Abstract
Background
Insurance-related outcomes disparities are well-known, but associations between distinct insurance types and trauma outcomes remain unclear. Prior studies have generally merged various insurance types into broad groups. The purpose of this study is to determine the association of specific insurance types with mortality after blunt injury.
Materials and Methods
Cases of blunt injury among adults aged 18-64 years with an Injury Severity Score (ISS)>9 were identified using the 2007-2009 National Trauma Data Bank. Crude mortality was calculated for ten insurance types. Multivariable logistic regression was employed to determine difference in odds of death between insurance types, controlling for ISS, Glasgow Coma Scale motor, mechanism of injury, sex, race and hypotension. Clustering was used to account for possible inter-facility variations.
Results
312,312 cases met inclusion criteria. Crude mortality ranged from 3.2-6.0% by insurance type. Private Insurance, Blue Cross Blue Shield, Workers Compensation, and Medicaid yielded the lowest relative odds of death, while Not Billed and Self Pay yielded the highest. Compared to Private Insurance, odds of death were higher for No Fault (OR 1.25, p=0.022), Not Billed (OR 1.77, p<0.001), and Self Pay (OR 1.78, p<0.001). Odds of death were higher for Medicare (OR 1.52, p<0.001) and Other Government (OR 1.35, p=0.049), while odds of death were lower for Medicaid (OR 0.89, p=0.015).
Conclusions
Significant differences in mortality after blunt injury were seen between insurance types, even among those commonly grouped in other studies. Policymakers may use this information to implement programs to monitor and reduce insurance-related disparities.
Keywords: Insurance type, Blunt injury, Disparities, Outcomes
INTRODUCTION
Injuries are the leading cause of death for Americans aged 1-44 years1 and the greatest source of years of potential life lost in those younger than 65.2 More than 406 billion dollars are spent annually in the United States on medical costs and lost productivity related to injuries.3 Despite the emergent nature of trauma, the burden of injuries and related mortality is unevenly distributed in the United States. Trauma disproportionately strikes racial and ethnic minorities and those of lower socioeconomic status, with myriad potential factors contributing to these inequities.4,5
Following the passage of the Emergency Medical Treatment and Active Labor Act (EMTALA) in 1986, which required hospitals to provide emergency care regardless of ability to pay,6 it was hoped that insurance-related outcomes disparities would be reduced. In theory, trauma, with its emergent nature and universal access to treatment, should be the great equalizer of outcomes. Yet studies have shown that uninsured patients are still more likely to die after trauma.7-10 Disparities in outcomes based on insurance status have been seen in patients sustaining traumatic brain injury (TBI),6,11 non-neurologic traumatic injury,12 injuries from motor vehicle crashes,13 injuries as a result of being struck by a motor vehicle as a pedestrian,14 burn injuries,15 and pediatric trauma injuries.16
Some studies have looked beyond the simple presence of health insurance as an outcomes predictor to the relationship between mortality and different types of insurance. These studies found that mortality rates were generally lower among privately insured patients, or there was no significant difference between groups.8,10-12,14,17 Analyses of the relationships between more specific types of insurance and trauma outcomes have been obscured by the merging of multiple insurance types into broad categories, such as Medicaid and Medicare into “public insurance” and all other types of insurance as “commercial” or “private” insurance.
A more nuanced understanding of the role of specific insurance types is particularly important given the recent passage of the Patient Protection and Affordable Care Act (PPACA) of 2010. PPACA aims to expand insurance coverage to approximately 32 of the currently 50 million uninsured Americans, however the exact type of coverage patients may receive is yet to be determined and there is a potential for variations in services and plans.18,19 With this anticipated expansion in healthcare coverage options it is imperative that we determine if specific insurance types are associated with improved or worse outcomes so that patients can be provided with efficacious choices for coverage. While cross-sectional studies such as this are limited in their ability to provide causal inference, they do shed light on key associations that should be further investigated in order to inform policy. It will be critical to track changes in outcomes for previously uninsured patients in order to determine the impact of this new healthcare legislation. The objective of this study is to determine whether there is an association between specific payer types and trauma mortality.
MATERIALS AND METHODS
This study is a retrospective, cross-sectional analysis of patients included in the National Trauma Databank (NTDB) from 2007-2009. The NTDB is maintained by the American College of Surgeons-Committee on Trauma and is the largest repository of trauma registry data in the United States. From 2007 through 2009, the database received reports from approximately 683 healthcare facilities for a total of 1,061,141 cases. Cases were defined as patients aged 18-64 suffering moderate to severe injury, defined by an Injury Severity Score (ISS) of 9 or greater, as the result of blunt trauma. Data were de-identified and each case was defined by a unique code. Cases were recorded as unique events that were not tied to patient identifiers; therefore, trauma recidivism could not be assessed.
