Abstract
Objectives
To classify older emergency department (ED) patients by health care use and to examine associations between group membership and future ED visits and hospital admissions.
Design
Secondary analysis
Setting
Medicare Current Beneficiary Survey
Participants
Adults aged > = 65 years with at least one treat-and-release ED visit between 1/1/00 and 9/30/07 (N = 4,964).
Measurements
Measures of health service use included (1) primary care visits, (2) treat-and-release ED visits, and (3) hospital days in the 12 months preceding the index ED visit.
Results
Five groups of ED patients with distinct patterns of health service use were identified. "Primary Carederly" (39%) had low rates of ED and hospital use and a high mean number of primary care (PC) visits. “Wellderly" (34%) had fewer visits of all types compared to other groups. “Chronically Illderly” (14%) patients had the highest mean number of PC visits and hospital days. “Acute Carederly” (9.8%) had lowest mean number of PC visits but higher ED visits and hospital days than all other groups except the Sickest Elderly. Patients in the “Sickest Elderly” group (3.2%) had the highest number of ED visits; mean number of hospital days was more than four times that of any other group. “Primary Carederly” and “Wellderly” had a lower risk of hospital admission within 30 days of the index ED visit, while all other groups had a higher risk.
Conclusion
Among older patients released from an ED, group membership was associated with future health services use. Classification of patients using readily available previous visit data may improve targeting of interventions to improve patient outcomes.
Keywords: emergency department, older adults, latent class analysis
INTRODUCTION
Older adults make up 13.1% of the United States population and this will grow to 19.3% by 2030 (1). The rapidly aging population is adding stress to an already overburdened health care system. There is widespread agreement that changes are needed to improve health outcomes for older patients while simultaneously reducing costs. An important site to consider when examining older adults’ use of health care is the Emergency Department (ED). Despite being physically attached to a hospital in many cases, the ED is a frequent site of ambulatory care for older Americans (2). Approximately 17% of community dwelling adults aged 65 or older have at least one treat-and-release ED visit each year. A growing body of evidence suggests that these are important events for seniors, because the time afterwards is fraught with risks including functional decline, repeat ED visits, and hospitalizations. Overall, 1 in 3 older patients return to the ED, are admitted to a hospital or nursing home, or die within 90 days following a treat-and-release ED visit (3).
A number of studies have found that previous ED visits and hospitalizations are independent predictors of subsequent unscheduled health care use after an ED visit (3–7). Indeed, this is consistent with a familiar axiom in health services research, “Previous health care use predicts future health care use”. A limitation of many of these studies is that only one type of health service use was investigated at a time. There is a need to account for other types of encounters such as primary care (PC) visits and to examine these visits in context with one another. Identifying patients with similar patterns of health service use may provide novel insights into groups of ED patients that may benefit from additional or alternative services such as disease self-management or care management programs.
Thus, the overall goal of this study was to examine patterns of health service use in older ED patients in a national sample of age-eligible Medicare beneficiaries. Specific study objectives were to identify groups of older ED patients with similar patterns of health care use in the previous year, to identify patient-level predictors of group membership, and to examine the associations between group membership and future ED visits and hospital admissions.
METHODS
Data Source
This study was a secondary analysis of data from Medicare Current Beneficiary Survey (MCBS) Cost and Use files (1999–2007) and linked Medicare claims. The MCBS is a continuous survey of a nationally representative sample of Medicare beneficiaries drawn from the Centers for Medicare and Medicaid Services (CMS) enrollment file (8). The MCBS sample is stratified by age (with over-sampling of persons 85 and older) and drawn within zip code clusters designated as primary sampling units (8). Beneficiaries are interviewed in person three times per year (if the person is unable to answer the questions, he or she is asked to designate a proxy respondent, usually a family member or close acquaintance who is familiar with his or her care). The results from the survey are then combined with Medicare administrative claims data to provide additional information such as health care utilization event dates (8). MCBS patient-reported information and associated claims data were obtained from CMS following approval of data use agreement # 21407. Approval for the study was obtained from the Institutional Review Board of Duke University Medical Center.
