Abstract
Objective
Following the introduction of highly active antiretroviral therapy (HAART) the risk of AIDS-defining cancers decreased but incidence of many non-AIDS-defining cancers has reportedly increased in those with HIV/AIDS. Whether melanoma risk has also changed in HIV/AIDS patients post-HAART is unknown and therefore we evaluated this in comparison with the risk before HAART.
Design
Systematic review and meta-analysis.
Methods
We searched Medline, Embase and ISI science citation index databases to April 2013. All cohort studies of patients diagnosed with HIV/AIDS that permitted quantitative assessment of the association with melanoma were eligible. Detailed quality assessment of eligible studies was conducted, focussing particularly on adjustment for ethnicity, a priori considered essential for an unbiased assessment of melanoma risk. Data were pooled using a random effects model.
Results
From 288 articles, we identified 21 that met the inclusion criteria, 13 presenting data for the post-HAART era and 8 for the pre-HAART era. Post-HAART the pooled relative risk (pRR) for the association between HIV/AIDS and melanoma was 1.26 (95% CI, 0.97–1.64) and 1.50 (95% CI 1.12–2.01) among studies that accounted for ethnicity, with evidence of significant heterogeneity (P = 0.004, I2 = 55.5). Pre-HAART pRRs were 1.26 (95% CI 1.11–1.43; Phet = 0.82) and 1.28 (95% CI 1.10–1.49) among studies adjusted for ethnicity.
Conclusions
People with HIV/AIDS remain at a significantly increased risk of developing melanoma in the post-HAART era. White skinned people with HIV/AIDS should be screened regularly and counselled against excessive sun exposure.
Introduction
Prior to the introduction of highly active antiretroviral therapy (HAART) in the latter part of the 1990s, a modestly increased incidence of cutaneous melanoma in people with human immunodeficiency virus infection/acquired immunodeficiency syndrome (HIV/AIDS) was observed. A meta-analysis of population-based data collected mostly prior to the introduction of HAART reported an overall Standardised Incidence Ratio (SIR) for melanoma of 1.24 (95% CI = 1.04-1.48) [1]. Since then there has been a decrease in incidence of AIDS-defining cancers including Kaposi's sarcoma and non-Hodgkin lymphoma, but a reported increase in incidence of many non-AIDS-defining cancers [2]. Whether the risk of melanoma in HIV/AIDS populations compared with the general population has increased since the introduction of HAART along with other non-AIDS-defining cancers is unknown however. It is important to quantify this risk given increased longevity of patients treated with HAART [3] and the consequent increased period at risk of melanoma against a background of rising rates in most white populations [4] together with some evidence of patients' predilection for recreational sun exposure [5]. The association between HIV and melanoma is also important to understand better, since laboratory studies have indicated a role for immune surveillance in melanoma genesis and increasingly immunotherapeutic approaches for the treatment of metastatic disease are being developed [6]. We conducted a systematic review and meta-analysis to evaluate melanoma risk in HIV/AIDS patients compared with the general population in the pre-HAART and post-HAART eras.
Patients and Methods
The systematic review and meta-analysis was conducted in accordance with the Meta-analysis of Observational Studies in Epidemiology guidelines for reviews of observational. Studies [7], and we followed the PRISMA statement [8] to guide reporting.
Data Sources and Searches
Eligible studies up to April 2013 were identified by searching the Medline 1950 (U.S. National Library of Medicine, Bethesda, MD) database using PubMed software as the search interface; Embase 1966 database (Elsevier Science, Amsterdam, Holland) using the Embase search interface; and the ISI Science Citation Index using the ISI Web of Science search interface. We used the following medical subject headings terms or text words (both the United States and United Kingdom spellings): melanoma, cancer, neoplasms, HIV, AIDS, human immunodeficiency virus, acquired immunodeficiency syndrome, aetiology, cohort (Appendix S1 – Search terms). Studies that had been commonly cited in the literature and review articles were also included as citation search terms in the ISI Science Citation Index (1990 to present) to identify subsequent studies that had referenced them. The search was not limited to studies published in English. We read the abstracts of all identified studies to exclude those that were clearly not relevant. The full texts of the remaining articles were read to determine if they met study inclusion criteria. Eligible studies were also identified by hand-searching the reference lists of retrieved articles.
Study Selection
We included cohort studies, including population-based record linkage studies, of adult populations (ie predominantly > 18 years of age) diagnosed with HIV/AIDS that permitted quantitative assessment of the association between HIV/AIDS and melanoma. Studies that reported different measures of relative risk (RR), namely Hazard Ratio (HR), Incidence Rate Ratio (IRR), and Standardised Incidence Ratio (SIR) were included. Excluded were studies reporting on paediatric cohorts (< 18 years of age) and studies with melanoma mortality as the outcome. Any discrepancies between investigators about inclusion of a study were resolved by joint evaluation of the manuscript. When multiple reports were published on the same population or subpopulation, we included the report with the longest follow-up duration or the largest population.
