Abstract
Purpose
To prospectively analyze, using validated outcome measures, symptom improvement in patients with mild to moderate cubital tunnel syndrome treated with rigid night splinting and activity modifications.
Methods
Nineteen patients (25 extremities) were enrolled prospectively between August 2009 and January 2011 following a diagnosis of idiopathic cubital tunnel syndrome. Patients were treated with activity modifications as well as a 3 month course of rigid night splinting maintaining 45 degrees of elbow flexion. Treatment failure was defined as progression to operative management. Outcome measures included patient-reported splinting compliance as well as the Quick Disabilities of the Arm, Shoulder, and Hand questionnaire and the Short Form-12. Follow-up included a standardized physical examination. Subgroup analysis included an examination of the association between splinting success and ulnar nerve hypermobility.
Results
Twenty-four of 25 extremities were available at mean follow-up of 2 years (range 15-32 months). Twenty one of 24 (88%) extremities were successfully treated without surgery. We observed a high compliance rate with the splinting protocol during the 3-month treatment period. Quick Disabilities of the Arm, Shoulder, and Hand scores improved significantly from 29 to 11, Short Form-12 physical component summary score improved significantly from 45 to 54 and SF-12 mental component summary score improved significantly from 54 to 62. Average grip strength increased significantly from 32 kg to 35 kg, and ulnar nerve provocative testing resolved in 82% of patients available for follow-up examination.
Discussion
Rigid night splinting when combined with activity modification appears to be a successful, well-tolerated, and durable treatment modality in the management of cubital tunnel syndrome. We recommend that patients presenting with mild to moderate symptoms consider initial treatment with activity modification and rigid night splinting for 3 months based on a high likelihood of avoiding surgical intervention.
Keywords: Conservative, Cubital tunnel syndrome, Nonoperative, Splinting, Treatment
Introduction
Cubital tunnel syndrome is the second-most common nerve compression syndrome and is the most common site of ulnar nerve compression.[1,2] Research regarding the anatomy of the ulnar nerve and the causes of ulnar nerve dysfunction suggest that cubital tunnel syndrome is likely multifactorial with components of direct compression as well as traction on the nerve related to elbow flexion.[3,4] The degree of nerve dysfunction may be classified based on the work by McGowan, later modified by Dellon, that classifies nerve dysfunction as mild, moderate, or severe based on history and physical examination findings. Mild disease, Dellon 1, is limited to intermittent paresthesias and subjective weakness; moderate disease, Dellon 2, includes intermittent paresthesias and objective weakness; severe disease, Dellon 3, has persistent paresthesias and objective weakness with or without intrinsic atrophy.[1,5-7]
The initial treatment of cubital tunnel syndrome may be nonoperative, which includes activity modification, nerve gliding exercises, and splinting.[8-10] A trial of conservative care is considered appropriate for patients with Dellon 1 symptoms. An understanding of the increased extraneural and intraneural pressure demonstrated in ulnar nerve compression has helped to better define conservative treatment options, especially splinting. It has been shown that prolonged elbow flexion, static or repetitive, induces strain on the ulnar nerve and increased extraneural and intraneural pressures within the cubital tunnel. These intra and extraneural pressures are at their lowest mean values at an elbow position of 40 to 50 degrees of flexion, and pressures are significantly greater in full elbow flexion or extension.[11] The goals of splinting are to alleviate symptoms and prevent progressive nerve dysfunction.
Various forms of splinting have been used in the treatment of cubital tunnel syndrome ranging from padded sleeves to rigid thermoplastic custom-fit orthoses. Patient compliance with splinting regimens can be difficult and represents a limiting factor in the utility of this treatment. Outcomes have been examined but splint compliance and duration of splinting remains uncertain.[12-14] Additionally, the response of patients with Dellon 2 symptoms to conservative care is unclear.[9,12,15]
Our goal in this investigation was to prospectively analyze, with validated patient-rated outcome measures, symptom improvement in patients with mild to moderate cubital tunnel syndrome treated with rigid night splinting and activity modification. We also assessed splint compliance during the 3-month trial. We hypothesized that patients treated with a 3-month course of rigid night splinting and activity modification would comply with the splinting protocol and demonstrate a clinically relevant and statistically significant improvement in validated outcome measures of both upper extremity function and general health measures.