Sample
We included MCBS subjects who were community-dwelling, aged 65 or older, enrolled in Medicare Fee for Service, and discharged alive from the ED between 2000 and 2006. Residents of long-term care facilities at the time they enrolled in MCBS were excluded because a different data collection instrument was used for these individuals. Subjects enrolled in a Medicare HMO plan were excluded because it was not possible to determine the dates of their health service use. MCBS operates on a 4-year rotating panel design; therefore, subjects enter and leave the survey each year. To be included in this analysis, participants were required to be in the survey the year preceding and following their ED visit, so that all relevant study data would be available. The final analytic sample size was 4,964 patients.
Measures
Measures of health service use included (1) primary care visits, (2) treat-and-release ED visits, and (3) hospital days in the 12 months preceding the index ED visit. Primary care visits included location of service codes for internal medicine, family medicine, geriatric medicine, and general practice. Dates of health service use were identified in CMS standard analytic files which have been linked to MCBS, from which other study variables were obtained. Demographic and health status variables included age, race, sex, and number of baseline chronic health conditions (self-reported) of the following 12: hypertension, arthritis, coronary heart disease, osteoporosis, diabetes, non-skin cancer, diabetes mellitus, chronic obstructive pulmonary disease (COPD), stroke, Alzheimer’s dementia, and Parkinson’s disease. Data for all independent variables were obtained from MCBS Cost and Use files during the year preceding the index ED visit and associated Medicare claims.
Analysis
Sample weights were applied; all proportions presented are weighted. To examine patterns of health service use in this sample of older ED patients, we estimated latent class analysis (LCA) models. LCA models differ from traditional regression, discriminant, and log linear models in that variation on observed indicators is modeled as a function of membership in unobserved (latent) classes (9,10). Unlike standard clustering techniques, LCA allows for statistical testing of model fit and class membership is probabilistic, with membership probabilities computed from the estimated model parameters (11). In the initial step of our analyses, we estimated a series of increasingly complex models (adding classes) to determine the optimal number of latent classes. Following standard practice we used the Bayesian Information Criterion (BIC) together with substantive interpretability (i.e. a discernible, potential meaning or significance of the class) in making this determination (11).
After defining the latent classes by measures of health service use, our next analytic objective was to determine how the set of classifying variables (measures of health service use), demographic and chronic conditions varied by latent class group. For this analysis, bivariate significance tests were obtained by assigning each sample member to her/his modal class and testing whether the prevalence of each of the set of demographic and health status variables were significantly different for members of that class compared with the other classes. To preserve Type I error, a 4-df omnibus test was conducted for each measure using either logistic regression or Ordinary Least Squares regression, as appropriate. If the omnibus test had a P-value ≤ 0.05 then the bivariate one degree of freedom tests for each latent class against all others were conducted.
Finally, proportional hazards models were used to examine the relationship between class membership and (1) first repeat treat-and-release ED visit and (2) first hospital admission within 30 days of the index visit. Latent class analyses were performed with the Latent Gold software package (Statistical Innovations, Belmont, MA) which provides likelihood-based information indices (the Akaike Information Criterion, the BIC, and the Consistent Akaike Information Criterion) to aid in assessing the number of latent classes needed to fit the data (14). The proportional hazards analyses were conducted with STATA v.10, and the remainder of the analyses were conducted using SAS v 9.3.
RESULTS
Determining the Number of Latent Classes
The BIC continually decreased as the number of classes increased; however, magnitude of changes in the BIC was reduced starting with the four-class model. The smallest class in the five-class model contained 3% of the entire sample, and given that the data set contained sufficient sample size to adequately estimate this small but independent class which had a distinct and interpretable pattern of use, we selected the five-class option as the final analytic classification model.
