Abstract
Adults with sickle cell disease(SCD) are a growing population. Recent national estimates of outcomes in acute chest syndrome(ACS) among adults with SCD are lacking. We describe the incidence, outcomes and predictors of mortality in ACS in adults. We hypothesize that any need for mechanical ventilation is an independent predictor of mortality.
Methods
We performed a retrospective analysis of the Nationwide Inpatient Sample(2004–2010),the largest all payer inpatient database in United States, to estimate the incidence and outcomes of ACS needing mechanical ventilation(MV) and exchange transfusion(ET) in patients >21 years. The effects of MV and ET on outcomes including length of stay(LOS) and in-hospital mortality(IHM) were examined using multivariable linear and logistic regression models respectively. The effects of age, sex, race, type of sickle cell crisis, race, co-morbid burden, insurance status, type of admission, and hospital characteristics were adjusted in the regression models.
Results
Of the 24,699 hospitalizations, 4.6% needed MV(2.7% for <96 hours, 1.9% for ≥96 hours), 6% had ET, with a mean length of stay(LOS) of 7.8 days and an in-hospital mortality rate(IHM) of 1.6%. There was a gradual yearly increase in ACS hospitalizations that needed MV(2.6% in 2004 to 5.8% in 2010). Hb-SS disease was the phenotype in 84.3% of all hospitalizations. After adjusting for a multitude of patient and hospital related factors, patients who had MV for <96 hours(OR = 67.53,p<0.01) or those who had MV for ≥96 hours(OR = 8.73,p<0.01) were associated with a significantly higher odds for IHM when compared to their counterparts. Patients who had MV for ≥96 hours and those who had ET had a significantly longer LOS in-hospitals(p<0.001).
Conclusion
In this large cohort of hospitalized adults with SCD patients with ACS, the need for mechanical ventilation predicted higher mortality rates and increased hospital resource utilization. Identification of risk factors may enable optimization of outcomes.
Introduction
Survival of children with sickle cell disease well into adulthood is commonplace in the current era, and due, at least in part, to advances in comprehensive care of these patients [1]. In fact, a landmark study performed nearly 20 years ago indicated that approximately 50 percent of patients with sickle cell disease survived beyond the fifth decade of life [2]. Acute chest syndrome is a major complication of sickle cell disease and a significant cause of morbidity and mortality in these patients [2], [3], [4]. Approximately 50 percent of patients with sickle cell disease will have an episode of acute chest syndrome during their lifetime [5], and mortality related to these episodes is four times higher in adults compared to children [5], [6].
A recent study of the effect of hospital type and provider specialty on outcomes of hospitalized adolescents and young adults (16–25 years) with sickle cell disease and acute chest syndrome found that general hospitals carry higher intubation risks for adolescents and young adults with sickle cell disease and acute chest syndrome compared with children's hospitals [7]. The impact of the need for mechanical ventilation on outcomes in adult patients with sickle cell disease and respiratory failure due to acute chest syndrome is unknown.
Although, there are no randomized trials demonstrating the optimal treatment of acute chest syndrome in adults with sickle cell disease, transfusion therapy- especially exchange transfusion- has remained the cornerstone of management in moderate to severe cases of acute chest syndrome in several centers [8], [9]. National estimates of exchange transfusion usage and its impact on outcomes, such as in-hospital mortality and length of stay, are largely unknown. Patient and hospital level predictors of mortality in acute chest syndrome in sickle cell disease adult patients are also lacking. As such, identification of risk factors can help assess prognosis and devise preventive strategies to optimize outcomes.
The objective of our study is to estimate the incidence and outcomes of acute chest syndrome needing mechanical ventilation and exchange transfusion in adult patients (>21 years of age) with sickle cell crisis. We hypothesize that the need for mechanical ventilation predicts higher mortality in these patients.
Materials and Methods
Design and description of the database
We performed a retrospective analysis of the Nationwide Inpatient Sample (NIS) for the years 2004 to 2010. The NIS is the largest inpatient all-payer hospital discharge database in the United States that is a part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ) [10]. The Nationwide Inpatient Sample contains data of all nonfederal acute-care general hospitals in the United States and has information on a multitude of patient and hospital level variables including age, gender, race, reason for hospitalization, secondary diagnoses, procedures performed during hospitalization, length of stay in-hospital, hospital charges, type of admission, insurance status, and hospital level variables (teaching status, bed size, and geographic location).
Data user agreement
The first author (VJA) completed the data user agreement with HCUP-AHRQ and obtained the patient/hospital de-identified data. As per University Hospitals Case Medical Center institutional review board (IRB) and in agreement with Federal Regulations 45 CFR 46.101 (b) which states “research involving the collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, if these sources are publicly available or if the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects,” such studies are permitted to be classified as research that is “exempt” from IRB full or expedited review. IRB was not consulted for approval since the current study was a retrospective analysis of hospital based discharge dataset that is available publicly for purchase from Agency for Healthcare Research and Quality (AHRQ). The HCUP-AHRQ data user agreement precludes us from reporting individual cell counts ≤10 to preserve patient confidentiality. Consequently, these numbers were not reported in our study.
