Abstract
Pancreatitis is a very rare adverse effect of quetiapine treatment, with only 5 cases of quetiapine-associated pancreatitis reported in the English literature to date. Herein, we report one patient who developed severe hypertriglyceridemia (>1000 mg/dL) after quetiapine administration, resulting in acute pancreatitis. An analysis of the underlying pathogenic mechanisms and a review of relevant literature are also presented. Clinicians should be aware of the potentially life-threatening metabolic disturbances and/or pancreatitis associated with quetiapine therapy.
Keywords: Quetiapine, hypertriglyceridemia, pancreatitis
INTRODUCTION
Quetiapine is one of the second-generation antipsychotic medications. Although second-generation antipsychotics have been associated with pancreatitis, pancreatitis is a very rare adverse effect of quetiapine treatment, with only 5 cases of quetiapine-associated pancreatitis reported in the English literature to date. Herein, we report one patient who developed both severe hypertriglyceridemia and acute pancreatitis after quetiapine administration. With this case report, we also present a review of the published cases of quetiapine-induced pancreatitis in an attempt to increase awareness of the risk of pancreatitis associated with quetiapine usage.
CASE REPORT
A 51-year-old woman with a history of bipolar affective disorder was presented to our hospital with an 8-h history of nausea and epigastric pain radiating caudally. Three months prior to admission, an elevated serum triglyceride level (408 mg/dL) was noted, but the patient didn't receive any lipid-lowering agents. Two months before presentation, she was treated for bipolar effective disorder with valproic acid 500 mg twice daily, quetiapine 600 mg at bedtime, and flurazepam 30 mg at bedtime. One month prior to admission, valproic acid was tapered and stopped, and quetiapine dose had been increased to 800 mg at bedtime. At current presentation, she was taking both quetiapine 800 mg and flurazepam 30 mg at bedtime. There was no history of alcohol abuse, recent abdominal trauma or surgery, preceding viral syndromes, or cholelithiasis, and no other concomitant medications were being used.
The initial physical examination indicated a diffuse abdominal tenderness without muscle guarding or rebound tenderness, and hypoactive bowel sounds were auscultated. Laboratory studies showed a leukocyte count of 9.9×109/L, with a differential count of 68% neutrophils and 24% lymphocytes. Serum electrolytes and liver function tests were within normal limits. Other pertinent laboratory values included a serum amylase of 352 IU/L (normal, 30-110 IU/L), serum lipase of 1210 IU/L (normal, 23-300 IU/L), triglyceride of 1508 mg/dL (normal, 35-150 mg/dL), and a total cholesterol level of 450 mg/dL (normal, 130-200 mg/dL). Abdominal ultrasound showed no evidence of gallbladder disease or dilatation of the bile ducts. Abdominal computed tomography showed a blurring contour from pancreatic head to tail, with minimal fluid collection at the pancreatic head region. A diagnosis of acute pancreatitis was made.
Then the patient was treated symptomatically with volume repletion and meperidine for pain relief. Quetiapine was suspected as the cause of severe hypertriglyceridemia, and was immediately withdrawn. In addition, treatment with oral fenofibrate 160 mg daily was commenced for reducing serum triglycerides. Ten days later, the patient was free of abdominal pain, the serum amylase and lipase values were normal, and the triglyceride level was reduced to 337 mg/dL. The patient was discharged on the following medications: aripiprazole 5 mg at bedtime, flurazepam 60 mg at bedtime, and fenofibrate 160 mg once daily. The patient was discharged with appointments for follow-up with the endocrinology and psychiatry services. She was asymptomatic at the 3-month follow-up.
DISCUSSION
Acute pancreatitis may be a severe disease with a high rate of morbidity and mortality. It can be caused by gallstones or alcoholism, and there are also reports of drug-induced, bacterial or viral-related, postsurgery, and genetic forms.1 Gallstones and alcoholism account for the causes of 75% of pancreatitis in one report.2 In contrast, drug-induced pancreatitis was relatively rare, with a reported incidence of 0.1-2%.3 Although over 500 drugs have been linked to pancreatitis, the pathophysiology of drug-induced pancreatitis is still unclear.4 Some hypotheses suggest that drug-induced pancreatitis is due to an accumulation of toxic metabolites, a hypersensitivity reaction to the drugs, or a consequence of drug-related metabolic effects such as hypertriglyceridemia.5 Herein, we presented one patient of severe hypertriglyceridemia (>1000 mg/dL) after quetiapine administration, resulting in acute pancreatitis.