Characteristics of Class Members
After the 5 groups were established, participants were assigned to the group to which he or she had the highest calculated probability of membership; misclassification error was 0.08 and mean membership probabilities ranged from 0.91 to 0.98 across classes. Demographics, health status, and utilization variables for each group are displayed in Table 1. All characteristics discussed in the following paragraph were significant (P<0.5) when each group was compared to all others. The first group ["Primary Carederly", 39%] used less ED and hospital care, but had higher mean PC use (6.2 visits). Members of this group were more likely to be female, live alone and have more chronic conditions. The second group ["Wellderly", 34%] had fewer health care visits of all types and members were on average younger (mean age 78.3), more likely to be male, and had fewer chronic conditions. The third group [“Chronically Illderly”, 14%] had similar ED use, but higher mean hospital days (5.4) and nearly double the mean number of PC visits (7.9). Members of this group were more likely to be older, white, and have more chronic conditions, especially heart disease (45%), diabetes (30%), and COPD (24%). The fourth group [“Acute Carederly”, 9.8%] had fewer PC visits but higher mean number of ED visits (0.3) and hospital days (8.3) compared to all others. These group members were more likely to be male, non-white and less likely to live alone. The final group ["Sickest Elderly", 3.2%] had high use of all types of care, particularly the hospital (mean 38.4 days), and were more likely to be non-white and have more chronic conditions.
