Abstract
Background
Prior studies have demonstrated that race and insurance status predict inpatient trauma mortality, but have been limited by their inability to adjust for direct measures of socioeconomic status (SES) and comorbidities. Our study aims to identify whether a relationship exists between SES and inpatient trauma mortality, after adjusting for known confounders.
Methods
Trauma patients aged 18–65 years with Injury Severity Scores (ISS) ≥ 9 were identified using the 2003–2009 Nationwide Inpatient Sample. Median household income (MHI) by zip code, available by quartiles, was used to measure SES. Multiple logistic regression analyses were performed to determine odds of inpatient mortality by MHI quartile, adjusting for ISS, type of injury, comorbidities, and patient demographics.
Results
267,621 patients met inclusion criteria. Patients in lower wealth quartiles had significantly higher unadjusted inpatient mortality compared with the wealthiest quartile. Adjusted odds of death were also higher compared with the wealthiest quartile for Q1 (OR 1.13, 95% CI 1.06–1.20), Q2 (OR 1.09, 95% CI 1.02–1.17), and Q3 (OR 1.11, 95% CI 1.04–1.19).
Conclusions
Median household income predicts inpatient mortality after adult trauma, even after adjusting for race, insurance status, and comorbidities. Efforts to mitigate trauma disparities should address SES as an independent predictor of outcomes.
Introduction
Mortality from traumatic injury has risen over the past decade. African-Americans are disproportionately affected by mortality from injury, having experienced a 20% increased rate of mortality from all injury causes over the past ten years.1 Mortality is further increased for uninsured versus insured patients, regardless of race, after both blunt and penetrating trauma.2–4 Mechanism of injury, injury severity, hospital trauma center status, and patient co-morbidities are also known predictors of mortality after trauma. A recent systematic review and meta-analysis by Haider et al. further highlighted disparities in trauma mortality, with minorities, the uninsured, and lower median household income earners experiencing increased mortality.5
Socioeconomic status (SES) is associated with worse health outcomes and higher mortality across a range of diseases, and this relationship holds for various measures of SES, including education, income, and occupational status.6,7 In particular, there has been a longstanding inverse correlation between SES and the prevalence of and mortality from specific diseases such as cardiovascular disease, cancer, and respiratory disease.8–10 Low SES has been found to be a predictor of all-cause mortality, as well as mortality from diabetes, accidents, suicides, and homicides, among others.11
Literature on the association between SES and trauma outcomes is limited and has focused on work-related injuries. For instance, Cubbin et al. found that blue-collar workers had a weighted age-adjusted injury mortality rate of 71.4 compared with 44.3 among white-collar workers.12 The mortality rate was more than double among patients with low income-to-needs ratios (109.5) compared with those with high income-to-needs ratios (52.2). A large Canadian study also found that low income, low education, and low or no occupation status was associated with increased mortality rates from unintentional injury.13 Canadians in the poorest income quintile had an age-standardized mortality rate (ASMR) per 100,000 person-years at risk of 64.1% for males and 35.1% for females compared with 38.4% for males and 23.0% for females in the richest income quintile.
While SES has been found to be an important predictor of mortality across a wide range of diseases, the link between SES and inpatient mortality following traumatic injury has not been well-studied in the American population. Moreover, various studies that have shown links between trauma mortality and factors such as race, insurance status, and trauma-center status have been limited by their inability to adjust for direct measures of SES, as well as comorbidities. While some of these studies use insurance status as a proxy, this measure may not be sufficient to fully capture socioeconomic status. The objective of this study was to determine whether a relationship exists between SES and inpatient mortality after adjusting for known confounders, including comorbidities.
Methods
Patient Population and Study Design
This study was a retrospective analysis of the Nationwide Inpatient Sample (NIS) database of the Healthcare Cost and Utilization Project (HCUP) This database includes data from over 1,000 hospitals in up to 44 states and approximately 8 million inpatient hospital stays each year.14
Trauma patients between the ages of 18–65 with moderate to severe injuries as measured by the Injury Severity Score (ISS ≥9) in the 2003–2009 database were included in the study. Only patients treated in hospitals designated as American College of Surgeons (ACS)/State verified trauma centers were included in the study and patients missing any data were excluded. There was very little missing data, which made it possible to undertake a complete case analysis. The outcome measure assessed was mortality following traumatic injury that warranted a hospital inpatient stay. Trauma patients were identified using the International Classification of Diseases, 9th edition (ICD-9) codes ≥800 and <905. The age group was chosen to ensure a focus on adult trauma, as opposed to trauma in elderly patients, who have been shown to be affected differently by trauma compared with adult patients. Only those patients with an ISS of at least 9 were included to ensure that patients were at risk of dying as a result of their injuries. ISS was generated for the dataset using the ICD-9 PIC program.
