating racial biases, for example, in health care (Krieger, 2003). Cultural factors also moderate health disparities. First-generation immigrants to the United States, such as foreign-born Hispanics, have better health than do second generation immigrants (American-born Hispanics), despite the fact that the former are poorer, face more language barriers, and are exposed to as much if not more prejudice. Indeed, foreign-born Latinos are as healthy as Whites, whereas American-born Latinos are as unhealthy as Blacks (Sternthal, Slopen, & Williams, 2011). Explaining the paradoxical “protective” effects of being a new immigrant is an important avenue for future research.
Identity Threat Interventions
Patients, particularly those who are members of traditionally stigmatized groups, may experience significant social identity threat in medical contexts (Burgess et al., 2010). Several social psychological interventions have proved successful in reducing social identity threat and improving academic performance among racial minorities who are negatively stereotyped in academic domains. One of these interventions, a “self-affirmation” exercise, affirms a sense of self-integrity. Implementing a brief self-affirmation intervention early in the school year resulted in improvements in racial minority students’ academic grades 2 years postintervention (Cohen, Garcia, Purdie-Vaughns, Apfel, & Br-zustoski, 2009). Another intervention focuses on activating a “sense of belonging” among group members who have been traditionally marginalized in academic institutions. A brief intervention increasing a sense of belonging resulted in better self-reported health and fewer reported doctor visits among Black youths 3 years postintervention (Walton & Cohen, 2011). Although these results seem remarkable, researchers believe that early interventions that promote a sense of self-integrity or belonging positively alter appraisals and beliefs in ways that continue to flourish and create a positive environment for marginalized group members. These interventions might be effectively applied to the health domain. For example, similar interventions may be effective at promoting healthier behaviors among disadvantaged group members or among individuals with an early diagnosis in which treatment adherence could promote longevity.
Conclusion
Social psychology offers a valuable perspective on health disparities because it bridges structural and societal factors with individual-level psychological and biological processes. Social psychological theory and research on intergroup relations thus complements traditional approaches to health disparities and provides unique insights into their causes and ways to reduce them. Social psychological research indicates that individual-level processes can be activated or inhibited by a range of external influences and also controlled, at least to some degree, by self-regulatory processes, and thus become potentially valuable targets for interventions. When particular interventions are prohibited by practical constraints (e.g., expense), understanding the ways interventions operate through the social psychological pathways identified here may help to identify alternative strategies that are more feasible.
Acknowledgments
Work on this article was supported by NIH Grant R01 HL079383 to Brenda Major and Wendy Berry Mendes, a Fellowship from the Center for Advanced Study in the Behavioral Sciences to Brenda Major, and by NIH Grant RO1HL0856331-0182 and NIDA Grant 1R01DA029888-01 to John F. Dovidio.
Footnotes
We relied on hundreds of references to write this article. In the interest of journal space, however, we limited our citations to review articles whenever possible. Interested readers can e-mail any of the authors to request a full reference list for this article.
Contributor Information
Brenda Major, University of California, Santa Barbara.
Wendy Berry Mendes, University of California, San Francisco.
John F. Dovidio, Yale University
References
- Ambady N, Weisbuch W. Nonverbal behavior. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of social psychology. 5. Vol. 1. Hoboken, NJ: Wiley; 2010. pp. 464–497. [Google Scholar]
- American Medical Association/NHMA/NMA Commission to End Health Care Disparities. Preliminary survey brief: Physicians are becoming engaged to address health disparities. 2005 Retrieved from http://www.ama-assn.org/ama/pub/physician-resources/public-health/eliminating-health-disparities/commission-end-health-care-disparities/quality-health-care-minorities-understanding-physicians.p.
- Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Matthews KA. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh Sleep SCORE Project. Health Psychology. 2011;30:351–359. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blascovich J, Mendes WB. Social psychophysiology and embodiment. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of social psychology. 5. Vol. 1. Hoboken, NJ: Wiley; 2010. pp. 194–227. [Google Scholar]
- Brodish A, Peck S, Malanchuk O, Eccles J. Racial/ethnic socialization in African American Families: The role of parent and youth reports. Developmental Psychology. doi: 10.1037/a0036800. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Warren J, Phelan S, Dovidio J, van Ryn M. Stereotype threat and health disparities: What medical educators and future physicians need to know. Journal of General Internal Medicine. 2010;25:S169–S177. doi: 10.1007/s11606-009-1221-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen GL, Garcia J, Purdie-Vaughns V, Apfel N, Brzustoski P. Recursive processes in self-affirmation: Intervening to close the minority achievement gap. Science. 2009;324:400–403. doi: 10.1126/science.1170769. [DOI] [PubMed] [Google Scholar]
- Cooper LA. Patient-client and perceived discrimination in health care. Paper presented at the Science of Research on Discrimination and Health Conference, National Cancer Institute; Bethesda, MD. 2011. Feb, [Google Scholar]
- Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. Handbook of social psychology. 4. Vol. 2. Boston, MA: McGraw Hill; 1998. pp. 504–553. [Google Scholar]
- Cuddy AJ, Fiske ST, Glick P. Warmth and competence as universal dimensions of social perception: The Stereotype Content Model and BIAS map. Advances in Experimental Social Psychology. 2008;40:61–149. doi: 10.1016/S0065-2601(07)00002-0. [DOI] [Google Scholar]
- Dovidio JF, Fiske ST. Under the radar: How unexamined biases on decision-making processes in clinical interactions can contribute to healthcare disparities. American Journal of Public Health. doi: 10.2105/AJPH.2011.300601. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, Gaertner SL. Aversive racism. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 36. San Diego, CA: Academic Press; 2004. pp. 1–51. [Google Scholar]
- Dovidio JF, Gaertner SL. Intergroup bias. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of social psychology. 5. Vol. 2. Hoboken, NJ: John Wiley & Sons; 2010. pp. 1084–1121. [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Epley N, Waytz A. Mind perception. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of social psychology. 5. Hoboken, NJ: John Wiley & Sons; 2010. pp. 498–541. [Google Scholar]
- Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng C, Kiviniemi M, O’Hara RE. Exploring the link between racial discrimination and substance use: What mediates? What buffers? Journal of Personality and Social Psychology. 2010;99:785–801. doi: 10.1037/a0019880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluszek A, Dovidio JF. The way they speak: A social psychological perspective on the stigma of nonnative accents in communication. Personality and Social Psychology Review. 2010;14:214–237. doi: 10.1177/1088868309359288. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for Black and White patients. Journal of General Internal Medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: Relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20:315–325. doi: 10.1037/0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swoboda S, Cronwee EE., III Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. Journal of the American Medical Association. 2011;306:942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebl M, Xu J. Weighing the care: Physicians’ reactions to the size of a patient. International Journal of Obesity. 2001;25:1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- Jackson PB, Williams DR, Stein DJ, Herman A, Williams SL, Redmond DL. Race and psychological distress: The South African Stress and Health Study. Journal of Health and Social Behavior. 2010;51:458–477. doi: 10.1177/0022146510386795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jost JT, Banaji MR, Nosek BA. A decade of System Justification Theory: Accumulated evidence of conscious and unconscious bolstering of the status quo. Political Psychology. 2004;25:881–919. doi: 10.1111/j.1467-9221.2004.00402.x. Retrieved from http://www.jstor.org/stable/3792282. [DOI] [Google Scholar]
- Kaiser CB, Vick SB, Major B. Prejudice expectations moderate preconscious attention to cue that are threatening to social identity. Psychological Science. 2006;17:332–338. doi: 10.1111/j.1467-9280.2006.01707.x. [DOI] [PubMed] [Google Scholar]
- Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: An ecosocial perspective. American Journal of Public Health. 2003;93:194–199. doi: 10.2105/AJPH.93.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin. 2005;131:202–223. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- Major B, Sawyer PJ. Attributions to discrimination: Antecedents and consequences. In: Nelson TD, editor. Handbook of prejudice, stereotyping, and discrimination. New York, NY: Psychology Press; 2009. pp. 89–110. [Google Scholar]
