Abstract
Purpose:
Conventional, transurethral resection of bladder tumor (TURBT) involves piecemeal resection of the tumor and has a very high recurrence rate. We evaluated the outcome of en-bloc TURBT (ET) in comparison with conventional TURBT (CT) in non-muscle invasive bladder carcinoma in terms of recurrencew and progression.
Materials and Methods:
From September 2007 to June 2011, in a prospective non-randomized interventional setting, ET was compared with CT in patients with solitary tumor of 2-4 cm size in terms of recurrence and progression. Pedunculated tumors, size >4 cm, tumors with associated hydroureteronephrosis and biopsy specimen with absent detrusor muscles were excluded. Fisher's exact test and survival analyses were used to compare the demography and the outcome.
Results:
A total of 21 patients of ET were compared with 24 patients of CT. Mean tumor size was 2.8 cm in ET and 3.3 cm in CT group. Location of tumor, stage and grade were comparable in both groups. Recurrence rate was 28.6% versus 62.5% (P = 0.03) and progression rate was 19% versus 33.3% (P = 0.32) in ET versus CT group respectively. Recurrence free survival was 45.1 (95% CI: 19.0-38 months) and 28.5 (95% CI: 35.4-54.7 months) in ET and CT group (P = 0.018). Progression free survival in ET and CT was 48.32 (95% CI: 35.5-53.0 months) and 44.26 (95% CI: 39.0-57.5 months), P = 0.46.
Conclusion:
There was a significant reduction in the recurrence rate and time to recurrence with ET. Rate of progression was also relatively less with ET, though not statistically significant.
Keywords: Bladder cancer, detrusor muscles, non-muscle invasive bladder cancer, progression free survival, recurrence free survival
INTRODUCTION
Bladder cancer is the seventh most common malignancy in men and 8th most common malignancy in women.[1] In India, bladder cancer is the fifth most common cancer in men according to Delhi based registry with age adjusted incidence rate of 5.8/100,000 person years.[2] It is predominantly a disease of the male population with male to female ratio of 8.6:1 with the median age at presentation of 60 years (ranges from 18 to 90 years).[3]
For non-muscle invasive bladder carcinoma (NMIBC), transurethral resection of bladder tumor (TURBT) is the cornerstone of treatment. Successful management of these tumors relies on adequate initial resection and accurate histological diagnosis. After TURBT alone, around 50-70% of patients develop recurrence.[4] Reasons for such a high recurrence rate for NMIBC have been cited as incomplete resection in initial TURBT, aggressive tumor biology, implantation of the tumor cells and possibly a field change to start with.
The conventional TURBT (CT) technique involves piecemeal resection of the tumor, which is contrary to the established oncological principles of removing tumor in other parts of the body. Unfortunately, there has never been a certain way to provide a complete resection of the visible tumor in the bladder. Inadequate resection may be responsible for the higher recurrence rate.[4] Similarly, it has been observed in one study that almost 81% of the tumors recurred at the site of previous resection, which indirectly suggests that the technique of resecting tumor is not adequate.[5]
In view of the high rate of recurrence, perhaps TURBT should be modified to provide en-bloc resection of the specimen, based on the established oncological principle of dissecting through normal tissue. Several studies have examined the feasibility of en-bloc TURBT (ET).[6,7,8] These studies on en-bloc tumor removal were attractive in their simplicity, use of existing equipment, clinical safety profile and adequacy of pathology, but they have not commented on the essential outcome, i.e., recurrence and progression rate. This study was aimed at conceptualizing the technique of “sculpting and resecting” in form of ET and comparing its outcomes in terms of recurrence and progression with the conventional technique of incising and scattering.
MATERIALS AND METHODS
After seeking an institutional ethics committee approval, a prospective non-randomized interventional study was conducted between September 2007 to June 2011. End points of the study, i.e., recurrence and progression rates were compared in two groups. ET was carried out by a single surgeon. To minimize the bias toward deliberate attempt by a surgeon who did ET to resect tumor completely, CT was carried out by two different urologists. All three urologists were senior consultants with more than 10 years of experience in endourology. Clinical data on the size (measured by ultrasonography in 37 patients and contrast enhanced computerized tomogram scan on 33 patients) and the location of the tumor were recorded.