Adults in the specified age range were selected to focus on the population with the highest burden of injury and avoid confounding factors that might occur at the extremes of age. Patients with burn injuries, penetrating injuries, or other non-blunt force traumatic injury were excluded from the analysis due to known differences in mortality between these populations. Cases with missing data on mortality, insurance, or any of the covariates (age, ISS, Glasgow Coma Scale motor, mechanism of injury, sex, race and hypotension) were excluded from both crude and multivariable analysis. Patients who were dead on arrival were also excluded from the analysis.
We assessed demographic data regarding patient age, sex, and race. Patients of races other than Black, White, and Hispanic were excluded due to limited numbers. Insurance types were defined as Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), and Self-pay (SLFP). These insurance types provided the finest resolution available in the NTDB for the included study years. While the NTDB does not provide specific instructions for coding groups such as Other Government, this category should contain such coverage as Tricare, SSI Benefits, and the Federal Employees Health Benefits Program. Also, specific instructions for coding Not Billed and Self Pay are not supplied, but both categories might be assumed to include uninsured patients. Crude proportions were calculated for demographic factors and for covariates of interest (ISS, GCS-M, hypotension, and mechanism of injury) by insurance type. The primary outcome measure for this study was inpatient mortality during the admission associated with the traumatic event.
Statistical Analysis
Statistical significance was set at p=0.05. Crude mortality rates were calculated by insurance type. Bivariate analyses were used to assess differences between crude mortality rates associated with each insurance type. Multivariable logistic regression was used to compare adjusted odds of death among members of nine different insurance type categories against the reference group of privately insured patients. Private insurance was chosen as the reference group to allow clear comparisons with other studies in the field that have used private insurance as the reference group.
Multivariable logistic regression models controlled for factors known to affect trauma outcomes, including: age,20 ISS,20 GCS-M,21 mechanism of injury22, sex23, race7 and hypotension on presentation.24 In all logistic regression models, clustering was used to account for possible inter-facility variations. Interaction terms were used to assess effect modification and were included in the analysis if they were found to be significant and to qualitatively alter the results. Finally, linear combinations of estimators were used to compare groups that were not directly compared in the primary regression model.
