Abstract
Infections of the central nervous system are a significant cause of neurologic dysfunction in resource-limited countries, especially in Africa. The prevalence is not known and is most likely underestimated because of the lack of access to accurate diagnostic screens. For children, the legacy of subsequent neurodisability, which affects those who survive, is a major cause of the burden of disease in Africa. Of the parasitic infections with unique effect in Africa, cerebral malaria, neurocysticercosis, human African trypanosomiasis, toxoplasmosis, and schistosomiasis are largely preventable conditions, which are rarely seen in resource-equipped settings. This article reviews the current understandings of these parasitic and other rarer infections, highlighting the specific challenges in relation to prevention, diagnosis, treatment, and the complications of coinfection.
Introduction
Infections of the central nervous system (CNS) are among the most devastating diseases with high mortality and morbidity. These are infections caused by various pathogens including bacteria, mycobacteria, virus, fungus, and parasites. Although these infections occur worldwide, Africa particularly bears a huge burden of these infections. The burden of these diseases is made worse because survivors are often left with neurologic sequelae affecting mobility, sensory organs, and cognitive functions, as well as epilepsy. They inflict suffering by causing lifelong disabilities, disfigurement, reduced economic productivity, and social stigma.1
CNS infections are underestimated as a cause of neurologic dysfunction in resource-limited countries, especially in Africa. According to World Health Organization (WHO) estimates, there are approximately 1 billion people who are affected by 1 or more neglected tropical diseases. These diseases are considered “neglected” because they occur mostly in the poorest of populations. Among these neglected tropical diseases are several infections that affect the CNS such as human African trypanosomiasis (HAT), Chagas disease, leprosy, malaria, and neurocysticercosis (NCC).2 Human immunodeficiency virus (HIV) and tuberculosis also create a heavy disease burden and are addressed in other articles of this edition.
In this review, we highlight the understandings from some of the parasitic infections that significantly affect the CNS in African children. In a parallel article, the key viral infections of significance in Africa are reviewed.
Cerebral Malaria
Pediatric cerebral malaria (CM) affects 3 million children each year resulting in approximately 1 million deaths, with 90% of CM-related deaths occurring in Africa.3 Recent reports suggest that cases of pediatric CM are falling significantly throughout areas where malaria is endemic.4
There has been a reduction in the numbers of malaria cases and malaria-related deaths by up to 50% over the past decade in several African countries including Tanzania, Kenya, and Zambia.5–7 Possible reasons for the reductions are multifactorial, which include not only improvement in quality of health systems, for example, better diagnostics and implementation of highly effective antimalarial drugs, but also scale investments in intervention strategies that result in achieving high coverage of bed nets and intensification of indoor residual spraying of insecticides. Moreover, there has been implementation of intermittent presumptive treatment in vulnerable groups.3 Climatic changes globally and changes in rainfall and humidity may also have affected malaria vectors.8 However, whether these trends persist remains to be seen.
The main pathologic process that leads to coma in pediatric CM is sequestration of parasitized red blood cells in the cerebral microcirculation leading to obstruction.9
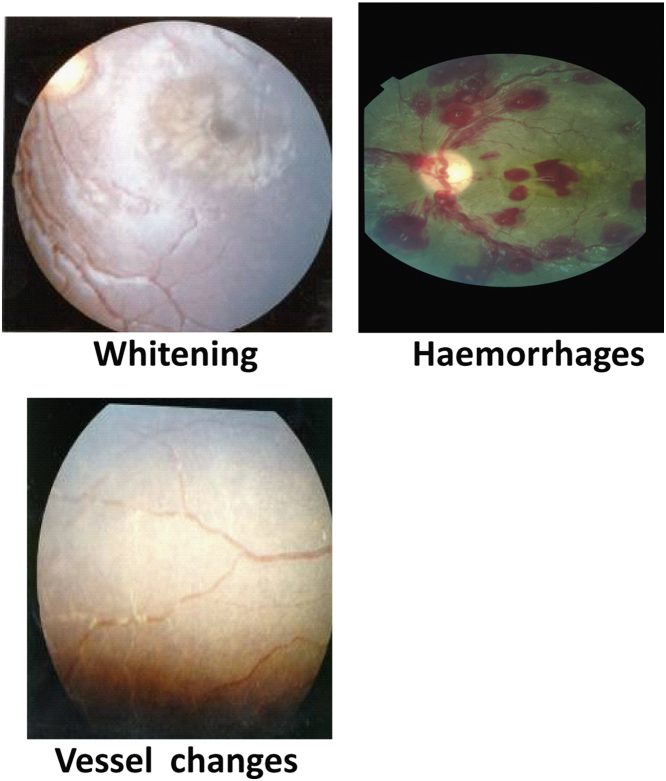
The Blantyre Coma Scale (Table) is used in patient assessments where CM is highly suspected based on (1) coma with no localizing response to pain that persists for more than 1 hour if the patient has experienced a generalized seizure, (2) asexual forms of Plasmodium falciparum found in the blood, and (3) exclusion of other causes of encephalopathy.10 Newer antimalarial agents that rapidly clear peripheral parasitemia improve survival, but mortality rates remain at 12%-25%.11 In high-transmission areas, asymptomatic parasitemia is common, and as such in a child with febrile illness and parasitemia, it represents a diagnostic dilemma as to whether the illness is owing to the parasitemia or another pathology. A postmortem study in Malawi of children meeting WHO case definition of CM found that 23% had a nonmalarial cause of their coma.9 Retinal examination is now recommended, as retinopathy has a high specificity and sensitivity to features diagnostic of CM (Fig. 1).12,13 Malaria and HIV coinfection cases are likely to occur in sub-Saharan Africa, where both diseases are endemic. There are few reports on the effect of HIV on the presentation and outcome of CM.14,15 Other viral infections can masquerade as CM, and such dual infections result in poorer outcome.16,17
Table.