Table 1.
Characteristics of Five Classes Generated According to Health Service Use
| Health Service Use in Previous 12 months |
Total Sample, N=4,964 |
Primary Carederly, n=1941 (39.1%) |
Wellderly, n=1684 (33.9%) |
Chronically Illderly, n=692 (13.9%) |
Acute Carederly, n=486 (9.8%) |
Sickest Elderly, n=161 (3.2%) |
|---|---|---|---|---|---|---|
|
# PC visits, mean (SD) |
4.0 (4.4) | 6.2 (3.5)* | 0.8 (0.9)* | 7.9 (5.8)* | 1.1 (1.4)* | 5.0 (4.5)* |
|
# ED visits, mean (SD) |
0.10 (0.5) | 0.06 (0.3)* | 0.05 (0.3)* | 0.12 (0.5) | 0.29 (1.2)* | 0.34 (1.0)* |
|
# Inpatient days, mean (SD) |
2.8 (8.4) | 0.04 (0.2)* | 0.03 (0.2)* | 5.42 (3.6)* | 8.3 (5.0)* | 38.4 (22.2)* |
|
Demographic and Health Characteristics |
Total Sample |
Primary Carederly |
Wellderly |
Chronically Illderly |
Acute Carederly |
Sickest Elderly |
| Age, mean (SD) | 78.9 (7.2) | 79.0 (7.1) | 78.3 (7.2)* | 79.8 (7.1)* | 79.4 (7.7) | 78.8 (6.6) |
| % Male | 39.7 | 33.9* | 44.4* | 39.5 | 45.5* | 44.7 |
| % White | 86.9 | 87.0 | 87.4 | 90.8* | 81.9* | 79.5* |
| % Income <10K | 21.4 | 20.9 | 20.6 | 21.1 | 24.5 | 27.3 |
| % Live alone | 36.5 | 39.4* | 35.5 | 35.0 | 32.3* | 31.1 |
|
Number chronic conditions, mean (SD) |
2.9 (1.5) | 3.0 (1.4)* | 2.5 (1.5)* | 3.3 (1.4)* | 3.3 (1.6)* | 3.6 (1.5)* |
|
Baseline Chronic Conditions |
||||||
| Hypertension | 70.4 | 74.1* | 62.7* | 75.4* | 72.4 | 79.5* |
| Arthritis | 69.4 | 73.4* | 62.6* | 73.8* | 68.9 | 75.2 |
| Heart disease | 35.4 | 34.3 | 29.2* | 45.4* | 45.3* | 40.4 |
| Osteoporosis | 24.6 | 27.7* | 19.7* | 27.9* | 23.7 | 26.7 |
| Diabetes | 24.2 | 25.9* | 17.8* | 30.1* | 28.0* | 35.4* |