To assess confounding by mechanism of injury, a sub-group analysis of only MVC-related trauma was performed using a similar regression model. Another sub-group analysis of patients with the worst injuries (ISS≥25) was also performed to assess the confounding effects of injury severity, in addition to a sub-group analysis of patients with a GCS-M of one. All statistical analyses were performed using STATA MP version 11, StataCorp, College Station, TX, 2009.
RESULTS
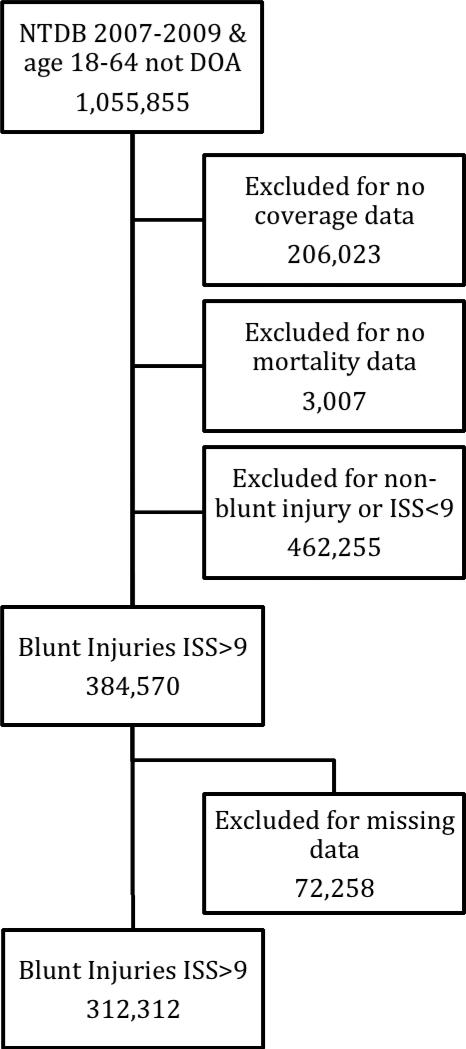
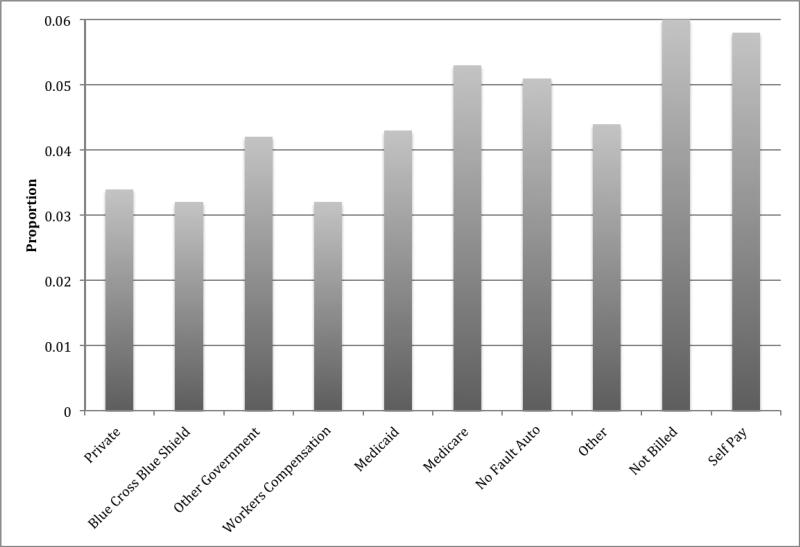
Of the 1,061,141 patients included in the National Trauma Data Bank from 2007-2009, a total of 312,312 cases met inclusion criteria (Figure 1). Crude mortality rates by insurance type ranged from 3.17% to 6.00% (Figure 2). The median age for the study population was 41 years, and the majority of patients (72%) were male (Table 1). Black and Hispanic patients comprised 12% and 13%, respectively, of the sample. The median ISS was 14, mean GCS-M was 5.39, and 3.91% of the population was hypotensive on presentation.
Figure 1.
Inclusion Criteria
Figure 2.
Crude Mortality by Insurance Type
Table 1.
Demographics and Baseline Characteristics (n=312,312)
| COVERAGE TYPE | PRIV | BCBS | OTHG | WCMP | MCAD | MCAR | NFLT | OTHE | NOBI | SLFP | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N= | 92482 | 22601 | 10536 | 14907 | 30941 | 16574 | 28588 | 23211 | 3919 | 68553 | 312312 |
| Age | Median (IQR) | 43 (26) | 44 (25) | 37 (26) | 42 (21) | 38 (24) | 54 (14) | 36 (25) | 38 (25) | 35 (22) | 35 (22) | 41 (25) |
| Sex | % Men | 69 | 69 | 79 | 89 | 66 | 65 | 66 | 71 | 79 | 79 | 72 |
| Race | % White | 85 | 86 | 56 | 73 | 64 | 79 | 80 | 71 | 58 | 63 | 75 |
| % Black | 8 | 7 | 13 | 7 | 20 | 14 | 11 | 13 | 16 | 17 | 12 | |
| % Hispanic | 7 | 6 | 31 | 20 | 15 | 6 | 9 | 16 | 25 | 20 | 13 | |
| ISS | Median | 14 | 14 | 14 | 13 | 14 | 13 | 14 | 14 | 14 | 14 | 14 |
| % with ISS≥25 | 16 | 16 | 18 | 15 | 21 | 15 | 20 | 19 | 17 | 17 | 18 | |
| GCS-M | % with score of 1 | 9 | 8 | 8 | 7 | 13 | 8 | 13 | 11 | 12 | 11 | 10 |
Interquartile Range (IQR). Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP).
Adjusted multivariable linear regression demonstrated significant differences in odds ratios by insurance type (Table 2). Compared to the reference group of Privately Insured patients, those with Medicaid had a significantly reduced odds of death [OR 0.89, 95% CI (0.81, 0.98)], whereas the adjusted odds of death were increased among patients categorized as Other Government [OR 1.35, 95% CI (1.00, 1.82)]; Medicare [OR 1.52, 95% CI (1.35, 1.70)]; No Fault Auto [OR 1.25, 95% CI (1.03, 1.52)], Not billed [OR 1.77, 95% CI (1.47, 2.14)] or Self-pay patients [OR 1.77, 95% CI (1.58, 1.98).
Table 2.