The Blantyre Coma Scale92
| Verbal | 0: No cry |
| 1: Inappropriate cry or moan | |
| 2: Appropriate cry | |
| Motor | 0: Nonspecific or no response |
| 1: Withdrawal from pain | |
| 2: Localizes pain | |
| Eye | 0: Not directed |
| 1: Directed eye movements | |
Figure 1.
The typical findings of malaria retinopathy. With permission from Dr Ian J C MacCormick. (Color version of figure is available online.)
Artemisinin-based combination therapies are now recommended by the WHO as first-line treatment of uncomplicated falciparum malaria in all areas where malaria is endemic.18 Parenteral artesunate is replacing quinine for the treatment of severe malaria.3 Unlike other parts of the world, resistance trends are yet to be seen in Africa.19
Neurocysticercosis
Cysticercosis is probably the most common parasitic infection of the CNS globally. It is due to the brain infiltration by the larval stage of the cestode Taenia solium (cysticerci). This parasite is commonly found in resource-poor countries of Latin America, Asia, and sub-Saharan Africa.20,21 NCC represents an important cause of seizures in children in endemic countries21 as well as a major cause of epilepsy in Africa.22,23 Lesions in NCC can be “active” when they are associated with parenchymal cysts on magnetic resonance imaging, or computed tomographic scans, or “inactive” when scans show calcifications, which are better appreciated on computed tomographic imaging (Fig. 2).24,25
Figure 2.
CT brain imaging of a 7-year-old girl from the Eastern Cape of South Africa with a severe seizure disorder, and associated neuroregression, secondary to neurocysticercosis. All stages of the disease are seen from the vesicular (cyst and scolex), colloidal (ring enhancement with edema), granular nodular degeneration (decreased enhancement and edema with early calcification) through to involution (calcification). CT, computed tomographic.
Clinical manifestations of NCC are influenced by the number, size, location, and stage of the parasites as well as the immune response of the host with the associated inflammation. Seizure disorders are typically seen in relation with degenerating cysts and the associated brain inflammation. However, NCC may present with almost any neurologic manifestation including encephalopathy and psychiatric disorders.26,27 Extraparenchymal NCC can present with signs of raised intracranial pressure.28 The overall prognosis is good, and clinical manifestations tend to decrease with time.29
A suspected diagnosis of NCC is confirmed with a combination of neuroimaging and serology.30,31 In most parts of Africa, neither resource is available, and management is based on clinical suspicion.
The effect of HIV coinfection on the natural history of NCC has not been fully studied. Small case series in HIV-coinfected individuals report the occurrence of basilar meningitis (racemose cysticercosis), also giant cysts that are uncommon in immunocompetent hosts.32–34
Praziquantel and albendazole are the recommended antiparasitic drugs for the treatment of NCC.35 The use of concomitant steroids is mandatory to decrease the risk of neurologic symptoms that may appear during treatment. However, no standard dose or duration is determined.36 NCC is a potentially eradicable disease. With successful implementation of treatment in humans and pigs as well as enforcement of hygienic measures, for example, enforcing pig pens, building of latrines, and hand washing after toilet use, cases of T. solium infestation may be prevented and therefore cases of epileptic seizures, reducing the burden of suffering. Consequently, this would reduce socioeconomic losses to African societies.37
Human African Trypanosomiasis
Infection with Trypanosoma brucei gambiense, which causes the West African trypanosomiasis, or Trypanosoma brucei rhodesiense, which causes the East African disease, is transmitted by the bite of an infected tsetse fly.
Over the last decade, stepped-up public health control efforts in the major endemic countries in sub-Saharan Africa have resulted in the reduction of cases of HAT from 300,000-500,000 cases to approximately 50,000-70,000 cases. However, 17,000 new cases still occur annually.38
These new cases of the Gambian sleeping sickness occurred in the Democratic Republic of the Congo (10,369 new cases in 2004), Angola, Sudan, Republic of Congo, and Central African Republic.38 T. b. rhodesiense was the cause for the remaining HAT cases found in sub-Saharan Africa, mostly in Malawi, Uganda, and the United Republic of Tanzania.38 Currently, Uganda is the only country with both Gambian and Rhodesian HAT, but to date, each focus of infection is geographically separated.39 Populations in the age group between 15 and 45 years and living in remote rural areas are considered especially vulnerable to both forms of HAT.38 Young children are also at risk of HAT, with cases in Gabon reported.40 Two 10-month-old infants with HAT have been reported, which implies that transplacental infection can occur.41
Following multiplication of the parasites at the infection site, a hemolymphatic stage occurs with waves of parasitemia (stage 1), which is followed by trypanosomes invading the nervous system and causing leukoencephalitis (the meningoencephalitic stage 2).42
Initially the trypanosomes are restricted to cerebral periventricular organs and the choroid plexus, outside the blood-brain barrier (BBB), as well as the dorsal root ganglia in the spinal cord. Later, parasites cross the BBB at postcapillary venules.43 Figure 2 illustrates the diffuse white matter involvement seen on neuroimaging.
The clinical course is different for the 2 forms of African trypanosomiasis; the West African disease is more indolent compared with the East African disease, which follows a more acute progression (Fig. 3). Both have 2 distinct phases after a chancre stage at the site of inoculation. The early, or hemolymphatic, stage consists of fever and lymphadenopathy. West African disease can be asymptomatic for several years before progressing to the second, or encephalitic, stage. East African disease is typically more rapid, progressing over several weeks to a spectrum of neurologic symptoms including headache, personality changes, daytime somnolence, and sensory, motor, and psychiatric disorders. This also includes the characteristic sleep disturbances that the disease is known for and progressive stupor.44
Figure 3.