| Cancer | 23.2 | 23.0 | 20.4 | 26.0 | 27.4* | 28.0 |
|
Chronic Obstructive Pulmonary Disease |
19.6 | 18.6 | 16.2* | 23.8* | 27.4* | 27.3* |
| Stroke | 18.2 | 16.5* | 14.8* | 22.8* | 24.5* | 34.8* |
| Dementia | 6.3 | 5.3* | 5.8 | 5.8 | 10.9* | 12.4* |
|
Parkinson’s disease |
2.3 | 2.0 | 2.0 | 2.5 | 3.5 | 4.4 |
PC = primary care, SD = standard deviation
P < 0.05; each group was compared to all others (ie the remainder of the sample)
All the four degree of freedom omnibus tests exploring distributional differences by latent class were significant except for the percent with income less than $10,000; no 1-df testing was done for this variable, but the latent group percentages are displayed for descriptive purpos
Relationship between Class Membership and Outcomes
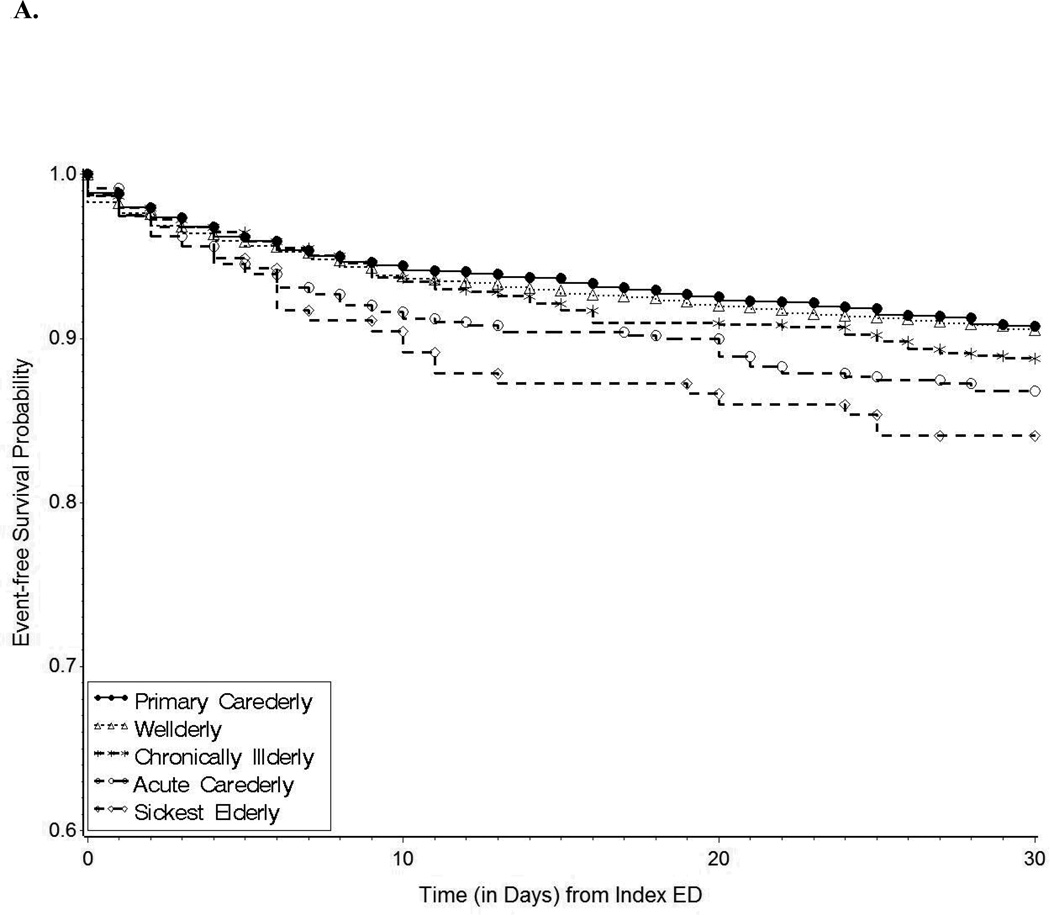
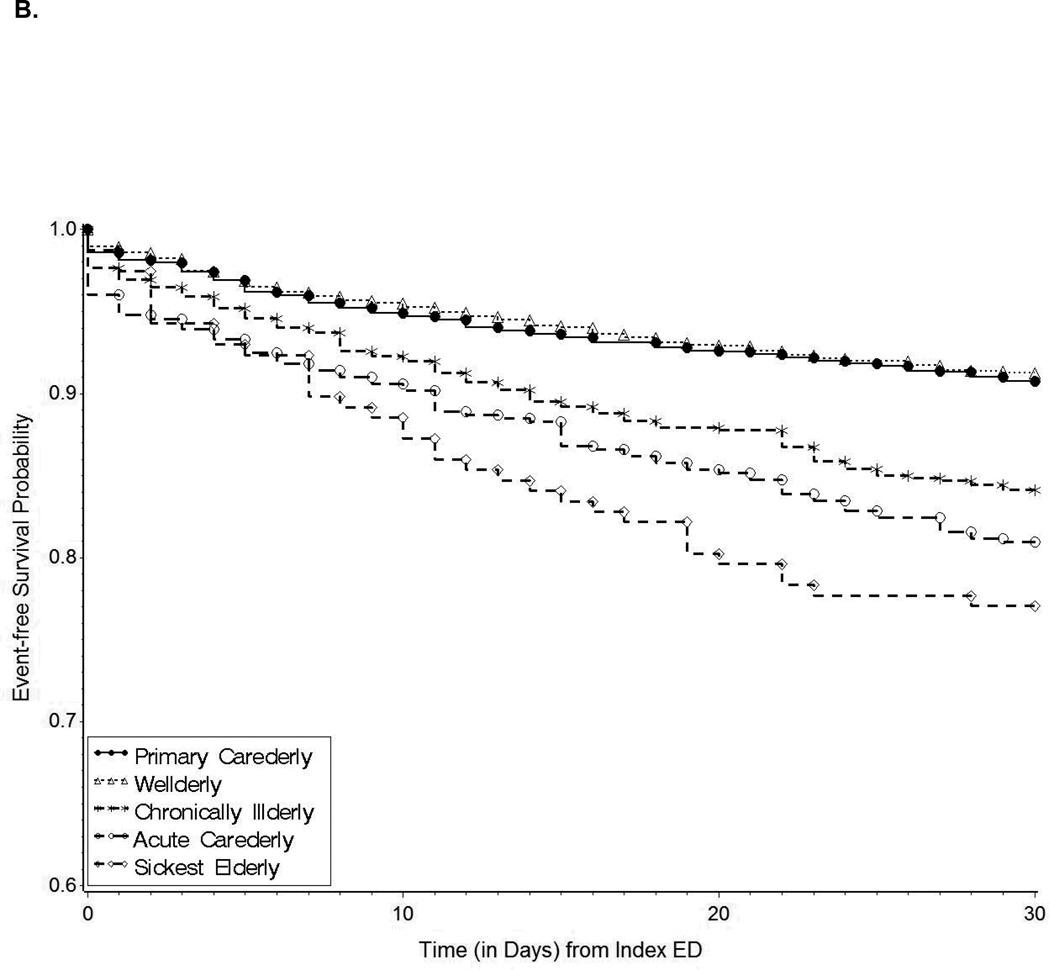
Overall 11.4% of older adults in the sample were hospitalized within 30 days of the index ED visit and 10.2% returned to the ED. The risk of a repeat treat-and-release ED visit was higher among members of the “Acute Carederly” and “Sickest Elderly” groups (Table 2). As displayed in Figure 1A, the excess risk for these two groups was apparent within one week after the index ED visit and was maintained throughout the 30-day observation period. Membership in the “Chronically Illderly”, “Acute Carederly”, and “Sickest Elderly” groups was associated with higher risk of hospitalization, compared to all others (Figure 1B). One in four patients in the “Sickest Elderly” group was hospitalized within 30 days of being released from the ED at their index visit.
