Abstract
Purpose
To investigate clinical implications of delta neutrophil index (DNI) to discriminate adult onset Still's disease (AOSD) from sepsis.
Materials and Methods
We reviewed the medical records of 13 patients with AOSD and 33 gender and age-matched patients with sepsis. In all subjects, microbial tests were performed to exclude or confirm sepsis. All laboratory data were measured two or three times during the first 3 days and represented by their mean levels. DNI was measured automatically by ADVIA 2120 for the first 3 days.
Results
There were no significant differences in white blood cell counts, neutrophil proportion, erythrocyte sedimentation rate and C-reactive protein between two groups. AOSD patients had notably lower DNI than sepsis patients regardless of the presence of bacteremia or not. However, both DNI and ferritin were not significant independent factors for predicting sepsis in the multivariate logistic regression analysis. Meanwhile, the area under the receiver operating characteristic curve (AUROC) of DNI was slightly higher than that of ferritin. When we set DNI of 2.75% as the cut-off value for predicting sepsis, 11 (84.6%) of AOSD patients had a DNI value below 2.75% and 2 (15.4%) of them had a DNI over 2.75% (relative risk for sepsis 176).
Conclusion
We suggest that DNI may be a useful marker for differential diagnosis of AOSD from sepsis in the early phase as supplementary to ferritin.
Keywords: Adult onset still's disease, delta neutrophil index, sepsis
INTRODUCTION
Adult-onset Still's disease (AOSD) is a systemic inflammatory disorder of unknown etiology.1 Several classification criteria for AOSD have so far been suggested, however, there are no objective laboratory tests for its diagnosis.2,3 Thus, diagnosis of AOSD is still based on heterogeneous clinical manifestations and laboratory results with exclusion of other febrile conditions.1 Especially in early phase, it is difficult to differentiate AOSD from infection due to their indistinguishable symptoms and laboratory findings, such as fever and leukocytosis. In order to distinguish the two diseases in early phase, several efforts have so far been made, however, a specific biomarker has not yet been established.4,5,6 Novel biomarkers that could represent the disease activities had been studied in other autoimmune inflammatory diseases.7
Delta neutrophil index (DNI) is an automatically calculated parameter that reflects the ratio of immature granulocytes (IGs) over total neutrophil count in the peripheral circulation 8.8,9 IGs are hematologic cells that do not reach full maturation of complete neutrophil nuclear lobulation,10 and are usually released to peripheral blood by catecholamines and pro-inflammatory cytokines in sepsis.11 DNI has been reported to be more predictive of sepsis severity and prognosis than traditional marker including white blood cell (WBC) counts, absolute neutrophil counts and C-reactive protein (CRP).8,9,12,13 With these reasons, DNI may be considered useful for discriminating AOSD from sepsis, but its clinical application has not been reported to date. In this study, therefore, we investigated clinical implications of DNI for discriminating the two diseases in early phase.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of 16 patients with AOSD with 19 episodes of fever at admission. They were admitted for fever at Yonsei University Medical Center from Jan 2010 to Mar 2012. Three patients were excluded because they had no febrile events at admission, and three episodes were excluded because microbial infections were confirmed through culture studies. All patients fulfilled Yamaguchi's criteria for AOSD,3 and had febrile episode at admission. We also reviewed the medical records of 33 gender- and age-matched patients who were admitted to the same institute during the same period, and who were diagnosed with sepsis, excluding hematologic disorder. Sepsis is defined as a systemic inflammatory response syndrome (SIRS) accompanied by proven microbial infection. SIRS was defined as two or more of the following conditions: 1) body temperature >38℃ or <36℃; 2) leukocytosis >12000/µL, leucopenia (<4000/µL); 3) heart rate >90 beats/min; 4) respiratory rate >24/min.8 Bacteremia was defined as the presence of microbial organisms in blood culture. This study was approved by the Institutional Review Board of Severance Hospital.