Data Extraction and Quality Assessment
Two investigators (CO, LK) independently abstracted data from identified studies using a standardised data abstraction form, with inconsistencies resolved by consensus. The following information was recorded for each study: design, location, years of data collection, source and definition of cohort, number of cases, person-year duration of follow-up, age of study population, variables used for statistical adjustment, point estimates (RR, HR, IRR or SIR), and 95% confidence intervals (95% CI). Where several risk estimates were presented (e.g. crude and adjusted), we abstracted those adjusted for the greatest number of potential confounders. Studies that reported results separately by time period (pre- and post-HAART) or other strata with no combined data were treated as independent data sets in the meta-analysis.
Two investigators (CO, LK) independently evaluated the quality of the studies by using a scoring system that was designed with reference to the following guidelines: Meta-analysis Of Observational Studies in Epidemiology (MOOSE) [7], Quality Assessment Tool for Systematic reviews of Observational studies (QATSO) [9], and Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [10]. A total score of 4–6 was considered high quality, 1–3, low-moderate quality. One point each was allocated for (a) representativeness of the exposed cohort (i.e. population-based); (b) diagnosis of HIV confirmed according to accepted laboratory testing criteria [11]; (c) description of calculation of person-years at risk; (d) consistency of melanoma ascertainment in HIV cohort and comparison population; (e) adjustments made for age, sex and ethnicity; and (f) adjustments made for other relevant factors, namely time period, cancer registry and region. Single-institution studies and those with selected patient representation were classified as non- population-based. Disagreements about any item were resolved through discussion.
Data Synthesis and Analysis
To pool individual study estimates for the risk of melanoma in HIV/AIDS in the pre-HAART and post-HAART time periods, we used random effects models [12]. The analyses were repeated using the weighted average method where the weight of each study is inversely proportional to the study variance (Table S1). Statistical heterogeneity among studies was assessed using the Q statistic [13] (significance level at P<0.05), and inconsistencies were quantified using the I2 statistic [14]. We performed a sensitivity analysis by omitting one study at a time, and calculated the pooled relative risk (pRR) for the remaining studies to evaluate whether the results were affected markedly by a single study. Finally, publication bias was evaluated through visual inspection of a funnel plot and with Begg's and Egger's tests [15], [16]. We defined the post-HAART was as after 1995. There was a rapid uptake of HAART in all countries in North America and Western and Central Europe [17] following the recommendations from an international panel on antiretroviral therapy for HIV infection, released in 1996 [18].
Subgroup analyses were carried out according to important study features: consistency of cancer ascertainment in cohort and comparison population; representativeness (population-based or clinic-based); quality score; geographic region; and adjustment for ethnicity. Since skin colour as indicated by ethnicity is strongly associated both with HIV/AIDS [19] and melanoma [20], ethnicity was considered a priori a major confounding factor and adjustment for ethnicity therefore regarded as essential for achieving an unbiased estimate of melanoma risk. A separate meta-analysis was conducted for studies that reported on risk of melanoma in cohorts of people diagnosed with AIDS where that population was clearly defined. All statistical analyses were performed using Stata Version 10 (Stata Corporation, College Station, TX).
Results
Search Results
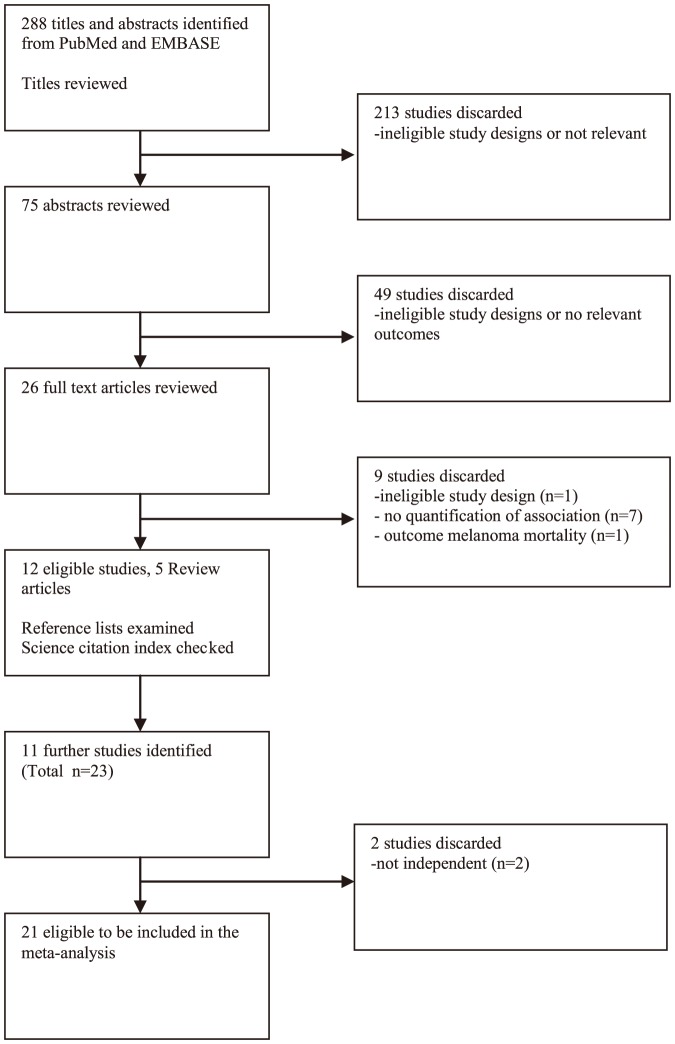
Details of the selection process for the eligible studies are shown in Figure 1. A total of 21 eligible studies were identified and included in our systematic review [2], [21]–[40]. We did not identify any relevant studies published in a language other than English, and no ineligible studies of children only were identified.