Selection of cases and outcome variables examined
All adult hospitalizations (age >21 years) with a diagnosis of acute chest syndrome (International Classification of Disease, 9th edition, clinical modification [ICD-9-CM] codes of 517.3) with sickle cell crisis (ICD-9-CM codes of 282.42, 282.62, 282.64, and 282.69) were selected. The NIS dataset has 25 diagnostic fields and we used all these fields to select cases. For several cases, acute chest syndrome is not the primary reason for hospitalization, but develops during the hospitalization. Consequently, both elective and non-elective admissions were selected for analysis. Performance of continuous invasive mechanical ventilation (MV [ICD-9-CM procedure codes of 96.70, 96.71, and 96.72]) and exchange transfusion (ET [procedure code of 99.01]) was obtained for these hospitalizations. Co-morbid burden was estimated by using the NIS-disease severity files. The number of co-morbid conditions was computed for each hospitalization. The types of co-morbid conditions examined included: AIDS, alcohol abuse, deficiency anemias, rhematoid arthritis/collage vascular diseases, chronic blood loss anemia, congestive heart failure, chronic pulmonary disease, coagulopathy, depression, diabetes – uncomplicated, diabetes with chronic complications, drug abuse, hypertension, hypothyroidism, liver disease, lymphoma, fluid and electrolyte disorders, metastatic cancer, neurological disorders, obesity, paralysis, peripheral vascular disorders, psychoses, pulmonary circulation disorders, renal failure, solid tumor without metastasis, peptic ulcer disease, valvular disease, and weight loss. Seasonal variations in outcomes were described using simple descriptive statistics.
Acute chest syndrome hospitalizations needing mechanical ventilation, exchange transfusion and in-hospital mortality were examined yearly for trends (2004 to 2010). The independent variables of interest included a set of factors at both patient level (age, gender, type of admission, insurance status, race/ethnicity, type of sickle cell crisis, and presence of co-morbid conditions) and hospital level (hospital teaching status, bed size, and hospital location). The type of sickle cell crisis examined included Sickle-cell thalassemia with crisis (ICD 9 CM Code 282.42), Hb-SS disease with crisis (282.62), Sickle-cell/HB-C disease with crisis (282.64), and other sickle-cell disease with crisis (282.69).
Analytical approach
The effects of mechanical ventilation and exchange transfusion on outcomes including length of stay (LOS) and in-hospital mortality were examined using multivariable linear and logistic regression models respectively. Since length of stay was skewed, it was log transformed and used as the dependent variable in the regression model. Taylor Linearization Methods was used to estimate the standard errors. In the multivariable logistic regression model for predicting in-hospital mortality, the odds ratios and 95% confidence intervals were computed for each level of independent variable. In both multivariable regression models, the effects of clustering of outcomes within-hospitals were accounted for. The effects of age, sex, type of sickle cell crisis, race, co-morbid burden, insurance status, type of admission, and hospital characteristics were adjusted in the regression models. All statistical analyses were conducted using SAS Version 9.3 (SAS Institute, Cary, NC) and SUDAAN Version 10.0.1 (Research Triangle Park, NC). All statistical tests were two-sided and a p-value of <0.05 was deemed to be statistically significant.
Results
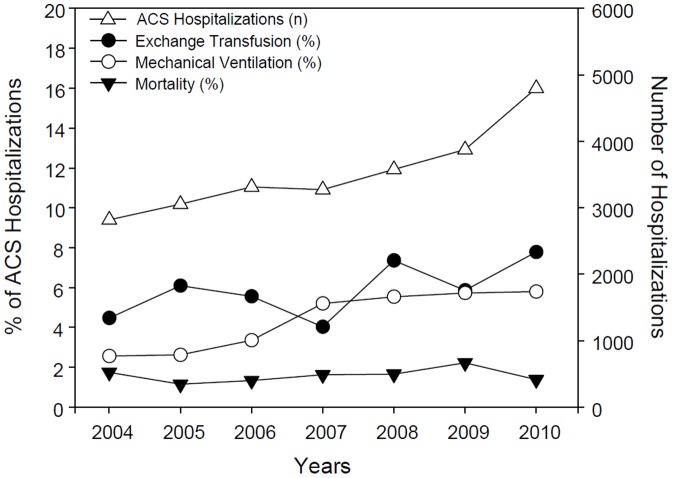
There were a total a total of 24,699 hospitalizations for sickle cell crisis with acute chest syndrome (range is 2,818 hospitalizations in year 2004 to 4,796 hospitalizations in year 2010) See Figure 1. Hb-SS disease was the phenotype in 84.3% of all hospitalizations, while 4.2% had sickle-cell thalassemia, 2.5% had sickle-cell/Hb-C disease, and 9.8% had other forms of sickle-cell disease (Table 1). Close to 2.7% of patients required mechanical ventilation for less than 96 consecutive hours, 1.9% had mechanical ventilation for 96 consecutive hours or more, and 6% had an exchange transfusion. There was a gradual yearly increase in the number of acute chest syndrome hospitalizations that needed mechanical ventilation. Use of exchange transfusions varied on yearly basis with the lowest being in 2007, the year when mechanical ventilation use was higher than exchange transfusions - See figure 1.