Materials and Methods
After institutional review board approval, patients were prospectively enrolled from our hand clinic between August 2009 and January 2011. Any adult patient diagnosed with an idiopathic cubital tunnel syndrome by typical findings on history, physical examination, and/ or nerve studies who was amenable to both nonoperative and operative treatment was eligible for inclusion. We graded the severity of cubital tunnel symptoms according to Dellon's classification. The distinction between mild, Dellon 1, and moderate, Dellon 2, disease was made based on weakness in grip/pinch strength of less than 80% of the contralateral, unaffected extremity. For those patients with bilateral disease, strength classification was based on Dellon's grip/pinch strength criteria as an uninvolved contralateral extremity was not available.[12] We excluded patients with severe, Dellon 3, disease as we advised them to have surgery. Patients with cubital tunnel syndrome secondary to elbow deformity, a congenital anomaly, a prior trauma, cervical radiculopathy, or previous elbow surgery were also excluded. Worker compensation patients were excluded due to potential confounding as a result of secondary gain considerations. While we did not exclude patients with a generalized neurological condition or diabetes, none of our patients had these conditions.
Nineteen patients (25 extremities) were enrolled. The 8 men and 11 women had a mean age of 43 years (range 21-72 years). There were 20 extremities with Dellon 1 disease and 5 with Dellon 2 disease. Symptoms had been present an average of 7 months (range, 1- 41 months) prior to presentation, and 5 patients had experienced symptoms for more than 6 months. Twenty four of the 25 extremities were available at a minimum follow-up of 1 year with a mean follow-up of 2 years (range 15-32 months). One patient with Dellon 2 disease was lost to follow-up and was excluded from final analysis.
All patients were treated with a rigid nighttime orthosis holding the elbow at a position of 45 degrees of flexion for 3 months. We allowed the orthosis (Hely & Weber, Santa Paula, CA) to be discontinued at 3 months. (Figure 1). The selected orthosis included malleable aluminum stays that allowed the orthosis to be molded to maintain the elbow at 45-degrees of flexion. In addition, each patient was given information regarding their diagnosis and various activity modifications to help reduce daytime aggravation of the ulnar nerve.
Figure 1.

Hely & Weber orthosis used in this investigation. The orthosis can be adjusted to keep the elbow at 45 degrees of flexion.
Patients were evaluated at enrollment and at 6 weeks, 3 months, 1 year, and at final follow-up as detailed below. Treatment failure was defined as progression to surgical intervention for cubital tunnel syndrome. The primary outcome measures were the Quick DASH, the SF-12, and self-reported splinting compliance during the first 3 months of treatment (100%, >80%, >50%, <50%, 0%). Treatment outcome was assessed by resolution or improvement of symptoms and improved QuickDASH and SF-12 scores. Per our standard clinical practice, all patients were requested to attempt conservative management with night splinting for a minimum of 3 months. After that, any persistent symptoms deemed unacceptable by the patient could be treated surgically.
Subjective Assessment
The QuickDASH and SF-12 questionnaires were completed at study enrollment for baseline data and at 6 weeks, 3 months, and at a minimum 1 year follow- up for final evaluation. The DASH is a 30-item questionnaire that measures function, symptoms, and quality-of-life issues related to upper extremity pathology.[16] It is scored from 0 to 100 with a higher score representing greater disability and a minimal clinically important difference of 10 points.[17] It has been validated and tested for reproducibility.[18,19] The QuickDASH is an 11-item version of the DASH that has been shown to correlate well with the DASH score in previous studies.[17]
The SF-12 is an abbreviated version of the Short-Form Health Survey 36 (SF-36). It is valid and reliable in the general population as a general health measurement scale. The SF-12 has 12 items and produces 2 summary scores: the physical component summary and the mental component summary scores. The SF-12 summary scores are highly correlated with the summary scores obtained from the full SF-36. The physical component summary and the mental component summary are norm-based T scores with a mean of 50 (SD 10) in the general population. Higher scores correlate with better health related quality of life. The minimal clinically important difference is estimated between 3-5 points for each subscale.[20,21]
Physical Examination
We performed a physical examination at initial and subsequent evaluations including quantitative grip strength (Jamar Dynamometer, Lafayette Instrument Company, Lafayette, IN), pinch strength (B&L Engineering, Santa Ana, CA), the presence or absence of Froment sign, and strength assessment of the first dorsal interosseous and flexor digitorum profundus to small finger (as graded by British Medical Council). Grip and pinch strength measurements were made on single maximal effort measures with the dynamometer in position 2. Grip and pinch strength were compared to the uninvolved contralateral side with less than 80% strength considered a significant difference representing moderate, Dellon 2, disease.