Figure 1. Flow chart of literature search for studies on the association between HIV/AIDS and risk of melanoma.
Characteristics of included studies
Eligible studies were published between 1999 and 2013 (Table 1). One was conducted in Australia [32], eight in Europe [24], [26], [29], [31], [33]–[35], [39], and twelve in North America [2], [21]–[23], [25], [27], [28], [30], [36]–[38], [40]. Of the 21 studies, nine used different methods to ascertain melanoma diagnoses in the HIV cohort and the comparison population [2], [24], [25], [29], [30], [33], [35], [37], [39], the remaining 12 relied on cancer registry data for both groups [21]–[23], [26]–[28], [31], [32], [34], [36], [38], [40]. Most studies reported on cohorts of people either infected with HIV or diagnosed with AIDS. Six studies defined their cohort as patients with AIDS [22], [23], [27], [28], [31], [36], though four of these six studies included time before onset of AIDS in calculations of person-years at risk [22], [23], [28], [31]. The study by Frisch et al. [22] and one additional study [26] had conducted separate analyses on subsets of the population after AIDS onset. Five studies were not population-based: one cohort included only men who have sex with men [37], one included women only [25], one was a cohort of veterans [40] and two studies reported on single-clinic patient cohorts [2], [33]. The remaining 16 studies reported on population-based patient cohorts, predominantly men (range 76%–92%). Median follow-up time was reported by only eight [2], [24], [29], [30], [32], [37], [39] of the 21 included studies and ranged from two to ten years. Eight studies presented estimates for the pre-HAART [21]–[24], [27], [31], [32], [34] and 13 for the post-HAART time periods [2], [24], [27], [31]–[39], [41]. Findings of five studies that did not present effect estimates stratified by time period [25], [26], [28]–[30] were included in an overall estimate of risk based on all studies time period notwithstanding.
Table 1. Characteristics of the 21 studies included in the meta-analysis of HIV and/or AIDS and the risk of melanoma.
| Study | Location | Study period | Cohort description | Cohort size | Cases | Male % | Cohort median age at recruitment | Age range | Effect estimates providedb | ||
| Pre-HAART | Post-HAART | AIDS | |||||||||
| Cohort studies | |||||||||||
| Calabresi et al., 2013 [39] | Italy, 1 province | 1999–2009 | HIV or AIDS | 5,090 | 8 | 82 | 35 | 19–64 | SIR | ||
| Vogel et al., 2011 [35] | Germany, Bonn | 1996–2009 | HIV or AIDS | 1,476 | 1 | 81 | NS | 16–85 | SIR | ||
| Seaberg et al., 2010 [37] | United States, 4 metropolitan areas | 1984–2007 | HIV | 6,949 | 9 | 100 | 32.6 | <30–>50 | SIR | ||
| Franceschi et al., 2010 [34] | Switzerland, 9 cancer registries | 1985–2007 | HIV or AIDS | 9,429 | 11 | 81 | 32 | >16 | SIR | SIR | |
| Powles et al., 2009 [33] | England, 1 clinical centre | 1996–2007 | HIV | 11,112 | 5 | 90 | NS | NS | SIR | ||
| Long et al., 2008 [2] | United States, 1 clinical centre | 1996–2005 | HIV | 2,566 | 4 | 68 | 38 | <30-> = 50 | SIR | ||
| Patel et al., 2008 [30] | United States, 13 cancer registries | 1992–2003 | HIV | 54,780 | NS | 76 | NS | 13–84 | |||
| Serraino et al., 2007 [29] | Italy, 19 clinical centres France, 1 region | 1988–2004 | HIV | 8074 | 2 | 81 | 31.3 | <35->50 | |||
| Hessol et al., 2004 [25] | United States | 1994–1995 | HIV or AIDS | 1,554 | 2 | 0 | NS | <30-50+ | |||
| Herida et al., 2003 [24] | France, 12 cancer | 1992–1999 | HIV | 77,025 | 19 | 84 | Pre-HAART | 15-69 | SIR | SIR | |
| registries | 39 (male); 33 (female) | ||||||||||
| Post-HAART | |||||||||||
| 42(male); 38 (female) | |||||||||||
| Record linkage studies | |||||||||||