Median household income (MHI), available by zip code, was used as a proxy for a more direct measure of socioeconomic status. Patients were grouped into the four available quartiles of MHI provided in the database, which ranged from low MHI to high MHI (Q1=0–25%, $1–40,999; Q2=25–50%, $41,000–50,999; Q3=50–75%, $51,000–66,999; Q4=75–100%, $67,000+). MHI values were obtained from the 2009 database, with slight differences in absolute dollar values for each year analyzed. Q4, the wealthiest quartile, was used as the reference group for the multivariate analyses.
Statistical Analyses
An exploratory data analysis was performed to determine the baseline participant characteristics, including age, gender, race/ethnicity, and insurance status. Injury characteristics were also analyzed, including ISS, Charlson Comorbidity Index (CCI), and type of injury. Continuous and categorical variables were compared by ANOVA and Chi-square tests.
Multiple logistic regression analyses were performed to determine the relative odds of inpatient mortality for the different MHI quartiles, adjusting for ISS, type of injury (blunt versus penetrating trauma), CCI, and patient demographics, including age, sex, race, and insurance status. The CCI was developed using a preexisting Stata module.15 An interaction term for race and insurance was also included in the model to account for the interaction between these two variables.
A multivariate analysis stratified by two groups of years (2003–2006 and 2007–2009) of injury/inpatient stay was also completed to examine whether inpatient mortality among MHI quartiles had changed over the course of the time period analyzed. We also analyzed length of stay (LOS) in the hospital, adjusting for the same confounders, to determine whether patients in the poorer quartiles had increased LOS as compared to Q4.
All statistical analyses were completed using Stata/IC Version 12 (StataCorp LP, College Station, Texas, USA). This study was reviewed and approved by the Institutional Review Board at the Johns Hopkins University School of Medicine.
Results
267,621 patients between the ages of 18–65 and with an ISS ≥ 9 met inclusion criteria, with the highest number of contributing patients belonging to the poorest quartile (n=83,714) and the lowest number of contributing patients belonging to the wealthiest quartile (n=52,562). The mean age of patients increased slightly with increasing wealth of the quartiles (Q1 mean age=40, interquartile range=27–53; Q2 mean age=41, interquartile range=27–54; Q3 mean age=42, interquartile range=28–54; Q4 mean age=43, interquartile range=29–56). Among all quartiles, there were more male patients than female patients, with a decrease in the ratio of male to female patients as wealth of the quartile increased (Table 1). Insurance status closely paralleled wealth, with higher proportions of Medicaid and Self-Pay patients in the lower wealth quartiles. There was also an increase in the proportion of white patients and a decrease in the proportion of Black, Hispanic, and Native American patients with increasing quartile wealth.
Table 1.