Adjusted Odds of Death by Insurance Type
| COVERAGE TYPE | PRIV | BCBS | OTHG | WCMP | MCAD | MCAR | NFLT | OTHE | NOBI | SLFP |
|---|---|---|---|---|---|---|---|---|---|---|
| n= 312312 | 92482 | 22601 | 10536 | 14907 | 30941 | 16574 | 28588 | 23211 | 3919 | 68553 |
| OR (95% CI) | -- | 0.95 (0.82, 1.10) | 1.35* (1.00, 1.82) | 1.00 (0.85, 1.19) | 0.89* (0.81, 0.98) | 1.52* (1.35, 1.70) | 1.25* (1.03, 1.52) | 1.18 (0.99, 1.41) | 1.77* (1.47, 2.14) | 1.77* (1.58, 1.98) |
Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP)
Reference group = Private Insurance
Adjusted for age, sex, race, ISS, MOI, GCS-M, and presence of hypotension
Statistically significant at p<0.05
Linear combinations of estimators were used to determine odds ratios and 95% confidence intervals for mortality between insurance types not formally compared by the logistic regression model (Table 3). Odds of death were significantly lower in the Blue Cross Blue Shield group and the Medicaid group when compared to the Other Government, Medicare, No Fault Auto, Other, Not billed and Self-pay patients. Patients with Workers Compensation also had significantly lower odds of death than patients in the Medicare, No Fault Auto, Not billed and Self-pay groups. Compared to the Not billed and Self-pay patients, patients with No Fault Auto insurance and patients with “Other” insurance had significantly reduced odds of death. Medicare patients also had significantly lower odds of death than Self-pay patients; however, there were no differences detected between Medicare patients and Not billed patients. No significant differences in odds of death were detected between the Not billed and Self-pay patients.
Table 3.
Adjusted odds ratios from linear combinations of estimators**
| BCBS | OGOV | WORKC | MCAD | MCAR | NFLT | OTHE | NOBI | |
|---|---|---|---|---|---|---|---|---|
| OGOV | 0.70* (0.51, 0.96) | |||||||
| WORKC | 0.95 (0.81, 1.11) | 1.35 (0.99, 1.83) | ||||||
| MCAD | 1.07 (0.91, 1.24) | 1.52* (1.12, 2.04) | 1.27 (0.94, 1.35) | |||||
| MCAR | 0.63* (0.54, 0.73) | 0.89 (0.66, 1.20) | 0.66* (0.55, 0.78) | 0.59* (0.51, 0.67) | ||||
| NFLT | 0.76* (0.62, 0.93) | 1.08 (0.77, 1.50) | 0.80* (0.66, 0.97) | 0.71* (0.58, 0.87) | 1.21 (0.98, 1.49) | |||
| OTHE | 0.80* (0.67, 0.96) | 1.14 (0.83, 1.57) | 0.84 (0.69, 1.04) | 0.75* (0.63, 0.90) | 1.28* (1.07, 1.54) | 1.07 (0.85, 1.32) | ||
| NOBI | 0.54* (0.41, 0.70) | 0.76 (0.54, 1.08) | 0 57* (0.43, 0.74) | 0.50* (0.41, 0.61) | 0.86 (0.68, 1.09) | 0.71* (0.53, 0.95) | 0.67* (0.51, 0.88) | |
| SLFP | 0.54* (0.48, 0.60) | 0.76 (0.57, 1.03) | 0.57* (0.49, 0.66) | 0.50* (0.44, 0.58) | 0.86* (0.74, 0.98) | 0.71* (0.59, 0.86) | 0.67* (0.57, 0.79) | 1.00 (0.78, 1.29) |
Blue Cross Blue Shield (BCBS), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP)
Adjusted for age, sex, race, ISS, MOI, GCS-M, and presence of hypotension
Statistically significant at p<0.05
Interpretation: Odds ratios represent (odds of mortality | column type)/(odds of mortality | row type). For example in the first cell OR=(Odds of mortality | BCBS)/(Odds of mortality | OGOV)=0.70
In a sub-group analysis of patients injured in motor vehicle collisions (Table 4), patients with Medicaid had lower odds of death than privately insured patients. In contrast, the odds of death were significantly higher among patients with Medicare, No Fault Auto, Not billed, and Self-pay compared to the privately insured. In another sub-group analysis of only severely injured patients (ISS>25), increased odds of death among these patient groups, as well as the Other Government and Other insurance groups, compared to those with private insurance, were found. Medicaid patients experienced lower odds of death in this analysis as well (Table 5). A final sub-group analysis of only those patients with a GCS-M of one showed similar results: a lower adjusted odds of death among Medicaid patients, and a higher adjusted odds of death among No Fault Auto, Other, Not billed and Self-pay patients, compared to those with Private Insurance (Table 6).
Table 4.