Table 2.
Association between Group Membership and Future Emergency Department (ED) Visits and Hospital Admissions
| Repeat ED visit | Hospital Admission | |||
|---|---|---|---|---|
| Latent Class Group |
% | Hazard Ratio (95% CI) |
% | Hazard Ratio (95% CI) |
| Primary Carederly | 9.29 | 0.87 (0.72, 1.03) | 8.75 | 0.68 (0.57, 0.81) |
| Wellderly | 8.95 | 0.84 (0.69, 1.03) | 8.60 | 0.68 (0.56, 0.83) |
|
Chronically Illderly |
11.21 | 1.17 (0.93, 1.48) | 16.18 | 1.59 (1.28, 1.96) |
| Acute Carederly | 12.83 | 1.33 (1.03, 1.73) | 18.83 | 1.79 (1.44, 2.26) |
| Sickest Elderly | 16.72 | 1.80 (1.19, 2.73) | 24.44 | 2.47 (1.84, 3.31) |
Separate models fit for each group; thus hazard ratios are for each designated group compared to remainder of the sample.
Figure 1.
Event-free survival probability according to group for 1A) repeat treat and release Emergency Department (ED) visits; and 1B) hospitalizations within 30 days.
DISCUSSION
Among this cohort of age-eligible Medicare beneficiaries with a treat-and-release ED visit, we identified five groups of patients with distinct patterns of health service utilization. The largest group (39%), the “Primary Carederly”, consists of patients with frequent primary care use but low hospital and ED use. The second group (34%), the “Wellderly”, has the lowest utilization in all categories of care and fewer chronic conditions. In contrast, the members of the third group, called “Chronically Illderly”, have high PC and hospital use, and a higher chronic disease burden. The fourth group (9.8%), the “Acute Carederly”, showed very low PC utilization but high hospital use (mean 8.3 days). The smallest group “Sickest Elderly,” showed average PC use but the highest utilization of the hospital and ED. In the U.S., a small number of chronic conditions account for a substantial portion of healthcare spending (14); however there is tremendous variability in use patterns among individuals. The results of this study extend prior work (12,13) by providing evidence of clinically meaningful clusters of healthcare utilization among older ED patients in a nationally representative, population-based sample.
An important finding is that group membership predicts risk of return to the hospital or ED. Based on past health visits alone, it can be anticipated that 73% of ED patients aged 65 or older [“Primary Carederly” + “Wellderly” groups] have low to average risk of subsequent return. This large group could be managed with usual ED discharge planning dependent on individual clinical circumstances. The remaining 27% of patients had higher than average risk of subsequent return, especially hospitalization, and may benefit from more intensive post-ED follow-up (15). The risk of hospital admission within 30 days was 2.4 times higher in the “Sickest Elderly” group, compared to all others. For this small group, rapid deployment of home based support services to prevent future hospitalization after an ED visit may be warranted (15). Hospitalization is extremely costly. In 2010, aggregate Medicare Fee for Service spending on inpatient care exceeded 146 billion dollars (16). The high prevalence of stroke and dementia in the “Sickest Elderly” group is consistent with mounting evidence about the high healthcare utilization and costs associated with dementia (17). This group may also benefit from palliative care services when appropriate, given the demonstrated clinical benefit and cost-savings associated with these programs (18).