Patient Demographics Stratified by SES Quartile
| Median Household Income Quartile (267,621 patients) | ||||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Number of Patients | 83,714 | 68,932 | 62,413 | 52,562 |
| Mean Age, yr (interquartile range) | 40 (27–53)* | 41 (27–54) | 42 (28–54) | 43 (29–56) |
| Gender, n (%) | ||||
| Male | 60,813 (72.64)‡ | 48,382 (70.19) | 43,320 (69.41) | 35,102 (66.78) |
| Female | 22,901 (27.36) | 20,550 (29.81) | 19,093 (30.59) | 17,460 (33.22) |
| Race/Ethnicity, n (%) | ||||
| White | 44,790 (53.50)† |
48,968 (71.04) | 46,389 (74.33) | 40,836 (77.69) |
| Black | 19,719 (23.56) | 7,934 (11.51) | 5,063 (8.11) | 3,090 (5.88) |
| Hispanic | 14,593 (17.43) | 8,350 (12.11) | 7,508 (12.03) | 4,803 (9.14) |
| Asian or Pacific Islander | 825 (0.99) | 961 (1.39) | 1,056 (1.69) | 1,731 (3.29) |
| Native American | 974 (1.16) | 404 (0.59) | 244 (0.39) | 116 (0.22) |
| Other | 2,813 (3.36) | 2,315 (3.36) | 2,153 (3.45) | 1,986 (3.78) |
| Insurance Status, n (%) | ||||
| Medicare | 8,422 (10.06)‡ | 6,475 (9.39) | 5,339 (8.55) | 3,809 (7.25) |
| Medicaid | 15,710 (18.77) | 8,975 (13.02) | 6,245 (10.01) | 3,521 (6.70) |
| Private Insurance | 28,398 (33.92) | 30,740 (44.59) | 32,403 (51.92) | 33,847 (64.39) |
| Self-Pay | 18,727 (22.37) | 12,782 (18.54) | 9,572 (15.34) | 5,418 (10.31) |
| No Charge | 2,162 (2.58) | 1,217 (1.77) | 936 (1.50) | 404 (0.77) |
| Other | 10,295 (12.30) | 8,743 (12.68) | 7,918 (12.69) | 5,563 (10.58) |
p<0.05
p<0.01
p<0.001
Table 2 outlines injury characteristics for patients meeting inclusion criteria, including unadjusted inpatient mortality rates. Mean ISS was the same for all quartiles, with the exception of Q4, which had a slightly lower ISS (Q1, Q2, Q3 mean ISS=13.8, interquartile range=9–17; Q4 mean ISS=13.6, interquartile range=9–16). Patients in poorer quartiles had an increasing number of comorbidities as measured by the CCI; however, in all quartiles, more than half of patients had a CCI of 0. Penetrating injury was significantly increased in the lowest wealth quartile (16.8%) compared to higher wealth quartiles (Q2=10%; Q3=7.6%; Q4= 5.1%). A further stratification into the two groups of years showed consistency among all quartiles in the number of patients admitted to the hospital for traumatic injuries that warranted an inpatient stay for all years. Crude mortality rates were significantly higher for the lower wealth quartiles (Q1=4.19%; Q2=3.73%; Q3=3.73%; Q4=3.15%).
Table 2.
Patient Injury Characteristics Stratified by SES Quartile
| Median Household Income Quartile | ||||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Type of Injury, n (%) | ||||
| Blunt | 69,691 (83.25)‡ | 62,044 (90.01) | 57,653 (92.37) | 49,887 (94.91) |
| Penetrating | 14,023 (16.75) | 6,888 (9.99) | 4,760 (7.63) | 2,675 (5.09) |
| Year of Admission, n (%) | ||||
| 2003 | 10,248 (12.24)‡ | 9,172 (13.31) | 8,975 (14.38) | 6,808 (12.95) |
| 2004 | 12,885 (15.39) | 10,014 (14.53) | 7,991 (12.80) | 7,472 (14.22) |
| 2005 | 10,117 (12.09) | 8,274 (12.00) | 8,178 (13.10) | 6,933 (13.19) |
| 2006 | 11,869 (14.18) | 9,281 (13.46) | 8,746 (14.01) | 7,382 (14.04) |
| 2007 | 12,585 (15.03) | 8,911 (12.93) | 8,031 (12.87) | 7,301 (13.89) |
| 2008 | 13,164 (15.72) | 11,625 (16.86) | 9,732 (15.59) | 7,751 (14.75) |
| 2009 | 12,846 (15.35) | 11,655 (16.91) | 10,760 (17.24) | 8,915 (16.96) |
| Mortality, n (%) | 3,510 (4.19)† | 2,571 (3.73) | 2,287 (3.66) | 1,657 (3.15) |
| Mean ISS, (interquartile range) | 13.8 (9–17)‡ | 13.8 (9–17) | 13.8 (9–17) | 13.6 (9–16) |
| Charlson Comorbidity Index (CCI), n (%) | ||||
| 0 | 65,295 (78.0)‡ | 53,669 (77.86) | 49,142 (78.74) | 41,666 (79.27) |
| 1 | 11,721 (14.0) | 9,767 (14.17) | 8,693 (13.93) | 7,051 (13.41) |
| 2 | 3,662 (4.38) | 3,085 (4.46) | 2,543 (4.07) | 2,133 (4.06) |
| 3–15 | 3,036 (3.63) | 2,411 (3.50) | 2,035 (3.26) | 1,712 (3.26) |
ISS=Injury Severity Score
p<0.05
p<0.01
p<0.001
Multivariate regression analyses, adjusting for the covariates discussed above, showed that patients in Q1, Q2, and Q3 had an increased odds of adjusted inpatient mortality, compared with the wealthiest Q4, the reference group (Figure 1). Over the seven-year study period, patients in Q1, the poorest quartile, had 13% increased odds of mortality (95% confidence interval [CI], 1.06–1.20). Patients in Q2 had 9% increased odds of mortality (95% CI, 1.02–1.17). Patients in Q3 showed similarly increased odds of mortality (11%; 95% CI, 1.04–1.19).