Data collection
On the first day of hospitalization, physicians assessed clinical manifestations, including fever, typical rash, arthralgia/arthritis, lymphadenopathy, sore throat, and abdominal pain. Splenomegaly or hepatomegaly was evaluated by abdominal CT scanning or ultrasonography. Pleuritis, pericarditis and pneumonitis were confirmed by chest X-ray or chest CT scanning or echocardiography. Kidney involvement was also assessed and defined as hematuria >5 red blood cells per high-power field or proteinuria >500 mg more than twice per 24 h on urinalysis. Laboratory data including WBC count, erythrocyte sedimentation rate (ESR), CRP, and ferritin were measured two or three times during the first 3 days and represented by their mean levels. In all subjects, microbial tests on blood, urine, sputum and sources suspected of infection were performed to confirm infectious disease.
Measurement of DNI
DNI was calculated by an automatic cell analyzer (ADVIA 2120 Hematology System, Siemens Healthcare Diagnostics, Forchheim, Germany) two or three times during the first 3 days. DNI was calculated using the following formula: DNI=[the neutrophil sub fraction and the eosinophil sub fraction measured in the myleoperioxidase (MPO) channel by the cytochemical MPO reaction]-[the polymorphic neutrophils (PMN) sub fraction measured in the nuclear lobularity channel by the reflected light beam].8
Statistical analysis
Mean differences in continuous variables between two groups were evaluated using Mann-Whitney U test, and among three groups by Kluskal-Wallis test. A chi-squared test was applied to determine the gender distribution and frequencies of clinical manifestations between the groups. Variables that had statistical significance (p-value <0.05) in univariate analysis were assessed using binary logistic regression to examine the odds ratio of DNI for predicting sepsis. Sensitivity and specificity of the cut-off value related to DNI was set using the receiver operating characteristic (ROC) curve. Statistical analyses were performed using the SPSS for Windows software (version 18.0, SPSS Inc., Chicago, IL, USA). Comparison of area under the receiver operating characteristic curve (AUROC) was performed using MedCalc (version 12.3.0, Ostend, Belgium). In all analyses, p-value <0.05 indicated statistical significance.
RESULTS
Clinical characteristics of patients with AOSD and those with sepsis
Clinical characteristics of all patients are described in Table 1. Mean age of AOSD patients (male 3, female 10) was 43.9±13.4 years old and that of sepsis patients (male 8, female 25) was 48.8±11.0 years old. The most common clinical manifestation in AOSD patients was fever (100%), followed by arthralgia/arthritis (92.3%), typical rash (69.2%) and sore throat (61.5%). Lymphadenopathy, organomegaly and pleuritis were also presented in patients with sepsis (21.2%, 6.1%, and 15.2%). Fever was documented, and microbial organisms were confirmed in all patients with sepsis. Twenty-four of 33 patients with sepsis (72.7%) had bacteremia. Eighteen (54.5%), 3 (9.1%), and 2 (6.1%) of sepsis patients had urinary tract infections, biliary infections and pneumonia, respectively. Other infections included infective endocarditis (n=1), peritonitis (n=1) and cytomegalovirus (CMV) infection (n=1).
Table 1.