| Silverberg et al., 2011 [38] | United States, 1 state | 1996–2008 | HIV or AIDS | 20,775 | 34 | 91 | 40.6 | NS | RR | ||
| Simard et al., 2010 [36] | United States, 15 regions | 1980–2004 | AIDS | 263,254 | 96 | 80 | 36 | 15-> = 50 | SIR | SIR | |
| Bedimo et al., 2009 [40] | United States | 1997–2004 | HIV or AIDS | 33,420 | 96 | 98 | NS | NS | IRR | ||
| Dal Maso et al., 2009 [31] | Italy, 24 cancer registries | 1986–2005 | HIVa or AIDS | 21,951 | 6 | Pre-HAART 32 | 16–69 | SIR | SIR | ||
| Post-HAART 38 | |||||||||||
| Van Leeuwen et al., 2009 [32] | Australia, national | 1982–2004 | HIV or AIDS | 17,175 | 53 | 92 | NS | 16–80 | SIR | SIR | |
| Hessol et al., 2007 [28] | United States, San Francisco | 1990–2000 | HIVa or AIDS | 14,210 | 36 | 96 | NS | 16–86 | |||
| Engels et al., 2006 [27] | United States, 6 states and | 1980–2002 | AIDS | 375,933 | 45 | 89 | Pre-HAART 37.7 | >15 | SIR | SIR | SIR |
| 5 cities | Post-HAART 39.3 | ||||||||||
| Newnham et al., 2005 [26] | England | 1985–2001 | HIV or AIDS | 33,190 HIV 12,126 AIDS | 2 | 79 HIV 88 AIDS | NS | 15–60 | SIR | ||
| Frisch et al., 2001 [22] | United States, 11 regions | 1978–1996 | HIVa or AIDS | 302,834 | 145 | 37 (male) 35 (female) | 15–69 | SIR | SIR | ||
| Gallagher et al., 2001 [23] | United States, New York State | 1981–1994 | HIVa or AIDS | 122,993 | 24 | 89 | NS | 15–69 | SIR | ||
| Cooksley et al., 1999 [21] | United States, single county | 1985–1994 | HIV or AIDS | 14,986 | 6 | 85 | 35 | <1–91 | SIR | ||
aHIV described if cohort entry was AIDS defined but person-year calculations included pre AIDS onset.
Compared with the general population.
Quality Assessment Results
Twelve (57%) of the 21 studies included in the meta-analysis were considered to be of high quality; the remaining 9 studies of low to moderate quality (Table S2). The most common limitation was lack of adjustment for ethnicity. Of the studies that had adjusted for ethnicity, Frisch et al. [22] provided detailed information on their method of adjustment but background cancer rates were not available for Hispanics and thus expected cancers in that ethnic group were based on cancer rates for whites (21% of both men and women in the cohort were Hispanic). Other studies reported that SIRs were adjusted for ethnicity [2], [23], [25], [27], [28], [36], [37], or matched [40], or a term for ethnicity was included in the regression model [30], [38].
Outcome
The summary estimates for the association between HIV/AIDS in the post-HAART period was 1.26, 95% CI 0.97–1.64) and 1.50 (95% CI 1.12–2.01) when restricted to studies that accounted for ethnicity during analyses (Fig. 2), compared with a pre-HAART pRR of 1.26 (95% CI 1.11–1.43; P het = 0.82) and 1.28 (95% CI 1.10–1.49) for studies adjusted for ethnicity (Fig. 3). Significant heterogeneity was evident in the post-HAART era only (P = 0.004, I2 = 55.5; Table 2).
Figure 2. Forest plot of the association between HIV/AIDS and melanoma in the post-HAART time period, stratified by adjustment for ethnicity.
Each line represents an individual study result with the width of the horizontal line indicating 95% CI, the position of the box representing the point estimate, and the size of the box being proportional to the weight of the study.
Figure 3. Forest plot of the association between HIV/AIDS and melanoma in the pre-HAART time period, stratified by adjustment for ethnicity.
Each line represents an individual study result with the width of the horizontal line indicating 95% CI, the position of the box representing the point estimate, and the size of the box being proportional to the weight of the study.
Table 2. Meta-analysis results using a Random Effects model: HIV/AIDS and risk of melanoma in the pre- and post-HAART time periods.