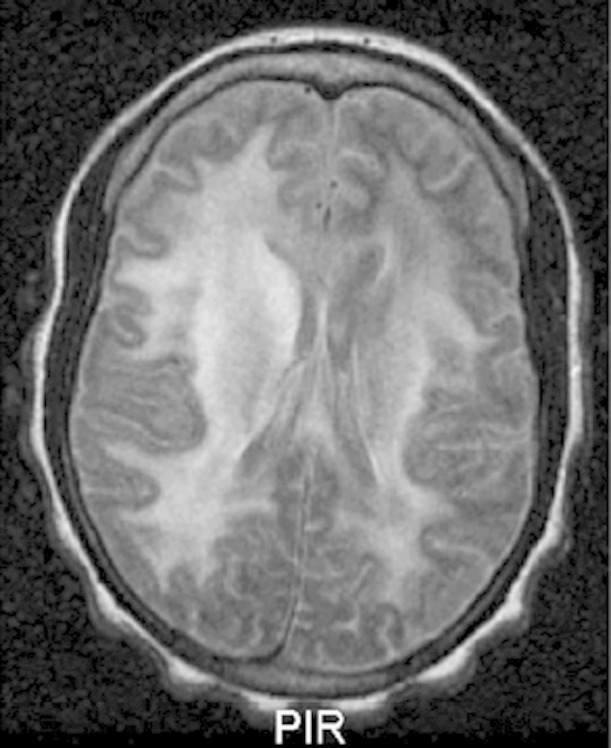
A 27-year-old patient with HAT demonstrating extensive white matter involvement.49
Diagnosis is confirmed by direct observation of intracellular trypomastigotes in serum or cerebrospinal fluid (CSF). Serum antibody detection tests are sensitive and specific for both acute and chronic forms of Trypanosoma brucei infections.45 It is not clear whether HIV infection alters the epidemiology or clinical course of either type of HAT. Reports are conflicting. In a rural Congolese hospital, among 18 patients treated with melarsoprol, 3 of the 4 HIV-positive individuals developed encephalopathy and died, whereas all the 14 HIV-negative patients recovered.46 However, another study in Côte d’Ivoire found no difference in clinical presentation and response to treatment in HAT patients with and without HIV.47
HAT is invariably lethal if left untreated. Suramin and pentamidine, although effective for stage 1 disease, penetrate the BBB poorly and are therefore ineffective at stage 2 disease. For the late encephalitic stage of HAT, the treatment of choice is arsenic compounds, such as melarsoprol, which are associated with severe and even lethal side effects. These agents are still widely used in Africa. There is also an increase in melarsoprol-refractory HAT cases.42 The alternative treatment is dl-α-difluoromethylornithine, which is only effective against the West African form of HAT, requires daily intravenous injection, has adverse effects, is expensive, and is not readily available.
There is no vaccine, or drug, for a prophylaxis against HAT. Control of African trypanosomiasis requires 2 strategic approaches: reducing the disease reservoir and controlling the tsetse fly vector. Humans are the main disease reservoir for T. b. gambiense, therefore the main control strategy for this subspecies is active case finding through population screening, followed by treatment of the infected persons when identified. Tsetse fly traps are sometimes used as an adjunct. Reducing the reservoir of infection for T. b. Rhodesiense on the contrary is more difficult, as there are a variety of animal hosts. Vector control is the primary strategy in use. This is usually done with traps or screens, in combination with insecticides and odors that attract the flies.48
Toxoplasmosis
Toxoplasmosis is a parasitic infection caused by the protozoan Toxoplasma gondii. It is widely distributed throughout the world, and it is known to cause infection in all warm-blooded animals, including humans. It is estimated that globally one-third of the human population is chronically infected with T. Gondii. In Africa, childhood toxoplasmosis is usually through congenital infections. The prevalence of toxoplasmosis varies by geographic location based on several factors including climate, agricultural practices, eating habits, feline population density, and socioeconomic status.49 There are few studies on the prevalence of toxoplasmosis in Africa. However, 1 study showed that To. gondii is widespread in Mali, and elsewhere in West Africa, in both urban and rural areas, and that rising seroprevalence in women of childbearing age indicates a significant risk of congenital disease.50
In children with HIV infection, toxoplasmosis is most often due to the reactivation of latent infection. One-third of HIV-infected people with serum antitoxoplasma IgG antibodies develop toxoplasma encephalitis.51,52 The incidence of toxoplasma encephalitis is reduced among HIV-infected people receiving trimethoprim-sulfamethoxazole or dapsone-pyrimethamine therapy as a prophylaxis against Pneumocystis carinii pneumonia.53
The severity of congenital toxoplasmosis is influenced largely by the timing of maternal infection, especially later in the pregnancy.54,55 Ocular disease, mainly chorioretinitis, mild or severe congenital neurologic defects, learning disabilities, or a combination occur.50,54,55 Learning difficulties develop with advancing age owing to recrudescence of bradyzoite cysts.56,57 In older children, toxoplasmosis typically presents as a subclinical infection. In the immunocompromised individuals, clinical manifestations of CNS toxoplasmosis typically include headache, altered mental status, seizures, focal neurologic deficits, hemiparesis, ataxia, and cranial nerve palsies.58,59
Although uncommon, toxoplasmosis of the spinal cord is reported in HIV-infected patients although very rare in HIV-negative individuals.60,61
Definitive diagnosis is made when tachyzoites are identified in biopsy samples. However, identification of anti–To. gondii antibodies by enzyme-linked immunosorbent assay is both sensitive and specific for the diagnosis. Polymerase chain reaction assay of CSF is highly specific and sensitive in some laboratories. Analysis is challenging even in resource-equipped settings and very limited in most parts of Africa.62 On neuroimaging, the existence of multiple ring-enhancing lesions in the basal ganglia or cerebrum, especially in the presence of antitoxoplasma IgG antibodies, suggests the presence of CNS toxoplasmosis and is sufficient to start presumptive treatment for CNS toxoplasmosis.