Adjusted Odds of Death by Insurance Type Among Patients Injured in MVCs
| COVERAGE TYPE | PRIV | BCBS | OTHG | WCMP | MCAD | MCAR | NFLT | OTHE | NOBI | SLFP |
|---|---|---|---|---|---|---|---|---|---|---|
| n=167,949 | 47142 | 10458 | 6006 | 3584 | 14991 | 5277 | 26440 | 15308 | 2052 | 36691 |
| OR (95% CI) | -- | 0.95 (0.81, 1.12) | 1.39 (0.92, 2.11) | 0.93 (0.71, 1.21) | 0.79* (0.70, 0.89) | 1.27* (1.07, 1.50) | 1.24* (1.03, 1.49) | 1.14 (0.95, 1.37) | 1.95* (1.61, 2.36) | 1.92* (1.71, 2.16) |
Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP)
Reference group = Private Insurance
Adjusted for age, sex, race, ISS, GCS-M, and presence of hypotension
Statistically significant at p<0.05
Table 5.
Adjusted Odds of Death by Insurance Type among Severely Injured Patients (ISS≥25)
| COVERAGE TYPE | PRIV | BCBS | OTHG | WCMP | MCAD | MCAR | NFLT | OTHE | NOBI | SLFP |
|---|---|---|---|---|---|---|---|---|---|---|
| n= 54,636 | 15188 | 3696 | 1874 | 2207 | 6552 | 2458 | 5787 | 4511 | 684 | 11679 |
| OR (95% CI) | -- | 0.99 (0.85, 1.16) | 1.43* (1.10, 1.85) | 1.06 (0.87, 1.28) | 0.84* (0.74, 0.94) | 1.27* (1.10, 1.47) | 1.22* (1.02, 1.46) | 1.23* (1.01, 1.48) | 2.22* (1.73, 2.85) | 1.87* (1.63, 2.15) |
Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP)
Reference group = Private Insurance
Adjusted for age, sex, race, MOI, GCS-M, and presence of hypotension
Statistically significant at p<0.05
Table 6.
Adjusted Odds of Death by Insurance Type among Patients with a GCS-M = 1
| COVERAGE TYPE | PRIV | BCBS | OTHG | WCMP | MCAD | MCAR | NFLT | OTHE | NOBI | SLFP |
|---|---|---|---|---|---|---|---|---|---|---|
| n= 31857 | 8169 | 1895 | 879 | 1058 | 3999 | 1402 | 3691 | 2499 | 471 | 7844 |
| OR (95% CI) | -- | 1.02 (0.87, 1.21) | 1.27 (0.94, 1.73) | 1.06 (0.85, 1.33) | 0.72* (0.63, 0.81) | 1.11 (0.95, 1.31) | 1.26* (1.02, 1.54) | 1.26* (1.02, 1.56) | 1.77* (1.43, 2.20) | 1.93* (1.67, 2.23) |
Blue Cross Blue Shield (BCBS), Private/Commercial (PRIV), Medicaid (MCAD), Medicare (MCAR), Workers Compensation (WCMP), No Fault Auto (NFLT), Other (OTHE), Other Government (OTHG), Not billed (NOBI), Self-pay (SLFP)
Reference group = Private Insurance
Adjusted for age, sex, race, ISS, MOI, and presence of hypotension
Statistically significant at p<0.05
DISCUSSION
This analysis of moderate to severely injured patients suffering blunt trauma demonstrates that the various insurance types included in the NTDB are associated with different mortality outcomes. It also demonstrates that insurance types that have been commonly analyzed together in prior studies have varying associations with mortality and indicates that merging insurance types into larger categories may not be appropriate when studying the association of mortality and healthcare coverage.
While Medicaid has been associated with worse outcomes in patients with lung cancer,25 uterine cancer,26 in patients undergoing cardiac valve operations,27 and even after lower-extremity injuries,28 we found that Medicaid was associated with a relative decrease in odds of death when compared to private insurance coverage. Given the inconsistency of our results with the bulk of the literature, which has shown that private insurance is associated with lower mortality than public insurance, we conducted several sub-group analyses. To address potential confounding by mechanism of injury or uneven distribution of injury severity, we performed sub-group analyses of patients who sustained injury from MVCs and patients who were severely injured (ISS>25), respectively. In both of these analyses the relationship between Medicaid and reduced odds of death was maintained (Table 4, Table 5).