| Pre-HAART | Post-HAART | |||||||
| Number of studies | Pooled effect estimate (95% CI) | I2 (%) | P heterogeneity | Number of studies | Pooled effect estimate (95% CI) | I2 (%) | P heterogeneity | |
| HIV/AIDS Cohorts | 8 | 1.26 (1.11–1.43) | 0 | 0.823 | 13 | 1.26 (0.97–1.64) | 55.5 | 0·004 |
| Adjusted for ethnicity | ||||||||
| Yes | 2 | 1.28 (1.10–1.49) | 0 | 0.924 | 6 | 1.50 (1.12–2.01) | 54.5 | 0.051 |
| No | 6 | 1.21 (0.95–1.55) | 0 | 0.567 | 7 | 1.03 (0.68–1.57) | 46.6 | 0.051 |
| AIDS only Cohorts | 3 | 1.11 (0.95–1.30) | 0 | 0.867 | 3 | 1.07 (0.83–1.39) | 0 | 0.750 |
| Melanoma ascertainment | ||||||||
| Internal/Registry | 1 | 1.82 (0.90–3.65) | - | - | 6 | 1.78 (1.17–2.71) | 5.1 | 0.388 |
| Registry only | 7 | 1.25 (1.09–1.42) | 0 | 0.821 | 7 | 1.11 (0.81–1.52) | 67.8 | 0.002 |
| Population-based | ||||||||
| Yes | 8 | 1.26 (1.11–1.44) | 0 | 0.823 | 10 | 1.15 (0.88–1.50) | 56.4 | 0.007 |
| No | 0 | - | - | - | 3 | 2.98 (1.49–5.93) | 0 | 0.759 |
| Study location | ||||||||
| Europe | 3 | 1.49 (0.85–2.61) | 0 | 0.702 | 6 | 1.44 (0.98–2.11) | 2.8 | 0.408 |
| North America | 4 | 1.27 (1.11–1.46) | 0 | 0.584 | 6 | 1.50 (1.12–2.01) | 54.5 | 0.051 |
| Australia | 1 | 1.09 (0.74–1.62) | - | - | 1 | 0.61 (0.40–0.92) | - | - |
| Study quality | ||||||||
| High | 6 | 1.26(1.11–1.44) | 0 | 0.975 | 6 | 1.14 (1.83–1.57) | 70.6 | 0.001 |
| Low-moderate | 2 | 1.14 (0.49–2.66) | 48.4 | 0.144 | 7 | 1.61 (1.03–2.52) | 16.9 | 0.297 |
For the pre-HAART time period, the summary estimates were not influenced by excluding one study at a time, with the pRR ranging from 1.21 (95% CI 0.98–1.48) with the omission of Frisch et al. [22] to 1.28 (95% CI, 1.12–1.47) with the omission of Van Leeuwen et al. [32]. The funnel plot was close to symmetrical and there was no evidence of publication bias using the Egger weighted regression method (P for bias = 0.38) or the Begg rank correlation method (P for bias = 0.72). Similarly, for the post-HAART time period, sensitivity analyses excluding individual studies resulted in summary estimates ranging from 1.20 (95% CI 0.90–1.59) with the omission of Silverberg et al. [38] to 1.38 (95% CI 1.10–1.74) with the omission of Van Leeuwen et al. [32]. Again, there was no evidence of publication bias (Egger P for bias = 0.58; Begg P for bias = 0.82).
For both time periods, the pRR was noticeably higher for studies that ascertained melanoma diagnosis using different methods for the HIV cohort and the comparison population (i.e. internal ascertainment for the HIV cohort and Registry ascertainment for the comparison population) (Table 2). In sub-group analyses restricted to studies that received a high quality score the summary estimate was higher in the pre-HAART period (pRR 1.26 pre-HAART and 1.14 post-HAART). In contrast, for studies that received a low-to-moderate quality score, the pooled estimate was higher in the post-HAART period (pRR 1.14 pre-HAART and 1.61 post-HAART).
Five studies did not present effect estimates stratified by time period [25], [26], [28]–[30], and the summary estimate including these five studies for all time periods (total n = 21) was 1·31 (95% CI, 1·11–1·55), with evidence of significant heterogeneity (P<0·001, I2 = 58%) (Figure S1). Also since several of the US studies used overlapping data, a sensitivity analysis excluding 2 of the 3 largest US studies in turn was conducted but showed little effect on the overall pooled estimate (for all time periods), ranging from 1.33 (with the exclusion of Simard et al. [36] and Engels et al. [27]) to 1.30 (with the exclusion of Simard et al. [36] and Fritsch et al. [22]).
The pRR for four studies that presented estimates of risk of melanoma in patients diagnosed with AIDS was 1.07 (95% CI 0.83–1.39), without significant heterogeneity (P = 0.75), and was similar in the pre-HAART and post-HAART time periods (Table 2). Removing the single study that had not adjusted for ethnicity [26] (contributed to the post-HAART estimate only) did not materially alter the pooled estimate (pRR 1.08, 95% CI 0.84–1.40).
Discussion
We have systematically reviewed the most recent epidemiologic data reporting the relationship between HIV/AIDS and melanoma in the HAART era and conducted a meta-analysis. Taking into account the potential confounding effects of ethnicity, our findings show that risk of melanoma in those with HIV/AIDS remains elevated in the HAART era, with a 50% increased risk. We observed significant heterogeneity by study design, with a higher summary estimate from cohort studies where melanoma ascertainment differed between the HIV/AIDS cohort and the comparison population. Our findings for the pre-HAART period are consistent with those of a previous meta-analysis of 6 population-based studies [1] that was published in 2007. Our meta-analysis for the pre-HAART period included two additional studies [21], [24] and further follow-up data for three of the six study populations included in the previous review [31], [32], [34]. A second meta-analysis published in 2009 [42] was based on 10 studies that were also included in the current review. Thus the current study substantially extends the body of evidence reviewed as well as newly documenting the association in the HAART era.