We used static 2-point discrimination of the small finger to assess for sensory changes in comparison to the contralateral hand as well as median nerve innervated digits and considered a discrimination greater than 5mm abnormal. Additionally, we performed provocative ulnar nerve testing, including a Tinel sign at the elbow and an elbow flexion compression test.[5] We assessed for a Tinel sign by applying 4 to 6 taps to the patient's ulnar nerve just proximal to the cubital tunnel. We recorded the presence or absence of the patient experiencing a tingling sensation in the small finger. We also assessed for a combined flexion with pressure provocation test by placing the patient's elbow in maximum flexion and, while in this position, placing pressure on the ulnar nerve just proximal to the cubital tunnel. We applied the test for a maximum of 60 seconds seeking reproduction of paresthesias in the ring or small finger. These data were used to determine severity and patients were classified according to Dellon. Finally, we evaluated all patients for stability of the ulnar nerve at the cubital tunnel and classified nerves as stable or unstable. Nerves were considered unstable if they were perchable, perching, or dislocating at the time of initial presentation.[22]
Nerve Studies
Electromyography and nerve conduction studies were performed on 20 of the 25 extremities and were positive in 17. The 17 with positive studies had slowed ulnar nerve conduction velocity across the elbow (judged against laboratory normal value provided on each study), but all had normal EMG findings. Four patients (5 elbows) declined electrophysiological studies but were included in the final analysis based on characteristic history and physical examination indicating cubital tunnel syndrome.[1] All 5 of these elbows had Dellon 1 cubital tunnel syndrome without intrinsic weakness.
Statistical Methods
An initial power analysis was conducted in order to determine the sample size needed for this study. The minimum detectable change of the DASH at 95% confidence is assumed to be 13 DASH points (SD 15 from the normative general population data). Therefore, to test the null hypothesis of equality of treatment group to pre-treatment group at P=0.05 with 80% power and assuming a uniform dropout rate of 10%, we determined that 25 extremities would be sufficient.
The results of the QuickDASH and SF-12 questionnaires and clinical variables were recorded at initial presentation and at each follow-up interval. A 2-sample paired t-test was used to evaluate the mean changes in QuickDASH score and SF-12 between the pre and post treatment visits. A Bonferroni correction was applied due to the multiple comparisons (P<0.0125 significant). Missing data were excluded during analysis.
Results
Twenty-one of 24 extremities were treated successfully without surgery, an 88% success rate. This included 18 of 20 Dellon 1 and 3 of 4 Dellon 2 cases. We analyzed the primary patient-rated outcome measures, the QuickDASH and SF-12 physical component summary and mental component summary, for the 21 successfully treated extremities (Table 1). All were significantly improved by the 3-month follow-up through final follow-up; none of those successfully treated by splinting and activity modification had worsening of the Dellon stage.
Table 1.
Patient-rated outcome measures collected during study.
| Initial | 6 Weeks | P value | 3 Months | P value | 1 Year | P value | Final | P value | |
|---|---|---|---|---|---|---|---|---|---|
| QuickDASH | 29 | 16.4 | <0.001* | 10.9 | <0.001* | 8.7 | <0.001* | 10.5 | <0.001* |
| SF-12 PCS | 45 | 48 | 0.05 | 52.3 | <0.001* | 54.8 | <0.001* | 53.6 | <0.001* |
| SF-12 MCS | 54.3 | 57.6 | 0.1 | 60.3 | 0.003* | 61.2 | <0.001* | 61.9 | <0.001* |
Statistically significant at P<0.0125
Patients were compliant with the orthosis at least 80% of the time for 15 of the 18 patients (24 extremities) available for follow-up at 6 weeks and 14 of the 18 patients at 3 months (Figure 2). The patients unable to adhere to the splinting protocol at least 50% of the time cited pain at the medial and/or lateral bony prominences of the elbow as the major reason for non-compliance. At the end of the 3- month trial, 4 patients continued intermittent orthosis wear for cubital tunnel symptom flare episodes. All continued to modify daily activities to minimize ulnar nerve symptoms as long as these modifications did not limit their daily life. Those modifications deemed to be necessary for daily life (i.e. overhead lifting activities and exercises) were resumed once nerve symptoms improved. Activity resumption did not cause symptom recurrence.
Figure 2.