Figure 1. Acute Chest Syndrome Hospitalizations and Outcomes per year.
The descriptive figure shows the number of acute chest syndrome hospitalizations per year- identified by “n” (2004 to 2010)- Right y axis. Outcomes such as Exchange transfusion(%), Mechanical Ventilation(%) and Mortality(%) are shown as percentages of acute chest syndrome hospitalizations.(2004 to 2010)- Left y axis.
Table 1. Type of sickle cell crisis and procedures performed.
| Type of sickle cell crisis (ICD-9-CM Code) | N (%) |
| Sickle-cell thalassemia with crisis (282.42) | 1029 (4.2%) |
| Hb-SS disease with crisis (282.62) | 20814 (84.3%) |
| Sickle-cell/HB-C disease with crisis (282.64) | 629 (2.5%) |
| Other sickle-cell disease with crisis (282.69) | 2415 (9.8%) |
| Procedures (ICD-9-CM procedure code) | |
| Continuous invasive mechanical ventilation for less than 96 consecutive hours (96.71) | 665 (2.7%) |
| Continuous invasive mechanical ventilation for 96 consecutive hours or more (96.72) | 468 (1.9%) |
| Exchange transfusion (99.01) | 1489 (6%) |
(N = 24699).
The characteristics of hospitalizations are summarized in table 2. The mean patient age was 33 years and males comprised 48.6% of all hospitalizations. A total of 20,089 hospitalizations had information on race. Of these, 92.3% were classified as blacks, 4.3% as Hispanics, 1.4% as whites, 0.3% as Asians/pacific islanders, 0.2% as Native Americans, and 1.4% were other races. A concomitant co-morbid condition was present in 63.7% of all hospitalizations. Close to 95.5% of all hospitalizations occurred on an emergent or urgent basis. About 29.6% of the hospitalizations were covered by Medicare, 40.5% by Medicaid, 20.2% by private insurance, and 3% by other insurance plans. About 6.7% were uninsured. About 73.5% were treated in teaching hospitals. Large bed size hospitals treated 72% of hospitalizations.
Table 2. Characteristics of hospitalizations.
| Characteristic | Response | N (%) |
| Sex | Male | 11999 (48.6%) |
| Female | 12696 (51.4%) | |
| Race | White | 288 (1.4%) |
| Black | 18552 (92.3%) | |
| Hispanic | 871 (4.3%) | |
| Asian/Pacific Islander | 55 (0.3%) | |
| Native American | 44 (0.2%) | |
| Other/Mixed races | 278 (1.4%) | |
| Insurance | Medicare | 7300 (29.6%) |
| Medicaid | 9976 (40.5%) | |
| Private | 4978 (20.2%) | |
| Uninsured | 1643 (6.7%) | |
| Other insurance | 738 (3%) | |
| Type of admission | Emergency/Urgent | 23556 (95.5%) |
| Elective | 1099 (4.5%) | |
| Number of co-morbid conditions | 0 | 8967 (36.3%) |
| 1 | 7694 (31.1%) | |
| 2 | 4414 (17.9%) | |
| 3 | 2032 (8.2%) | |
| 4 | 974 (3.9%) | |
| 5 | 414 (1.7%) | |
| 6 | 155 (0.6%) | |
| 7 | 35 (0.1%) | |
| > = 8 | 13 (0.05%) | |
| Types of co-morbid conditions | AIDS | 89 (0.4%) |
| Alcohol abuse | 241 (1%) | |
| Deficiency anemias | 556 (2.2%) | |
| Rhematoid arthritis/collage vascular diseases | 278 (1.1%) | |
| Chronic blood loss anemia | 144 (0.6%) | |
| Congestive heart failure | 1699 (6.9%) | |
| Chronic pulmonary disease | 3546 (14.3%) | |
| Coagulopathy | 1294 (5.2%) | |
| Depression | 1596 (6.5%) | |
| Diabetes – uncomplicated | 648 (2.6%) | |
| Diabetes with chronic complications | 69 (0.3%) | |
| Drug abuse | 1742 (7%) | |
| Hypertension | 3552 (14.4%) | |
| Hypothyroidism | 280 (1.1%) | |
| Liver disease | 577 (2.3%) | |
| Lymphoma | 54 (0.2%) | |
| Fluid and electrolyte disorders | 6221 (25.2%) | |
| Metastatic cancer | 0 | |
| Neurological disorders | 1102 (4.5%) | |
| Obesity | 559 (2.3%) | |
| Paralysis | 294 (1.2%) | |
| Peripheral vascular disorders | 106 (0.4%) | |
| Psychoses | 595 (2.4%) | |
| Pulmonary circulation disorders | 2564 (10.4%) | |
| Renal failure | 1023 (4.1%) | |
| Solid tumor without metastasis | 25 (0.1%) | |
| Peptic ulcer disease | DS | |
| Valvular disease | 721 (2.9%) | |
| Weight loss | 292 (1.2%) | |
| Hospital teaching status | Non-teaching status | 6472 (26.5%) |
| Teaching status | 17963 (73.5%) | |
| Hospital bed size | Small | 1711 (7%) |
| Medium | 5128 (21%) | |
| Large | 17596 (72%) | |
| Hospital region | Northeast | 6492 (26.3%) |
| Midwest | 4289 (17.4%) | |
| South | 11530 (46.7%) | |
| West | 2388 (9.7%) | |
| Age in years | Mean | 33.2 |
| Standard error | 0.19 |
DS: Discharge information is suppressed as individual cell count is < = 10 (as per data user agreement with HCUP-AHRQ).