On the other hand, as shown in Table 1, the Medicaid population had a significantly higher proportion of patients with a GCS-M of one. The principal driver of the apparent survival advantage associated with Medicaid may be the disproportionate distribution of low GCS-M scores and the concomitant lower mortality within this group. While determining the cause of the apparent survival advantage in this subgroup is not possible due to the cross-sectional nature of this study, the results suggest that caution should be taken when drawing conclusions based on grouped insurance data.
Additionally it must be noted that multiple studies demonstrate that public insurance is associated with decreased access to care,29 decreased cancer screening services,30 decreased cancer survival,31 and differential discharge to rehabilitation centers for TBI patients when compared with private insurance.32 It is therefore necessary to further prospectively explore the true relationship between public insurance and outcomes among trauma patients in order to avoid the inherent limitations of this analysis and those of other retrospective studies.
These results further suggest that it is important to examine each insurance type individually when discussing both the etiology of mortality differences and potential confounding factors. Not surprisingly, Medicare had the highest mortality of the government insurance types. Medicare patients had the highest median age, and likely more comorbidities. Indeed, to qualify for Medicare in our study age group, patients must suffer from a disabling injury or illness. This group cannot be considered to have similar underlying baseline risk of mortality due to their comorbidities as prior studies have demonstrated that comorbidities are associated with worse outcomes. 20,33 Caution should be taken when combining Medicare with Medicaid or other government insurance types for analysis, as the Medicare group is likely to suffer an increased burden of death and is not directly comparable with the other governmental insurance types. Furthermore, while insurance type appears to be associated with disparate outcomes after blunt injury, other sources of disparities in trauma outcomes, such as provider bias,34 hospital type,35 and comorbid conditions cannot be ignored.
Although the reasons for disparate outcomes by insurance type are not clear, the strong trends demonstrated in this study should be considered as the Patient Protection and Affordable Care Act is implemented. As we move forward in extending coverage to millions of uninsured and underinsured Americans, it is of the utmost importance that we dynamically track outcomes associated with coverage type to determine the effects of increased coverage and its impact on reducing or eliminating health disparities. It has been suggested that health information technology systems mandated by PPACA should be used to collect more meaningful data on race,36 and ethnicity as this will help track the resolution of race and ethnicity based health care disparities. The results of this study suggest that we should extend this further to enhance the type and amount of data collected regarding payer and healthcare coverage so that inequities based on insurance or access can be uncovered and reduced or eliminated.
There are a few important limitations in this study. First, the cross-sectional nature of the study limits the conclusions that can be drawn regarding the etiologies of disparate outcomes. However, these studies are necessary for generating hypotheses and highlighting associations that should be investigated. Further studies could use a prospective design in order to determine causal linkages. Second, while this study goes further than previous studies by breaking insurance type into ten categories, groups within the NTDB such as Privately Insured, Other Government and Other insurance are heterogeneous conglomerations of multiple coverage types. Because no instructions are provided to those who enter these data, there exists the possibility of substantial variation in the coding within these categories. There is no clear delineation made between Not Billed and Self Pay and in our analyses, these groups appeared quite similar. Future work should determine differences between insurance types that are not clearly differentiated in the database. Another limitation is the temporality of documentation of insurance coverage. There is no distinct time frame in which coders determine coverage and therefore reported coverage may vary between institutions. Hence, there exists the possibility of survival bias for those hospitals that report coverage at time of discharge. This would occur if the uninsured patients that were more likely to survive were offered medical assistance, whereas those who were more likely to die remained in the uninsured category. Future studies assess both admission and discharge insurance coverage. Finally, due to a lack of information, this study was not able to adjust for co-morbidities, which are known to influence trauma outcomes.20,33 Indeed, factors such as comorbidities may have stronger relationships with patient outcomes than insurance type and future studies should attempt to shed light on this important confounding variable. Data on comorbidities are available in the NTDB but they are not documented for up to 30% of patients.
Substantial variability in mortality by insurance type was observed in this study. The factors leading to this variability and the relationship between insurance types, mortality, and possible confounders such as comorbid conditions must be explored. Prior studies that have lumped Medicare and Medicaid patients together as having government insurance may have failed to detect important differences in mortality outcomes. Future studies should focus on elucidating the factors that lead to insurance-related disparities with an aim to improve health outcomes for all patients, regardless of their ability to pay.
Acknowledgements
The authors would like to acknowledge Erin Hall for contributions to the statistical analysis and Valerie Scott for comments on the manuscript.
Sources of funding: Financial support for this work was provided by: National Institutes of Health/ NIGMS K23GM093112-01; American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care and Hopkins Center for Health Disparities Solutions (Dr. Haider) and grant number 5TL1RR025007 from the National Center Research Resources to the Johns Hopkins University School of Medicine, which funds the Predoctoral Clinical Research Training Program (P. Weygandt).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: None.