Clinical Characteristics of Patients with AOSD and Those with Sepsis
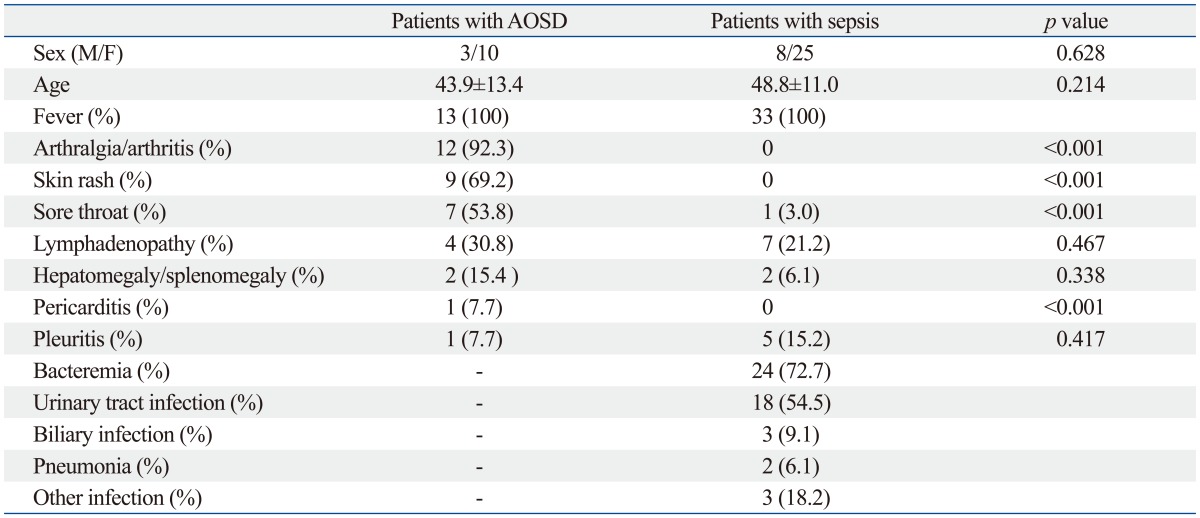
AOSD, adult onset Still's disease.
The number of patients with AOSD were 13 and that of patients with sepsis were 33. Biliary infection: confirmed microbial growth in bile through culture study. Values are expressed as the mean±standard deviation.
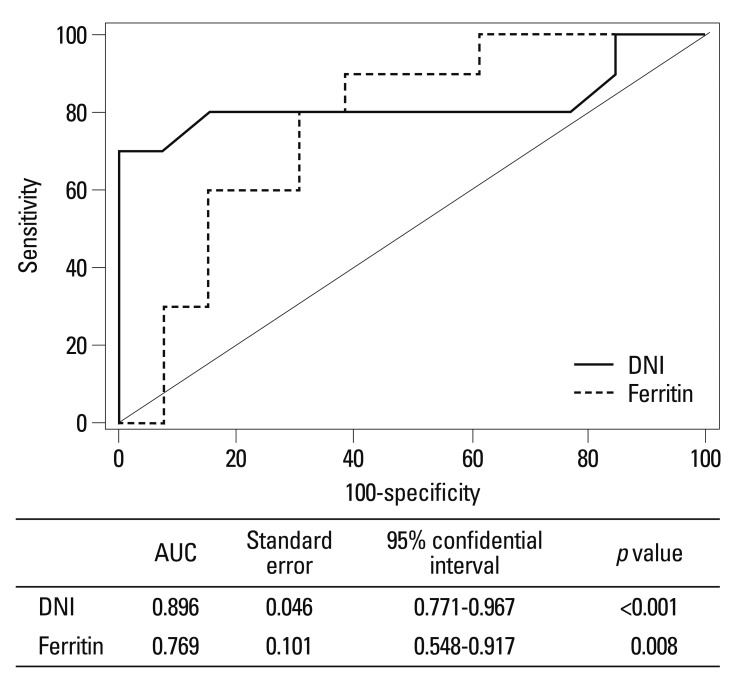
Univariate and multivariate analysis
There were no significant differences in WBC counts or neutrophil proportions between the two groups. AOSD patients had significantly lower mean DNI than sepsis patients (1.8±1.0% vs. 9.1±7.6%, p<0.001), while ESR and CRP levels were not different between the two groups. Ferritin levels in AOSD patients were elevated compared to sepsis patients (5565.8±6536.8 vs. 891.5±1100.6, p=0.030). Sepsis patients had lower albumin level and higher total bilirubin level than AOSD patients (Table 2). We performed a binary logistic regression analysis of these variables with significant differences, and found that the usefulness of DNI did not surpass that of ferritin for differential diagnosis sepsis from AOSD (Table 2). Meanwhile, we compared AUROC of ferritin and the DNI, and found that AUROC of the DNI had slightly higher than that of ferritin, but difference of area was not statically significant [area under curve (AUC)=0.896 vs. AUC=0.769, p=0.68] (Fig. 1).