In resource-limited countries, such as sub-Saharan Africa, at present, the treatment of toxoplasmosis is usually initiated on presumptive diagnosis in at-risk groups such as HIV-positive individuals, and the clinical diagnosis is made because of clinical (and where possible, radiologic) response to specific therapy. This is owing to the unavailability of resources to make the radiologic and serologic confirmation of the infection.63
There is treatment available for acute infection. However, no drugs are known to be effective against these latent forms of toxoplasmosis.
Immunocompromised individuals are particularly at risk of death from primary or recrudescent infection. Drugs for the treatment of CNS toxoplasmosis should include pyrimethamine, sulfadiazine, and folinic acid.64
Schistosomiasis (Bilharzia)
The worldwide prevalence of CNS schistosomiasis has a marked variability (0.3%-30%).65,66 In endemic areas such as Malawi, schistosomiasis is a frequent cause of nontraumatic myelopathies (6%).67 Neuroschistosomiasis is probably the most severe clinical form of the schistosome infection.68–71
From case studies, there is a suggestion that neurologic complications early in the course of infection are due to egg deposition, and this follows the migration of adult worms to the brain or spinal cord. Granuloma formation follows with thousands of eggs deposited. This is the hallmark of neuroschistosomiasis.70,71
Schistosomiasis infection of the CNS includes signs and symptoms of increased intracranial pressure, myelopathy, and radiculopathy.68–71 Complications of intracerebral disease may include headache, visual disturbances, delirium, seizures, motor deficit, ataxia, and encephalopathy. Features of acute transverse myelitis and subacute myeloradiculopathy of the lumbosacral region are probably the most commonly reported neurologic manifestations of both Schistosoma mansoni and Schistosoma haematobium infection. However, acute encephalitis following involvement of the cortex, subcortical white matter, basal ganglia, or internal capsule is the usual presentation in infection by Schistosoma japonicum.70,71
In HIV-infected individuals, schistosomiasis induces less granuloma formation around the egg. The few cases of CNS schistosomiasis in HIV-infected people suggest that this may predispose to a disseminated, or miliary, form of the infection.72,73
The finding of eggs in the stool, or positive serology result, is supportive but not direct evidence of schistosomiasis of the CNS. A positive diagnostic finding coupled with neuroimaging, and in the context of neurologic symptoms, makes neuroschistosomiasis a likely diagnosis. Definitive diagnosis requires histopathologic study at biopsy when there is schistosome eggs and granulomas.64 Radiologic and histopathologic diagnoses are unavailable in most African settings making the management of neuroschistosomiasis a challenge.
Praziquantel is the effective treatment for all Schistosoma species, and is curative in 60%-90% of cases.74 Artemether, unlike praziquantel, is more effective against immature migrating larvae (schistosomula), and in combination with praziquantel has synergistic properties.75 When praziquantel is ineffective, oxamniquine may be used for treatment.76
The control of schistosomiasis is mostly based on large-scale treatment of at-risk population groups, access to safe water, improved sanitation, hygiene education, and snail control.
To reduce disease burden, periodic treatment of at-risk populations is recommended, as this cures mild symptoms, prevents infected people from developing severe, late-stage chronic disease, and also stops the infection spreading to others. A major limitation to schistosomiasis control is access to praziquantel, with only 10% of affected people receiving treatment in 2011.77
Miscellaneous Parasitic Infections of the CNS
Naegleria fowleri (Primary Amebic Meningoencephalitis)
Primary amebic meningoencephalitis (PAM) is caused by N. fowleri. It is commonly referred to as “brain-eating ameba.” This is a free-living single-celled organism which is present throughout the world.78 Most infections occur in children and young adults who play or dive in bodies of stagnant freshwater.79 Less than 100 cases are reported worldwide. Most likely this reflects underreporting.
The infection is almost invariably fatal, with mortality approaching 95%, which usually occurs within 72 hours of onset of symptoms.80 Early recognition of infection can result in effective treatment for a few patients.81
Signs of meningitis are common, and some patients present with seizures or coma. Differentiation between PAM and bacterial meningitis can be difficult, particularly in sub-Saharan African, hence the underreporting. Diagnosis is by polymerase chain reaction analysis, but this is unavailable in most African settings where the disease occurs.82
Neuroimaging is usually normal at onset; however, severe edema may be present in some patients.83 Autopsy findings are usually localized to the posterior fossa and brain stem.64,84 Treatment is with intrathecal amphotericin B.85
Neurologic Complications of Paragonimus Infections
This is the only lung fluke that is capable of infecting humans. An estimated 20 million people are infected worldwide, with 10 million in China alone.86 The “oriental lung fluke,” Paragonimiasis westermani, is endemic throughout Asia and Western Africa. Meningoencephalitis is the most common CNS complication and may persist for 6-8 weeks. Symptoms during chronic CNS infection are often vague and may include headache, weakness, or nausea. Other CNS complications include transverse myelitis and myelopathy.87 Seizures are usually present in patients with more extensive CNS involvement. Untreated CNS disease carries a mortality rate of almost 5%.88 Definitive diagnosis of CNS involvement requires demonstration of eggs in CSF or brain biopsy material, and this causes diagnostic challenges in African settings.89 Plain skull radiographs can be used, and they are often dramatic, demonstrating a characteristic “soap-bubble” appearance.90 The treatment of choice for paragonimiasis is Praziquantel.91
Conclusion and Future Directions
Although parasitic infections of the CNS seem to be infections of resource-limited countries, with the increasing amount of international travel, all travelers to endemic regions are potentially at risk, with such infections becoming increasingly prevalent throughout the world. With the advent of increasing global travel, more potent immunosuppression, and HIV infection, parasitic and viral CNS infections will likely become even more commonplace. Basic familiarity with common pathogens can make diagnosis more expeditious and efficient. For the clinician confronted with a patient with suspected parasitic infection, additional assistance with diagnostic evaluation and therapy can be obtained at the following Web sites www.cdp.cdc.gov/dpdx/and www.who.int/inffs/en/index.html.