REFERENCES
- 1.National Vital Statistics System, National Center for Health Statistics, CDC. National Vital Statistics System, National Center for Health Statistics, CDC Accessed at http://www.cdc.gov/Injury/wisqars/pdf/10LCD-Age-Grp-US-2008-a.pdf.
- 2.Segui-Gomez M, MacKenzie EJ. Measuring the public health impact of injuries. Epidemiol Rev. 2003;25:3–19. doi: 10.1093/epirev/mxg007. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Corso PS, Miller TR. Incidence and economic burden of injuries in the United States. Oxford University Press; New York, NY: 2006. Associates. [Google Scholar]
- 4.McKenna MT, Michaud CM, Murray CJ, Marks JS. Assessing the burden of disease in the united states using disability-adjusted life years. Am J Prev Med. 2005 Jun;28(5):415–23. doi: 10.1016/j.amepre.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Greene WR, Oyetunji TA, Bowers U, Haider AH, Mellman TA, Cornwell EE, Siram SM, Chang DC. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am. J. Surg. 2010 Apr;199(4):554–557. doi: 10.1016/j.amjsurg.2009.11.005. 2010. [DOI] [PubMed] [Google Scholar]
- 6.Alban RF, Berry C, Ley E, Mirocha J, Margulies DR, Tillou A, et al. Does health care insurance affect outcomes after traumatic brain injury? analysis of the national trauma databank. Am Surg. 2010 Oct;76(10):1108–11. [PubMed] [Google Scholar]
- 7.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008 Oct;143(10):945–9. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 8.Haas JS, Goldman L. Acutely injured patients with trauma in massachusetts: Differences in care and mortality, by insurance status. Am J Public Health. 1994 Oct;84(10):1605–8. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salim A, Ottochian M, DuBose J, Inaba K, Teixeira P, Chan LS, et al. Does insurance status matter at a public, level I trauma center? J Trauma. 2010 Jan;68(1):211–6. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 10.Rosen H, Saleh F, Lipsitz S, Rogers SO, Jr, Gawande AA. Downwardly mobile: The accidental cost of being uninsured. Arch Surg. 2009 Nov;144(11):1006–11. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 11.Heffernan DS, Vera RM, Monaghan SF, Thakkar RK, Kozloff MS, Connolly MD, et al. Impact of socioethnic factors on outcomes following traumatic brain injury. J Trauma. 2011 Mar;70(3):527–34. doi: 10.1097/TA.0b013e31820d0ed7. [DOI] [PubMed] [Google Scholar]
- 12.Zarzaur BL, Stair BR, Magnotti LJ, Croce MA, Fabian TC. Insurance type is a determinant of 2-year mortality after non-neurologic trauma. J Surg Res. 2010 May 15;160(2):196–201. doi: 10.1016/j.jss.2009.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tepas JJ, 3rd, Pracht EE, Orban BL, Flint LM. Insurance status, not race, is a determinant of outcomes from vehicular injury. J Am Coll Surg. 2011 Apr;212(4):722, 7. doi: 10.1016/j.jamcollsurg.2010.12.016. discussion 727-9. [DOI] [PubMed] [Google Scholar]
- 14.Maybury RS, Bolorunduro OB, Villegas C, Haut ER, Stevens K, Cornwell EE, 3rd, et al. Pedestrians struck by motor vehicles further worsen race- and insurance-based disparities in trauma outcomes: The case for inner-city pedestrian injury prevention programs. Surgery. 2010 Aug;148(2):202–8. doi: 10.1016/j.surg.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Farrell RT, Bennett BK, Gamelli RL. An analysis of social support and insurance on discharge disposition and functional outcomes in patients with acute burns. J Burn Care Res. 2010 May-Jun;31(3):385–92. doi: 10.1097/BCR.0b013e3181db516b. [DOI] [PubMed] [Google Scholar]
- 16.Rosen H, Saleh F, Lipsitz SR, Meara JG, Rogers SO., Jr Lack of insurance negatively affects trauma mortality in US children. J Pediatr Surg. 2009 Oct;44(10):1952–7. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 17.Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010 Aug;17(8):809–12. doi: 10.1111/j.1553-2712.2010.00819.x. [DOI] [PubMed] [Google Scholar]
- 18.Williams DR, McClellan MB, Rivlin AM. Beyond the affordable care act: achieving real improvements in americans’ health. Health Affairs. 2010 Aug;29(8):1481–1488. doi: 10.1377/hlthaff.2010.0071. [DOI] [PubMed] [Google Scholar]