Table 2.
Laboratory Results between Patients with AOSD and Those with Sepsis in Univariate and Multivariate Analysis
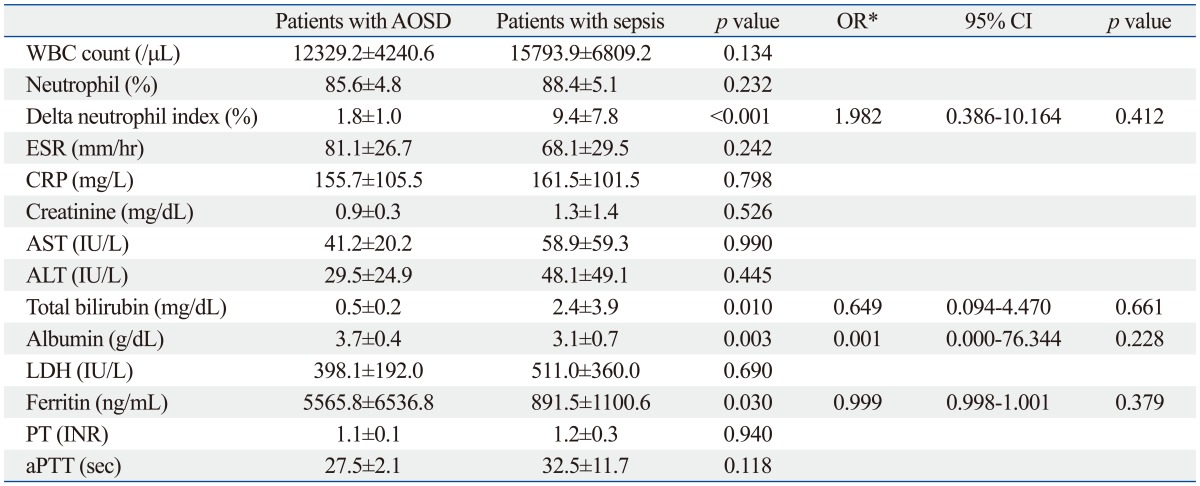
WBC, white blood cell; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactate dehydrogenase; PT, prothrombin time; aPTT, activated partial thromboplastic time; CI, confidence interval; OR, odds ratio; AOSD, adult onset Still's disease; DNI, delta neutrophil index; INR, international normalized ratio.
Continuous variables are expressed as mean±standard deviation, and compared by Mann-Whitney U test between the two groups.
*Odds ratio for predicting sepsis by binary logistic regression analysis of DNI, ferritin, albumin and total bilirubin.
Fig. 1.
Comparison of AUROC between delta neutrophil index (DNI) and ferritin. AUC of DNI was slightly higher than that of ferritin [0.896 (p<0.001) vs. 0.769 (p=0.008), respectively]. However, difference between the areas of DNI and ferritin was 0.0538, not statistically significant (p=0.68). AUC, area under curve.