References
- 1.KindhauserMK (ed): World Health Organisation. Global defense against the infectious disease threat. Communicable Diseases, 2003. Available at: http://whqlibdoc.who.int/publications/2003/9241590297.pdf. Accessed February 2014.
- 2.Hotez P., Raff S., Fenwick A. Recent progress in integrated neglected tropical disease control. Trends Parasitol. 2007;23(11):511–514. doi: 10.1016/j.pt.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organisation. World Malaria Report 2009, 2009. Available at: http://whqlibdoc.who.int/publications/2009/9789241563901_eng.pdf. Accessed February 2014.
- 4.White N.J., Pukrittayakamee S., Hien T.T. Malaria. Lancet. 2013 doi: 10.1016/S0140-6736(13)60024-0. [DOI] [PubMed] [Google Scholar]
- 5.Mmbando B.P., Vestergaard L.S., Kitua A.Y. A progressive declining in the burden of malaria in north-eastern Tanzania. Malar J. 2010;9:216. doi: 10.1186/1475-2875-9-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Meara W.P., Bejon P., Mwangi T.W. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet. 2008;372(9649):1555–1562. doi: 10.1016/S0140-6736(08)61655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chizema-Kawesha E., Miller J.M., Steketee R.W. Scaling up malaria control in Zambia: Progress and impact 2005-2008. Am J Trop Med Hyg. 2010;83(3):480–488. doi: 10.4269/ajtmh.2010.10-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parham P.E., Michael E. Modelling climate change and malaria transmission. Adv Exp Med Biol. 2010;673:184–199. doi: 10.1007/978-1-4419-6064-1_13. [DOI] [PubMed] [Google Scholar]
- 9.Taylor T.E., Fu W.J., Carr R.A. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat Med. 2004;10(2):143–145. doi: 10.1038/nm986. [DOI] [PubMed] [Google Scholar]
- 10.Newton C.R., Warrell D.A. Neurological manifestations of falciparum malaria. Ann Neurol. 1998;43(6):695–702. doi: 10.1002/ana.410430603. [DOI] [PubMed] [Google Scholar]
- 11.Newton C.R., Hien T.T., White N. Cerebral malaria. J Neurol Neurosurg Psychiatry. 2000;69(4):433–441. doi: 10.1136/jnnp.69.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewallen S., Harding S.P., Ajewole J. A review of the spectrum of clinical ocular fundus findings in P. falciparum malaria in African children with a proposed classification and grading system. Trans R Soc Trop Med Hyg. 1999;93(6):619–622. doi: 10.1016/s0035-9203(99)90071-8. [DOI] [PubMed] [Google Scholar]
- 13.Beare N.A., Taylor T.E., Harding S.P. Malarial retinopathy: A newly established diagnostic sign in severe malaria. Am J Trop Med Hyg. 2006;75(5):790–797. [PMC free article] [PubMed] [Google Scholar]
- 14.Flateau C., Le Loup G., Pialoux G. Consequences of HIV infection on malaria and therapeutic implications: A systematic review. Lancet Infect Dis. 2011;11(7):541–556. doi: 10.1016/S1473-3099(11)70031-7. [DOI] [PubMed] [Google Scholar]
- 15.Hochman S., Kim K. The impact of HIV and malaria coinfection: What is known and suggested venues for further study. Interdiscip Perspect Infect Dis. 2009;2009:617954. doi: 10.1155/2009/617954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mallewa M., Fooks A.R., Banda D. Rabies encephalitis in malaria-endemic area, Malawi, Africa. Emerg Infect Dis. 2007;13(1):136–139. doi: 10.3201/eid1301.060810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mallewa M., Faragher B., Banda D. Viral CNS infections in children from a malaria-endemic area of Malawi: A prospective cohort study. Lancet Global Health. 2013;1(3):e153–e160. doi: 10.1016/S2214-109X(13)70060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organisation. Guidelines for the Treatment of Malaria (ed 2), 2010. Available at: http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf?ua=1. Accessed February 2014.