Figure 1.
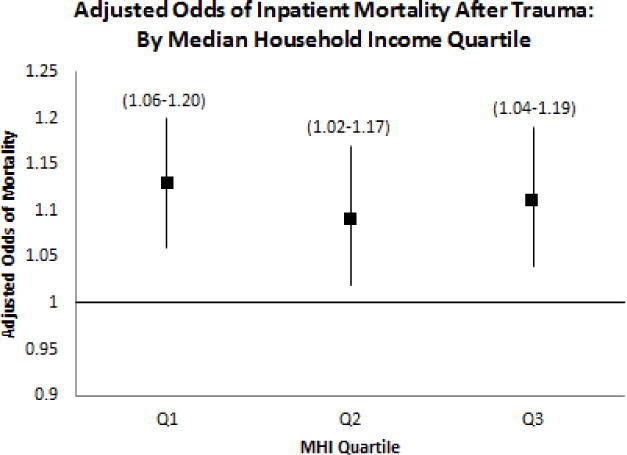
Adjusted odds of inpatient mortality following traumatic injury in adults aged 18–65 with ISS≥9. The reference group is median household income [MHI) quartile 4 [Q4), the wealthiest quartile [75–100%; $67,000+), indicated by the horizontal line at y=l. There are increased odds of mortality for MHI Ql (0–25% quartile; $1–40,999), MHI Q2 (25–50% quartile; $41,000–50,999), and MHI Q3 (50–75% quartile; $51,000–00,999). Vertical bars and values in brackets indicate 95% confidence intervals.
An analysis of the two groups of years (2003–2006 and 2007–2009), adjusting for the same covariates, showed a significant improvement in mortality odds for Q2 over time. The odds of death for Q2 compared with Q4 decreased from 1.15 (95% CI 1.13–1.16) in 2003–2006 to 1.03 (95% CI, 1.01–1.05) in 2007–2009 (Figure 2). The same significant decrease in mortality odds over time was observed for Q3 as well, with these patients showing a 14% increased odds of mortality in the 2003–2006 group (95% CI, 1.13–1.15) and a 8% increased odds of mortality in the 2007–2009 group (95% CI, 1.06–1.09) when compared with Q4. Q1 showed no difference in mortality odds between the two periods of time, with a 13% increased odds of mortality in the 2003–2006 group (95% CI, 1.11–1.15) and a 14% increased odds of mortality in the 2007–2009 group (95% CI, 1.09–1.18).
Figure 2.
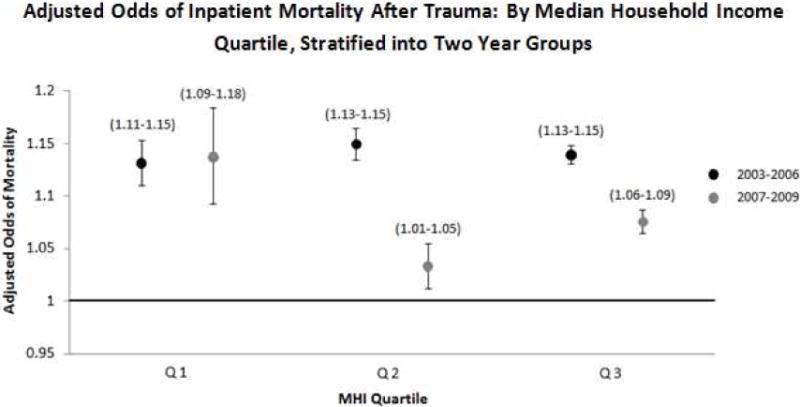
Adjusted odds of inpatient mortality following traumatic injury in adults aged 18–65 with ISS≥9= stratified into two year groups. The reference group is median household income (MHI) quartile 4 (Q4), the wealthiest quartile. MHI Q2 and Q3 show decreased odds of mortality in the 2007–2009 group compared to their respective 2003–2006 group odds of mortality values. MHI Q1 shows no difference in the increased odds of mortality between the groups. Vertical bars and values in brackets indicate 95% confidence intervals.