Sample size
Two sided Z-test with pooled variance was used to calculate the sample size. With existing recurrence rate of 60% with CT, an estimate of reduction of recurrence rate by 40% gave a sample of 23 patients in each group to achieve 82% power at the significance level of 0.05.
Inclusion criteria
Patients presenting for the first time with single tumor on imaging and the tumor size from 2 to 4 cm were included in the study.
Exclusion criteria
Patients with prior TURBT and recurrences, pedunculated tumors, multiple tumors, biopsy specimen with absent detrusor muscles and those with tumor size of more than 4 cm were excluded. Tumors less than 2 cm were excluded as the technique would not make a real difference in them.
Treatment and follow-up
Patients were followed-up after an initial TURBT with check cystoscopy at 3 months interval for initial 2 years, 6 monthly for next 2 years and then yearly. Progression was defined as any upgradation of stage or grade.
Final analysis
A total of 70 patients were included, 30 had ET and 40 had CT. As patients with stage T2 and those with absence of detrusor muscle on the first TURBT were excluded, for the final analyses there were 21 and 24 patients in ET and CT groups respectively [Graph 1].
Graph 1.
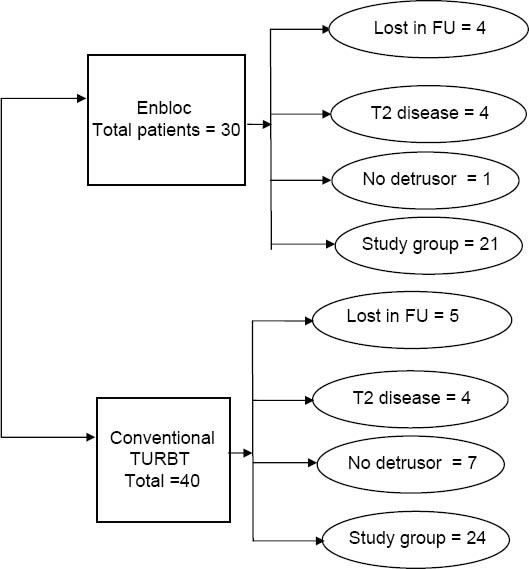
Study population
Technique of ET, “sculpting and resection technique”
The usual Tungsten loop electrode and 26 Fr resectoscope (Storz, Germany) with 30° lens and monopolar cautery was used. The angle of the loop electrode was changed manually from 90° to 45° for ET as published before [Figure 1].[8] Feasibility of en-bloc resection was initially established in tumors of less than 2 cm in six cases before initiating this study.
Figure 1.
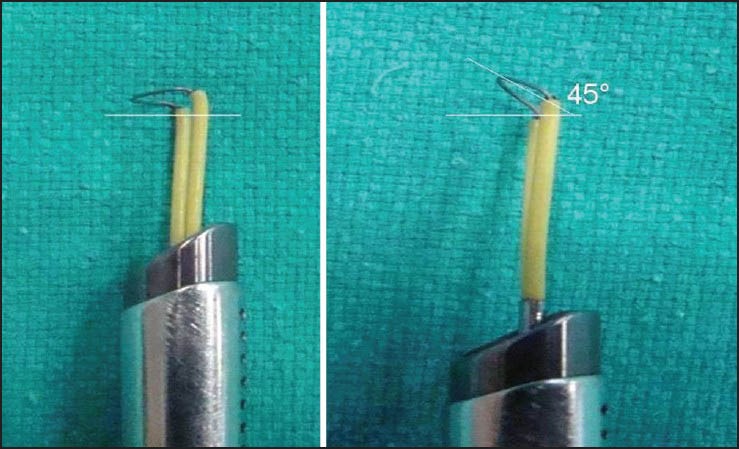
Angle of the loop electrode was changed manually from 90° to 45° for en-bloc transurethral resection of bladder tumor
Normal mucosa around the tumor base was scored by using coagulation current at setting of 60-80 W (Valley Lab, USA). Blood vessels entering the tumor were coagulated first. Retrograde resection was started in the deep layer of detrusor muscle elevating the tumor off the base with the help of angle of the loop and beak of the resectoscope. Free lying tumor which was too large to be taken out through urethra was cut into 2-3 pieces in a way that all the layers are there in the piece of the tumor tissue. In a partially filled bladder with minimal inflow, the tumors were divided using a cutting current with the tumor sited over the trigone for the current to pass. Once the groove was created, the loop was entangled in the groove and tumor was lifted away from the trigone and then cut against the beak of the resectoscope. Use of a nephroscope and grasping forceps was helpful in retrieving the tumor, the largest single piece being a 3 cm tumor in a female.