- 19.Dondorp A.M., Nosten F., Yi P. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361(5):455–467. doi: 10.1056/NEJMoa0808859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roman G., Sotelo J., Del Brutto O. A proposal to declare neurocysticercosis an international reportable disease. Bull World Health Organ. 2000;78(3):399–406. [PMC free article] [PubMed] [Google Scholar]
- 21.Grill J., Pillet P., Rakotomalala W. Neurocysticercosis: Pediatric aspects. Arch Pediatr. 1996;3(4):360–368. doi: 10.1016/0929-693x(96)84693-8. [DOI] [PubMed] [Google Scholar]
- 22.Quet F., Guerchet M., Pion S.D. Meta-analysis of the association between cysticercosis and epilepsy in Africa. Epilepsia. 2010;51(5):830–837. doi: 10.1111/j.1528-1167.2009.02401.x. [DOI] [PubMed] [Google Scholar]
- 23.Winkler A.S., Blocher J., Auer H. Epilepsy and neurocysticercosis in rural Tanzania—An imaging study. Epilepsia. 2009;50(5):987–993. doi: 10.1111/j.1528-1167.2008.01867.x. [DOI] [PubMed] [Google Scholar]
- 24.Arseni C., Cristescu A. Epilepsy due to cerebral cysticercosis. Epilepsia. 1972;13(2):253–258. doi: 10.1111/j.1528-1157.1972.tb05259.x. [DOI] [PubMed] [Google Scholar]
- 25.Medina M.T., Rosas E., Rubio-Donnadieu F. Neurocysticercosis as the main cause of late-onset epilepsy in Mexico. Arch Intern Med. 1990;150(2):325–327. [PubMed] [Google Scholar]
- 26.Chayasirisobhon S., Menoni R., Chayasirisobhon W. Correlation of electroencephalography and the active and inactive forms of neurocysticercosis. Clin Electroencephalogr. 1999;30(1):9–11. doi: 10.1177/155005949903000106. [DOI] [PubMed] [Google Scholar]
- 27.Forlenza O.V., Filho A.H., Nobrega J.P. Psychiatric manifestations of neurocysticercosis: A study of 38 patients from a neurology clinic in Brazil. J Neurol Neurosurg Psychiatry. 1997;62(6):612–616. doi: 10.1136/jnnp.62.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia H.H., Del Brutto O.H., Nash T.E. New concepts in the diagnosis and management of neurocysticercosis (Taenia solium) Am J Trop Med Hyg. 2005;72(1):3–9. [PubMed] [Google Scholar]
- 29.Carpio A. Diagnostic criteria for human cysticercosis. J Neurol Sci. 1998;161(2):185–188. doi: 10.1016/s0022-510x(98)00227-5. [DOI] [PubMed] [Google Scholar]
- 30.Serpa J.A., Yancey L.S., White A.C., Jr. Advances in the diagnosis and management of neurocysticercosis. Expert Rev Anti Infect Ther. 2006;4(6):1051–1061. doi: 10.1586/14787210.4.6.1051. [DOI] [PubMed] [Google Scholar]
- 31.Almeida C.R., Ojopi E.P., Nunes C.M. Taenia solium DNA is present in the cerebrospinal fluid of neurocysticercosis patients and can be used for diagnosis. Eur Arch Psychiatry Clin Neurosci. 2006;256(5):307–310. doi: 10.1007/s00406-006-0612-3. [DOI] [PubMed] [Google Scholar]
- 32.Thornton C.A., Houston S., Latif A.S. Neurocysticercosis and human immunodeficiency virus infection. A possible association. Arch Neurol. 1992;49(9):963–965. doi: 10.1001/archneur.1992.00530330087021. [DOI] [PubMed] [Google Scholar]
- 33.Soto Hernandez J.L., Ostrosky Zeichner L., Tavera G. Neurocysticercosis and HIV infection: Report of two cases and review. Surg Neurol. 1996;45(1):57–61. doi: 10.1016/0090-3019(95)00259-6. [DOI] [PubMed] [Google Scholar]
- 34.Delobel P., Signate A., El Guedj M. Unusual form of neurocysticercosis associated with HIV infection. Eur J Neurol. 2004;11(1):55–58. doi: 10.1046/j.1351-5101.2003.00696.x. [DOI] [PubMed] [Google Scholar]
- 35.Sotelo J., del Brutto O.H., Penagos P. Comparison of therapeutic regimen of anticysticercal drugs for parenchymal brain cysticercosis. J Neurol. 1990;237(2):69–72. doi: 10.1007/BF00314663. [DOI] [PubMed] [Google Scholar]
- 36.Proano J.V., Madrazo I., Avelar F. Medical treatment for neurocysticercosis characterized by giant subarachnoid cysts. N Engl J Med. 2001;345(12):879–885. doi: 10.1056/NEJMoa010212. [DOI] [PubMed] [Google Scholar]
- 37.Winkler A.S., Willingham A.L., 3rd, Sikasunge C.S. Epilepsy and neurocysticercosis in sub-Saharan Africa. Wien Klin Wochenschr. 2009;121(suppl 3):3–12. doi: 10.1007/s00508-009-1242-3. [DOI] [PubMed] [Google Scholar]
- 38.Simarro P., Diarra A., Ruiz Postigo J. The Human African Trypanosomiasis Control and Surveillance Programme of the World Health Organization 2000-2009: The way forward. PLoS Negl Trop Dis. 2011;5(2):e1007. doi: 10.1371/journal.pntd.0001007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fevre E.M., Picozzi K., Fyfe J. A burgeoning epidemic of sleeping sickness in Uganda. Lancet. 2005;366(9487):745–747. doi: 10.1016/S0140-6736(05)67179-6. [DOI] [PubMed] [Google Scholar]
- 40.Koko J., Ategbo S.J., Gahouma D. Human African trypanosomiasis: Report of three cases. Arch Pediatr. 2013;20(8):871–873. doi: 10.1016/j.arcped.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 41.Traub N., Hira P.R., Chintu C. Congenital trypanosomiasis: Report of a case due to Trypanosoma brucei rhodesiense. East Afr Med J. 1978;55(10):477. [PubMed] [Google Scholar]
- 42.Brun R., Schumacher R., Schmid C. The phenomenon of treatment failures in human African trypanosomiasis. Trop Med Int Health. 2001;6(11):906–914. doi: 10.1046/j.1365-3156.2001.00775.x. [DOI] [PubMed] [Google Scholar]