Disposition status following hospitalization is summarized in table 3. Routine discharge was the outcome in 86.2% of the hospitalizations, while, 1.7% were transferred to another acute care hospital, 1.9% were transferred to a long term care facility, 5.3% were discharged to a home health care facility, and 3.2% were discharged against medical advice. A total of 393 patients died in-hospitals (mortality rate of 1.6%).
Table 3. Disposition status.
| Disposition status | N (%) |
| Routine discharge | 21287 (86.2%) |
| Transfer to another acute care facility | 431 (1.7%) |
| Transfer to another long term care facility (eg. Skilled nursing facility) | 464 (1.9%) |
| Home health care | 1313 (5.3%) |
| Discharged against medical advice | 793 (3.2%) |
| In-hospital mortality | 393 (1.6%) |
Results of the multivariable analysis examining predictors of in-hospital mortality are summarized in table 4. Patients who had mechanical ventilation for less than 96 consecutive hours (OR = 67.53, 95% CI = 34.12–133.63, p<0.01) or those who had mechanical ventilation for 96 consecutive hours or more (OR = 8.73, 95% CI = 2.16–35.24, p<0.01) were associated with a significantly higher odds for in-hospital mortality when compared to those who did not require mechanical ventilation.
Table 4. Predictors of In-hospital mortality.
| Characteristic | Response | OR (95% CI) | p-value |
| Type of sickle cell crisis | Hb-SS disease with crisis | 0.71 (0.33–1.51) | 0.37 |
| All other crisis | Reference | ||
| Procedure | Continuous invasive mechanical ventilation for <96 consecutive hours | 67.53 (34.12–133.63) | <0.001 |
| Continuous invasive mechanical ventilation for ≥96 consecutive hours | 8.73 (2.16–35.24) | <0.001 | |
| Exchange transfusion | 0.13 (0.02–1.16) | 0.07 | |
| Age in years | Each 1 year increase in age | 1.02 (0.99–1.06) | 0.17 |
| Sex | Female | 0.67 (0.33–1.35) | 0.26 |
| Male | Reference | ||
| Race | Black | 0.27 (0.05–1.49) | 0.13 |
| White | Reference | ||
| Type of admission | Elective | 0.86 (0.15–4.95) | 0.87 |
| Emergency/Urgent | Reference | ||
| Comorbid conditions | Each 1 unit increase in co-morbid conditions | 1.17 (0.97–1.41) | 0.11 |
| Insurance status | Medicare | 1.21 (0.24–6.06) | 0.82 |
| Medicaid | 2.08 (0.41–10.46) | 0.38 | |
| Private insurance | 2.04 (0.43–9.77) | 0.37 | |
| Other insurance | 0.70 (0.03–14.94) | 0.82 | |
| Uninsured | Reference | ||
| Teaching status of hospital | Teaching | 1.46 (0.67–3.21) | 0.34 |
| Non teaching | Reference | ||
| Hospital bed size | Large bed | 0.95 (0.48–1.91) | 0.89 |
| Small/Medium | Reference | ||
| Hospital region | Northeast | 0.78 (0.23–2.65) | 0.69 |
| Midwest | 1.09 (0.28–4.30) | 0.90 | |
| South | 0.58 (0.18–1.85) | 0.36 | |
| West | Reference |
The mean hospital LOS was 7.8 days. Results of the multivariable analysis examining predictors of length of stay are summarized in table 5. Patients who had mechanical ventilation for 96 consecutive hours or more (estimate = 0.9252, 95% CI = 0.81816–1.0318, p<0.001) and those who had an exchange transfusion had a significantly longer hospitalizations (estimate = 0.4033 95% CI = 0.3120–0.4947, p<0.001) after adjusting for all other patient and hospital related factors. Increase in age was associated with shorter hospital length of stay (estimate = −0.0066, 95% CI = −0.0094–−0.0038, p<0.001). Females were associates with longer length of stay compared to males (estimate = 0.0880, 95% CI = 0.0376–0.1384, p<0.001). Patients hospitalized on an elective basis had longer length of stay (estimate = 0.2428 95% CI = 0.1364–0.3492, p<0.001) compared to those hospitalized on an emergent or urgent basis. Those covered by Medicaid (estimate = 0.0940, 95% CI = 0.0009–0.1871, p = 0.048) and other insurance plans (estimate = 0.1974, 95% CI = 0.0561–0.3386, p = 0.006) were associated with longer length of stay compared to the uninsured. Large bed size hospitals were associated with longer length of stay compared to small/medium bed size hospitals (estimate = 0.0655 95% CI = 0.0033–0.1277, p = 0.04). Seasonal variation in acute chest syndrome hospitalizations, mechanical ventilation and in-hospital mortality is shown in table 6.