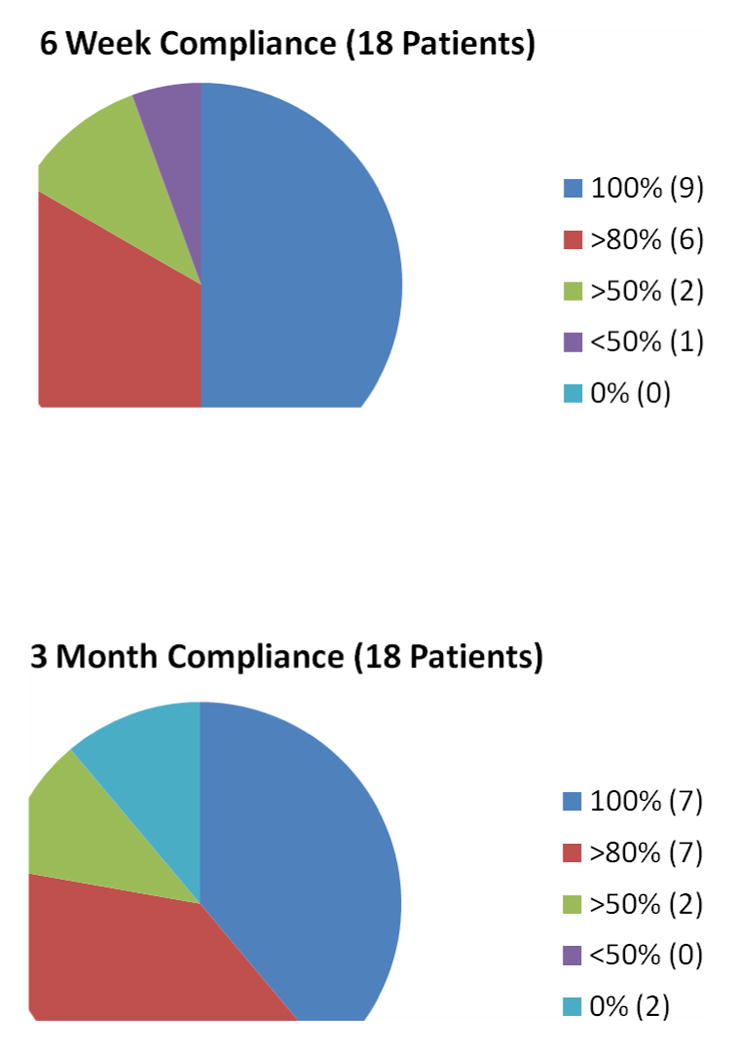
Night splinting compliance at 6 weeks and 3 months.
Eleven of the 21 successfully treated extremities were available for a final physical examination by a surgeon not involved in the initial care of the patient at an average of 22 months from initial presentation. Average grip strength of the affected extremity increased from 32kg (+/- 15) to 35kg (+/- 15) (P=0.04). Key pinch strength of the affected extremity remained unchanged at 10kg (+/-2). The 2 extremities initially presenting with a Froment sign resolved at follow- up. There were 2 extremities with decreased strength of the first dorsal interosseous muscle pre-treatment, with a British Medical Council strength of 4, and both were normal at follow- up. Similarly, 3 extremities had 4/5 flexor digitorum profundus strength of the small finger pre-treatment and improved to 5/5 at final follow-up. Three extremities had abnormal two-point discrimination (8 mm for each) of the small finger pre-treatment. These normalized at follow- up. Nine of 11 extremities had resolution of provocative ulnar nerve tests at final follow-up.
Sixteen of the 24 extremities had a stable ulnar nerve, and 15 of these had symptom resolution with splinting. There were 8 unstable ulnar nerves, and 6 had symptom resolution with splinting.
Treatment Failures
Three patients had persistent symptoms and underwent surgery. One patient wore her splint less than 50% of the time due to medial elbow boney prominence pain, and another wore her splint more than 80% of the time. The third patient had bilateral symptoms and wore his splint 100% of the time for the first 3 months. He had resolution of symptoms on his non-dominant left side; but secondary to continued symptoms on his dominant side, he underwent surgery 1 year after initiating nonoperative treatment..
Discussion
Eighty-eight percent of patients in this cohort with mild or moderate symptoms were treated successfully with rigid night splinting and activity modifications. Both QuickDASH and SF-12 scores showed statistically and clinically relevant improvement within 3 months of treatment. The improvements noted at 3 months were maintained at final average follow-up of 2 years.