The potential clinical applicability of our study stems from the fact that all of the variables that we used to construct the latent class models in this analysis are readily available in most electronic health record systems. The next step in moving these findings towards utility in clinical practice would be to perform a validation study, ideally in a separate population, to examine the predictive validity of groups that were established based on explicit criteria. If validated, these models offer health systems and policy makers a new and powerful means of predicting future use patterns based on readily available data. Moreover, understanding these use patterns may suggest opportunities for intervention (e.g., future work could test the hypothesis that days of hospitalization in the “sickest elderly” group may be reduced through interventions that increase this group’s utilization of primary care).
There are several limitations to this study that merit acknowledgement. In LCA, class assignment is based on probability. High mean membership probabilities (0.91–0.98) and low misclassification error (0.08) suggest good separation among classes and minimal bias (19–23), but a clinician or administrator faced with a patient in the ED may have a difficult time determining which of the 5 classes the individual most closely resembles. Also some of the differences between groups, while statistically significant, may not be clinically meaningful. A validation study would be required before these groups could be recommended for clinical use. Chronic conditions were identified based on self-report. A previous study found that 59% of patients with a CMS claim for dementia in the previous year also had self- or proxy-reported dementia; (24) thus the true prevalence of dementia in this population may be higher than the 6.3% reported here. Next, in models predicting hospital and ED use, we did not account for other factors that are known to influence utilization such as geography. Finally, changes in health care delivery since the study period may affect the generalizability of our findings.
These limitations notwithstanding, this study demonstrates an important use of LCA to identify groups of older ED patients with unique patterns of previous health service use. Group membership was predictive of future unscheduled health care use, providing a compelling example of how readily available data (frequency and type of health care visits) from electronic health records can be combined into meaningful clusters using LCA. This type of innovative use of electronic health records represents a new frontier in health information technology and is consistent with a main goal of the widespread implementation of electronic medical record systems: improving the quality and cost of care provided to seniors (25).
ACKNOWLEDGMENTS
Funding: This research was supported by the Brookdale Foundation and conducted, in part, while Dr. Hastings was supported by a VA Health Services Research and Development Career Development Award (RCD 06-019). Dr. Whitson was supported by K23 AG032867 from the National Institute on Aging. Dr. Johnson was supported by a K08AG028975 from the National Institute on Aging.
Sponsor’s Role: None.
Footnotes
Portions of this work were presented at the Annual Scientific Meeting of the American Geriatrics Society in Seattle, WA on May 3, 2012 and the VA HSR&D Career Development Awardee Meeting in National Harbor, MD on July 16, 2012.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions
Each author contributed intellectually or practically to this research.
S. Nicole Hastings - study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript
Heather Whitson - study concept and design, analysis and interpretation of data, and preparation of manuscript
Richard Sloane - study concept and design, analysis and interpretation of data, and preparation of manuscript
Lawrence Landerman - study concept and design, analysis and interpretation of data, and preparation of manuscript
Carolyn Horney - study concept and design, analysis and interpretation of data, and preparation of manuscript
Kimberly Johnson - study concept and design, analysis and interpretation of data, and preparation of manuscript
Additionally, Caroline Connor provided editorial assistance.
REFERENCES
- 1.Greenberg S. [Accessed January 26, 2013];Administration on Aging U.S. Department of Health and Human Services. A profile of older Americans. 2011 Available at: www.aoa.gov/aoaroot/aging_statistics/Profile/2011/docs/2011profile.pdf.