Table 5. Predictors of length of stay in-hospital.
| Characteristic | Response | Estimate* (95% CI) | p-value |
| Type of sickle cell crisis | Hb-SS disease with crisis | −0.0054 (−0.0769–0.0660) | 0.88 |
| All other crisis | Reference | ||
| Procedure | Continuous invasive mechanical ventilation for <96 consecutive hours | 0.0398 (−0.1290–0.2087) | 0.64 |
| Continuous invasive mechanical ventilation for ≥96 consecutive hours | 0.9252 (0.81816–1.0318) | <0.001 | |
| Exchange transfusion | 0.4033 (0.3120–0.4947) | <0.001 | |
| Age in years | Each 1 year increase in age | −0.0066 (−0.0094–−0.0038) | <0.001 |
| Sex | Female | 0.0880 (0.0376–0.1384) | <0.001 |
| Male | Reference | ||
| Race | Black | −0.0373 (−0.2424–0.1678) | 0.72 |
| Hispanic | −0.1428 (−0.3721–0.0866) | 0.22 | |
| Asian/Pacific islanders | −0.1910 (−0.5377–0.1557) | 0.28 | |
| Native Americans | −0.0619 (−0.4368–0.3129) | 0.75 | |
| Other races | 0.1458 (−0.1217–0.4132) | 0.28 | |
| White | Reference | ||
| Type of admission | Elective | 0.2428 (0.1364–0.3492) | <0.001 |
| Emergency/Urgent | Reference | ||
| Co-morbid conditions | Each 1 unit increase in co-morbid conditions | 0.1062 (0.0864–0.1260) | <0.001 |
| Insurance status | Medicare | 0.0870 (−0.0145–0.1886) | 0.09 |
| Medicaid | 0.0940 (0.0009–0.1871) | 0.048 | |
| Private insurance | 0.0109 (−0.0947–0.1164) | 0.84 | |
| Other insurance | 0.1974 (0.0561–0.3386) | 0.006 | |
| Uninsured | Reference | ||
| Teaching status of hospital | Teaching | 0.0560 (−0.0106–0.1226) | 0.10 |
| Non teaching | Reference | ||
| Hospital bed size | Large bed | 0.0655 (0.0033–0.1277) | 0.04 |
| Small/Medium | Reference | ||
| Hospital region | Northeast | 0.0348 (−0.0709–0.1406) | 0.52 |
| Midwest | 0.0219 (−0.0945–0.1384) | 0.71 | |
| South | 0.0582 (−0.0428–0.1591) | 0.26 | |
| West | Reference |
Mean length of stay in-hospital is 7.8 days (standard error is 0.13)
*Positive estimate implies increased LOS compared to the reference variable. Negative estimate implies decreased LOS compared to the reference variable.
Table 6. Sensitivity Analysis to Examine Seasonal Variations.
| Variable | January–March | April–June | July–September | October–December |
| Sickle-cell thalassemia with crisis (282.42) | 291 | 172 | 265 | 301 |
| Hb-SS disease with crisis (282.62) | 5336 | 4771 | 5308 | 5372 |
| Sickle-cell/HB-C disease with crisis (282.64) | 113 | 113 | 211 | 181 |
| Other sickle-cell disease with crisis (282.69) | 592 | 495 | 663 | 655 |
| Continuous invasive mechanical ventilation for <96 consecutive hours (96.71) | 162 | 176 | 192 | 136 |
| Continuous invasive mechanical ventilation for ≥96 consecutive hours (96.72) | 123 | 102 | 115 | 129 |
| Exchange transfusion (99.01) | 347 | 333 | 373 | 436 |
| In-hospital mortality(total number) | 88 | 69 | 142 | 93 |
| In-hospital mortality as % of all hospitalizations | 1.39% | 1.24% | 2.20% | 1.42% |
Note: For 47 hospitalizations, information on discharge quarter was not available.