We further completed a sensitivity analysis to ensure that the observed increased odds of mortality for poorer quartiles were not driven by penetrating trauma injuries, focusing on blunt trauma only. We found that the relationship was still preserved, with individuals in the poorer quartiles Q1, Q2, and Q3 experiencing significantly increased odds of mortality as compared to Q4, the wealthiest quartile (Table 3). An analysis of SES and LOS showed a statistically significant difference in LOS for Q1 (3.63 hours increase) as compared to Q4, however, this difference is not clinically significant. There were no significant differences in LOS for Q2 and Q3 as compared to Q4 (Table 4).
Table 3.
Odds of inpatient mortality for Q1, Q2, and Q3 compared to the wealthiest quartile, Q4, for patients experiencing blunt trauma injuries.
| Median Household Income Quartile | |||
|---|---|---|---|
| Odds of Inpatient Mortality | Q1 | Q2 | Q3 |
| Odds Ratio | 1.08 | 1.09 | 1.11 |
| 95% Confidence Interval | 1.01–1.16 | 1.01–1.17 | 1.03–1.19 |
Table 4.
Difference of increased Length of Stay for Q1, Q2, and Q3 compared to the wealthiest quartile, Q4.
| Median Household Income Quartile | |||
|---|---|---|---|
| Difference of Increased Length of Stay | Q1 | Q2 | Q3 |
| Length of Stay (hour) | 3.63 | 0.68 | 1.58 |
| 95% Confidence Interval | 0.77–6.50 | −2.20–3.57 | −1.52–4.50 |
Discussion
This study of adult trauma patients in the HCUP NIS database from 2003–2009 used median household income by zip code to determine the relationship between SES and inpatient mortality. Patients in the poorer quartiles of median household income experienced higher risk-adjusted mortality after traumatic injury than their equivalently injured, wealthier counterparts.
The disparities identified in this paper are consistent with previous studies that have linked low SES to higher disease prevalence and mortality. Prior studies that identified insurance status, race and trauma center status as predictors of mortality following trauma were limited by their inability to adjust for direct measures of SES, as well as comorbidities. The present study utilizes median household income as a more direct measure of SES, as well as the Charlson Comorbidity Index to adjust for comorbidities. To the best of our knowledge, this is the first study of its kind in the United States to examine the relationship between SES and inpatient mortality after trauma, using MHI and adjusting for important confounders of inpatient mortality such as co-morbid conditions, which are thought to be a fundamental cause of disparities.5
There are several hypotheses for the observed disparity in inpatient mortality following trauma that warrant a discussion. It is possible that individuals living in poorer localities tend to obtain treatment at hospitals with known patterns of worse clinical and functional outcomes. It has been previously demonstrated that hospitals with a larger minority trauma patient population have higher mortality rates, with these mortality rates being even greater for uninsured patient populations.16 Other studies have found that low-performing hospitals tend to serve a greater proportion of minority, uninsured, and low-income patients.17,18 The observed outcomes in our study may thus be partly due to the fact that the populations residing in socioeconomically disadvantaged zip codes are more likely to be minorities and less insured, as our exploratory data analysis of the demographics shows. These patients are thus at increased risk of higher mortality rates as a function of the hospitals at which they are treated. Further studies aimed at determining the type of hospitals where patients of varying SES seek care and the track record of those hospitals should be completed. Future studies should also aim to analyze whether differences exist in hospital characteristics, such as teaching status, location, bed size, and ownership, between patients of varying SES status. If hospital characteristics are found to impact inpatient mortality following traumatic injury, health policy efforts aimed at improving those hospitals may be an important intervention to reduce health disparities.