Six, weekly doses of intravesical Bacillus Calmette-Guerin (BCG) (Oncovac, Danish 1331 strain) was instilled in patients with Ta high grade and T1 disease. The compliance rate for BCG at our center is as high as 85% and was similar in both CT and ET.
Histopathological examination was carried out using the 2004 World Health Organization - International Society of Urological Pathological grading system. Blood loss was calculated in terms of fall in hemoglobin levels measured before and a day after TURBT.
Statistical analysis
Fisher's exact test was applied to compare the recurrence and progression rate. P < 0.05 was considered significant. Recurrences free survival (RFS) and progression-free survival (PFS) were calculated using Kaplan-Meier method and long rank test. All statistical analyses were performed using SPSS 16 Chicago, USA.
RESULTS
There were 40 patients in CT and 30 with ET group. Patients who had detrusor muscle invasion or had no detrusor muscle in the first TURBT were excluded from the analyses. Patients in whom follow-up was not present were also excluded [Graph 1].
At the final analysis 21 patients of ET were compared with 24 patients with CT. The mean age was 52.6 ± 12.2 and 55 ± 13.6 years in ET and CT group. Location of the tumor, stage and grade were comparable in both the groups. Median follow-up period was 40 months and 30 months in ET and CT groups respectively [Tables 1 and 2].
Table 1.
Stage, grade and locations of tumor in two groups on initial TURBT
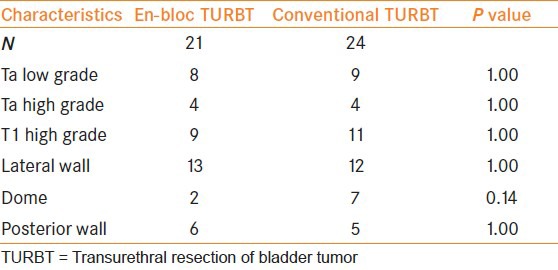
Table 2.
Tumor characteristics and the outcome in two groups of TURBT
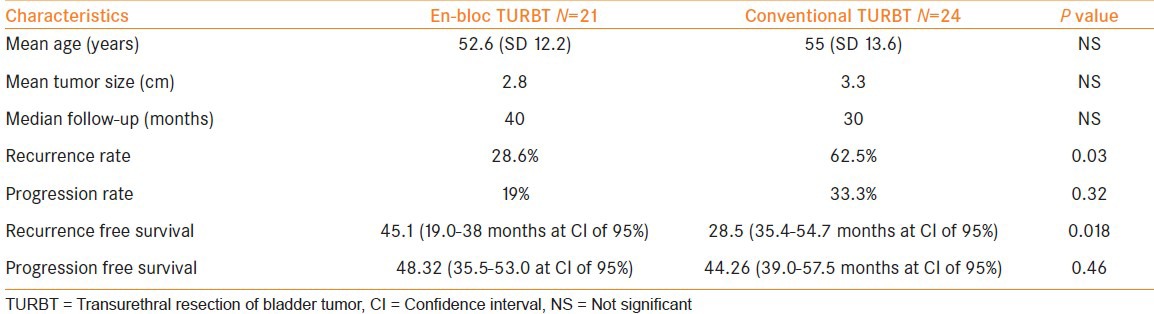
Recurrence rate was 28.6% versus 62.5% (P = 0.03) and progression rate was 19% versus 33.3% (P = 0.32) in ET versus CT group respectively [Table 2]. In the ET group, the recurrence in non-lamina invasive NMIBC tumors was 16%, where as it was 53% in CT. Similarly in lamina invasive tumor, the recurrence rate was 44% and 72% in ET and CT group.
Mean RFS was 45.1 months (95% CI: 19.0-38 months) with ET and 28.5 months (95% CI: 35.4-54.7 months) in CT with P value of 0.018 [Figure 2 and Table 2]. Regarding the site of tumor recurrence, only 1 (16%) patient had recurrence at the same site in ET group while 6 (40%) patients had recurrence at the same site with CT [Table 3].