Large triglyceride increases have been reported in patients receiving quetiapine therapy.6 As the triglycerides removal is a saturable process, substantial quetiapine-induced enhancement in lipid levels may occur in some patients with a preexisting hypertriglyceridemia that are near the point of saturation. Indeed, our patient had a triglyceride level of 408 mg/dL before quetiapine administration. After a 2-month period of quetiapine administration, serum triglyceride level increased to 1508 mg/dL, without any dietary changes or alcohol consumption. When triglyceride levels are elevated, chylomicrons tend to be present, and may obstruct capillaries, leading to pancreatitis. Moreover, excess free fatty acids from triglycerides may lead to further cytotoxic injury, releasing inflammatory mediators and aggravating the pancreatitis.7
Table 1 summarized 6 cases with acute pancreatitis resulting from quetiapine therapy.8,9,10 Most outcomes were favorable and the pancreatitis, if recognized early and treated promptly, was resolved with supportive treatment. These reports demonstrated that severe hypertriglyceridemia may not be the only pathophysiology of quetiapine-induced acute pancreatitis, as hypertriglyceridemia was not reported in one case when acute pancreatitis developed. Further studies are clearly required to clarify the pancreatotoxicity of quetiapine. However, in those patients with a history of hypertriglyceridemia, such as in this case, quetiapine should be used more cautiously, owing to the severe and life-threatening adverse effects. Among these reported cases, the dosage and frequency of quetiapine therapy varied largely. Almost all pancreatitis developed more than 1 month after quetiapine administration was started. Therefore, it is important to consider quetiapine as a possible cause of acute pancreatitis in patients presenting with pancreatitis after several weeks of quetiapine exposure, even those receiving a low dosage.
Table 1.
Published Cases of Quetiapine-Induced Pancreatitis
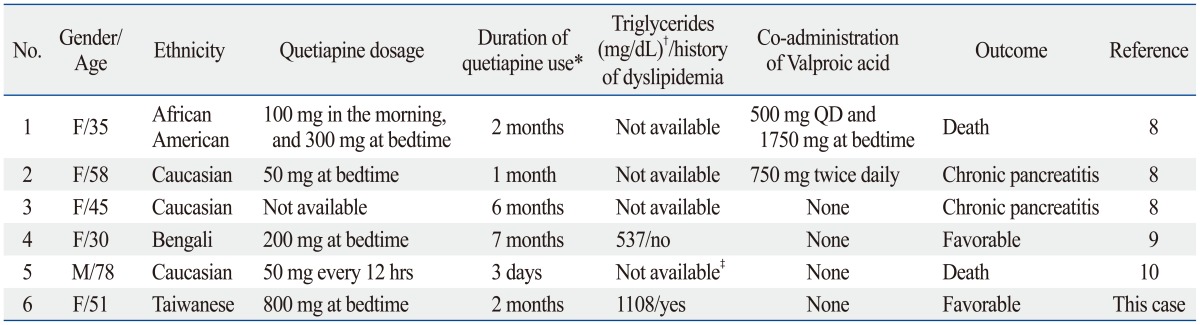
QD, every day.
*The period from initiation of quetiapine to onset of acute pancreatitis.
†Fasting serum triglyceride levels when acute pancreatitis developed.
‡In the case report, the authors stated no hypertriglyceridemia was observed.
In conclusion, clinicians should be aware that when treating patients with quetiapine, metabolic disturbances and/or pancreatitis can occur with potentially life-threatening results. Furthermore, it would seem prudent to monitor fasting lipids more frequently in patients on quetiapine, especially in patients with a preexisting dyslipidemia. When hyperlipidemia is detected before initiation of quetiapine, an appropriate diet and drug treatment are suggested to minimize the risk of hypertriglyceridemia-induced acute pancreatitis.7
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Frossard JL, Steer ML, Pastor CM. Acute pancreatitis. Lancet. 2008;371:143–152. doi: 10.1016/S0140-6736(08)60107-5. [DOI] [PubMed] [Google Scholar]
- 2.Cappell MS. Acute pancreatitis: etiology, clinical presentation, diagnosis, and therapy. Med Clin North Am. 2008;92:889–923. doi: 10.1016/j.mcna.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Balani AR, Grendell JH. Drug-induced pancreatitis : incidence, management and prevention. Drug Saf. 2008;31:823–837. doi: 10.2165/00002018-200831100-00002. [DOI] [PubMed] [Google Scholar]
- 4.Nitsche CJ, Jamieson N, Lerch MM, Mayerle JV. Drug induced pancreatitis. Best Pract Res Clin Gastroenterol. 2010;24:143–155. doi: 10.1016/j.bpg.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Badalov N, Baradarian R, Iswara K, Li J, Steinberg W, Tenner S. Drug-induced acute pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007;5:648–661. doi: 10.1016/j.cgh.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Duncan EJ, Woolson SL, Hamer RM, Dunlop BW. Risk of lipid abnormality with haloperidol, olanzapine, quetiapine, and risperidone in a Veterans Affairs population. Int Clin Psychopharmacol. 2009;24:204–213. doi: 10.1097/YIC.0b013e32832d6c18. [DOI] [PubMed] [Google Scholar]
- 7.Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH, et al. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:2969–2989. doi: 10.1210/jc.2011-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gropper D, Jackson CW. Pancreatitis associated with quetiapine use. J Clin Psychopharmacol. 2004;24:343–345. doi: 10.1097/01.jcp.0000126667.90691.88. [DOI] [PubMed] [Google Scholar]
- 9.Rashid J, Starer PJ, Javaid S. Pancreatitis and diabetic ketoacidosis with quetiapine use. Psychiatry (Edgmont) 2009;6:34–37. [PMC free article] [PubMed] [Google Scholar]
- 10.Potolidis E, Mandros C, Karakitsos D, Kountra PM. Quetiapine-associated pancreatitis in a geriatric critical care patient with delirium. Case Rep Psychiatry. 2012;2012:625954. doi: 10.1155/2012/625954. [DOI] [PMC free article] [PubMed] [Google Scholar]