The role of conservative treatment for patients with mild to moderate cubital tunnel symptoms is unclear. Previous authors have found that those presenting with mild, acute symptoms may resolve spontaneously or can be treated with information and activity modifications to relieve ulnar nerve irritation.[23-25] Eisen et al. followed 22 patients with mild symptoms for a mean of 22 months and noted 90% spontaneous recovery.[26] However other authors have concluded that those with moderate symptoms will fail conservative management.[1]
Night splinting has long been considered a staple of conservative treatment for cubital tunnel syndrome, but 2 issues bear consideration: the ability of the splint to maintain the elbow at the ideal position of 40-50 degrees of flexion[11] and patient compliance with night splinting. An evaluation of various elbow orthoses by Apfel et al. demonstrated that only the Hely & Weber cubital tunnel splint, an adjustable rigid orthosis with stockinet arm bands, was rigid enough to prevent flexion beyond 53 degrees and also prevent full extension; other splints failed to maintain a position of mid-flexion.[27] Our experience with the Hely & Weber splint has been similar, and we believe it effectively immobilizes the elbow at 45 degrees of flexion.
Patient compliance is vital to the effectiveness of night splinting for cubital tunnel. Previous studies have failed to quantitatively evaluate patient compliance with splinting protocols. In our current cohort, the relatively short duration of treatment (3 months) seems to be well tolerated by a majority of our patients. Over 80% of our cohort wore their rigid night splints greater 80% of the time with less than 5-10% of patients wearing it less than 50% of the time. Factors that seem to influence patient compliance include splinting with a comfortable, non-bulky splint for a relatively short duration treatment period of 3 months.
There is no consensus on the treatment length for rigid night splinting. Seror studied 22 patients treated with night splinting for 6 months and showed success similar to ours.[13] Dellon et al, prospectively evaluated 121 patients given conservative treatment for 3 to 6 months. Treatments ranged from nighttime towel wrapping to thermoplastic splinting along with daytime activity modifications. After 6 months of treatment, their success rate was 42% for those with mild symptoms and 34% for those with moderate symptoms. Additionally, the need for surgical intervention was 21% within 6 years for those with mild symptoms and 33% within 3 years for those with moderate symptoms.[12] This is in comparison to our surgical intervention rate of 13% at 2 years with a more standardized, but shorter treatment protocol.
One previous study suggested that night splinting was not more effective than other conservative treatment modalities. Svernlöv et al. prospectively evaluated 57 patients with nerve gliding exercises, splinting, or information aimed at protecting the ulnar nerve and reported that there was no treatment benefit of night splinting compared to the other groups as 51 of 57 patients were improved at 6 months. Their population, despite including Dellon 1 and 2 patients, was different than ours as 85% of our patients had positive nerve studies while 76% of their patients had normal nerve studies. Additionally, patient compliance with splinting was not recorded, and the orthosis they used was meant to prevent elbow flexion beyond 45 degrees, but it was unclear how successful it was at preventing flexion or if it was able to prevent full extension.[14] This study provides useful information and supports the concept that many of these patients will improve with conservative measures.
The primary weakness of our study was the lack of a control group from which we could assess the natural history of untreated, mild cubital tunnel symptoms. A randomized trial with a splinting group and an observational group and/ or an activity modification group would be the ideal. Additionally, our study population was predominately Dellon 1 patients and 4 Dellon 2 patients. While 3 of the 4 Dellon Type 2 patients improved during the course of this study, they represented a small cohort of moderately affected patients.