Healthcare provider heuristics may also play a role in the observed inequities in survival. Heuristics refers to using an experience-based approach to problem solving and is often employed in times when exhaustive research would unreasonable. One such example of a situation would be a physician’s treatment of a patient. While healthcare providers aim to provide equal care to all patients, heuristics are often inevitable, particularly in acute care settings. Physicians are taught early in their careers the importance of efficient patient care and that time is of the essence, particularly in emergency and acute care settings. Providers in acute care settings are thus tasked with making quick decisions and often rely on previous patient experience to assist them in these decisions. Previously held stereotypes of various patient groups, including socioeconomic groups, may influence a provider’s ability to provide equal treatment to all patients. It is important to highlight that the use of heuristics in medicine is likely not intentional or even conscious, but rather the result of time restrictions that lead to their use in order to treat patients quickly and efficiently.
Unconscious or implicit biases held by health care providers may further contribute to mortality disparities; however the data on this subject is conflicting. An individual’s personal beliefs about various patient groups shape the heuristics that he or she applies to patient care, and these beliefs may be difficult to change.19,20 Moreover, individuals are often unaware of their stereotypes, including when and how they implement them when performing tasks, such as providing care. While Green et al. found that physicians with increased unconscious bias were less likely to treat Black patients with thrombolytics,21 on the other hand, a recent study of implicit race and social class bias and vignette-based clinical decision-making among medical students failed to show an association.22 If future studies do suggest that provider biases make a difference, then efforts to reduce disparities should include acknowledging and correcting these biases. There may be ways that providers can become aware of their own biases and how it affects their provision of care to patients.23 Provider education can be instrumental in bringing biases to the forefront and helping to ensure that equal care is provided to all patients.
Yet another potential mechanism for disparities is suggested by Downing et al. who reports that uninsured patients may receive delayed care, due to physicians’ desires to spare patients unnecessary healthcare expenses.2 This altruistic act may cause more harm than benefit, particularly if patients have serious injuries, as the patients with our study with Injury Severity Scores of 9 or higher most likely did. It is thus possible that uninsured patients, the greatest proportion of whom reside in socioeconomically disadvantaged neighborhoods, are delayed in seeking and receiving care for their traumatic injuries, which may contribute to the observed disparity in mortality.
It is important to note that the wealth quartile groups may have been fundamentally different in terms of baseline health status, although our analyses were adjusted for comorbidities. We also adjusted for race, sex, age, insurance status, injury severity, and type of injury, so it is unlikely that the mortality disparity demonstrated here is solely due to these factors. That being said, a limitation of this study is that within the HCUP NIS database, MHI is given a quartile rank by zip code. It is often the case that within a zip code, household incomes are variable. By making the generalization that all residents within a particular zip code fall under one MHI quartile, some specificity is lost and there is the possibility of aggregation bias. However, the use of MHI quartiles as a direct measure of SES has become a standard and valid method in other studies evaluating the impact of SES on prevalence of and mortality from a variety of diseases.24,25 Another limitation of our study is the inability to determine the proximity to a level one trauma center based on zip codes, given the lack of uniformity in zip code geography. Patients’ proximities to level one trauma centers would influence how quickly they receive care and may impact mortality. A final limitation is the inability to analyze differences in readmissions and number of operations among the different quartiles, due to the lack of information in the database and the bundling of procedures in the database, respectively. Overall, these findings suggest that among patients residing in socioeconomically disadvantaged zip codes, there may be mechanisms aside from race, insurance status, injury severity, comorbidities, and type of injury contributing to the disparity in survival after trauma. It is clear that socioeconomic status is an important contributor to disparities in mortality rates among adult trauma patients. The reasons for this observed disparity are most likely complex and nuanced. The hospitals where care is received, the heuristics and biases employed by physicians in treating patients, and the general health status of patients in lower income neighborhoods are all factors that may influence the mortality disparities identified. Health policy and education efforts to minimize healthcare disparities in trauma should address SES as an independent predictor of patient outcomes, taking into account the various potential contributing factors related to SES. Only by developing a more comprehensive understanding of the underlying causes, informed by the knowledge that socioeconomic status is a clear predictor of outcomes, will we will be able to design and implement more effective interventions to mitigate trauma mortality disparities.
Acknowledgments
The authors would like to thank Dr. Eric Bass for his support throughout the study and his assistance in preparing a presentation on the study results.