Figure 2.
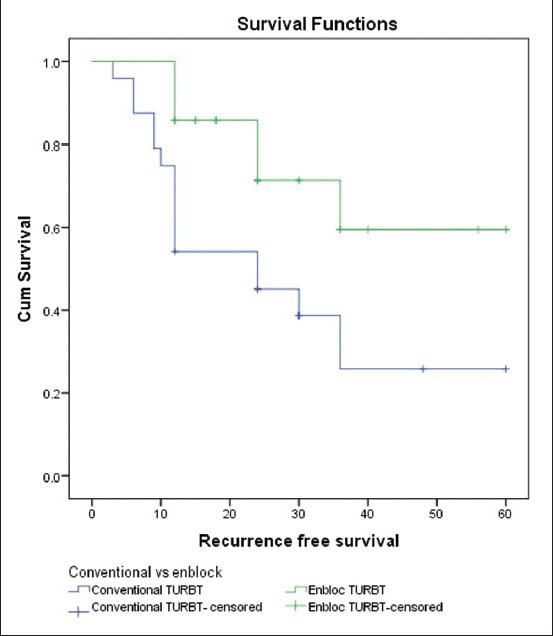
Recurrence free survival
Table 3.
Site of recurrences in two groups
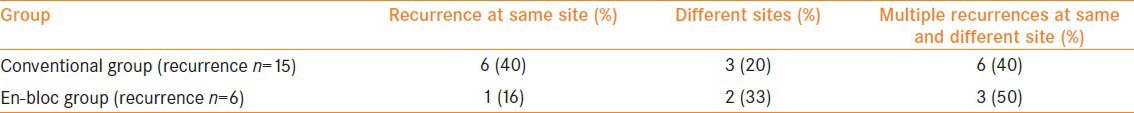
Four patients in en-bloc and eight patients in conventional group had disease progression (19% vs. 33.3%, P = 0.32). Mean PFS in ET and CT group was 48.32 months (95% CI: 35.5-53.0 months) and 44.26 months (95% CI: 39.0-57.5 months) with P value of 0.46 [Figure 3 and Table 2]. In ET group, three patients had progressed without prior recurrence; one had progressed after one recurrence. In CT group, six patients had progressed on first recurrence; one had progressed after one recurrence and one patient had progressed after two recurrences.
Figure 3.
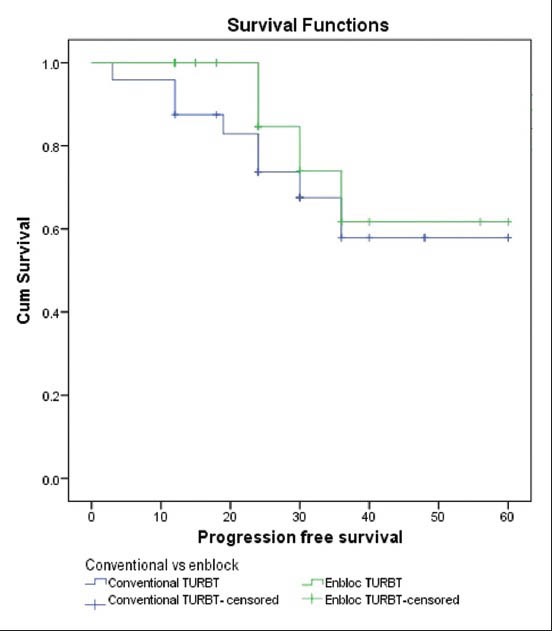
Progression free survival
Discussion
TURBT is a procedure with a varied outcome in terms of adequacy of resection, recurrence and progression. There is no clinical yardstick to judge the completeness of resection. There are a few surrogate markers to assess adequate resection such as presence of detrusor muscle in the specimen and the rate of subsequent recurrence.[5,9,10] Successful management of bladder tumors (particularly non-muscle-invasive tumors), relies on adequate initial resection and accurate histological diagnosis.