A strength of our systematic review was the extensive quality assessment of relevant studies. Limitations included the potential for publication bias. Studies which were excluded from the meta-analysis because they did not provide essential data generally had a null result; therefore the meta-analysis may have over-estimated a more modest true association. On the other hand, the studies that were included may not have sufficiently covered the latent period for melanoma development (the time period between the onset of environmental exposure and tumor occurrence), leading to an underestimation of the association. Limited control of confounding in included studies may have influenced the results. For example, none of the included studies had data on key melanoma risk factors such as skin type, prevalence of melanocytic nevi, family history, though these factors are not associated with HIV/AIDS and are thus unlikely to have influenced the observed associations. Ethnicity, as a surrogate for skin colour, was accounted for in only 11 of the 21 included studies, yet was deemed essential for assessment of the true (unconfounded) magnitude of melanoma risk experienced by those with HIV/AIDS. Moreover, median follow-up time was not well reported by the included studies, and so was not able to be included in meaningful sensitivity analyses. We acknowledge the possibility that some cases in the post-HAART period may not have received the full recommended treatment as there were still controversies regarding treatment in the latter part of the 1990s [43]. There was also potential for double-counting of some US patient populations who contributed 51% of the weight to the pooled estimate in the post-HAART analyses, although it is very difficult to determine the existence or extent of overalap. A sensitivity analysis including in turn only one of the 3 largest US studies concerned, however, demonstrated little effect on the overall pooled estimate. Lastly, substantial heterogeneity was observed across studies. In subgroup analyses, although moderate heterogeneity still remained, the summary estimates showed positive relations in almost all subgroups. While melanoma incidence continued to rise amongst young men in nearly all parts of the world during the time period covered in these analyses, this would not have affected our results since included studies described melanoma risk in people with HIV/AIDS compared to the general population using standardized incidence ratios.
The increased risk of melanoma in populations with HIV/AIDS may be related to effects of HIV infection on the immune system although these are complex, including not only immunodeficiency, but also chronic immune activation and inflammation, and immune dysfunction and senescence [44]. We attempted to examine the influence of immunosuppression by examining the relationship in patients diagnosed with AIDS, characterized by severe immunodeficiency, however too few eligible studies were identified for the results to be informative. Similarly, there were insufficient data on duration of HIV infection, degree and duration of immunosuppression and duration of HAART to examine these factors in stratified analyses or meta-regression. One study presented results for risk of melanoma amongst individuals infected with HIV by recent CD4 count only, and reported elevated RRs for individuals with CD4 counts <200 and 201–499 cells/mL, but not for ≥500 cells/Ml [38]. Large-scale cohort studies with patient-level clinical data including CD4 count and use of HAART have the potential to better inform the management of melanoma risk (amongst other cancers) in populations with HIV/AIDS by better understanding the impact of immunosuppression, as well as how known risk factors operate differently in these populations versus the general population. Future collection of detailed clinical information on how melanomas are diagnosed (and whether it occurs as part of a physical examination for HIV/AIDS related symptoms), tumour location, and timing in relation to level of immunosuppression would greatly assist in understanding the relationship between the two diseases.
Immunosuppression is known to be associated with melanoma, shown by the increased risk of organ transplant recipients treated with immunosuppressive drugs [1]. Tumour-associated antigens are expressed by melanoma cells [45], and indirect evidence to support a role in immune surveillance derives from clinical observations including spontaneous tumour regression in some patients with primary melanoma [46] and regression associated with autoimmune skin depigmentation and vitiligo [47], observations that eventually led to the development of immunotherapeutic approaches for the treatment of metastatic disease [6], [48], [49]. Other possible explanations for the observed increased risk of melanoma include heightened medical surveillance for skin lesions including Kaposi's sarcoma, and high prevalence in the white HIV/AIDS population of lifestyle-related skin cancer risk factors such as high recreational sun exposure or use of tanning beds [5].
In summary, this meta-analysis points to a significantly increased risk of melanoma in HIV/AIDS populations in the HAART era. Whilst sub-group analyses revealed heterogeneity across some study characteristics, the pooled estimates in most sub-groups (most notable for studies that have appropriately adjusted for race/ethnicity and those rated of higher quality on the basis of our quality score) are indicative of a significantly increased risk. White skinned people with HIV/AIDS would benefit from regular screening of the skin for suspicious pigmented lesions, and since they also have a significantly increased risk of developing keratinocyte skin cancers (at least two-fold) [50] they should be counselled to avoid excessive sun exposure.
Supporting Information
Forest plot of the association between HIV/AIDS and melanoma (all studies).
(TIF)
Meta-analysis results using the weighted average method: HIV/AIDS and risk of melanoma in the pre- and post-HAART time periods.
(DOCX)
Assessment of the quality of the studies included in the meta-analysis of HIV/AIDS and risk of melanoma.
(DOCX)
Search strategy to identify cohorts of patients with HIV/AIDS reporting on risk of melanoma.
(DOCX)
PRISMA checklist.
(DOC)
Acknowledgments
We wish to thank Dr. M. Iannaacone, A/Prof. K. Khosrotehrani and Dr. C. Nagle for their critical reviews of the manuscript. CMO declares that all significant contributors have been acknowledged.