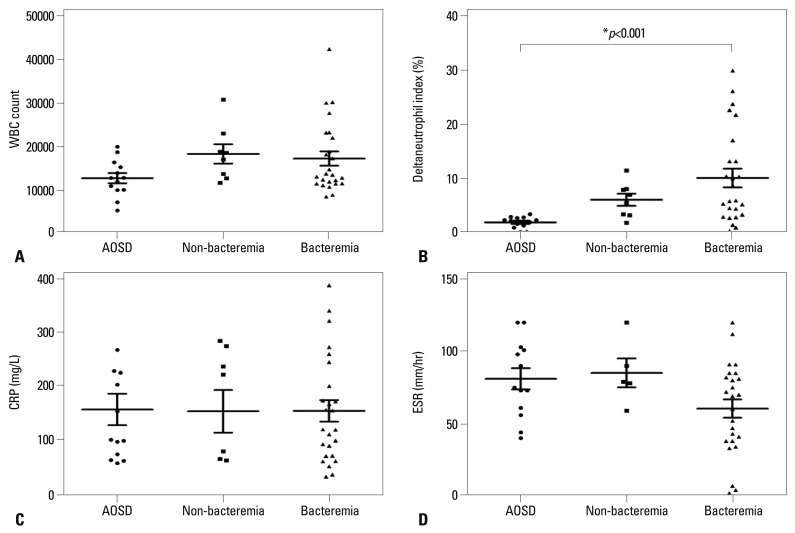
Sub-group analysis according to the presence of bacteremia
We further assigned sepsis patients to two sub-groups based on the presence of bacteremia. There were no significant differences in WBC counts and levels of ESR and CRP. However, AOSD patients had significantly lower DNI levels than sepsis patients with and without bacteremia (1.8±1.0% vs. 9.9±8.9%, p=0.001 and 1.8±1.0% vs. 7.9±3.7%, respectively) (Fig. 2).
Fig. 2.
Sub-group analysis according to the presence of bacteremia. Patients in sepsis group were divided into 10 patients of sepsis without bacteremia group and 27 patients of sepsis with bacteremia group. The levels of WBC count (A), CRP (C) and ESR (D) had no difference between three groups. The delta neutrophil index (B) had significant difference in AOSD, non-bacteremia and bacteremia group (1.8±1.0 vs. 7.9±3.7 vs. 9.9±8.9, p<0.001 respectively). WBC, white blood cell; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; AOSD, adult onset Still's disease.
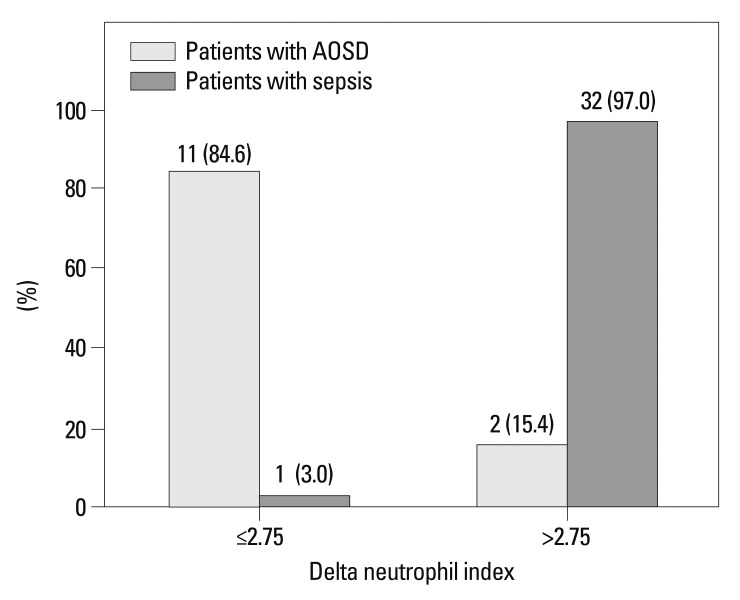
The cut-off value of DNI for differential diagnosis of sepsis from AOSD
We used AUROC to identify the optimal cut-off value of DNI for predicting sepsis in order to make differential diagnosis from AOSD. Thus, we selected a DNI of 2.75% as the cut-off value to maximize sensitivity (82.1%) and specificity (84.6%). In AOSD patients, 11 (84.6%) had a DNI value below 2.75% and 2 (15.4%) had a DNI over 2.75%. In contrast, only 1 sepsis patient (3.0%) had a DNI below 2.75%, while the remainder (97.0%) had a DNI value over 2.75%. And the relative risk for sepsis was 176.0 (95% confidential interval 14.501-2136.176) (Fig. 3).
Fig. 3.