- 2.McCaig LF, Burt CW. Advanced Data from Vital and Health Statistics; No. 358. Hyattsville: National Center for Health Statistics; 2005. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. [Google Scholar]
- 3.Hastings SN, Oddone EZ, Fillenbaum G, et al. Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care. 2008;46:771–777. doi: 10.1097/MLR.0b013e3181791a2d. [DOI] [PubMed] [Google Scholar]
- 4.Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238–247. doi: 10.1067/mem.2002.121523. [DOI] [PubMed] [Google Scholar]
- 5.Hastings SN, Schmader KE, Sloane RJ, et al. Adverse health outcomes after discharge from the emergency department—incidence and risk factors in a veteran population. J Gen Intern Med. 2007;22:1527–1531. doi: 10.1007/s11606-007-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCusker J, Bellavance F, Cardin S, et al. The prediction of hospital utilization among elderly patients during the 6 months after an emergency department visit. Ann Emerg Med. 2000;36:438–445. doi: 10.1067/mem.2000.110822. [DOI] [PubMed] [Google Scholar]
- 7.Friedmann PD, Jin L, Karrison TG, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19:125–129. doi: 10.1053/ajem.2001.21321. [DOI] [PubMed] [Google Scholar]
- 8.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev. 1994;15:153–163. [PMC free article] [PubMed] [Google Scholar]
- 9.Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika. 1974;61:215–231. [Google Scholar]
- 10.Land KC. Introduction to the Special Issue on Finite Mixture Models. Sociol Methods Res. 2001;29:275–281. [Google Scholar]
- 11.Vermunt JK, Magidson J. Latent Class Cluster Analysis. Ch. 3. In: Hagenaars JA, Mccutcheon AL, editors. Advances in Latent Class Analysis. Cambridge University Press; 2000a. [Google Scholar]
- 12.Huang J, Weng R, Lai C, et al. Exploring medical utilization patterns of emergency department users. J Formos Med Assoc. 2008;107:119–128. doi: 10.1016/S0929-6646(08)60125-4. [DOI] [PubMed] [Google Scholar]
- 13.Hastings SN, Horney C, Landerman LR, et al. Exploring patterns of health service use in older emergency department patients. Acad Emerg Med. 2010;17:1086–1092. doi: 10.1111/j.1553-2712.2010.00870.x. [DOI] [PubMed] [Google Scholar]
- 14.The High Concentration of U.S. Health Care Expenditures: Research in Action, Issue 19. Rockville, MD: Agency for Healthcare Research and Quality; 2006. Jun, [Accessed July 1, 2013]. Available at: http://www.ahrq.gov/research/findings/factsheets/costs/expriach/index.html. [Google Scholar]
- 15.Hastings SN, Heflin MT. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med. 2005;12:978–986. doi: 10.1197/j.aem.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed July 2, 2013];Medpac: A data book: Healthcare spending and the Medicare Program. Available at: http://www.medpac.gov/chapters/Jun12DataBookSec6.pdf.
- 17.Hurd MD, Martorell P, Delavande A, et al. Monetary costs of dementia in the United States. N Engl J Med. 2013;368:1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with us hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 19.Henry KL, Muthén B. Multilevel latent class analysis: An application of adolescent smoking typologies with individual and contextual predictors. Struct Equ Modeling. 2010 Apr 1;17:193–215. doi: 10.1080/10705511003659342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bouwmeester S, Sijtsma K, Vermunt JK. Latent class regression analysis for describing cognitive developmental phenomena: An application to transitive reasoning. Eur J Develop Psychol. 2004;1:67–86. [Google Scholar]
- 21.Hybels CF, Blazer DG, Pieper CF, et al. Profiles of depressive symptoms in older adults diagnosed with major depression: A latent cluster analysis. Am J Geriatr Psychiatry. 2009;17:387–396. doi: 10.1097/JGP.0b013e31819431ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Political Analysis. 2010;18:450–469. [Google Scholar]
- 23.Asparouhov T, Muthen B. Auxiliary Variables in Mixture Modeling: A 3-Step Approach Using Mplus.Mplus Web Notes: No 15 Version 6. 2013. Feb 7, [Google Scholar]
- 24.Gruber-Baldini AL, Stuart B, Zuckerman IH, et al. Treatment of dementia in community-dwelling and institutionalized medicare beneficiaries. J Am Geriatr Soc. 2007;55:1508–1516. doi: 10.1111/j.1532-5415.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 25.Atkins D, Cullen T. The future of health information technology: Implications for research. Med Care. 2013;51:S1–S3. doi: 10.1097/MLR.0b013e3182848a52. [DOI] [PubMed] [Google Scholar]