Financial support for this work was provided by: National Institutes of Health/NIGMS K23GM093112-01 and American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care (Dr. Haider).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rockett IR, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. American journal of public health. 2012 Nov;102(11):e84–92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Downing SR, Oyetunji TA, Greene WR, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? The Journal of trauma. 2011 Jan;70(1):130–134. doi: 10.1097/TA.0b013e3182032b34. discussion 134–135. [DOI] [PubMed] [Google Scholar]
- 3.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008 Oct;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 4.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. American journal of surgery. 2010 Apr;199(4):554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Haider AWP, Bentley J, Monn M, Rehman K, Zarzaur B, et al. Disparities in trauma care and outcomes in the united states: A systematic review and meta-analysis. J Trauma Acute Care Surg. 2012 doi: 10.1097/TA.0b013e31828c331d. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health. No easy solution. JAMA : the journal of the American Medical Association. 1993 Jun 23–30;269(24):3140–3145. [PubMed] [Google Scholar]
- 7.Syme SL, Berkman LF. Social class, susceptibility and sickness. American journal of epidemiology. 1976 Jul;104(1):1–8. doi: 10.1093/oxfordjournals.aje.a112268. [DOI] [PubMed] [Google Scholar]
- 8.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. American journal of public health. 1992 Jun;82(6):816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraus JF, Borhani NO, Franti CE. Socioeconomic status, ethnicity, and risk of coronary heart disease. American journal of epidemiology. 1980 Apr;111(4):407–414. doi: 10.1093/oxfordjournals.aje.a112915. [DOI] [PubMed] [Google Scholar]
- 10.Berg JW, Ross R, Latourette HB. Economic status and survival of cancer patients. Cancer. 1977 Feb;39(2):467–477. doi: 10.1002/1097-0142(197702)39:2<467::aid-cncr2820390215>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 11.Patno ME. Mortality and economic level in an urban area. Public health reports. 1960 Sep;75:841–851. [PMC free article] [PubMed] [Google Scholar]
- 12.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. American journal of public health. 2000 Jan;90(1):70–77. doi: 10.2105/ajph.90.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burrows S, Auger N, Gamache P, Hamel D. Individual and area socioeconomic inequalities in cause-specific unintentional injury mortality: 11-year follow-up study of 2.7 million Canadians. Accident; analysis and prevention. 2012 Mar;45:99–106. doi: 10.1016/j.aap.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Overview of the Nationwide Inpatient Sample (NIS) 2003–2009 http://www.hcupus.ahrq.gov/nisoverview.jsp.
- 15.Stagg V. CHARLSON Stata module to calculate Charlson index of comorbidity. 2012 2006 http://ideas.repec.org/c/boc/bocode/s456719.html.
- 16.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012 Jan;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspectives in biology and medicine. 2005 Winter;48(1 Suppl):S42–53. [PubMed] [Google Scholar]
- 18.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Archives of internal medicine. 2007 Jun 25;167(12):1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- 19.Gorini A, Pravettoni G. An overview on cognitive aspects implicated in medical decisions. European journal of internal medicine. 2011 Dec;22(6):547–553. doi: 10.1016/j.ejim.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Warner JL, Najarian RM, Tierney LM., Jr Perspective: Uses and misuses of thresholds in diagnostic decision making. Academic medicine : journal of the Association of American Medical Colleges. 2010 Mar;85(3):556–563. doi: 10.1097/ACM.0b013e3181ccd59b. [DOI] [PubMed] [Google Scholar]
- 21.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of general internal medicine. 2007 Sep;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA : the journal of the American Medical Association. 2011 Sep 7;306(9):942–951. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marewski JN, Gigerenzer G. Heuristic decision making in medicine. Dialogues in clinical neuroscience. 2012;14(1):77–89. doi: 10.31887/DCNS.2012.14.1/jmarewski. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rangel EL, Burd RS, Falcone RA., Jr Socioeconomic disparities in infant mortality after nonaccidental trauma: a multicenter study. The Journal of trauma. 2010 Jul;69(1):20–25. doi: 10.1097/TA.0b013e3181bbd7c3. [DOI] [PubMed] [Google Scholar]
- 25.Arthur M, Hedges JR, Newgard CD, Diggs BS, Mullins RJ. Racial disparities in mortality among adults hospitalized after injury. Medical care. 2008 Feb;46(2):192–199. doi: 10.1097/MLR.0b013e31815b9d8e. [DOI] [PubMed] [Google Scholar]