- 43.Kristensson K., Nygard M., Bertini G. African trypanosome infections of the nervous system: Parasite entry and effects on sleep and synaptic functions. Prog Neurobiol. 2010;91(2):152–171. doi: 10.1016/j.pneurobio.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 44.Kennedy P.G. Human African trypanosomiasis of the CNS: Current issues and challenges. J Clin Invest. 2004;113(4):496–504. doi: 10.1172/JCI21052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cattand P., de Raadt P. Laboratory diagnosis of trypanosomiasis. Clin Lab Med. 1991;11(4):899–908. [PubMed] [Google Scholar]
- 46.Blum J., Nkunku S., Burri C. Clinical description of encephalopathic syndromes and risk factors for their occurrence and outcome during melarsoprol treatment of human African trypanosomiasis. Trop Med Int Health. 2001;6(5):390–400. doi: 10.1046/j.1365-3156.2001.00710.x. [DOI] [PubMed] [Google Scholar]
- 47.Meda H.A., Doua F., Laveissiere C. Human immunodeficiency virus infection and human African trypanosomiasis: A case-control study in Cote d’Ivoire. Trans R Soc Trop Med Hyg. 1995;89(6):639–643. doi: 10.1016/0035-9203(95)90425-5. [DOI] [PubMed] [Google Scholar]
- 48.Brun R., Blum J., Chappuis F. Human African trypanosomiasis. Lancet. 2010;375(9709):148–159. doi: 10.1016/S0140-6736(09)60829-1. [DOI] [PubMed] [Google Scholar]
- 49.Feldman H.A. Toxoplasmosis. N Engl J Med. 1968;279(25):1370–1375. doi: 10.1056/NEJM196812192792505. [contd] [DOI] [PubMed] [Google Scholar]
- 50.Ouologuem D.T., Djimde A.A., Diallo N. Toxoplasma gondii seroprevalence in Mali. J Parasitol. 2013;99(2):371–374. doi: 10.1645/GE-3239.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Porter S.B., Sande M.A. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992;327(23):1643–1648. doi: 10.1056/NEJM199212033272306. [DOI] [PubMed] [Google Scholar]
- 52.Luft B.J., Remington J.S. AIDS commentary. Toxoplasmic encephalitis. J Infect Dis. 1988;157(1):1–6. doi: 10.1093/infdis/157.1.1. [DOI] [PubMed] [Google Scholar]
- 53.Edge M.D., Rimland D. Community-acquired bacteremia in HIV-positive patients: Protective benefit of co-trimoxazole. AIDS. 1996;10(14):1635–1639. doi: 10.1097/00002030-199612000-00007. [DOI] [PubMed] [Google Scholar]
- 54.Desmonts G., Couvreur J. Toxoplasmosis in pregnancy and its transmission to the fetus. Bull N Y Acad Med. 1974;50(2):146–159. [PMC free article] [PubMed] [Google Scholar]
- 55.Dunn D., Wallon M., Peyron F. Mother-to-child transmission of toxoplasmosis: Risk estimates for clinical counselling. Lancet. 1999;353(9167):1829–1833. doi: 10.1016/S0140-6736(98)08220-8. [DOI] [PubMed] [Google Scholar]
- 56.Holland G.N. Ocular toxoplasmosis: The influence of patient age. Mem Inst Oswaldo Cruz. 2009;104(2):351–357. doi: 10.1590/s0074-02762009000200031. [DOI] [PubMed] [Google Scholar]
- 57.Melamed J. Contributions to the history of ocular toxoplasmosis in Southern Brazil. Mem Inst Oswaldo Cruz. 2009;104(2):358–363. doi: 10.1590/s0074-02762009000200032. [DOI] [PubMed] [Google Scholar]
- 58.Conti D.J., Rubin R.H. Infection of the central nervous system in organ transplant recipients. Neurol Clin. 1988;6(2):241–260. [PubMed] [Google Scholar]
- 59.Patchell R.A. Neurological complications of organ transplantation. Ann Neurol. 1994;36(5):688–703. doi: 10.1002/ana.410360503. [DOI] [PubMed] [Google Scholar]
- 60.Straathof C.S., Kortbeek L.M., Roerdink H. A solitary spinal cord toxoplasma lesion after peripheral stem-cell transplantation. J Neurol. 2001;248(9):814–815. doi: 10.1007/s004150170101. [DOI] [PubMed] [Google Scholar]
- 61.Vyas R., Ebright J.R. Toxoplasmosis of the spinal cord in a patient with AIDS: Case report and review. Clin Infect Dis. 1996;23(5):1061–1065. doi: 10.1093/clinids/23.5.1061. [DOI] [PubMed] [Google Scholar]
- 62.Joseph P., Calderon M.M., Gilman R.H. Optimization and evaluation of a PCR assay for detecting toxoplasmic encephalitis in patients with AIDS. J Clin Microbiol. 2002;40(12):4499–4503. doi: 10.1128/JCM.40.12.4499-4503.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Luft B.J., Remington J.S. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15(2):211–222. doi: 10.1093/clinids/15.2.211. [DOI] [PubMed] [Google Scholar]
- 64.Walker M., Zunt J.R. Parasitic central nervous system infections in immunocompromised hosts. Clin Infect Dis. 2005;40(7):1005–1015. doi: 10.1086/428621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vidal C.H., Gurgel F.V., Ferreira M.L. Epidemiological aspects in neuroschistosomiasis. Arq Neuropsiquiatr. 2010;68(1):72–75. doi: 10.1590/s0004-282x2010000100016. [DOI] [PubMed] [Google Scholar]
- 66.Ferrari T.C. A laboratory test for the diagnosis of neuroschistosomiasis. Neurol Res. 2010;32(3):252–262. doi: 10.1179/016164110X12644252260718. [DOI] [PubMed] [Google Scholar]
- 67.Naus C.W., Chipwete J., Visser L.G. The contribution made by Schistosoma infection to non-traumatic disorders of the spinal cord in Malawi. Ann Trop Med Parasitol. 2003;97(7):711–721. doi: 10.1179/000349803225002363. [DOI] [PubMed] [Google Scholar]