Discussion
Advances in medical technology, immunizations, infection control, improved patient education, and multidisciplinary care have led to an increasing number of adults living with sickle cell disease [12], [13]. Although it is known that disease severity and mortality rate are much higher in adults with sickle cell disease and acute chest syndrome compared to children [2], [6], [11], current national estimates of hospital resource utilization and outcomes in adults with acute chest syndrome are lacking. To our knowledge, our study is the largest cohort of hospitalized adult patients with sickle cell disease and acute chest syndrome whose outcomes were assessed using a multitude of patient and hospital level characteristics at a national level.
Consistent with prior studies [3], [14], we showed that adults with Hb-SS phenotype accounted for the highest rate of acute chest syndrome hospitalizations. Further, in the present study, although, Hb-SS disease with crisis accounted for the majority of hospitalizations, neither the in-hospital mortality nor the length of stay were influenced by the genotype of sickle cell disease. This could suggest that, rather than the genotype, it is the severity of acute chest syndrome and resulting respiratory failure (as evidenced by the need of mechanical ventilation) that influences mortality.
In our study, acute respiratory failure requiring mechanical ventilation was found in 4.6% of hospitalizations with an overall all cause in-hospital mortality rate of 1.6% which is lower in comparison to the 13% mechanical ventilation and 3% mortality in the National Acute Chest Syndrome Group (NACS-671 episodes) study [5], [18]. This lower mortality could be due to the advances in medical care and management strategies over the past decade. Interestingly, the mortality for patients with acute chest syndrome patients requiring mechanical ventilation in the NACS study was better than the overall mortality rate for patients with acute chest syndrome (19% compared to approximately 30%, respectively). It is very intriguing to note that, in our study, any need for mechanical ventilation was an independent predictor of mortality, with the odds of mortality being highest in the first 96 hours. Our results are consistent with a single center intensive care unit experience of higher risk of mortality in invasively mechanically ventilated patients (12–52 years) with acute chest syndrome [29]. Our results contrast those of a recent study in adolescents and young adults (16–25 years) with sickle cell disease admitted with acute chest syndrome in that although nearly 45% of those patients required mechanical ventilation, the in-hospital mortality was 0.6% of all hospitalizations [7].
The mean length of hospitalization in our study was 7.8 days which is lower compared to 10.5 days in the NACS study [18]. In our study, the predictors of increased LOS included mechanical ventilation (≥96 hours), need for exchange transfusion and increased co morbid burden, factors that are intuitively anticipated to cause increased LOS. It is of interest to note that in our study for every 1 year increase in age, the LOS was lower, although marginally low. A prior study using similar national administrative database found that older children with sickle cell disease and vaso-occlusive crisis had a longer LOS [25].
Prior studies have demonstrated that both simple and exchange transfusions alleviate organ dysfunction in patients with sickle cell crisis and acute chest syndrome [5], [15], [16], [17]. Although, no definitive randomized controlled trials exist to evaluate the timing of blood transfusion (simple or exchange) in acute chest syndrome in adults, most experts recommend no transfusions for mild, simple transfusions for moderate and exchange transfusions for severe acute chest syndrome. In our study, 6% of the hospitalizations received exchange transfusion and after adjustment of known confounding factors, exchange transfusion was not an independent predictor of in-hospital mortality, although it did lead to a 40% increase in length of stay. This is in sharp contrast to the exchange transfusion rate of 3% in adolescents/young adults hospitalized for acute chest syndrome [7]. The timing and impact of exchange transfusion on outcomes in the adult population merits further research.
A prior study showed that hospitals with low volume of admissions for sickle cell disease had higher mortality rates compared to high volume hospitals [24], a finding that is true across other disease processes as well [26], [27]. In contrast, our study found that a multitude of patient and hospital level factors such as increasing age, race, gender, co-morbid conditions, insurance, teaching status, hospital bed size or region did not influence the in-hospital mortality rate, further underscoring that the severity of illness and need for mechanical ventilation are more pertinent factors. No prior study has looked at seasonal variations in outcomes for sickle cell disease patients with acute chest syndrome. In the present study, the in-hospital mortality ranged from a low of 1.24% (April–June) to a high of 2.20% (July–September). The impact of viral infections (which have seasonal variation) on sickle cell acute chest syndrome hospitalization outcomes merits further research.