An ideal TURBT would mean complete resection of the visible tumor, resection of the surrounding healthy looking mucosa for up to 1 cm and then the removal of detrusor muscle. Herr and Donat described three ways to measure the quality of a good TURBT, i.e., complete resection, presence of deep muscle in the specimen and the rate of recurrence at the site of previous TURBT.[9] They also suggested classifying tumor resection as R0; microscopic negative margin, R1 with microscopic positive margin and R2 that is macroscopic positive margin. This kind of assessment is not practical in CT, but could be possible in en-bloc resection, where we can have a piece of tumor tissue, which has all three layers, i.e., urothelium, lamina propria and detrusor muscle in contiguity. The outer-most surface of the detrusor muscle in the resected specimen could then be inked to assess margin status and thereby discerning a true perspective of level of resection, i.e., R0-R1 [Figure 4].
Figure 4.
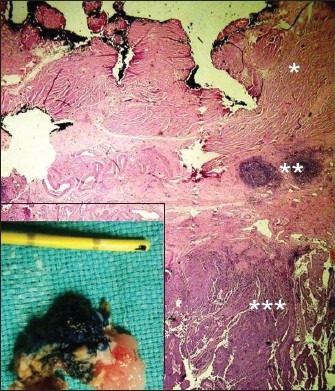
En-bloc resection provides a tissue piece of the bladder with all the layers in contiguity to assess the T stage and margin status. In inset, a 3 cm tumor removed en-bloc
Inadequacy of CT is not only judged by absence of detrusor muscle in an initial specimen, but also by the rate of recurrence. Recurrence is seen in 50-70% of non-muscle invasive bladder cancer, mostly during the 1st year.[6,11,12] These may be due to incomplete resection, cell implantation or the tumor biology itself.[13] Incomplete resection seems to be the most important reason for the recurrence. In a review of seven randomized controlled trials, after controlling established factors for recurrence such as tumor size, multiplicity, stage and grade, it was concluded that a wide range of recurrence rate, i.e., 0-46%, was due to the difference in quality of resection.[4] Inadequate resection leading to higher rate of recurrence at the same site is supported by another study where 81% of recurred tumor occurred at the site of previous resection.[5]
Various techniques using different kinds of loops and laser have been described to improve the quality of TURBT. En-bloc resection technique is one of the ways to provide better pathological evaluation for Ta and T1 tumors.[14] In a study on ET, a flat loop electrode was used to resect tumors of less than 2.5 cm.[14] Although the authors did not describe presence or absence of detrusor muscle in the resected specimen, they concluded that invasion of lamina was better delineated with en-bloc resection. A limitation of this technique was the inability to use a flat loop for tumors located at the anterior and upper posterior wall. Another limitation was that tumor of more than 2.5 cm was considered a contraindication.
It may not matter much whether we do ET or CT for a small size papillary tumor, but for tumors of 2-4 cm size, ET would give better tissue configuration for assessing the exact T stage and commenting on margin status. There is paucity of literature on ET for tumors of 2-4 cm size. We used a 45° angle loop electrode, which helped in scooping out the tumor in retrograde fashion. Once the tumor was resected en-bloc, removal of 4 cm size tumor from the urethra is a challenge particularly in a male patient. We could remove 3 cm size tumor in a female, but in males we had to cut the free lying tumor into two or three pieces. The most common technique was to place a nephroscope and hold the tumor with forceps to remove the whole assembly along with the tumor.
Results of this prospective non-randomized study have shown that recurrence rate in ET was significantly lower than CT. The progression rate, though not significant, was lower with ET. Best results of ET were seen in non-lamina invasive bladder cancer, where recurrence rate was reduced to 16% as compared with 53% with CT. Therefore, en-bloc resection not only provided a tissue piece with all the layers of bladder in contiguity for better histopathological characterization, but also resulted in reduction in the recurrence rate. Looking at the pattern of recurrence in our patients, it seems that ET is a better way to reduce the risk of recurrence as it provides a complete resection as only 1 (16%) patient had recurrence at the same site as compared to 6 (40%) patients in CT group 6 (40%) patients in CT group
Regarding the learning curve, ET is rather more controlled technique of resection than CT as it gives better hemostasis and thereby a good vision, which is crucial to avoid complications. Depth of the resection could also be modified with ET and it does not take more than three cases to get a knack of this technique if it is started with a relatively small tumor.
There are limitations of this study. First, tumor retrieval from the bladder was technically difficult and it had to be cut into 2-3 pieces once it was lying free in the bladder. Second, there could be surgeon related factors as CT was done by two different surgeons. Finally, it is not a randomized study.