- 19.DeNavas-Walt C, Proctor BD, Smith JC, U.S. Census Bureau Income, poverty, and health insurance coverage in the united states 2010. 2011:60–239. [Google Scholar]
- 20.Milzman DP, Boulanger BR, Rodriguez A, Soderstrom CA, Mitchell KA, Magnant CM. Pre-existing disease in trauma patients: a predictor of fate independent of age and injury severity score. J. Trauma. 1992 Feb;32(2):236–43. discussion 243-4. [PubMed] [Google Scholar]
- 21.Healey C, Osler TM, Rogers FB, Healey MA, Glance LG, Kilgo PD, et al. Improving the glasgow coma scale score: Motor score alone is a better predictor. J Trauma. 2003 Apr;54(4):671, 8. doi: 10.1097/01.TA.0000058130.30490.5D. discussion 678-80. [DOI] [PubMed] [Google Scholar]
- 22.Haider AH, Chang DC, Haut ER, Cornwell EE, 3rd, Efron DT. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009 May 1;153(1):138–42. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Haider AH, Crompton JG, Oyetunji T, Stevens KA, Efron DT, Kieninger AN, et al. Females have fewer complications and lower mortality following trauma than similarly injured males: A risk adjusted analysis of adults in the national trauma data bank. Surgery. 2009 Aug;146(2):308–15. doi: 10.1016/j.surg.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Edelman DA, White MT, Tyburski JG, Wilson RF. Post-traumatic hypotension: Should systolic blood pressure of 90-109 mmHg be included? Shock. 2007 Feb;27(2):134–8. doi: 10.1097/01.shk.0000239772.18151.18. [DOI] [PubMed] [Google Scholar]
- 25.Slatore CG, Au DH, Gould MK, American Thoracic Society Disparities in Healthcare Group An official american thoracic society systematic review: Insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med. 2010 Nov 1;182(9):1195–205. doi: 10.1164/rccm.2009-038ST. [DOI] [PubMed] [Google Scholar]
- 26.Fedewa SA, Lerro C, Chase D, Ward EM. Insurance status and racial differences in uterine cancer survival: A study of patients in the national cancer database. Gynecol Oncol. 2011 Jul;122(1):63–8. doi: 10.1016/j.ygyno.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Lapar DJ, Bhamidipati CM, Walters DM, Stukenborg GJ, Lau CL, Kron IL, et al. Primary payer status affects outcomes for cardiac valve operations. J Am Coll Surg. 2011 May;212(5):759–67. doi: 10.1016/j.jamcollsurg.2010.12.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N. Engl. J. Med. 2002 Dec;347(24):1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 29.Hing E, Burt CW. Characteristics of office-based physicians and their medical practices: united states, 2005-2006. Vital Health Stat. 2008 Apr 13;166:1–34. 2008. [PubMed] [Google Scholar]
- 30.Ioannou GN, Chapko MK, Dominitz JA. Predictors of colorectal cancer screening participation in the united states. Am J Gastroenterol. 2003 Sep;98(9):2082–91. doi: 10.1111/j.1572-0241.2003.07574.x. [DOI] [PubMed] [Google Scholar]
- 31.Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008 Jan-Feb;58(1):9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 32.Chan L, Doctor J, Temkin N, MacLehose RF, Esselman P, Bell K, Dikmen S. Discharge disposition from acute care after traumatic brain injury: The effect of insurance type. Arch. Phys. Med. Rehabil. 2001 Sep;82(9):1151–1154. doi: 10.1053/apmr.2001.24892. [DOI] [PubMed] [Google Scholar]
- 33.McGwin G, Jr, MacLennan PA, Fife JB, Davis GG, Rue LW., 3rd Preexisting conditions and mortality in older trauma patients. J Trauma. 2004 Jun;56(6):1291–6. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 36.Haider AH, Pronovost PJ. Health information technology and the collection of race, ethnicity, and language data to reduce disparities in quality of care. Jt Comm J Qual Patient Saf. 2011 Oct;37(10):435–6. doi: 10.1016/s1553-7250(11)37054-7. [DOI] [PubMed] [Google Scholar]
- 34.Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swoboda S, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011 Sep 7;306(9):942–51. doi: 10.1001/jama.2011.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haider AH, Ong'uti S, Efron DT, Oyetunji TA, Crandall ML, Scott VK, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: A nationwide analysis of 434 hospitals. Arch Surg. 2011 Sep 19; doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]