- 68.Ross A.G., Bartley P.B., Sleigh A.C. Schistosomiasis. N Engl J Med. 2002;346(16):1212–1220. doi: 10.1056/NEJMra012396. [DOI] [PubMed] [Google Scholar]
- 69.Ferrari T.C. Involvement of central nervous system in the schistosomiasis. Mem Inst Oswaldo Cruz. 2004;99(5 suppl 1):59–62. doi: 10.1590/s0074-02762004000900010. [DOI] [PubMed] [Google Scholar]
- 70.Gryseels B., Polman K., Clerinx J. Human schistosomiasis. Lancet. 2006;368(9541):1106–1118. doi: 10.1016/S0140-6736(06)69440-3. [DOI] [PubMed] [Google Scholar]
- 71.Carod-Artal F.J. Neurological complications of Schistosoma infection. Trans R Soc Trop Med Hyg. 2008;102(2):107–116. doi: 10.1016/j.trstmh.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 72.Livramento J.A., Machado L.R., Spina-Franca A. Cerebrospinal fluid abnormalities in 170 cases of AIDS. Arq Neuropsiquiatr. 1989;47(3):326–331. doi: 10.1590/s0004-282x1989000300013. [DOI] [PubMed] [Google Scholar]
- 73.Nobre V., Braga E., Rayes A. Opportunistic infections in patients with AIDS admitted to an university hospital of the Southeast of Brazil. Rev Inst Med Trop Sao Paulo. 2003;45(2):69–74. doi: 10.1590/s0036-46652003000200003. [DOI] [PubMed] [Google Scholar]
- 74.Kardaman M.W., Amin M.A., Fenwick A. A field trial using praziquantel (BiltricideR) to treat Schistosoma mansoni and Schistosoma haematobium infection in Gezira, Sudan. Ann Trop Med Parasitol. 1983;77(3):297–304. doi: 10.1080/00034983.1983.11811711. [DOI] [PubMed] [Google Scholar]
- 75.Xiao S., Tanner M., N’Goran E.K. Recent investigations of artemether, a novel agent for the prevention of schistosomiasis japonica, mansoni and haematobia. Acta Trop. 2002;82(2):175–181. doi: 10.1016/s0001-706x(02)00009-8. [DOI] [PubMed] [Google Scholar]
- 76.Ferrari M.L., Coelho P.M., Antunes C.M. Efficacy of oxamniquine and praziquantel in the treatment of Schistosoma mansoni infection: A controlled trial. Bull World Health Organ. 2003;81(3):190–196. [PMC free article] [PubMed] [Google Scholar]
- 77.World Health Organisation. Schistosomiasis. Fact sheet N°115, 2013. Available at: http://www.who.int/mediacentre/factsheets/fs115/en/. Accessed February 2014.
- 78.Parija S.C., Jayakeerthee S.R. Naegleria fowleri: A free living amoeba of emerging medical importance. J Commun Dis. 1999;31(3):153–159. [PubMed] [Google Scholar]
- 79.Gyori E. December 2002: 19-year old male with febrile illness after jet ski accident. Brain Pathol. 2003;13(2):237–239. [PubMed] [Google Scholar]
- 80.Jain R., Prabhakar S., Modi M. Naegleria meningitis: A rare survival. Neurol India. 2002;50(4):470–472. [PubMed] [Google Scholar]
- 81.Barnett N.D., Kaplan A.M., Hopkin R.J. Primary amoebic meningoencephalitis with Naegleria fowleri: Clinical review. Pediatr Neurol. 1996;15(3):230–234. doi: 10.1016/s0887-8994(96)00173-7. [DOI] [PubMed] [Google Scholar]
- 82.Reveiller F.L., Cabanes P.A., Marciano-Cabral F. Development of a nested PCR assay to detect the pathogenic free-living amoeba Naegleria fowleri. Parasitol Res. 2002;88(5):443–450. doi: 10.1007/s00436-002-0591-x. [DOI] [PubMed] [Google Scholar]
- 83.Schumacher D.J., Tien R.D., Lane K. Neuroimaging findings in rare amebic infections of the central nervous system. Am J Neuroradiol. 1995;16(suppl 4):930–935. [PMC free article] [PubMed] [Google Scholar]
- 84.Ferrante A. Free-living amoebae: Pathogenicity and immunity. Parasite Immunol. 1991;13(1):31–47. doi: 10.1111/j.1365-3024.1991.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 85.Loschiavo F., Ventura-Spagnolo T., Sessa E. Acute primary meningoencephalitis from entamoeba Naegleria Fowleri. Report of a clinical case with a favourable outcome. Acta Neurol (Napoli) 1993;15(5):333–340. [PubMed] [Google Scholar]
- 86.Blair D., Xu Z.B., Agatsuma T. Paragonimiasis and the genus Paragonimus. Adv Parasitol. 1999;42:113–222. doi: 10.1016/s0065-308x(08)60149-9. [DOI] [PubMed] [Google Scholar]
- 87.Oh S.J. Cerebral and spinal paragonimiasis. A histopathological study. J Neurol Sci. 1969;9(2):205–236. doi: 10.1016/0022-510x(69)90072-0. [DOI] [PubMed] [Google Scholar]
- 88.Kang S.Y., Kim T.K., Kim T.Y. A case of chronic cerebral Paragonimiasis westermani. Korean J Parasitol. 2000;38(3):167–171. doi: 10.3347/kjp.2000.38.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kim T.Y., Joo I.J., Kang S.Y. Recombinant Paragonimus westermani yolk ferritin is a useful serodiagnostic antigen. J Infect Dis. 2002;185(9):1373–1375. doi: 10.1086/339880. [DOI] [PubMed] [Google Scholar]
- 90.Oh S.J. Paragonimus meningitis. J Neurol Sci. 1968;6(3):419–433. doi: 10.1016/0022-510x(68)90028-2. [DOI] [PubMed] [Google Scholar]
- 91.Katz N., Zicker F., Chaves A. Clinical trials with pyrantel pamoate in intestinal parasitoses. Rev Inst Med Trop Sao Paulo. 1972;14(3):212–221. [PubMed] [Google Scholar]
- 92.Newton C.R., Chokwe T., Schellenberg J.A. Coma scales for children with severe falciparum malaria. Trans R Soc Trop Med Hyg. 1997;91(2):161–165. doi: 10.1016/s0035-9203(97)90207-8. [DOI] [PubMed] [Google Scholar]