Funding Statement
LLK was funded by special purpose donations for melanoma research to the QIMR Berghofer Medical Research Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM (2007) Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 370: 59–67. [DOI] [PubMed] [Google Scholar]
- 2. Long JL, Engels EA, Moore RD, Gebo KA (2008) Incidence and outcomes of malignancy in the HAART era in an urban cohort of HIV-infected individuals. AIDS 22: 489–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, et al. (1998) Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 338: 853–860. [DOI] [PubMed] [Google Scholar]
- 4. Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, et al. (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49: 1374–1403. [DOI] [PubMed] [Google Scholar]
- 5. Flegg PJ (1990) Potential risks of ultraviolet radiation in HIV infection. Int J STD AIDS 1: 46–48. [DOI] [PubMed] [Google Scholar]
- 6. Cebon J, Gedye C, John T, Davis ID (2007) Immunotherapy of advanced or metastatic melanoma. Clin Adv Hematol Oncol 5: 994–1006. [PubMed] [Google Scholar]
- 7. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62: 1006–1012. [DOI] [PubMed] [Google Scholar]
- 9. Wong WC, Cheung CS, Hart GJ (2008) Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol 5: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, et al. (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med 147: W163–194. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation (W.H.O.) (2006) W.H.O. case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Switzerland.
- 12. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 13. Hardy RJ, Thompson SG (1998) Detecting and describing heterogeneity in meta-analysis. Stat Med 17: 841–856. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 15. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 16. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Bmj 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vella S, Schwartlander B, Sow SP, Eholie SP, Murphy RL (2012) The history of antiretroviral therapy and of its implementation in resource-limited areas of the world. AIDS 26: 1231–1241. [DOI] [PubMed] [Google Scholar]
- 18. Carpenter CC, Fischl MA, Hammer SM, Hirsch MS, Jacobsen DM, et al. (1996) Antiretroviral therapy for HIV infection in 1996. Recommendations of an international panel. International AIDS Society-USA. JAMA 276: 146–154. [PubMed] [Google Scholar]
- 19. Moore RD (2011) Epidemiology of HIV infection in the United States: implications for linkage to care. Clin Infect Dis 52 Suppl 2 S208–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cress RD, Holly EA (1997) Incidence of cutaneous melanoma among non-Hispanic whites, Hispanics, Asians, and blacks: an analysis of california cancer registry data, 1988-93. Cancer Causes Control 8: 246–252. [DOI] [PubMed] [Google Scholar]
- 21. Cooksley CD, Hwang LY, Waller DK, Ford CE (1999) HIV-related malignancies: community-based study using linkage of cancer registry and HIV registry data. Int J STD AIDS 10: 795–802. [DOI] [PubMed] [Google Scholar]
- 22. Frisch M, Biggar RJ, Engels EA, Goedert JJ (2001) Association of cancer with AIDS-related immunosuppression in adults. Jama 285: 1736–1745. [DOI] [PubMed] [Google Scholar]
- 23. Gallagher B, Wang Z, Schymura MJ, Kahn A, Fordyce EJ (2001) Cancer incidence in New York State acquired immunodeficiency syndrome patients. Am J Epidemiol 154: 544–556. [DOI] [PubMed] [Google Scholar]
- 24. Herida M, Mary-Krause M, Kaphan R, Cadranel J, Poizot-Martin I, et al. (2003) Incidence of non-AIDS-defining cancers before and during the highly active antiretroviral therapy era in a cohort of human immunodeficiency virus-infected patients. J Clin Oncol 21: 3447–3453. [DOI] [PubMed] [Google Scholar]
- 25. Hessol NA, Seaberg EC, Preston-Martin S, Massad LS, Sacks HS, et al. (2004) Cancer risk among participants in the women's interagency HIV study. J Acquir Immune Defic Syndr 36: 978–985. [DOI] [PubMed] [Google Scholar]
- 26. Newnham A, Harris J, Evans HS, Evans BG, Moller H (2005) The risk of cancer in HIV-infected people in southeast England: a cohort study. Br J Cancer 92: 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Engels EA, Pfeiffer RM, Goedert JJ, Virgo P, McNeel TS, et al. (2006) Trends in cancer risk among people with AIDS in the United States 1980-2002. AIDS 20: 1645–1654. [DOI] [PubMed] [Google Scholar]
- 28. Hessol NA, Pipkin S, Schwarcz S, Cress RD, Bacchetti P, et al. (2007) The impact of highly active antiretroviral therapy on non-AIDS-defining cancers among adults with AIDS. Am J Epidemiol 165: 1143–1153. [DOI] [PubMed] [Google Scholar]
- 29. Serraino D, Piselli P, Busnach G, Burra P, Citterio F, et al. (2007) Risk of cancer following immunosuppression in organ transplant recipients and in HIV-positive individuals in southern Europe. Eur J Cancer 43: 2117–2123. [DOI] [PubMed] [Google Scholar]
- 30. Patel P, Hanson DL, Sullivan PS, Novak RM, Moorman AC, et al. (2008) Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992–2003. Ann Intern Med 148: 728–736. [DOI] [PubMed] [Google Scholar]