CONCLUSION
The technique of TURBT is constantly evolving. It demands meticulous care and attention to achieve adequate cancer control and improve recurrence rates. In our study, though ET did not significantly affect the progression rate, it showed a significant reduction in the recurrence rate for NMIBC in comparison with CT. The concept of removing a bladder tumor by CT should be changed to a technique of en-bloc resection to provide better cancer control and long term outcome in non-muscle invasive bladder cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grasso M. Bladder cancer: a major public health issue. Eur Urol Suppl. 2008;7:510–15. [Google Scholar]
- 2.Raina V, Tyagi BB, Manoharan N. New Delhi: Delhi Cancer Registry, Dr. B.R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences; 2007. Mar, Cancer Incidence and Mortality in Delhi UT-Urban, 2002-2003. [Google Scholar]
- 3.Gupta P, Jain M, Kapoor R, Muruganandham K, Srivastava A, Mandhani A. Impact of age and gender on the clinicopathological characteristics of bladder cancer. Indian J Urol. 2009;25:207–10. doi: 10.4103/0970-1591.52916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brausi M, Collette L, Kurth K, van der Meijden AP, Oosterlinck W, Witjes JA, et al. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: A combined analysis of seven EORTC studies. Eur Urol. 2002;41:523–31. doi: 10.1016/s0302-2838(02)00068-4. [DOI] [PubMed] [Google Scholar]
- 5.Mariappan P, Smith G, Lamb AD, Grigor KM, Tolley DA. Pattern of recurrence changes in noninvasive bladder tumors observed during 2 decades. J Urol. 2007;177:867–75. doi: 10.1016/j.juro.2006.10.048. [DOI] [PubMed] [Google Scholar]
- 6.Saito S. Transurethral en bloc resection of bladder tumors. J Urol. 2001;166:2148–50. [PubMed] [Google Scholar]
- 7.Ukai R, Kawashita E, Ikeda H. A new technique for transurethral resection of superficial bladder tumor in 1 piece. J Urol. 2000;163:878–9. [PubMed] [Google Scholar]
- 8.Upadhyay R, Kapoor R, Srivastava A, Krishnani N, Mandhani A. Does En-bloc transurethral resection of bladder tumor give a better yield in terms of presence of detrusor muscle in the biopsy specimen? Indian J Urol. 2012;28:275–9. doi: 10.4103/0970-1591.102700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herr HW, Donat SM. A re-staging transurethral resection predicts early progression of superficial bladder cancer. BJU Int. 2006;97:1194–8. doi: 10.1111/j.1464-410X.2006.06145.x. [DOI] [PubMed] [Google Scholar]
- 10.Grimm MO, Steinhoff C, Simon X, Spiegelhalder P, Ackermann R, Vogeli TA. Effect of routine repeat transurethral resection for superficial bladder cancer: A long-term observational study. J Urol. 2003;170:433–7. doi: 10.1097/01.ju.0000070437.14275.e0. [DOI] [PubMed] [Google Scholar]
- 11.Parmar MK, Freedman LS, Hargreave TB, Tolley DA. Prognostic factors for recurrence and followup policies in the treatment of superficial bladder cancer: Report from the British Medical Research Council Subgroup on superficial bladder cancer (urological cancer working party) J Urol. 1989;142:284–8. doi: 10.1016/s0022-5347(17)38731-1. [DOI] [PubMed] [Google Scholar]
- 12.Sylvester RJ, Oosterlinck W, van der Meijden AP. A single immediate postoperative instillation of chemotherapy decreases the risk of recurrence in patients with stage Ta T1 bladder cancer: A meta-analysis of published results of randomized clinical trials. J Urol. 2004;171:2186–90. doi: 10.1097/01.ju.0000125486.92260.b2. 2435. [DOI] [PubMed] [Google Scholar]
- 13.Maruniak NA, Takezawa K, Murphy WM. Accurate pathological staging of urothelial neoplasms requires better cystoscopic sampling. J Urol. 2002;167:2404–7. [PubMed] [Google Scholar]
- 14.Herr HW. The value of a second transurethral resection in evaluating patients with bladder tumors. J Urol. 1999;162:74–6. doi: 10.1097/00005392-199907000-00018. [DOI] [PubMed] [Google Scholar]