The particular strength of our study rests on the size and breadth of our sample. NIS is the largest all-payer hospital discharge database in United States and represents experiences beyond a single center. The outcomes assessed in this large cohort of patients reflect the impact of advances in medical care in the given time frame. Identifying predictors of worse outcomes is useful in devising preventive management strategies to optimize outcomes. There are, however, several methodological limitations to this study. Due to its retrospective nature, the cause and effect relationship between the independent variables and occurrence of a particular event cannot be firmly established. There are also inhered limitations associated with the use of a large secondary hospital discharge administrative datasets. Nevertheless, a recent study demonstrated the effective use of a large multi-institute administrative dataset in assessing the outcomes of adolescents and young adults with acute chest syndrome [7]. In addition, prior studies have shown that the combination of administrative data with certain clinical data can be used efficiently to stratify surgical risk [19], [20]. Although we used a multivariable regression analysis to account for the confounding effects of patient and hospital level variables, the risk adjustment performed is not comprehensive owing to the lack of adequate patient level data and severity of the disease process (mild, moderate or severe acute chest syndrome) in the NIS dataset. However, a number of chronic conditions beyond sickle cell disease and admission type (elective, urgent) were used for disease severity adjustment. Also, the nature of the dataset precludes us from assessing the impact of certain factors that are known to influence outcomes such as long term treatment with hydroxyurea, which has been shown to decrease the acute chest syndrome frequency and mortality [21], [22], [23]. Hospital readmissions of adult patients with sickle cell anemia are common and are associated with higher mortality [28]. The lack of patient identifiers precludes us from identifying readmissions in our study. Finally, our study results indicate that those with continuous invasive mechanical ventilation of <96 hours duration were associated with a very high odds of in-hospital mortality. The reasons for high mortality rates in this cohort are multifold and include: severity of acute chest syndrome, time of starting mechanical ventilation, or death during mechanical ventilation. The NIS dataset does not provide information on the severity of acute chest syndrome, event leading to death, or time of starting the mechanical ventilation. Consequently, we are unable to examine these factors.
Despite these limitations, our study reveals that acute chest syndrome is not an infrequent cause of hospitalization in adults with sickle cell disease. There was a gradual yearly increase in the number of hospitalizations due to acute chest syndrome, and an increase in mechanical ventilation in such patients. Our findings lend support to the need for better understanding the factors predisposing to respiratory failure in this growing cohort of the population.
Conclusions
In this large cohort of hospitalized adults with sickle cell disease and acute chest syndrome, the need for mechanical ventilation predicted higher mortality rates and increased hospital resource utilization. Identification of risk factors may enable optimization of outcomes.
Funding Statement
The authors have no support or funding to report.
References
- 1. Vichinsky E (1991) Comprehensive care in sickle cell disease: its impact on morbidity and mortality. Semin Hematol 28: 220–226. [PubMed] [Google Scholar]
- 2.Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, et al. (1994) Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med; 330(23): 1639. PMID: 7993409. [DOI] [PubMed]
- 3.Thomas AN, Pattison C, Serjeant GR (1982) Causes of death in sickle-cell disease in Jamaica. Br Med J (Clin Res Ed) 285(6342): 633. PMID: 6819042. [DOI] [PMC free article] [PubMed]
- 4.Vichinsky EP, Neumayr LD, Earles AN, Williams R, Lennette ET, et al. (2000) Causes and outcomes of the acute chest syndrome in sickle cell disease. N Engl J Med 342: 1855–1865[Erratum, N Engl J Med 2000;343:824.]. [DOI] [PubMed]
- 5.Castro O, Brambilla DJ, Thorington B, Reindorf CA, Scott RB, et al. (1994) The acute chest syndrome in sickle cell disease: incidence and risk factors. The Cooperative Study of Sickle Cell Disease. Blood. 84(2): 643. PMID: 7517723. [PubMed]
- 6. Vichinsky EP, Styles LA, Colangelo LH, Wright EC, Castro O, et al. (1997) Acute chest syndrome in sickle cell disease: clinical presentation and course. Cooperative Study of Sickle Cell Disease Blood. 89(5) 1787 PMID: 9057664 [PubMed] [Google Scholar]