Proportion of patients with AOSD and sepsis according to delta neutrophil index. Patients in two groups were divided according to cut-off value of DNI, 2.75%. In patients with AOSD, 11 patients (84.6%) had DNI below 2.75% and 2 patients (15.4%) had DNI over 2.75%. In patients with sepsis, 1 patient (3.0%) had DNI below 2.75% and the rest of them (97.0%) showed DNI over 2.75% (p<0.001). AOSD, adult onset Still's disease; DNI, delta neutrophil index.
DISCUSSION
AOSD is generally a mild and self-limiting disease, and it could progress to a chronic course with relapse and occasional life-threatening complications in one-third of patients. Kim, et al.14 indicated that short diagnostic delay was a good prognostic factor as a result of effective treatment, and response to glucocorticoid therapy was also an important prognostic factor. Moreover, mortality rate of AOSD was 9-10%, and main cause of death was sepsis, pneumonia and disease progression.14,15,16 Especially in sepsis, early recognition and early antibiotics therapy within the first six hours significantly decreased in-hospital mortality.17 Therefore, early differential diagnosis AOSD from sepsis might be a crucial for leading to a good prognosis.14,17,18 Nonetheless, in the clinical settings, and from the clinical point of view, there are several difficulties as follows: 1) it is difficult to distinguish between AOSD and sepsis in the early phase before the report on the results of culture studies; 2) treatment strategies are different between the two diseases; and 3) the long incubation period of culture studies hinders a rapid final diagnosis.
Several biomarkers for the differential diagnosis of the two diseases have so far been suggested, but definite biomarker had not yet been established clinically. Calprotectin produced by monocytes could not distinguish AOSD from microbial infection, despite good correlations with AOSD activity.4,5 And serum levels of cytokines involved in pathophysiology of AOSD did not show significant differences between the two diseases either.4 In addition, hyperferritinemia has been suggested as a most useful marker of AOSD,6 and hyperferritinemia with low glycosylated ferritin had been reported as a more powerful marker. However, they were also insufficient to differentiate AOSD from sepsis because elevated ferritin was often observed in other inflammatory diseases including sepsis and it might not be elevated in the early phase of AOSD.19 Fautrel, et al.20 could not show significant differences of hyperferritinemia with low glycosylated ferritin between AOSD and infection. Previous study suggested that only clinical manifestation could differentiate AOSD from sepsis.4 We compared clinical characteristics between two groups and clinical manifestations, including typical rash and arthralgia, could differentiate between two diseases, but nonspecific symptoms such as lymphadenopathy were often present in patients with sepsis in this study.
Thus, a useful serologic marker is needed to discriminate AOSD from sepsis. We introduced a novel value, DNI for the differential diagnosis of AOSD from sepsis. In the present study, we first verified that DNI in AOSD was significantly lower than in sepsis. One of typical feature of AOSD is leukocytosis with neutrophilia, which was similar to sepsis. The mechanism of leukocytosis remains uncertain although a previous study reported that granulocyte hyperplasia is found in the bone marrow of AOSD patients.21 However, over 80% of neutrophil are mature PMN in AOSD,18 which might be responsible for our results.
Previous studies showed that DNI was early prognostic factor for sepsis when they measured DNI within 24 hours of the onset of SIRS or within the first 24 hours of intensive care unit admission.12,13 With this reason, we analyzed mean DNI during the first 3 days of hospitalization and speculated that DNI could give a supplementary clue for the differential diagnosis between AOSD and sepsis in the early phase before confirming the result of culture studies. We demonstrated in the present study that DNI in patients with AOSD was markedly lower than in patients with sepsis. Moreover, DNIs in three patients who were admitted for AOSD flare were compared to those with confirmed microbial infection at admission, and DNIs of sepsis were found higher than those of AOSD flare in all three patients; 11.7%, 9.2%, and 3.9% vs. 1.2%, 2.8%, and 2.6% (data not shown).