- Major B, Townsend S. Coping with prejudice, stereotyping, and discrimination. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping, and discrimination. Thousand Oaks, CA: Sage; 2010. pp. 410–425. [DOI] [Google Scholar]
- Malat J, Hamilton MA. Preference for same-race health care providers and perceptions of discrimination in health care. Journal of Health and Social Behavior. 2006;47:173–187. doi: 10.1177/002214650604700206. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology. 2011;62:501–530. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcrae N, Bodenhausen GV, Milne AB, Jetten J. Out of mind but back in sight: Stereotypes on the rebound. Journal of Personality and Social Psychology. 1994;67:808–817. doi: 10.1037/0022-3514.67.5.808. [DOI] [Google Scholar]
- McEwen BS. Protective and damaging effects of the mediators of stress and adaptation: Allostasis and allostatic load. In: Schulkin J, editor. Allostasis, homeostasis, and the costs of physiological adaptation. New York, NY: Cambridge; 2004. pp. 65–98. [Google Scholar]
- Mendes WB, Koslov K. Brittle smiles: Overcorrection during intergroup interactions. 2011. Manuscript submitted for publication. [Google Scholar]
- Mendes WB, Major B, McCoy S, Blascovich J. How attributional ambiguity shapes physiological and emotional responses to social rejection and acceptance. Journal of Personality and Social Psychology. 2008;94:278–291. doi: 10.1037/0022-3514.94.2.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology. 2002;83:896–918. doi: 10.1037/0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Oyserman D, Fryberg SA, Yoder N. Identity-based motivation and health. Journal of Personality and Social Psychology. 2007;93:1011–1027. doi: 10.1037/0022-3514.93.6.1011. [DOI] [PubMed] [Google Scholar]
- Oyserman D, Uskul AK, Yoder N, Nesse RM, Williams DR. Unfair treatment and self-regulatory focus. Journal of Experimental Social Psychology. 2007;43:505–512. doi: 10.1016/j.jesp.2006.05.014. [DOI] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Albrecht TL, Orom H, Coleman DK, Underwood W. Health and heath care disparities. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The Sage handbook of prejudice, stereotyping and discrimination. Thousand Oaks, CA: Sage; 2010. pp. 472–489. [DOI] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. doi: 10.1016?j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinel EC. Stigma consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037/0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Richeson JA, Shelton JN. Negotiating interracial interactions: Costs, consequences, and possibilities. Current Directions in Psychological Science. 2007;16:316–320. doi: 10.1111/j.1467-8721.2007.00528.x. [DOI] [Google Scholar]
- Schmader T, Johns M, Forbes C. An integrated process model of stereotype threat effects on performance. Psychological Review. 2008;115:336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidanius J, Pratto F. Social dominance: An intergroup theory of social hierarchy and oppression. New York, NY: Cambridge University Press; 1999. [DOI] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Steele CM, Spencer SJ, Aronson J. Contending with group image: The psychology of stereotype threat and social identity threat. Advances in Experimental Social Psychology. 2002;34:379–440. doi: 10.1016/S0065-2601(02)80009-0. [DOI] [Google Scholar]
- Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: How much does stress really matter? Du Bois Review. 2011;8:95–113. doi: 10.1017/S1742058X11000087. doi: 1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetler C, Chen E, Miller GE. Written disclosure of experiences with racial discrimination and antibody response to an influenza vaccine. International Journal of Behavioral Medicine. 2006;13:60–68. doi: 10.1207/s15327558ijbm1301_8. [DOI] [PubMed] [Google Scholar]
- Tajfel H, Turner JC. An integrative theory of intergroup conflict. In: Austin WG, Worchel S, editors. The social psychology of intergroup relations. Monterey, CA: Brooks/Cole; 1979. pp. 33–48. [Google Scholar]
- Townsend SSM, Major B, Gangi CE, Mendes WB. From “in the air” to “under the skin”: Cortisol responses to social identity threat. Personality and Social Psychology Bulletin. 2011;37:151–164. doi: 10.1177/0146167210392384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trawalter S, Richeson JA, Shelton JN. Predicting behavior during interracial interactions: A stress and coping approach. Personality and Social Psychology Review. 2009;13:243–268. doi: 10.1177/1088868309345850. [DOI] [PubMed] [Google Scholar]
- van Ryn M, Burgess DJ, Dovidio JF, Phelan SM, Saha S, Malat J, Perry S. The impact of racism on clinician cognition, behavior, and clinical decision-making. Du Bois Review. 2011;8:199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vorauer JD. An information search model of evaluative concerns in intergroup interaction. Psychological Review. 2006;113:862–886. doi: 10.1037/0033-295X.113.4.862. [DOI] [PubMed] [Google Scholar]
- Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331:1447–1451. doi: 10.1126/science.1198364. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]