- 7.Jan S, Slap G, Smith-Whitley K, Dai D, Keren R, et al. (2013) Association of hospital and provider types on sickle cell disease outcomes. Pediatrics. 2013 Nov;132(5): 854–61. Epub, Oct 28. PMID: 24167173. doi: 10.1542/peds.2013-0089. [DOI] [PubMed]
- 8.Melton CW, Haynes J Jr (2006) Sickle acute lung injury: role of prevention and early aggressive intervention strategies on outcome. Clin Chest Med. 27(3): 487. PMID: 16880058. [DOI] [PubMed]
- 9.Reagan MM, DeBaun MR, Frei-Jones MJ (2011) Multi-modal intervention for the inpatient management of sickle cell pain significantly decreases the rate of acute chest syndrome. Pediatr Blood Cancer. 56(2): 262. PMID: 21157894. [DOI] [PMC free article] [PubMed]
- 10.The Healthcare Cost and Utilization Project sponsored by Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/nisoverview.jsp. [PubMed]
- 11. Powars D, Weidman JA, Odom-Maryon T, Niland JC, Johnson C (1988) Sickle cell chronic lung disease: prior morbidity and the risk of pulmonary failure. Medicine (Baltimore) 67: 66–76. [PubMed] [Google Scholar]
- 12.Quinn CT, Rogers ZR, McCavit TL, Buchanan GR (2010) Improved survival of children and adolescents with sickle cell disease. Blood. 2010 Apr 29;115(17): 3447–52. Epub, Mar 1. PMID: 20194891. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed]
- 13.Quinn CT, Rogers ZR, Buchanan GR (2004) Survival of children with sickle cell disease. Blood. 2004 Jun 1;103(11): 4023–7. Epub Feb 5. PMID: 14764527. [DOI] [PMC free article] [PubMed]
- 14.Maitre B, Habibi A, Roudot-Thoraval F, Bachir D, Belghiti DD, et al. (2000) Acute chest syndrome in adults with sickle cell disease. Chest. 117(5): 1386. PMID: 10807826. [DOI] [PubMed]
- 15. Vichinsky EP, Haberkern CM, Neumayr L, Earles AN, Black D, et al. (1995) A comparison of conservative and aggressive transfusion regimens in the perioperative management of sickle cell disease: the Preoperative Transfusion in Sickle Cell Disease Study Group. N Engl J Med 333: 206–213. [DOI] [PubMed] [Google Scholar]
- 16. Mallouh AA, Asha M (1988) Beneficial effect of blood transfusion in children with sickle cell chest syndrome. Am J Dis Child 142: 178–182. [DOI] [PubMed] [Google Scholar]
- 17. Emre U, Miller ST, Gutierez M, Steiner P, Rao SP, et al. (1995) Effect of transfusion in acute chest syndrome of sickle cell disease. J Pediatr 127: 901–904. [DOI] [PubMed] [Google Scholar]
- 18.Gladwin MT, Vichinsky E (2008) Pulmonary Complications of Sickle Cell Disease. N Engl J Med; 359: 2254–2265, November 20, 2008. doi: 10.1056/NEJMra0804411. [DOI] [PubMed]
- 19. Fry DE, Pine M, Jordan HS, Elixhauser A, Hoaglin DC, et al. (2007) Combining administrative and clinical data to stratify surgical risk. Ann Surg. Nov 246(5): 875–85. [DOI] [PubMed] [Google Scholar]
- 20. Pine M, Jordan HS, Elixhauser A, Fry DE, Hoaglin DC, et al. (2007) Enhancement of claims data to improve risk adjustment of hospital mortality. JAMA. Jan 3 297(1): 71–6. [DOI] [PubMed] [Google Scholar]
- 21. Stallworth JR, Jerrell JM, Tripathi A (2010) Cost effectiveness of hydroxyurea in reducing the frequency of pain episodes and hospitalization in pediatric sickle cell disease. Am J Hematol 85(10): 795–797. [DOI] [PubMed] [Google Scholar]
- 22. Wang WC, Ware RE, Miller ST, Iyer RV, Casella JF, et al. (2011) BABY HUG investigators. Hydoxycarbarmide in very young children with sickle-cell anaemia: a multi-center, randomized, controlled trial (BABY HUG) Lancet 377(9778): 1663–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Steinberg MH, Barton F, Castro O, Pegelow CH, Ballas SK, et al. (2003) Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA 289(13): 1645–1651. [DOI] [PubMed] [Google Scholar]
- 24. McCavit TL, Lin H, Zhang S, Ahn C, Quinn CT, et al. (2011) Hospital volume, hospital teaching status, patient socioeconomic status and outcomes in patients hospitalized with sickle cell disease. Am J Hematol 86(4): 377–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Panepinto JA, Brousseau DC, Hillery CA, Scott JP (2005) Variation in-hospitalizations and hospital length of stay in children with vaso-occlusive crises in sickle cell disease. Pediatr Blood Cancer. Feb 44(2): 182–6. [DOI] [PubMed] [Google Scholar]
- 26. Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137: 511–520. [DOI] [PubMed] [Google Scholar]
- 27.Ross JS, Normand ST, Wang Y, Ko DT, Chen J, et al. (2010) Hospital Volume and 30-Day Mortality for Three Common Medical Conditions. N Engl J Med, 362:1110–1118March 25, 2010 doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed]
- 28.Ballas SK, Lusardi M (2005) Hospital readmission for adult acute sickle cell painful episodes: frequency, etiology, and prognostic significance. Am J Hematol. May;79(1): 17–25. PMID: 15849770. [DOI] [PubMed]
- 29.Tawfic QA, Kausalya R, Al-Sajee D, Burad J, Mohammed AK, et al. (2012) Adult sickle cell disease: A Five year experience of Intensive care management in a University hospital in Oman. SQU MED J, Vol 12, ISS 2, PP: 177–183. Epub, 9th Apr. [DOI] [PMC free article] [PubMed]