Next, we also divided sepsis patients into two sub-groups depending on the presence of bacteremia, since DNI was reported to be associated with positive blood culture rates in suspected sepsis.8 Contrary to the above results, mean DNI in sepsis patients with bacteremia was slightly higher than in those without, but both mean DNIs of two subgroups were significantly higher than those in AOSD group. These results suggested that DNI could distinguish AOSD from sepsis in the early phase, regardless of the presence of bacteremia.
In addition to DNI, albumin, total bilirubin, and ferritin levels were also significantly different between the two groups in univariate analysis. When we analyzed variables, except ferritin, by using binary logistic analysis, DNI was an independent factor for predicting sepsis. However, in the multivariate analysis including ferritin, the usefulness of DNI for predicting sepsis did not surpass that of ferritin level. We compared AUROC between DNI and ferritin because hyperferritinemia was the most reliable biomarker for diagnosis of AOSD to date. Consequently, we identified that DNI had slightly higher AUC than that of ferritin despite of no statistical significance.
To evaluate the weight of the clinical implication of DNI for differentiating AOSD and sepsis, we set the cut-off value of DNI for differentiating AOSD and sepsis at 2.75%, with a sensitivity of 82.1% and a specificity of 84.6%, and found that its relative risk for sepsis was 176. In previous study that compared patients with sepsis and healthy controls, the cut-off value for sepsis was 2.7%, similar to our result.13 DNI cannot be used for differentiation AOSD from other inflammatory disease, except infection, because elevated DNI is specific for sepsis. However, we have the possibility that DNI can be a reliable marker for distinguishing between AOSD and sepsis that have relatively high sensitivity and specificity. Also, DNI is included in the complete blood count test, which is routinely performed without additional costs or tests when patients with fever are admitted to a hospital. Considering that there are only a few objective laboratory results to help physicians to discriminate AOSD and sepsis in their early phase, DNI can be a raid and efficious marker for it. Consequently, we suggest that DNI might be useful to differentiate AOSD from sepsis as a supplementary variable to ferritin, although DNI could not be an independent predictive value for differential diagnosis between the two diseases.
This study has two limitations: first, small number of AOSD patients was enrolled in the study due to its rare incidence, and second, other biomarkers such as procalcitonin or calprotectin were not analyzed. If future study includes larger number of AOSD patients and measure these biomarkers together, it might reveal a dynamic role for differential diagnosis of AOSD from sepsis in early phase.
In conclusion, we suggest that DNI might be a useful marker for differential diagnosis between AOSD from sepsis at an early phase of the two diseases when their disease patterns are indistinguishable.
ACKNOWLEDGEMENTS
The authors are grateful to Dong-Su Jang (Medical Illustrator, Medical Research Support Section, Yonsei University College of Medicine, Seoul, Korea) for his help with the figures.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Bagnari V, Colina M, Ciancio G, Govoni M, Trotta F. Adult-onset Still's disease. Rheumatol Int. 2010;30:855–862. doi: 10.1007/s00296-009-1291-y. [DOI] [PubMed] [Google Scholar]
- 2.Fautrel B, Zing E, Golmard JL, Le Moel G, Bissery A, Rioux C, et al. Proposal for a new set of classification criteria for adult-onset still disease. Medicine (Baltimore) 2002;81:194–200. doi: 10.1097/00005792-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. Preliminary criteria for classification of adult Still's disease. J Rheumatol. 1992;19:424–430. [PubMed] [Google Scholar]