Based on the findings of this study, we treat patients with mild to moderate cubital tunnel symptoms with instructions on activity modification and rigid night splinting for 3 months prior to surgical consideration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dellon AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am. 1989;14(4):688–700. doi: 10.1016/0363-5023(89)90192-5. [DOI] [PubMed] [Google Scholar]
- 2.Bozentka DJ. Cubital tunnel syndrome pathophysiology. Clin Orthop Relat Res. 1998;(351):90–94. [PubMed] [Google Scholar]
- 3.Britz GW, Haynor DR, Kuntz C, et al. Ulnar nerve entrapment at the elbow: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery. 1996;38(3):458–465. doi: 10.1097/00006123-199603000-00007. discussion 465. [DOI] [PubMed] [Google Scholar]
- 4.Feindel W, Stratford J. Cubital tunnel compression in tardy ulnar palsy. Can Med Assoc J. 1958;78(5):351–353. [PMC free article] [PubMed] [Google Scholar]
- 5.Novak CB, Lee GW, Mackinnon SE, Lay L. Provocative testing for cubital tunnel syndrome. J Hand Surg Am. 1994;19(5):817–820. doi: 10.1016/0363-5023(94)90193-7. [DOI] [PubMed] [Google Scholar]
- 6.Listed NA. Practice parameter: electrodiagnostic studies in ulnar neuropathy at the elbow. American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation. Neurology. 1999;52(4):688–690. doi: 10.1212/wnl.52.4.688. [DOI] [PubMed] [Google Scholar]
- 7.McGowan A. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32-B(3):293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 8.Byron P. Upper extremity nerve gliding: programs used at the Philadelphia Hand Center. In: Hunter J, Mackin E, Callahan A, editors. Rehabilitation of the Hand: Surgery and Therapy. 4th. St Louis: Mosby; 1995. pp. 951–956. [Google Scholar]
- 9.Coppieters MW, Bartholomeeusen KE, Stappaerts KH. Incorporating nerve-gliding techniques in the conservative treatment of cubital tunnel syndrome. J Manipulative Physiol Ther. 2004;27(9):560–568. doi: 10.1016/j.jmpt.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Oskay D, Meric A, Kirdi N, et al. Neurodynamic mobilization in the conservative treatment of cubital tunnel syndrome: long-term follow-up of 7 cases. J Manipulative Physiol Ther. 2010;33(2):156–163. doi: 10.1016/j.jmpt.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Gelberman RH, Yamaguchi K, Hollstien SB, et al. Changes in interstitial pressure and cross-sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow. An experimental study in human cadavera. J Bone Joint Surg Am. 1998;80(4):492–501. doi: 10.2106/00004623-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Dellon AL, Hament W, Gittelshon A. Nonoperative management of cubital tunnel syndrome: an 8-year prospective study. Neurology. 1993;43(9):1673–1677. doi: 10.1212/wnl.43.9.1673. [DOI] [PubMed] [Google Scholar]
- 13.Seror P. Treatment of ulnar nerve palsy at the elbow with a night splint. J Bone Joint Surg Br. 1993;75(2):322–327. doi: 10.1302/0301-620X.75B2.8444959. [DOI] [PubMed] [Google Scholar]
- 14.Svernlov B, Larsson M, Rehn K, Adolfsson L. Conservative treatment of the cubital tunnel syndrome. J Hand Surg Eur Vol. 2009;34(2):201–207. doi: 10.1177/1753193408098480. [DOI] [PubMed] [Google Scholar]
- 15.Szabo RM, Kwak C. Natural history and conservative management of cubital tunnel syndrome. Hand Clin. 2007;23(3):311–318. v–vi. doi: 10.1016/j.hcl.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 17.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDermid JC, Richards RS, Donner A, Bellamy N, Roth JH. Responsiveness of the short form-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg Am. 2000;25(2):330–340. doi: 10.1053/jhsu.2000.jhsu25a0330. [DOI] [PubMed] [Google Scholar]
- 19.Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–146. [PubMed] [Google Scholar]
- 20.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med. 2001;33(5):344–349. doi: 10.3109/07853890109002088. [DOI] [PubMed] [Google Scholar]
- 22.Calfee RP, Manske PR, Gelberman RH, et al. Clinical assessment of the ulnar nerve at the elbow: reliability of instability testing and the association of hypermobility with clinical symptoms. J Bone Joint Surg Am. 2010;92(17):2801–2808. doi: 10.2106/JBJS.J.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szabo RM. Entrapment and compression neuropathies. In: Green DP, editor. Green's Operative Hand Surgery. 4th. New York, NY: Churchill-Livingstone; 1999. [Google Scholar]
- 24.Folberg CR, Weiss AP, Akelman E. Cubital tunnel syndrome. Part II: Treatment. Orthop Rev. 1994;23(3):233–241. [PubMed] [Google Scholar]
- 25.Sailer SM. The role of splinting and rehabilitation in the treatment of carpal and cubital tunnel syndromes. Hand Clin. 1996;12(2):223–241. [PubMed] [Google Scholar]
- 26.Eisen A, Danon J. The mild cubital tunnel syndrome. Its natural history and indications for surgical intervention. Neurology. 1974;24(7):608–613. doi: 10.1212/wnl.24.7.608. [DOI] [PubMed] [Google Scholar]
- 27.Apfel E, Sigafoos GT. Comparison of range-of-motion constraints provided by splints used in the treatment of cubital tunnel syndrome--a pilot study. J Hand Ther. 2006;19(4):384–391. doi: 10.1197/j.jht.2006.07.028. quiz 392. [DOI] [PubMed] [Google Scholar]