- 31. Dal Maso L, Polesel J, Serraino D, Lise M, Piselli P, et al. (2009) Pattern of cancer risk in persons with AIDS in Italy in the HAART era. Br J Cancer 100: 840–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Leeuwen MT, Vajdic CM, Middleton MG, McDonald AM, Law M, et al. (2009) Continuing declines in some but not all HIV-associated cancers in Australia after widespread use of antiretroviral therapy. AIDS 23: 2183–2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Powles T, Robinson D, Stebbing J, Shamash J, Nelson M, et al. (2009) Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol 27: 884–890. [DOI] [PubMed] [Google Scholar]
- 34. Franceschi S, Lise M, Clifford GM, Rickenbach M, Levi F, et al. (2010) Changing patterns of cancer incidence in the early- and late-HAART periods: the Swiss HIV Cohort Study. Br J Cancer 103: 416–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vogel M, Friedrich O, Luchters G, Holleczek B, Wasmuth JC, et al. (2011) Cancer risk in HIV-infected individuals on HAART is largely attributed to oncogenic infections and state of immunocompetence. Eur J Med Res 16: 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Simard EP, Pfeiffer RM, Engels EA (2010) Spectrum of cancer risk late after AIDS onset in the United States. Arch Intern Med 170: 1337–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Seaberg EC, Wiley D, Martinez-Maza O, Chmiel JS, Kingsley L, et al. (2010) Cancer incidence in the multicenter AIDS Cohort Study before and during the HAART era: 1984 to 2007. Cancer 116: 5507–5516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Silverberg MJ, Chao C, Leyden WA, Xu L, Horberg MA, et al. (2011) HIV infection, immunodeficiency, viral replication, and the risk of cancer. Cancer Epidemiol Biomarkers Prev 20: 2551–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calabresi A, Ferraresi A, Festa A, Scarcella C, Donato F, et al.. (2013) Incidence of AIDS-defining cancers and virus-related and non-virus-related non-AIDS-defining cancers among HIV-infected patients compared with the general population in a large health district of northern Italy, 1999–2009. HIV Med. [DOI] [PubMed]
- 40. Bedimo RJ, McGinnis KA, Dunlap M, Rodriguez-Barradas MC, Justice AC (2009) Incidence of non-AIDS-defining malignancies in HIV-infected versus noninfected patients in the HAART era: impact of immunosuppression. J Acquir Immune Defic Syndr 52: 203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Engels EA, Biggar RJ, Hall HI, Cross H, Crutchfield A, et al. (2008) Cancer risk in people infected with human immunodeficiency virus in the United States. Int J Cancer 123: 187–194. [DOI] [PubMed] [Google Scholar]
- 42. Shiels MS, Cole SR, Kirk GD, Poole C (2009) A meta-analysis of the incidence of non-AIDS cancers in HIV-infected individuals. J Acquir Immune Defic Syndr 52: 611–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yeni PG, Hammer SM, Carpenter CC, Cooper DA, Fischl MA, et al. (2002) Antiretroviral treatment for adult HIV infection in 2002: updated recommendations of the International AIDS Society-USA Panel. JAMA 288: 222–235. [DOI] [PubMed] [Google Scholar]
- 44. Dubrow R, Silverberg MJ, Park LS, Crothers K, Justice AC (2012) HIV infection, aging, and immune function: implications for cancer risk and prevention. Curr Opin Oncol 24: 506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Houghton AN, Gold JS, Blachere NE (2001) Immunity against cancer: lessons learned from melanoma. Curr Opin Immunol 13: 134–140. [DOI] [PubMed] [Google Scholar]
- 46. Kalialis LV, Drzewiecki KT, Klyver H (2009) Spontaneous regression of metastases from melanoma: review of the literature. Melanoma Res 19: 275–282. [DOI] [PubMed] [Google Scholar]
- 47. Le Gal FA, Avril MF, Bosq J, Lefebvre P, Deschemin JC, et al. (2001) Direct evidence to support the role of antigen-specific CD8(+) T cells in melanoma-associated vitiligo. J Invest Dermatol 117: 1464–1470. [DOI] [PubMed] [Google Scholar]
- 48. Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, et al. (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, et al. (2012) Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 366: 2443–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Silverberg MJ, Leyden W, Warton EM, Quesenberry CP Jr, Engels EA, et al. (2013) HIV infection status, immunodeficiency, and the incidence of non-melanoma skin cancer. J Natl Cancer Inst 105: 350–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plot of the association between HIV/AIDS and melanoma (all studies).
(TIF)
Meta-analysis results using the weighted average method: HIV/AIDS and risk of melanoma in the pre- and post-HAART time periods.
(DOCX)
Assessment of the quality of the studies included in the meta-analysis of HIV/AIDS and risk of melanoma.
(DOCX)
Search strategy to identify cohorts of patients with HIV/AIDS reporting on risk of melanoma.
(DOCX)
PRISMA checklist.
(DOC)