- 4.Rau M, Schiller M, Krienke S, Heyder P, Lorenz H, Blank N. Clinical manifestations but not cytokine profiles differentiate adult-onset Still's disease and sepsis. J Rheumatol. 2010;37:2369–2376. doi: 10.3899/jrheum.100247. [DOI] [PubMed] [Google Scholar]
- 5.Jung SY, Park YB, Ha YJ, Lee KH, Lee SK. Serum calprotectin as a marker for disease activity and severity in adult-onset Still's disease. J Rheumatol. 2010;37:1029–1034. doi: 10.3899/jrheum.091120. [DOI] [PubMed] [Google Scholar]
- 6.Van Reeth C, Le Moel G, Lasne Y, Revenant MC, Agneray J, Kahn MF, et al. Serum ferritin and isoferritins are tools for diagnosis of active adult Still's disease. J Rheumatol. 1994;21:890–895. [PubMed] [Google Scholar]
- 7.Cantarini L, Giani T, Fioravanti A, Iacoponi F, Simonini G, Pagnini I, et al. Serum amyloid A circulating levels and disease activity in patients with juvenile idiopathic arthritis. Yonsei Med J. 2012;53:1045–1048. doi: 10.3349/ymj.2012.53.5.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci. 2008;38:241–246. [PubMed] [Google Scholar]
- 9.Ansari-Lari MA, Kickler TS, Borowitz MJ. Immature granulocyte measurement using the Sysmex XE-2100. Relationship to infection and sepsis. Am J Clin Pathol. 2003;120:795–799. doi: 10.1309/LT30-BV9U-JJV9-CFHQ. [DOI] [PubMed] [Google Scholar]
- 10.Selig C, Nothdurft W. Cytokines and progenitor cells of granulocytopoiesis in peripheral blood of patients with bacterial infections. Infect Immun. 1995;63:104–109. doi: 10.1128/iai.63.1.104-109.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cavallazzi R, Bennin CL, Hirani A, Gilbert C, Marik PE. Is the band count useful in the diagnosis of infection? An accuracy study in critically ill patients. J Intensive Care Med. 2010;25:353–357. doi: 10.1177/0885066610377980. [DOI] [PubMed] [Google Scholar]
- 12.Park BH, Kang YA, Park MS, Jung WJ, Lee SH, Lee SK, et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect Dis. 2011;11:299. doi: 10.1186/1471-2334-11-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, et al. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012;37:242–246. doi: 10.1097/SHK.0b013e3182454acf. [DOI] [PubMed] [Google Scholar]
- 14.Kim HA, Sung JM, Suh CH. Therapeutic responses and prognosis in adult-onset Still's disease. Rheumatol Int. 2012;32:1291–1298. doi: 10.1007/s00296-011-1801-6. [DOI] [PubMed] [Google Scholar]
- 15.Ohta A, Yamaguchi M, Tsunematsu T, Kasukawa R, Mizushima H, Kashiwagi H, et al. Adult Still's disease: a multicenter survey of Japanese patients. J Rheumatol. 1990;17:1058–1063. [PubMed] [Google Scholar]
- 16.Zeng T, Zou YQ, Wu MF, Yang CD. Clinical features and prognosis of adult-onset still's disease: 61 cases from China. J Rheumatol. 2009;36:1026–1031. doi: 10.3899/jrheum.080365. [DOI] [PubMed] [Google Scholar]
- 17.Fautrel B. Adult-onset Still disease. Best Pract Res Clin Rheumatol. 2008;22:773–792. doi: 10.1016/j.berh.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Gauer RL. Early recognition and management of sepsis in adults: the first six hours. Am Fam Physician. 2013;88:44–53. [PubMed] [Google Scholar]
- 19.Fautrel B. Ferritin levels in adult Still's disease: any sugar? Joint Bone Spine. 2002;69:355–357. doi: 10.1016/s1297-319x(02)00409-8. [DOI] [PubMed] [Google Scholar]
- 20.Fautrel B, Le Moël G, Saint-Marcoux B, Taupin P, Vignes S, Rozenberg S, et al. Diagnostic value of ferritin and glycosylated ferritin in adult onset Still's disease. J Rheumatol. 2001;28:322–329. [PubMed] [Google Scholar]
- 21.Min JK, Cho CS, Kim HY, Oh EJ. Bone marrow findings in patients with adult Still's disease. Scand J Rheumatol. 2003;32:119–121. doi: 10.1080/03009740310000148. [DOI] [PubMed] [Google Scholar]